Abstract
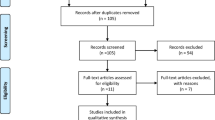
Menstrual function is strongly affected by nutritional status and energy availability in female athletes, and impaired menstrual function can impact bone mineral density. Nutritional interventions have been proposed to mitigate menstrual dysfunction. The purpose of this systematic review was to assess the ability of nutritional interventions, directed at improving energy availability, to restore normal menstrual status in female athletes. PubMed, Cinahl, and SportDiscus databases were comprehensively searched. Included studies had to investigate the impact of increasing energy availability in female athletes through a nutritional intervention. The primary outcome measure of interest was menstrual status. Included studies were reviewed for methodological rigor using the American Academy of Dietetics Quality Criteria Checklist. Five studies met the inclusion criteria. Of the athletes who completed the interventions in the studies, 0–100% resumed normal menses. For those that improved, the mean length of time for return to menses ranged from 2.63 to 15.6 months. The length of the interventions (3–9 months), mean ages of the participants (17–1-22.6 years), and particular dietary intervention(s) (counseling, education, and nutritional supplementation) varied between the studies. Nutritional interventions may restore normal menses in some female athletes. Educational strategies targeted at improved eating and understanding the energy demands of sport, as well as weekly interaction with athletes should be considered.

Similar content being viewed by others
Data Availability
Data for articles reviewed can be found in Table 2. All articles are available upon request.
References
Dusenbery M. & Lee J. Charts: the state of women’s athletics, 40 years after Title IX. Available at: http://www.motherjones.com/politics/2012/06/charts-womens-athletics-title-nine-ncaa; 2012. (Accessed October 18, 2016).
De Souza MJ, Nattiv A, Joy, E., Misra M, Williams NI, Mallinson RJ, ... Matheson G. 2014 female athlete triad coalition consensus statement on treatment and return to play of the female athlete triad: 1st International Conference held in San Francisco, California, May 2012 and 2nd International Conference held in Indianapolis, Indiana, M. Br J Sports Med.2014;48(4): 289–289. doi: https://doi.org/10.1136/bjsports-2013-093218.
Nativ A, Loucks AB, Manore MM, Sanborn CF, Sundgot-Borgen J, Warren MP. American college of sports medicine position stand. The female athlete triad. Med Sci Sports Exerc. 2007;39(10):1867–2.
Gibbs JC, Williams NI, De Souza JM. Prevalence of individual and combined components of the female athlete triad. Med Sci Sports Exerc. 2013;45(5):985–96.
Warr BJ, Woolf K. The female athlete triad: patients do best with a team approach to care. JAAPA : Official Journal of the American Academy of Physician Assistants. 2011;24(4):50–5.
Zach KN, Machin ALS, Hoch AZ. Advances in management of the female athlete triad and eating disorders. Clin Sports Med. 2011;30(3):551–73.
Manore MM, Kam LC, & Loucks AB. The female athlete triad: components, nutrition issues, and health consequences. 2007 IAAF Consensus Conference on Nutrition for Athletics. J Sports Sci. 2007;25: S61–71. Department of Nutrition and Exercise Sciences, Oregon State University, Milam Hall 103, Corvallis, OR 97331, USA.
Nazem TG, Ackerman KE. The female athlete triad. Sports Health. 2012;4(4):302–11.
Kelsey JL, Bachrach LK, Procter-Gray E, Nieves J, Greendale GA, Sowers M, et al. Risk factors for stress fracture among young female cross-country runners. Med Sci Sports Exerc. 2007;39(9):1457–63. https://doi.org/10.1249/mss.0b013e318074e54b.
Williams NI, Mallinson RJ, De Souza MJ. Rationale and study design of an intervention of increased energy intake in women with exercise-associated menstrual disturbances to improve menstrual function and bone health: the REFUEL study. Contemp Clin Trials Commun. 2019;14:100325.
Ackerman KE, Pierce L, Guereca G, Slattery M, Lee H, Goldstein M, et al. Hip structural analysis in adolescent and young adult oligoamenorrheic and eumenorrheic athletes and nonathletes. J Clin Endocrinol Metab. 2013;98:1742–9.
Southmayd EA, Hellmers AC, De Souza MJ. Food versus pharmacy: assessment of nutritional and pharmacological strategies to improve bone health in energy-deficient exercising women. Curr Osteoporos Rep. 2017;15:459–72.
Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Lebrun C, et al. The IOC consensus statement: beyond the female athlete triad--relative energy deficiency in sport (RED-S). Br J Sports Med. 2014;48(7):491–7. https://doi.org/10.1136/bjsports-2014-093502.
Thralls KJ, Nichols JF, Barrack MT, Kern M, Rauh MJ. Body mass-related predictors of the female athlete triad among adolescent athletes. Int J Sport Nutr Exerc Metab. 2016;26(1):17–25. https://doi.org/10.1123/ijsnem.2015-0072.
Matzkin E, Curry EJ, Whitlock K. Female athlete triad: past, present, and future. J Am Acad Orthop Surg. 2015;23(7):424–32. https://doi.org/10.5435/JAAOS-D-14-00168.
Barrack MT, Ackerman KE, Gibbs JC. Update on the female athlete triad. Curr Rev Musculoskelet Med. 2013;6(2):195–204. https://doi.org/10.1007/s12178-013-9168-9.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche P, Loannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(jul21 1):b2700–0. https://doi.org/10.1136/bmj.b2700.
Durieux, N., Pasluea, F., & Howick, J., n.d. OCEBM Levels of Evidence - CEBM. Available at: http://www.cebm.net/ocebm-levels-of-evidence/ (Accessed 9 October 2015).
Academy of Nutrition and Dietetics Reference Library. Academy of nutrition and dieticians evidence analysis manual. Available at: https://www.andeal.org/evidence-analysis-manual ; 2005 (Accessed January 16, 2017).
Cialdella-Kam L, Guebels CP, Maddalozzo GF, Manore MM. Dietary intervention restored menses in female athletes with exercise-associated menstrual dysfunction with limited impact on bone and muscle health. Nutrients. 2014;6(8):3018–39. https://doi.org/10.3390/nu6083018.
Guebels CP, Kam LC, Maddalozzo GF, Manore MM. Active women before/after an intervention designed to restore menstrual function: resting metabolic rate and comparison of four methods to quantify energy expenditure and energy availability. Int J Sport Nutr Exerc Metab. 2014;24(1):37–46. https://doi.org/10.1123/ijsnem.2012-0165.
Arends JC, Cheung MYC, Barrack MT, Nattiv A. Restoration of menses with nonpharmacologic therapy in college athletes with menstrual disturbances: a 5-year retrospective study. Int J Sport Nutr Exerc Metab. 2012;22(2):98–108.
Lagowska K, Kapczuk K, Friebe Z, Bajerska A. Effects of dietary intervention in young female athletes with menstrual disorders. J Int Soc Sports Nutr. 2014a;11:21. https://doi.org/10.1186/1550-2783-11-21.
Lagowska K, Kapczuk K, Jeszka J. Nine–month nutritional intervention improves restoration of menses in young female athletes and ballet dancers. J Int Soc Sports Nutr. 2014b;11(1):52. https://doi.org/10.1186/s12970-014-0052-9.
Abood DA, Black DR, Birnbaum RD. Nutrition education intervention for college female athletes. J Nutr Educ Behav. 2004;36:135–9. https://doi.org/10.1016/S1499-4046(06)60150-4
Mallinson RJ, Williams NI, Olmsted MP, Scheid JL, Riddle MS, De Souza MJ. A case report of recovery of menstrual function following a nutritional intervention in two exercising women with amenorrhea of varying duration. J Int Soc Sports Nutr. 2013;10(1):34. https://doi.org/10.1186/1550-2783-10-34.
Pantano KJ. Strategies used by physical therapists in the U.S. for treatment and prevention of the female athlete triad. Phys Ther Sport. 2009;10(1):3–11.
Papanek PE. The female athlete triad: an emerging role for physical therapy. J Orthop Sports Phys Ther. 2003;33(10):594–614.
Kopp-Wodroffe S, Manore MM, Dueck CA, Skinner JS, Matt KS. Energy and nutrient status of amennorheic athletes participating in a diet and exercise training intervention program. J Int Soc Sports Nutr. 1999;9:70–88.
Dueck CA, Matt KS, Manore MM, Skinner JS. Treatment of athletic amenorrhea with a diet and training intervention program. J Int Soc Sports Nutr. 1996;6(1):24–40.
Author information
Authors and Affiliations
Contributions
LS contributed to study design, data collection, data analysis and interpretation, drafting and article revision, and approval of the final manuscript. JB contributed to data collection and analysis, drafting of article, and approval of the final manuscript. BH contributed to data analysis and interpretation, drafting and revision, and approval of the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
IRB approval is not needed for a systematic review.
Informed Consent
No informed consent is needed for a systematic review.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Medicine
Rights and permissions
About this article
Cite this article
Stickler, L.G., Hoogenboom, B.J. & Brown, J. The Impact of Nutritional Intervention on Menstrual Dysfunction in Female Athletes: a Systematic Review. SN Compr. Clin. Med. 1, 669–676 (2019). https://doi.org/10.1007/s42399-019-00107-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42399-019-00107-z