Abstract
The aim
The present study aims to conduct a descriptive analysis by reviewing in vivo and in vitro studies concerned with the antibacterial effect of Er:YAG laser (2940 nm) and their effects on implant surfaces at different parameters for peri-implantitis treatment.
Materials and methods
The PubMed and Google Scholar had been used to search for articles focused on the antibacterial effect of Er:YAG laser (2940 nm) in the treatment of peri-implantitis and their effects on implant surfaces. This literature search was limited to 10 years (January 2007–March 2017).
Results
The safe settings of Er:YAG laser (2940 nm) which may be used as an antibacterial effect without surface alteration or increase of temperature in the treatment of peri-implantitis are 100 mJ/pulse, 1 W, 10 Hz, and 12.74 J/cm2 for 60 s.
Conclusion
A consideration should be taken when Er:YAG laser 2940 nm wavelength is used to avoid a negative thermal and characteristic effect on the implant surfaces, where the favorable settings which can be used in the treatment of peri-implantitis are 100 mJ/pulse, 1 W, 10 Hz, and 12.74 J/cm2 for 60 s.


Similar content being viewed by others
Abbreviations
- ERL:
-
Er;YAG laser
- TPS:
-
Titanium plasma sprayed
- PW:
-
Pulse wave
- MR:
-
Mucosal recession
- HA:
-
Hydroxyapatite
- s:
-
Second
- PD:
-
Pocket depth
- SLA:
-
Sand blasted, large grit, acid-etched
- μs:
-
Microsecond
- PI:
-
Plaque index
- Y-TZP:
-
Yittrium-stabilized tetragonal zirconia polycrystal
- ms:
-
Millisecond
- BOP:
-
Bleeding on probing
- CPS:
-
Cotton pellets + plastic curets + sterile saline
- μm:
-
Micrometer
- LS-LPS:
-
Low-power setting
- HS-HPS:
-
High power setting
- CAL:
-
Clinical attachment level
- TiO2:
-
Fluoride modified
- SAE:
-
Sandblasted and acid-etched
- AO:
-
Anodic oxidized
- N info:
-
No information
- M:
-
Machined
- Ra:
-
Roughness
References
Misch CE (2007) Contemporary implant dentistry, 3rd edn. Mosby, St. Louis, pp 3–25
Greenstein G, Cavallaro J, Romanos G, Tarnow D (2008) Clinical recommendation for avoiding and managing surgical complications associated with implant dentistry. A review. J Periodontol 79:1317–1329. https://doi.org/10.1902/jop.2008.070067
Porter JA, von Fraunhofer JA (2005) Success or failure of dental implants? A literature review with treatment considerations. Gen Dent 53(6):423–432
Malet J, Mora F, Bouchard P (2012) Implant dentistry at a glance, 1st edn. Wiley-Blackwell, Chichester, pp 24, 25, 102, 103, 106–108
Rosen P, Cochran D, Froum S, McAllister B, Renvert S, Wang H-L (2013) Peri-implant mucositis and peri-implantitis: a current understanding of their diagnosis and clinical implications. J Periodontol 84:436–443. https://doi.org/10.1902/jop.2013.134001
Figuero E, Graziani F, Sanz I, Herrera D, Sanz M (2014) Management of peri-implant mucositis and peri-implantitis. Periodontol 66:255–273
Romanos GE, Gupta B, Yunker M, Romanos EB, Malmstrom H (2013) Laser use in dental implantology. Implant Dent 22:282–288. https://doi.org/10.1097/ID.0b013e3182885fcc
Scott Froum DDS (2011) Review of the treatment protocols for peri-implantitis. online article available at website http://www.dentistryiq.com/articles/2011/10/review of the treatment protocols for peri-implantitis.html.
Alshehri FA (2016) The role of lasers in the treatment of peri-implant diseases: a review. Saudi Dent J 28:103–108
Javed F, Romanos GE (2009) Impact of diabetes mellitus and glycemic control on the osseointegration of dental implants: a systematic literature review. J Periodontol 80:1719–1730. https://doi.org/10.1902/jop.2009.090283
Renvert S, Quirynen M (2015) Risk indicators for peri-implantitis. A narrative review. Clin Oral Implants Res 26:15–44. https://doi.org/10.1111/clr.12636
Maruyama N, Maruyama F, Takeuchi Y, Aika- wa C, Izumi Y, Nakagawa I (2014) Intraindividual variation in core microbiota in peri-implantitis and periodontitis. Sci Rep 4:6602. https://doi.org/10.1038/srep06602
Heitz-Mayfield LJ, Lang NP (2010) Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis. Periodontol 53:167–181. https://doi.org/10.1111/j.1600-0757.2010.00348.x
Renvert S, Polyzois I (2015) Risk indicators for peri-implant mucositis: a systematic literature review. J Clin Periodontol 42:172–186. https://doi.org/10.1111/jcpe.12346
Lang NP, Berglundh T (2011) Periimplant diseases: where are we now?—consensus of the seventh European workshop on periodontology. J Clin Periodontol 38:178–181. https://doi.org/10.1111/j.1600-051X.2010.01674.x
Linkevicius T, Puisys A, Vindasiute E, Linke-viciene L, Apse P (2013) Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin Oral Implants Res 24:1179–1184. https://doi.org/10.1111/j.1600-0501.2012.02570.x
Dalago HR, Schuldt Filho G, Rodrigues MA, Renvert S, Bianchini MA (2016) Risk indicators risk indicators for peri-implantitis. A cross sectional study with 916 patients. Clinical Oral Implants 00:1–7. https://doi.org/10.1111/clr.12772
Strietzel FP, Reichart PA, Kale A, Kulkarni M, Wegner B, Kuchler I (2007) Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis. J Clin Periodontol 34:523–544. https://doi.org/10.1111/j.1600-051X.2007.01083.x
Klokkevold PR, Han TJ (2007) How do smoking, diabetes, and periodontitis affect outcomes of implant treatment? Int J Oral Maxillofac Implants 22:173–202
Rinke S, Ohl S, Ziebolz D, Lange K, Eickholz P (2011) Prevalence of peri-implant disease in partially edentulous patients: a practice based cross sectional study. Clin Oral Implants Res 22:826–833. https://doi.org/10.1111/j.1600-0501.2010.02061.x
Laine ML, Leonhardt A, Roos-Jansa ker AM et al (2006) IL1RN gene polymorphism is associated with periimplantitis. Clin Oral Implants Res 17:380–385. https://doi.org/10.1111/j.1600-0501.2006.01249.x
Fu J-H, Hsu Y-T, Wang H-L (2012) Identifying occlusal overload and how to deal with it to avoid marginal bone loss around implants. Eur J Oral Implantol 5:91–103
Oates TW, Dowell S, Robinson M, McMahan CA (2009) Glycemic control and implant stabilization in type 2 diabetes mellitus. J Dent Res 88:367–371. https://doi.org/10.1177/0022034509334203
Krennmair G, Seemann R, Piehslinger E (2010) Dental implants in patients with rheumatoid arthritis: clinical outcome and peri-implant findings. J Clin Periodontol 37:928–936. https://doi.org/10.1111/j.1600-051X.2010.01606.x
Galindo-Moreno P, Fauri M, Avila-Ortiz G, Fernandez Barbero JE, Cabrera-Leon A, Sanchez-Fernandez E (2005) Influence of alcohol and tobacco habits on peri-implant marginal bone loss: a prospective study. Clin Oral Implants Res 16:579–586. https://doi.org/10.1111/j.1600-0501.2005.01148.x
Froum SJ, Rosen PS (2012) A proposed classification for peri-implantitis. Int J Periodontics Restorative Dent 32:533–540
Bobia F, Pop RV (2010) Periimplantitis. Aetiology, diagnosis, treatment. A review from the literature. Curr Health Sci J 36:171–175
Algraffee H, Borumandi F, Cascarini L (2011) Peri-implantitis (review). Br J Oral Maxillofac Surg 50:689–694. https://doi.org/10.1016/j.bjoms.2011.11.020
Prathapachandran J, Suresh N (2012) Management of peri-implantitis. Dent Res J (Isfahan) 9:516–521
Roncati M, Lucchese A, Carinci F (2013) Non-surgical treatment of peri-implantitis with the adjunctive use of an 810 nm diode laser. J Indian Soc Periodontol 17:812–815
Smeets R, Henningseng A, Jung O, Heiland M, Hammächer C, Stein JM (2014) Definition, etiology, prevention and treatment of peri-implantitis, a review. Head Face Med 10:4–8. https://doi.org/10.1186/1746-160X-10-34
Meyle J (2012) Mechanical, chemical and laser treatments of the implant surface in the presence of marginal bone loss around dental implants. Eur J Oral Implantol 5:71–81
Khandge N, Pradhan S, Doshi Y, Kulkarni A (2013) Comparison of the effects of different laser wavelengths on implants surfaces. Int J Laser Dentistry 3:14–18
Convissar RA (2015) Principles and practice of laser dentistry, 2nd edn, pp 107–109
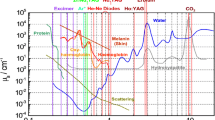
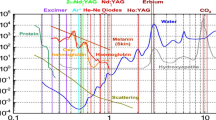
Dr. rer. Medic. René Franzen lectures. Module 5, 24-30.10.2016. Master of science in laser in dentistry, EN2015, Aachen university
Dr. rer. Medic. René Franzen lectures. Module 3, 14-18.03.2016. Master of science in laser in dentistry, EN2015, Aachen University
Bader C, Krejci I (2006) Indication and limitation of Er:YAG laser applications in dentistry. Am J Dent 19:181
Kreisler M, Kohnen W, Marinello C, Götz H, Duschner H, Jansen B, D'Hoedt B (2002) Bactericidal effect of the Er:YAG laser on dental implant surface: an in vitro study. J Periodontol 73:1292–1298. https://doi.org/10.1902/jop.2002.73.11.1292
Takasaki AA, Aoki A, Mizutani K, Kikuchi S, Oda S, Ishikawa I (2007) Er:YAG laser therapy for peri-implant infection: a histological study. Lasers Med Sci 22:143–157. https://doi.org/10.1007/s10103-006-0430-x
Yan M, Liu M, Wang M, Yin F, Xia H (2015) The effects of Er:YAG on the treatment of peri-implantitis: a meta-analysis of randomized controlled trials. Lasers Med Sci 30:1843–1853. https://doi.org/10.1007/s10103-014-1692-3
Kamel MS, Khosa A, Tawse-Smith A, Leichter J (2014) The use of laser therapy for dental implant surface decontamination: a narrative review of in vitro studies. Lasers Med Sci 29:1977–1985. https://doi.org/10.1007/s10103-013-1396-0
Stübinger S, Etter C, Miskiewicz M, Homann F, Saldamli B, Wieland M, Sader R (2010) Surface alteration of polished and sandblasted and acid-etched titanium implants after Er:YAG, carbon dioxide, and diode laser irradiation. Int J Oral Maxillofac Implants 25:104–111
Romanos GE, Gutknecht N, Dieter S, Schwarz F, Crespi R, Sculean A (2009) Laser wavelengths and oral implantology: Review Article. Lasers Med Sci 24:961–970
Friedmann A, Antic L, Bernimoulin J-P, Purucker P (2006) In vitro attachment of osteoblasts on contaminated rough titanium surfaces treated by Er:YAG laser. J Biomed Mater Res 79A:53–60. https://doi.org/10.1002/jbm.a.30699
Schwarz F, Sahm N, Iglhaut G, Becker J (2011) Impact of the method of surface debridement and decontamination on the clinical outcome following combined surgical therapy of peri-implantitis: a randomized controlled clinical study. J Clin Periodontol 38:276–284. https://doi.org/10.1111/j.1600-051X.2010.01690.x
Wang Y, Zhang Y, Miron RJ (2015) Health, maintenance, and recovery of soft tissues around implants. Clin Implant Dent Relat Res 18:618–634. https://doi.org/10.1111/cid.12343
Takasaki AA, Mizutani K, Schwarz F et al (2009) Application of antimicrobial photodynamic therapy in periodontal and peri-implant diseases. Periodontol 51:109–140. https://doi.org/10.1111/j.1600-0757.2009.00302.x
Rutger Persson G, Roos-Jansaker A-M, Lindahl C, Renvert S (2011) Microbiologic results after non-surgical erbium-doped:yttrium, aluminum, and garnet laser or air-abrasive treatment of peri-implantitis: a randomized clinical trial. J Periodontol 82:1267–1278. https://doi.org/10.1902/jop.2011.100660
Renvert S, Lindahl C, Roos Jansaker A-M, Persson GR (2011) Treatment of peri-implantitis using Er:YAG laser or an air-abrasive device: a randomized clinical trial. J Clin Periodontol 38:65–73. https://doi.org/10.1111/j.1600-051X.2010.01646.x
Badran Z, Bories C, Struillou X, Saffarzadeh A, Verner C, Soueida A (2011) Er:YAG laser in the clinical management of severe peri-implantitis: a case report. J Oral Implantol. https://doi.org/10.1563/AAID-JOI-D-09-00145.1
Schwarz F, John G, Mainusch S, Sahm N, Becker J (2012) Combined surgical therapy of peri-implantitis evaluating two methods of surface debridement and decontamination. A two-year clinical follow up report. J Clin Periodontol 39:789–797. https://doi.org/10.1111/j.1600-051X.2012.01867.x
Schwarz F, Hegewald A, John G, Sahm N, Becker J (2013) Four-year follow-up of combined surgical therapy of advanced peri-implantitis evaluating two methods of surface decontamination. J Clin Periodontol 40:962–967. https://doi.org/10.1111/jcpe.12143
Schwarz F, John G, Hegewald A, Becker J (2015) Non-surgical treatment of peri-implant mucositis and peri-implantitis at zirconia implants: a prospective case series. J Clin Periodontol 42:783–788. https://doi.org/10.1111/jcpe.12439
Hauser-Gerspach I, Mauth C, Waltimo T, Meyer J, Stübinger S (2014) Effects of Er:YAG laser on bacteria associated with titanium surfaces and cellular response in vitro. Lasers Med Sci 29:1329–1337. https://doi.org/10.1007/s10103-013-1303-8
Scarano A, Nardi G, Murmura G, Rapani M, Mortellaro C (2016) Evaluation of the removal bacteria on failed titanium implants after irradiation with erbium-doped yttrium aluminium garnet laser. J Craniomaxillofac Surg 27:1202–1204. https://doi.org/10.1097/SCS.0000000000002735
Chen C-J, Ding S-J, Chen C-C (2016) Effects of surface conditions of titanium dental implants on bacterial adhesion. Photomed Laser Surg 34:379–388. https://doi.org/10.1089/pho.2016.4103
Al-Hashedi AA, Laurenti M, Benhamou V, Tamimi F (2016) Decontamination of titanium implants using physical methods. Clin Oral Implants Res 00:1–9. https://doi.org/10.1111/clr.12914
Stübinger S, Homann F, Etter C, Miskiewicz M, Wieland M, Sader R (2008) Effect of Er:YAG, CO2 and diode laser irradiation on surface properties of zirconia endosseous dental implants. Lasers Surg Med 40:223–228. https://doi.org/10.1002/lsm.20614
Duarte PM, Reis AF, de Freitas PM, Ota-Tsuzuki C (2009) Bacterial adhesion on smooth and rough titanium surfaces after treatment with different instruments. J Periodontol 80:1824–1832. https://doi.org/10.1902/jop.2009.090273
Cavalcanti AN, Pilecki P, Foxton RM, Watson TF, Oliveira MT, Gianinni M, Marchi GM (2009) Evaluation of the surface roughness and morphologic features of Y-TZP ceramics after different surface treatments. Photomed Laser Surg 27:473–479. https://doi.org/10.1089/pho.2008.2293
Kim S-W, Kwon Y-H, Chung J-H, Shin S-I, Herr Y (2010) The effect of Er:YAG laser irradiation on the surface microstructure and roughness of hydroxyapatite-coated implant. J Periodontal Implant Sci 40:276–282. https://doi.org/10.5051/jpis.2010.40.6.276
Stübinger S, Etter C, Miskiewicz M, Homann F, Saldamli B, Wieland M, Sader R (2010) Surface alterations of polished and sandblasted and acid-etched titanium implants after Er:YAG, carbon dioxide, and diode laser irradiation. Int J Oral Maxillofac Implants 25:104–111
Lee J-H, Kwon Y-H, Herr Y, Shin S-I, Chung J-H (2011) Effect of erbium-doped: yttrium, aluminium and garnet laser irradiation on the surface microstructure and roughness of sand-blasted, large grit, acid-etched implants. J Periodontal Implant Sci 41:135–142. https://doi.org/10.5051/jpis.2011.41.3.135
Galli C, Macaluso GM, Elezi E, Ravanetti F, Cacchioli A, Gualini G, Passeri G (2011) The effects of Er:YAG laser treatment on titanium surface profile and osteoblastic cell activity: an in vitro study. J Periodontol 82:1169–1177. https://doi.org/10.1902/jop.2010.100428
Shin S-I, Min H-K, Park B-H, Kwon Y-H, Park J-B, Herr Y, Heo S-J, Chung J-H (2011) The effect of Er:YAG laser irradiation on the scanning electron microscopic structure and surface roughness of various implant surfaces: an in vitro study. Lasers Med Sci 26:767–776. https://doi.org/10.1007/s10103-010-0819-4
Kim J-H, Herr Y, Chung J-H, Shin S-I, Kwon Y-H (2011) The effect of erbium-doped: yttrium, aluminium and garnet laser irradiation on the surface microstructure and roughness of double acid-etched implants. J Periodontal Implant Sci 41:234–241. https://doi.org/10.5051/jpis.2011.41.5.234
Geminiani A, Caton JG, Romanos GE (2011) Temperature increase during CO2 and Er:YAG irradiation on implant surfaces. Implant Dent 20:1. https://doi.org/10.1097/ID.0b013e3182310d57
Park J-H, Heo S-J, Koak J-Y, Kim S-K, Han C-H, Lee J-H (2012) Effects of laser irradiation on machined and anodized titanium disks. Int J Oral Maxillofac Implants 27:265–272
Yamamoto A, Tanabe T (2013) Treatment of peri-implantitis around TiUnite-surface implants using Er:YAG laser Microexplosion. Int J Periodontics Restorative Dent 33:21–29. https://doi.org/10.11607/prd.1593
Shin S-I, Lee E-K, Kim J-H, Lee J-H, Kim S-H, Kwon Y-H, Herr Y, Chung J-H (2013) The effect of Er:YAG laser irradiation on hydroxyapatite-coated implants and fluoride-modified TiO2-blasted implant surfaces: a microstructural analysis. Lasers Med Sci 28:823–831. https://doi.org/10.1007/s10103-012-1162-8
Taniguchi Y, Aoki A, Mizutani K, Takeuchi Y, Ichinose S, Takasaki AA, Schwarz F, Izumi Y (2013) Optimal Er:YAG laser irradiation parameters for debridement of microstructured fixture surfaces of titanium dental implants. Lasers Med Sci 28:1057–1068. https://doi.org/10.1007/s10103-012-1171-7
Turp V, Akgungor G, Sen D, Tuncelli B (2014) Evaluation of surface topography of zirconia ceramic after Er:YAG laser etching. Photomed Laser Surg 32:533–539. https://doi.org/10.1089/pho.2014.3730
Arami S, Tabatabae MH, Namdar SF, Chiniforush N (2014) Effects of different lasers and particle abrasion on surface characteristics of zirconia ceramics. J Dent, Tehran University of Medical Sciences 11:233–241
Ayobian-Markazi N, Karimi M, Safar-Hajhosseini A (2015) Effects of Er:YAG laser irradiation on wettability, surface roughness, and biocompatibility of SLA titanium surfaces: an in vitro study. Lasers Med Sci 30:561–566. https://doi.org/10.1007/s10103-013-1361-y
Caglar I, Yanıkoglu N (2016) The effect of sandblasting, Er:YAG laser, and heat treatment on the mechanical properties of different zirconia cores. Photomed Laser Surg 34:17–26. https://doi.org/10.1089/pho.2015.3980
Prof. Dr. med. dent. Norbert Gutknecht lectures. Module 3. 14-20.03.2016. Master of science in laser in dentistry. Aachen University. “EN2015”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Smeo, K., Nasher, R. & Gutknecht, N. Antibacterial effect of Er:YAG laser in the treatment of peri-implantitis and their effect on implant surfaces: a literature review. Laser Dent Sci 2, 201–211 (2018). https://doi.org/10.1007/s41547-018-0043-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41547-018-0043-2