Abstract
The hydroxyl radical, one of the reactive oxygen species, has one unpaired electron in the structure, so that it tends to deprive other substances of an electron which is so-called oxidation. It is known that hydroxyl radicals produced by immunological response kill invading microorganisms by the oxidation. Besides the immune system, it has been demonstrated that hydroxyl radicals play an important role in the bactericidal action of antibiotics. In this context, we have conducted a research to develop disinfection techniques utilizing artificially generated hydroxyl radicals. We adopted photolysis of H2O2, sonolysis of water and the other photo-chemical reaction as generators of hydroxyl radicals. A series of studies demonstrated that the microbicidal activity of hydroxyl radicals was sufficient to kill bacteria in an experimental biofilm as well as planktonic bacteria and fungi within a short-treatment time. In addition, the safety aspect is confirmed by an in vivo study and a literature review. Thus, it is suggested that disinfection treatment utilizing artificially generated hydroxyl radicals can be applicable to medical/dental therapy as novel disinfection treatments.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Dental caries and periodontitis, two major dental diseases, are infectious diseases caused by pathogenic bacteria found in dental plaque [1, 2]. Thus, effective removal of the dental plaque (i.e. bacterial biofilm) and maintaining oral hygiene are the keys in prevention and treatment. In dental practice, mechanical removal of dental plaque from the lesion site is the primary treatment modality because the effect of chemical disinfection is rather weak against biofilm in which bacteria are protected from such chemicals by a matrix [3, 4]. However, it is sometimes difficult to mechanically remove the dental plaque properly at narrow or anatomically complex lesion sites in oral cavity. Thus, an adjunctive treatment with antiseptics as well as local and systemic antimicrobial chemotherapy is performed in some cases. However, these treatments possess a risk of adverse effect caused by e.g. leakage of chemical solution and induction of bacterial drug resistance [5, 6]. Therefore, it is expected to develop a novel disinfection treatment which can be used in combination with conventional mechanical treatment with minimum adverse effect.
Application of antibiotics and antiseptics to the treatment and the prevention of dental infectious diseases has been studied. For example, it has been reported that systemic administration of metronidazole and amoxicillin together with scaling and root planing (SRP) improves the periodontal condition than SRP alone [7, 8]. However, the systemic administration of antibiotics is limited to a treatment of severe periodontitis because of the risk of adverse effect. Local application of antibiotics known as local drug delivery system (LDDS) has also been studied to treat periodontitis. The antibiotics in the form of gel, such as doxycycline and minocycline, are delivered to periodontal pockets after SRP. However, since there is a contradiction in the clinical benefit of LDDS [9–13], the clinical application is also limited to specific cases.
Besides the antibiotics, antiseptics have also been studied for periodontal therapy. For instance, mouthrinse with chlorhexidine (CHX) is a most widely studied as an adjunctive treatment for periodontitis [14]. It has been reported that CHX can effectively prevent plaque accumulation [15]. However, repeated use of CHX results in the discoloration of the teeth as well as the tongue, and in the taste perturbation [16, 17]. Thus, mouthrinse with CHX is limited to the case where meticulous plaque control is required, such as plaque control during treatment of severe periodontitis or after periodontal surgery [18]. Accordingly, although CHX has been proven effective as a preventive agent, it has not been recommended as a therapeutic agent in periodontal therapy [14]. The other example of disinfectant used as a mouthrinse is hydrogen peroxide (H2O2) which is widely used as a disinfectant for skin wound at a concentration of ≤3 %. Based on the clinical studies, mouthrinse with H2O2 apparently prevents plaque accumulation [19–21] though its plaque prevention effect is weaker than that of CHX [22]. Thus, mouthrinse with H2O2 is rarely used in dental therapy.
Photodynamic therapy (PDT), a newly developed chemical disinfection treatment, has been applied to the treatment of periodontitis over the last decade [23]. The PDT consists of light, oxygen and a photosensitizer. Once the photosensitizer is irradiated with light of a specific wavelength, it absorbs photons and transfers the excitation energy to molecular oxygen which is in turn metamorphosed to its diamagnetic form, singlet oxygen [24]. Since singlet oxygen is unstable and has high reactivity, it oxidizes bacterial cell components resulting in cell death [23, 25]. The advantage of PDT is that it exerts bactericidal activity only when a photosensitizer is irradiated with light. Without irradiation, photosensitizer does not exert cytotoxic effect, indicating that residual toxicity after the treatment is negligible. Furthermore, it is suggested that the PDT does not induce bacterial resistance because singlet oxygen oxidize bacterial cell components non-selectively [26, 27]. This is a major advantage in comparison with antibiotics. Based on the bactericidal activity of PDT demonstrated by in vitro studies [28–31], the therapeutic effect of PDT following SRP has been studied expecting an additional effect. However, the clinical results are controversial between the studies [32–35]. Thus, clinical benefit of using PDT as an adjunctive treatment in periodontal therapy is still unclear.
To solve the problems of chemical disinfection treatment, novel disinfection treatment techniques in which artificially generated hydroxyl radicals kill bacteria have been developed in our laboratory. Our recent study demonstrated that hydroxyl radicals would not induce bacterial resistance as singlet oxygen does not [36]. In addition, hydroxyl radicals have higher oxidation power than singlet oxygen [25], resulting in higher antimicrobial activity. In this chapter, the generation systems of hydroxyl radicals and their microbicidal activity are discussed based on our recent works.
2 Application of Hydroxyl Radicals to Disinfection Treatment
The hydroxyl radical is one of the reactive oxygen species (ROS). Since the hydroxyl radical has one unpaired electron in the structure, it tends to deprive other substances of an electron which is so-called oxidation [37]. It is well-known that hydroxyl radicals are involved in various biochemical reactions, and hydroxyl radical-induced oxidative damage on cells and tissues leads to specific diseases if hydroxyl radicals are generated chronically [38, 39]. On the other hand, the cytotoxic effect of hydroxyl radicals is also used in a positive way. For instance, hydroxyl radicals are produced by immunological response to kill invading microorganisms [40, 41]. Besides the immune system, it has been demonstrated that ROS, especially hydroxyl radicals would play an important role in the mechanism of bacterial cell death induced by antibiotics via the reaction with primary target followed by Fenton like reaction [42, 43]. In this context, we have conducted research to develop novel disinfection techniques utilizing artificially generated hydroxyl radicals.
The key for the use of hydroxyl radicals as a disinfectant in vivo is to control the yield and the exposure time. Otherwise hydroxyl radicals will kill not only bacteria but also normal cells causing adverse reactions to the body. These factors are largely dependent on the generation systems of hydroxyl radicals. Hydroxyl radicals are generated basically by either one-electron reduction of H2O2 or homolytic fission of chemical bond [37]. Representative examples are summarized in Table 17.1.
To control the yield of hydroxly radicals, the reaction of hydroxyl radical generation system should be terminated appropriately when necessary. From this viewpoint, reaction involving homolytic fission is advantageous because the reaction can be terminated by cessation of irradiation of γ-ray, ultraviolet ligh or ultrasound. Since hydroxyl radicals have a very short lifetime (approximately 10−9 s) [44, 45, 25], residual toxicity would be negligible after the termination of reaction. On the other hand, it might be difficult to control the reaction of one-electron reduction of H2O2 during the disinfection treatment. The chemicals involved in the reaction of homolytic fission are basically safe because they are only H2O and H2O2. Indeed, a subcommittee of the US Food and Drug Administration concluded that H2O2 as a disinfectant is safe at concentrations of up to 3 % [46]. Although H2O2 is also one of ROS, it is expected that hydroxyl radicals can kill bacteria more effectively than H2O2 because hydroxyl radicals have much higher reactivity and oxidative power [47]. Considering the safety aspect of reaction energy, exposure of normal tissue to γ-ray should be avoided. Thus, radiolysis of H2O cannot be applied to disinfection treatment in vivo. The irradiation of ultraviolet light (UV), which is electromagnetic wave with a wavelength of <400 nm, to normal tissue would also cause adverse effect especially when UV light with a short wavelength known as UVB (280–315 nm) and UVC (100–280 nm) is used [48]. Besides UV light, we have found that visible blue light (wavelength: around 400 nm) can also photolyze H2O2 and it will probably be used without adverse effects as long as the treatment time is not so long. As for ultrasound irradiation, ultrasound device with a frequency of <5 MHz has been utilized in medical diagnostic imaging. Thus, the frequency of ultrasound itself is supposed to be safe. Therefore, we have been studying photolysis of H2O2 and sonolysis of H2O to develop new disinfection techniques to treat infectious diseases.
2.1 Photolysis of H2O2
In dental and medical fields, the bactericidal activity of 3 % H2O2 is well recognized and used as a disinfectant. However, the bactericidal effect is not sufficient to treat periodontal diseases as discussed above. To improve the bactericidal activity, we studied the effect of visible blue light irradiation of H2O2 (i.e. photolysis of H2O2). Ikai et al. used a laser with a wavelength of 405 nm at an irradiance of 940 mW/cm2 and demonstrated that the yield of hydroxyl radicals generated by photolysis of H2O2 increased with laser irradiation time [49]. The laser irradiation of bacterial suspensions in 1 M H2O2 (corresponds to approximately 3 % H2O2) resulted in a >4-log reduction of the viable counts of bacteria, such as Staphylococcus aureus, Aggregatibacter actinomycetemcomitans, Streptococcus mutans and Enterococcus faecalis, within 3 min of treatment [49]. Furthermore, treatment of S. mutans in an experimental biofilm also resulted in a >5-log reduction of viable counts within 3 min [49]. Concerning the periodontal pathogens other than A. actinomycetemcomitans, Ikai et al. also investigated the bactericidal effect of photolysis of H2O2 on Porphyromonas gingivalis. It was demonstrated that photolysis of 500 mM H2O2 killed P. gingivalis in an experimental biofilm with a >5-log reduction of viable counts within 30 s [50]. As for H2O2 solution, Oyamada et al. compared the bactericidal activity of photoysis of oxydol products (2.5–3.0 % H2O2 solution), which is an over-the-counter drug with quality guaranteed by Japanese Pharmacopoeia, to substitute them for H2O2 of reagent grade [51]. It was demonstrated that any of the oxydol products that have been already approved by an authority can be used for the disinfection technique in terms of bactericidal activity. Thus, based on these findings, we have been developing a therapeutic device for the treatment of periodontitis, and a clinical trial will be conducted in the near future. In the therapeutic device, H2O2 is released from the forefront of scaler tip of the device to the lesion site concomitantly with laser irradiation through an optical fiber during ultrasound scaling (Fig. 17.1).
Nakamura et al. conducted a kinetic analysis and demonstrated that hydroxyl radicals generated by photolysis of H2O2 directly reacted with microorganisms [52]. In addition, it was demonstrated that the catalase activity of microorganisms influenced the microbial resistance to oxidative stress induced by photolysis of H2O2. Nonetheless, Candida albicans, a catalase positive yeast-like fungus whose catalase activity is more potent than that of catalase positive bacteria such as S. aureus could also be killed with a >4-log reduction of viable counts within 10 min when treated with the photolysis of 250 mM H2O2 using LEDs at an irradiance of 80 mW/cm2. This finding suggests that photolysis of H2O2 can effectively kill not only bacteria but also fungi. Shirato et al. evaluated the effect of thermal energy on the yield of and the bactericidal action of hydroxyl radicals generated by photolysis of H2O2 [53]. The results demonstrated that thermal energy accelerated the generation of hydroxyl radicals by photolysis of H2O2, which in turn resulted in a synergistic bactericidal effect of hydroxyl radicals and thermal energy. When photolysis of H2O2 was performed at 55 °C, S. aureus and E. faecalis were killed with a >5-log reduction of viable counts within 1 min even though the irradiance of light was 110 mW/cm2 and the concentration of H2O2 was 500 mM. This synergistic effect will be beneficial especially when it comes to cleaning of medical instruments or dental prostheses which can tolerate the temperature of 55 °C. Based on these findings, Kanno et al. applied photolysis of H2O2 to cleaning of removable dentures and conducted a clinical test [54]. They demonstrated that microorganisms in denture plaque were reduced by approximately 7-log within 20 min. In addition to the in vitro tests, in vivo antibacterial effect of photolysis of H2O2 was proven effective. Hayashi et al. evaluated antibacterial activity of photolysis of H2O2 on skin infection [55]. Infection of S. aureus was established in the full-thickness skin wounds of immunosuppressed rats. Then, the wound was treated by photolysis of 1 M H2O2. Two minutes treatment resulted in significant reduction in viable counts in comparison with the treatment by H2O2 alone. Thus, the disinfection technique based on photolysis of H2O2 is expected to be applied to a wide range of fields other than treatment for periodontitis.
Besides the bactericidal activity, it was demonstrated that photolysis of H2O2 caused lag of regrowth of the surviving bacteria after the disinfection treatment, known as the postantiboitic effect (PAE). Odashima et al. demonstrated that photolysis of 250 mM H2O2 with a treatment time of 10 s significantly delayed the regrowth of S. aureus colony on agar plate [56]. The PAE would be beneficial because it contributes to giving time for host immune defense system to overcome the infection. More importantly, it has been demonstrated that repeated treatment by photolysis of H2O2 does not induce bacterial resistance to this disinfection technique. Ikai et al. evaluated the risk of inducing bacterial resistance to disinfection treatment with photolysis of H2O2 using S. aureus, E. faecalis, Escherichia coli, Streptococcus salivarius, Pseudomonas aeruginosa, S. mutans, and A. actinomycetemcomitans [36]. The antibacterial activity against any of the bacterial species tested was not affected by repeated exposure to the disinfection treatment up to 40 times suggesting that the repeated treatment does not induce bacterial resistance.
Regarding the safety aspect of the disinfection system, Yamada et al. conducted an animal study in which histological analyses of oral mucosa and the full-thickness skin wounds in rats treated by the disinfection technique with photolysis of 1 M H2O2 were performed [57]. Since topical treatment had no detrimental effect on the oral mucosa and the healing process of full thickness skin wounds, it is expected that the acute locally injurious property of the disinfection technique is low. Moreover, Kanno et al. assessed the risk of carcinogenicity by using the hydroxyl radical for the treatment of oral infections by reviewing the literatures [58]. The reviewed studies reported possible involvement of hydroxyl radicals in some sort of chemically-induced mutagenicity and carcinogenicity. However, manifestation of carcinogenicity requires chronic exposure to the carcinogens that generate hydroxyl radicals, such as heavy metals. Thus, it was concluded that there is little or no risk of carcinogenicity as long as the hydroxyl radical is used as a disinfectant for the short-term treatment of oral cavity. Therefore, the disinfection treatment with photolysis of H2O2 is expected to be a novel alternative to antiseptics and antibiotics.
2.2 Sonolysis of Water
The antimicrobial effect of ultrasound has been studied in various fields, such as water treatment, food decontamination and medical disinfection [59]. The mechanism of killing microorganisms is mainly due to cavitation effect in which tiny gas bubbles formed in liquid medium by alternating compression and expansion collide violently, creating shock waves in a localized region with high temperature (5,500 °C) and pressure (50 MPa) [60]. When water is used as a liquid medium, the shock wave produced by the cavitation effect fragments the molecules of H2O into hydroxyl radicals and hydrogen atoms, which is so-called sonolysis of water [61]. Then, the localized heating and pressure together with the free radicals damage microorganisms resulting in cell death [60].
In this context, we examined fungicidal effect of ultrasound irradiation at a frequency of 1.6 MHz [62] to develop a treatment of onychomycosis (i.e. fungal nail infections). It was demonstrated that the ultrasound irradiation killed the dermatophytes, such as Trichophyton mentagrophytes and Trichophyton rubrum, with a yield of hydroxyl radicals that is proportion to ultrasound duration. In particular, when the treatment was performed at 50 °C, the fungi were killed with a 5-log of viable counts within 10 min. Thus, it is suggested that the ultrasound irradiation and heat treatment exerted a combination effect in fungicidal activity. This finding was in accordance with previous studies which evaluated the combination effect of heat and ultrasound on bactericidal activity [63, 64].
As for application of sonolysis of water to dentistry, other research groups have conducted studies. For instance, it has been demonstrated that ultrasound irradiation of 1.5 % (450 mM) H2O2 using a device for endodontic treatment generates hydroxyl radicals resulting in killing of E. faecalis [65]. However, the reduction of bacterial number within the treatment time of 90 s was less than 1-log. Thus, the clinical benefit of this treatment is still unclear. The other example is the ultrasonic scaler used for periodontal therapy. It has been reported that hydroxyl radicals are generated during scaling around ultrasonic scaler tip [66–68]. However, the role of hydroxyl radicals generated by ultrasonic scaler is still unknown.
The microbicidal activity of ultrasound irradiation varies dependently on the type of microorganisms treated (i.e. Gram-positive or negative bacteria, spore forming bacteria, and fungi). In addition, it has been reported that the microbicidal activity of ultrasound irradiation alone is relatively low (<1-log) and/or requires extended irradiation time (~60 min) unless it is used at high intensity [69]. Therefore, as suggested by Piyasena et al. [60], it would be beneficial to use ultrasound in conjunction with other disinfection techniques, such as heat treatment, antiseptics and antibiotics.
2.3 Other Hydroxyl Radical Generation Systems
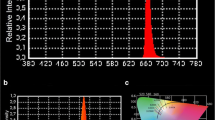
More recently, we found that photo-irradiated polyphenolic compounds could generate hydroxyl radicals as well as H2O2. Since it has been reported that polyphenolic compounds exert antimicrobial effect via production of H2O2 by auto-oxidation in a liquid medium [70, 71], we tried to enhance the antimicrobial activity by means of exposure of polyphenolic compounds to blue light, which enhances the H2O2 production through photo-oxidation of the compounds resulting in hydroxyl radical production via photolysis of the resultant H2O2 (Fig. 17.2). Nakamura et al. demonstrated that hydroxyl radicals were generated when gallic acid, a polyphenolic compound, was irradiated with blue light (wavelength: 400 nm) at an irradiance of 80 mW/cm2 [72]. It was also demonstrated that S. aureus was killed by the photo-irradiation of gallic acid with a >5-log reduction of viable counts within 15 min. Since the bactericidal activity was attenuated by adding hydroxyl radical scavengers, such as dimethyl sulfoxide and sodium formate, it is suggested that the hydroxyl radical is the main contributor to the bactericidal effect. Later, they showed similar bactericidal activity of photo-irradiated proanthocyanidin which is also a type of polyphenolic compounds [73]. The advantage of this disinfection technique is that polyphenols are supposed to be safe for humans because they are edible compounds naturally occurring in fruits, vegetables, nuts, seeds, and flowers. In addition, since those polyphenolic compounds are noteworthy for its antioxidative activity [74, 75], they might alleviate the oxidative damage in the tissue after the disinfection treatment. Therefore, it is expected that this disinfection technique is applicable to the fields of medical and food sanitation.
Based on the findings described above, we studied the combination effect of photolysis of H2O2 and photo-irradiation of proanthocyanidin. Since both disinfection techniques utilize the same light source (wavelength: around 400 nm), they can be performed at once if the liquid contains H2O2 and proanthocyanidin. Ikai et al. demonstrated that combination of H2O2 and proanthocyanidin worked synergistically to kill S. mutans when photo-irradiated [76]. This synergistic effect would probably contribute to shortening the treatment time and/or to reducing the concentration of H2O2 for more safety.
3 Summary
In the present review, we described our recent works on microbicidal effect of the artificially generated hydroxyl radicals. As discussed above, the microbicidal activity of hydroxyl radicals is sufficient to kill bacteria in an experimental biofilm as well as planktonic bacteria and fungi within a short-treatment time. At the same time, the safety aspect is also confirmed by an in vivo study and a literature review. Therefore, they can be applicable as novel disinfection treatments in medical/dental therapy. Further studies are in progress to understand the bactericidal mechanism of each disinfection system and also of a combination of each system for the more sophisticated medical devices.
References
Marsh PD, Nyvad B. The oral microflora and biofilms on teeth. In: Fejerskov O, Kidd E, editors. Dental caries. The disease and its clinical management. Oxford: Blackwell Munksgaard; 2003. p. 49–70.
Socransky SS, Haffajee AD. Microbiology of periodontal disease. In: Lindhe J, Karring T, Lang NP, editors. Clinical periodontology and implant dentistry. 4th ed. Oxford: Blackwell; 2003. p. 106–49.
Costerton JW, Lewandowski Z, Caldwell DE, Korber DR, Lappin-Scott HM. Microbial biofilms. Annu Rev Microbiol. 1995;49:711–45. doi:10.1146/annurev.mi.49.100195.003431.
Cargill KL, Pyle BH, Sauer RL, McFeters GA. Effects of culture conditions and biofilm formation on the iodine susceptibility of Legionella pneumophila. Can J Microbiol. 1992;38(5):423–9. doi:10.1139/m92-071.
Russell AD. Antibiotic and biocide resistance in bacteria: introduction. J Appl Microbiol. 2002;92(Suppl):1S–3. doi:10.1046/j.1365-2672.92.5s1.14.x.
Tenover FC. Mechanisms of antimicrobial resistance in bacteria. Am J Med. 2006;119:S3–S10. doi:10.1016/j.amjmed.2006.03.011.
Winkel EG, Van Winkelhoff AJ, Timmerman MF, Van der Velden U, Van der Weijden GA. Amoxicillin plus metronidazole in the treatment of adult periodontitis patients. A double-blind placebo-controlled study. J Clin Periodontol. 2001;28:296–305. doi:10.1034/j.1600-051x.2001.028004296.x.
Berglundh T, Krok L, Liljenberg B, Westfelt E, Serino G, Lindhe J. The use of metronidazole and amoxicillin in the treatment of advanced periodontal disease. A prospective, controlled clinical trial. J Clin Periodontol. 1998;25:354–62.
Tomasi C, Wennstrom JL. Locally delivered doxycycline as an adjunct to mechanical debridement at retreatment of periodontal pockets: outcome at furcation sites. J Periodontol. 2011;82:210–8. doi:10.1902/jop.2010.100308.
Tomasi C, Koutouzis T, Wennstrom JL. Locally delivered doxycycline as an adjunct to mechanical debridement at retreatment of periodontal pockets. J Periodontol. 2008;79:431–9. doi:10.1902/jop.2008.070383.
Wennstrom JL, Newman HN, MacNeill SR, Killoy WJ, Griffiths GS, Gillam DG, et al. Utilisation of locally delivered doxycycline in non-surgical treatment of chronic periodontitis. A comparative multi-centre trial of 2 treatment approaches. J Clin Periodontol. 2001;28:753–61.
Novak MJ, Dawson 3rd DR, Magnusson I, Karpinia K, Polson A, Ryan ME, et al. Combining host modulation and topical antimicrobial therapy in the management of moderate to severe periodontitis: a randomized multicenter trial. J Periodontol. 2008;79:33–41. doi:10.1902/jop.2008.070237.
Tonetti MS, Cortellini P, Carnevale G, Cattabriga M, de Sanctis M, Pini Prato GP. A controlled multicenter study of adjunctive use of tetracycline periodontal fibers in mandibular class II furcations with persistent bleeding. J Clin Periodontol. 1998;25:728–36. doi:10.1111/j.1600-051X.1998.tb02514.x.
Addy M. The use of antiseptics in periodontal therapy. In: Lindhe J, Karring T, Lang NP, editors. Clinical periodontology and implant dentistry. Oxford: Blackwell; 2003.
Loe H, Schiott CR. The effect of mouthrinses and topical application of chlorhexidine on the development of dental plaque and gingivitis in man. J Periodontal Res. 1970;5:79–83. doi:10.1111/j.1600-0765.1970.tb00696.x.
Watts A, Addy M. Tooth discolouration and staining: a review of the literature. Br Dent J. 2001;190:309–16. doi:10.1038/sj.bdj.4800959a.
Lang NP, Catalanotto FA, Knopfli RU, Antczak AA. Quality-specific taste impairment following the application of chlorhexidine digluconate mouthrinses. J Clin Periodontol. 1988;15:43–8. doi:10.1111/j.1600-051X.1988.tb01553.x.
Addy M, Moran JM. Clinical indications for the use of chemical adjuncts to plaque control: chlorhexidine formulations. Periodontol 2000. 1997;15:52–4. doi:10.1111/j.1600-0757.1997.tb00104.x.
Wennstrom J, Lindhe J. Effect of hydrogen peroxide on developing plaque and gingivitis in man. J Clin Periodontol. 1979;6:115–30.
Boyd RL. Effects on gingivitis of daily rinsing with 1.5% H2O2. J Clin Periodontol. 1989;16:557–62.
Hasturk H, Nunn M, Warbington M, Van Dyke TE. Efficacy of a fluoridated hydrogen peroxide-based mouthrinse for the treatment of gingivitis: a randomized clinical trial. J Periodontol. 2004;75:57–65. doi:10.1902/jop.2004.75.1.57.
Gusberti FA, Sampathkumar P, Siegrist BE, Lang NP. Microbiological and clinical effects of chlorhexidine digluconate and hydrogen peroxide mouthrinses on developing plaque and gingivitis. J Clin Periodontol. 1988;15:60–7. doi:10.1111/j.1600-051X.1988.tb01556.x.
Konopka K, Goslinski T. Photodynamic therapy in dentistry. J Dent Res. 2007;86:694–707. doi:10.1177/154405910708600803.
Soukos NS, Goodson JM. Photodynamic therapy in the control of oral biofilms. Periodontol 2000. 2011;55:143–66. doi:10.1111/j.1600-0757.2010.00346.x.
Redmond RW, Kochevar IE. Spatially resolved cellular responses to singlet oxygen. Photochem Photobiol. 2006;82:1178–86. doi:10.1562/2006-04-14-IR-874.
Pedigo L, Gibbs A, Scott R, Street C. Absence of bacterial resistance following repeat exposure to photodynamic therapy. Proc SPIE. 2009;7380:73803H1–7. doi:10.1117/12.822834.
Tavares A, Carvalho CM, Faustino MA, Neves MG, Tome JP, Tome AC, et al. Antimicrobial photodynamic therapy: study of bacterial recovery viability and potential development of resistance after treatment. Mar Drugs. 2010;8:91–105. doi:10.3390/md8010091.
Burns T, Wilson M, Pearson G. Mechanism of killing of Streptococcus mutans by light-activated drugs. Proc SPIE. 1996;2625:288–97.
Wood S, Nattress B, Kirkham J, Shore R, Brookes S, Griffiths J, et al. An in vitro study of the use of photodynamic therapy for the treatment of natural oral plaque biofilms formed in vivo. J Photochem Photobiol B. 1999;50:1–7. doi:10.1016/S1011-1344(99)00056-1.
Zanin IC, Lobo MM, Rodrigues LK, Pimenta LA, Hofling JF, Goncalves RB. Photosensitization of in vitro biofilms by toluidine blue O combined with a light-emitting diode. Eur J Oral Sci. 2006;114:64–9. doi:10.1111/j.1600-0722.2006.00263.x.
Ishiyama K, Nakamura K, Ikai H, Kanno T, Kohno M, Sasaki K, et al. Bactericidal action of photogenerated singlet oxygen from photosensitizers used in plaque disclosing agents. PLoS One. 2012;7:e37871. doi:10.1371/journal.pone.0037871.g001.
Bassir SH, Moslemi N, Jamali R, Mashmouly S, Fekrazad R, Chiniforush N, et al. Photoactivated disinfection using light-emitting diode as an adjunct in the management of chronic periodontitis: a pilot double-blind split-mouth randomized clinical trial. J Clin Periodontol. 2013;40:65–72. doi:10.1111/jcpe.12024.
Pourabbas R, Kashefimehr A, Rahmanpour N, Babaloo Z, Kishen A, Tenenbaum HC, et al. Effects of photodynamic therapy on the clinical and gingival crevicular fluid inflammatory biomarkers in chronic periodontitis: a split-mouth randomized clinical trial. J Periodontol. 2014. doi:10.1902/jop.2014.130464.
Alwaeli HA, Al-Khateeb SN, Al-Sadi A. Long-term clinical effect of adjunctive antimicrobial photodynamic therapy in periodontal treatment: a randomized clinical trial. Lasers Med Sci. 2013. doi:10.1007/s10103-013-1426-y.
Theodoro LH, Silva SP, Pires JR, Soares GH, Pontes AE, Zuza EP, et al. Clinical and microbiological effects of photodynamic therapy associated with nonsurgical periodontal treatment. A 6-month follow-up. Lasers Med Sci. 2012;27:687–93.
Ikai H, Odashima Y, Kanno T, Nakamura K, Shirato M, Sasaki K, et al. In vitro evaluation of the risk of inducing bacterial resistance to disinfection treatment with photolysis of hydrogen peroxide. PLoS One. 2013;8:e81316. doi:10.1371/journal.pone.0081316.
Halliwell B, Gutteridge JM. The chemistry of free radicals and related ralactive species. Free radicals in biology and medicine. 4th ed. Oxford: Oxford University Press; 2007. p. 30–78.
Clark IA, Cowden WB, Hunt NH. Free radical-induced pathology. Med Res Rev. 1985;5:297–332.
Cross CE, Halliwell B, Borish ET, Pryor WA, Ames BN, Saul RL, et al. Oxygen radicals and human disease. Ann Intern Med. 1987;107:526–45.
Badwey JA, Karnovsky ML. Active oxygen species and the functions of phagocytic leukocytes. Annu Rev Biochem. 1980;49:695–726. doi:10.1146/annurev.bi.49.070180.003403.
Clifford DP, Repine JE. Hydrogen peroxide mediated killing of bacteria. Mol Cell Biochem. 1982;49:143–9.
Kohanski MA, Dwyer DJ, Hayete B, Lawrence CA, Collins JJ. A common mechanism of cellular death induced by bactericidal antibiotics. Cell. 2007;130:797–810. doi:10.1016/j.cell.2007.06.049.
Wright GD. On the road to bacterial cell death. Cell. 2007;130:781–3. doi:10.1016/j.cell.2007.08.023.
Pryor WA. Oxy-radicals and related species: their formation, lifetimes, and reactions. Annu Rev Physiol. 1986;48:657–67. doi:10.1146/annurev.ph.48.030186.003301.
Sies H, Stahl W, Sundquist A. Antioxidant functions of vitamins. Vitamins E and C, beta-caroten, and other carotenoids. Ann N Y Acad Sci. 1992;669:7–20.
FDA. Oral health care drug products for over-the-counter human use; Antigingivitis/antiplaque drug products; Establishment of a monograph. Fed Regist. 2003;68:32232–86.
Augusto O, Miyamoto S. Chapter 2. Oxygen radicals and related species. In: Pantopoulos K, Schipper H, editors. Principles of free radical biomedicine, vol. 1. New York: Nova; 2012. p. 19–41.
Maverakis E, Miyamura Y, Bowen MP, Correa G, Ono Y, Goodarzi H. Light, including ultraviolet. J Autoimmun. 2010;34:J247–57. doi:10.1016/j.jaut.2009.11.011.
Ikai H, Nakamura K, Shirato M, Kanno T, Iwasawa A, Sasaki K, et al. Photolysis of hydrogen peroxide, an effective disinfection system via hydroxyl radical formation. Antimicrob Agents Chemother. 2010;54:5086–91. doi:10.1128/AAC.00751-10.
Ikai H, Nakamura K, Shirato M, Kanno T, Iwasawa A, Niwano Y, et al. Bactericidal effect of hydroxyl radical generated by photolysis of hydrogen peroxide. In: Sasaki K, Suzuki O, Takahashi N, editors. Interface Oral Health Science 2011. Tokyo: Springer; 2012.
Oyamada A, Ikai H, Nakamura K, Hayashi E, Kanno T, Sasaki K, et al. In vitro bactericidal activity of photo-irradiated oxydol products via hydroxyl radical generation. Biocontrol Sci. 2013;18:83–8. doi:10.4265/bio.18.83.
Nakamura K, Kanno T, Mokudai T, Iwasawa A, Niwano Y, Kohno M. Microbial resistance in relation to catalase activity to oxidative stress induced by photolysis of hydrogen peroxide. Microbiol Immunol. 2012;56:48–55. doi:10.1111/j.1348-0421.2011.00400.x.
Shirato M, Ikai H, Nakamura K, Hayashi E, Kanno T, Sasaki K, et al. Synergistic effect of thermal energy on bactericidal action of photolysis of H2O2 in relation to acceleration of hydroxyl radical generation. Antimicrob Agents Chemother. 2012;56:295–301. doi:10.1128/AAC.05158-11.
Kanno T, Nakamura K, Ikai H, Hayashi E, Shirato M, Mokudai T, et al. Novel denture cleaning system based on hydroxyl radical disinfection. Int J Prosthodont. 2012;25:376–80.
Hayashi E, Mokudai T, Yamada Y, Nakamura K, Kanno T, Sasaki K, et al. In vitro and in vivo anti-Staphylococcus aureus activities of a new disinfection system utilizing photolysis of hydrogen peroxide. J Biosci Bioeng. 2012;114:193–7. doi:10.1016/j.jbiosc.2012.03.020.
Odashima Y, Nakamura K, Ikai H, Kanno T, Meirelles L, Sasaki K, et al. Postantibiotic effect of disinfection treatment by photolysis of hydrogen peroxide. J Chemother. 2014;26:92–100. doi:10.1179/1973947813Y.0000000114.
Yamada Y, Mokudai T, Nakamura K, Hayashi E, Kawana Y, Kanno T, et al. Topical treatment of oral cavity and wounded skin with a new disinfection system utilizing photolysis of hydrogen peroxide in rats. J Toxicol Sci. 2012;37:329–35. doi:10.2131/jts.37.329.
Kanno T, Nakamura K, Ikai H, Kikuchi K, Sasaki K, Niwano Y. Literature review of the role of hydroxyl radical in chemically-induced mutagenicity and carcinogenicity for the risk assessment of disinfection system utilizing photolysis of hydrogen peroxide. J Clin Biochem Nutr. 2012;51:9–14. doi:10.3164/jcbn.11-105.
Erriu M, Blus C, Szmukler-Moncler S, Buogo S, Levi R, Barbato G, et al. Microbial biofilm modulation by ultrasound: current concepts and controversies. Ultrason Sonochem. 2014;21:15–22. doi:10.1016/j.ultsonch.2013.05.011.
Piyasena P, Mohareb E, McKellar RC. Inactivation of microbes using ultrasound: a review. Int J Food Microbiol. 2003;87:207–16. doi:10.1016/S0168-1605(03)00075-8.
Riesz P, Kondo T. Free radical formation induced by ultrasound and its biological implications. Free Radic Biol Med. 1992;13:247–70. doi:10.1016/0891-5849(92)90021-8.
Iwasawa A, Saito K, Mokudai T, Kohno M, Ozawa T, Niwano Y. Fungicidal action of hydroxyl radicals generated by ultrasound in water. J Clin Biochem Nutr. 2009;45:214–8. doi:10.3164/jcbn.08-261.
Ordonez JA, Sanz B, Hernandez PE, Lopez-Lorenzo P. A note on the effect of combined ultrasonic and heat treatments on the survival of thermoduric streptococci. J Appl Bacteriol. 1984;56:175–7. doi:10.1111/j.1365-2672.1984.tb04711.x.
McClements DJ. Advances in the application of ultrasound in food analysis and processing. Trends Food Sci Technol. 1995;6:293–9. doi:10.1016/S0924-2244(00)89139-6.
Kobayashi Y, Hayashi M, Yoshino F, Tamura M, Yoshida A, Ibi H, et al. Passive ultrasonic irrigation in the presence of a low concentration of hydrogen peroxide enhances hydroxyl radical generation and bactericidal effect against Enterococcus faecalis. J Oral Sci. 2014;56:35–9. doi:10.2334/josnusd.56.35.
Felver B, King DC, Lea SC, Price GJ, Damien WA. Cavitation occurrence around ultrasonic dental scalers. Ultrason Sonochem. 2009;16:692–7. doi:10.1016/j.ultsonch.2008.11.002.
Walmsley AD, Lea SC, Felver B, King DC, Price GJ. Mapping cavitation activity around dental ultrasonic tips. Clin Oral Investig. 2013;17:1227–34. doi:10.1007/s00784-012-0802-5.
Price GJ, Tiong TJ, King DC. Sonochemical characterisation of ultrasonic dental descalers. Ultrason Sonochem. 2014. doi:10.1016/j.ultsonch.2013.12.029.
Iqbal K, Ohl SW, Khoo BC, Neo J, Fawzy AS. Effect of high-intensity focused ultrasound on Enterococcus faecalis planktonic suspensions and biofilms. Ultrasound Med Biol. 2013;39:825–33. doi:10.1016/j.ultrasmedbio.2012.12.006.
Arakawa H, Maeda M, Okubo S, Shimamura T. Role of hydrogen peroxide in bactericidal action of catechin. Biol Pharm Bull. 2004;27:277–81. doi:10.1248/bpb.27.277.
Taguri T, Tanaka T, Kouno I. Antibacterial spectrum of plant polyphenols and extracts depending upon hydroxyphenyl structure. Biol Pharm Bull. 2006;29:2226–35. doi:10.1248/bpb.29.2226.
Nakamura K, Yamada Y, Ikai H, Kanno T, Sasaki K, Niwano Y. Bactericidal action of photo-irradiated gallic acid via reactive oxygen species formation. J Agric Food Chem. 2012;60:10048–54. doi:10.1021/jf303177p.
Nakamura K, Shirato M, Ikai H, Kanno T, Sasaki K, Kohno M, et al. Photo-irradiation of proanthocyanidin as a new disinfection technique via reactive oxygen species formation. PLoS One. 2013;8:e60053. doi:10.1371/journal.pone.0060053.
Kondo K, Kurihara M, Miyata N, Suzuki T, Toyoda M. Scavenging mechanisms of (−)-epigallocatechin gallate and (−)-epicatechin gallate on peroxyl radicals and formation of superoxide during the inhibitory action. Free Radic Biol Med. 1999;27:855–63. doi:10.1016/S0891-5849(99)00133-1.
Yilmaz Y, Toledo RT. Major flavonoids in grape seeds and skins: antioxidant capacity of catechin, epicatechin, and gallic acid. J Agric Food Chem. 2004;52:255–60. doi:10.1021/jf030117h.
Ikai H, Nakamura K, Kanno T, Shirato M, Meirelles L, Sasaki K, et al. Synergistic effect of proanthocyanidin on the bactericidal action of the photolysis of H2O2. Biocontrol Sci. 2013;18:137–41. doi:10.4265/bio.18.137.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is distributed under the terms of the Creative Commons Attribution Noncommercial License, which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Copyright information
© 2015 The Author(s)
About this paper
Cite this paper
Sheng, H., Nakamura, K., Kanno, T., Sasaki, K., Niwano, Y. (2015). Microbicidal Activity of Artificially Generated Hydroxyl Radicals. In: Sasaki, K., Suzuki, O., Takahashi, N. (eds) Interface Oral Health Science 2014. Springer, Tokyo. https://doi.org/10.1007/978-4-431-55192-8_17
Download citation
DOI: https://doi.org/10.1007/978-4-431-55192-8_17
Published:
Publisher Name: Springer, Tokyo
Print ISBN: 978-4-431-55125-6
Online ISBN: 978-4-431-55192-8
eBook Packages: MedicineMedicine (R0)