Abstract
The aesthetic and functional implications of an appropriate dorsal contour are immense and contribute significantly to the overall rhinoplasty results. The authors discuss anatomy of the upper, middle, and lower thirds of the nose, goals for augmentation, materials used for dorsal augmentation, evaluation of the patient, harvesting the grafts, determining the needs of the dorsum with contour deformity, contour deformity with middle nasal vault collapse, contour deformities with significant loss of structural support, and defects encompassing the bony dorsum. Augmentation and reconstruction of the nasal dorsum is a challenging component of rhinoplasty. The role of the middle nasal vault in function and aesthetics is vital, and maintenance of the support mechanisms is paramount to the ideal dorsal profile. The interplay between the nasal pyramid, cartilaginous septum and upper lateral cartilages, and lower third of the nose must be taken into consideration during reconstruction.
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The aesthetic and functional implications of an appropriate dorsal contour are immense and contribute significantly to the overall rhinoplasty results. Spanning from the nasion to the tip, the dorsal contour and its integrity play a key role in profile, function, and tip projection. This chapter will focus on the principles and techniques commonly utilized for dorsal nasal augmentation.
2 Anatomy
Prior to any discussion of dorsal augmentation, one must gain a firm knowledge of the anatomy of the nose, the various bony and cartilaginous relationships, and their collective roles in attaining both an aesthetically pleasing and functional form. Failure to reconstitute or reinforce the support mechanisms of the nasal dorsum during rhinoplasty can lead to disastrous outcomes – some of which may not manifest until years later. Moreover, failing to adequately refine the dorsal profile will surely lead to an unhappy patient and higher rates of revision rhinoplasty.
2.1 The Upper Third of the Nose
The junction of the nasal and frontal bones defines the upper third of the nose at its most cephalic portion. On profile, this contributes to the depth of the radix and inferiorly the rhinion as the nasal bone transitions to the cartilaginous portion of the nasal dorsum. When observing the nose from an anterior view, a soft concave line from the medial brow extending to the nasal tip is initiated by the contour of the nasal bones [1]. The degree of contribution from the nasal bones to the dorsal profile is dependent on the length of the nasal bones. Short nasal bones will typically have less of a significant effect on dorsal profile and function than a nose with longer nasal bones. The keystone area, defined as the articulations between the upper lateral cartilages-septal complex and caudal nasal bones, is paramount for the overall integrity of the nasal dorsum. These connections are reinforced via fibrous mucoperiosteal and mucoperichondrial attachments. Anatomic studies have shown that this point of articulation should be preserved or reconstituted during any type of nasal surgery [2].
2.2 The Middle Third of the Nose
The foundation of the middle third of the nose rests on the strength of the cartilaginous nasal septum. Articulating with the bony septum cephalically, the septum serves to maintain the overall dorsal profile and position of the upper lateral cartilages (ULCs) – thereby serving as a support beam for the middle nasal vault [3]. The ULCs ride underneath the nasal bones cephalad and articulate with the septum medially to contribute the internal nasal valve, an area bound by the septum, ULCs, and the anterior head of the inferior turbinate. The internal nasal valve functionally provides the majority of resistance to nasal airflow, contributing up to 50% of the total resistance [4]. Minor contributions to the middle nasal vault and internal nasal valve are made by the fibrous attachments of the mucoperichondrial tissue internally and the soft tissue envelope externally.
2.3 The Lower Third of the Nose
The most caudal aspect of the septum lends support to the nasal tip and contributes to its projection. While Tardy et al. [5] have described many factors that develop and support the nasal tip, one cannot omit the septum’s integral role in maintaining nasal projection. This is best exemplified by the saddle nose deformity where the loss of dorsal cartilaginous support allows the roof of the middle vault to collapse leading to de-projection and over-rotation of the nasal tip. Furthermore, determining the appropriate height of the cartilaginous dorsum plays a key role in defining an aesthetically pleasing tip projection point.
3 Goals for Augmentation
The shape of the nasal dorsum should be tailored appropriately for gender and ethnicity. Ideally, the nasofrontal angle should be between 115° and 130°, keeping in mind that the extent of glabellar projection and initial height of the nasal dorsum can significantly impact this measurement. Other adjunctive maneuvers, such as a radix grafts, may be necessary to bring this angle into its ideal range. In females, a straight dorsal line that transitions into a subtle, refined supratip break compliments the delicacy of the nose. For the male patient, a straight to slightly convex nasal dorsum confers a stronger, more masculine look. In ethnic patients with platyrrhine noses, one should avoid the temptation to heighten the dorsum excessively – as this tends to elevate the tip and give the nose a more leptorrhine appearance. The length of the dorsum is typically used to help set the position of the nasal tip. If more projection or counter-rotation is desired, lengthening the nose can be accomplished by way of extended spreader grafts [3]. Conversely, resection of the most caudal aspect of the septum can shorten the nose and result in rotation of the tip.
4 Materials Used for Dorsal Nasal Augmentation
4.1 Alloplastic Materials
As early as the nineteenth century, alloplastic materials were utilized to contour the nasal dorsum [6]. Some surgeons initially turned to rigid plastics, relying on the graft’s non-immunogenic properties, as these were well tolerated in the body [7]. Their major drawback lay within the fact that once infected, they tended to extrude. Silicone implants remain in wide use for dorsal augmentation, especially in Asia. A fibrous capsule surrounds these smooth implants, which do not integrate with the adjacent tissue and are therefore prone to shifting and buckling [8]. Proponents of these implants refer to their ease of use and, if necessary, ease of removal. Tham et al. [9] retrospectively analyzed 355 patients in which silicone implants were utilized for nasal augmentation and concluded that silicone was effective, economical, and safe for surgical correction of the Asian nose with its thicker soft tissue envelope. Unfortunately, follow-up averaged just over 4 months, and removal or replacement of the implant was necessary in 7.8% of patients. Longer-term studies have also reported higher extrusion and infection rates [10, 11].
Medpor (Porex Surgical, Newnan, USA) is a porous high-density polyethylene material which allows the ingrowth of connective tissue and more complete integration of the implant into the soft tissue [8]. A stable, firm surface must be present to permit incorporation, and initial sterile handling of the implant is critical in lowering long-term infection risks [12]. However, the possibility of infection and subsequent extrusion makes this option less ideal, and the authors discourage its use in favor of autologous materials. The tissue ingrowth also makes this material extremely hard to remove (Fig. 34.1).
4.2 Homografts
Homografts are harvested from cadaveric sources. Prior to harvesting, donors are screened for systemic diseases and local infectious processes. They are then stored in solution and subjected to gamma irradiation at 30,000–40,000 Gy in order to sterilize and reduce the antigenicity of the graft. Homografts display good tissue compatibility and low rate of infection [13]. Other benefits include availability of large volumes of cartilage and avoidance of donor-site morbidity. Gunter et al. found no difference in the rate of warping of irradiated cadaveric cartilage and fresh cadaveric cartilage in vitro over a 4-week period [14]. In both groups, those grafts carved from the periphery of the cartilage tended to warp at a higher rate than those from more central portions of the rib.
The degree of homograft resorption when used in facial reconstructive surgery remains controversial [15]. Early studies demonstrated that the rate of resorption was highly dependent on the implanted region [16]. Kridel and Konior [13] published a series of 122 procedures using the irradiated costal cartilage for nasal augmentation. Over the average follow-up of 15 months, four (3.3%) of the homografts showed significant resorption. In two of these four cases, resorption was attributed to infection from the use of braided sutures. This resorption rate was much lower than that of previously reported studies which failed to specifically address nasal reconstruction [15, 16]. A larger follow-up study was later published by the same group, totaling 357 patients. Although they advocate irradiated cartilage is well-tolerated and had a decreased number of complications from their prior study, over 40% of the subjects were followed for 1 year or less and almost 15% required revision surgery [17].
Non-cartilaginous, processed homografts are also available. Acellular dermis (AlloDerm®, LifeCell Corporation, Branchburg, NJ) utilizes human donor skin dermal tissue matrix, which can be placed over a stable existing structural framework to augment the nasal dorsum. Although the biocompatibility of the graft is suitable, long-term results have shown high resorption rates and the need for overcorrection when the graft is used for augmentation [18]. The lack of rigidity of the material limits its use as a camouflage onlay graft.
4.3 Autografts
Autografts utilize the patient’s own tissue and are the gold standard for rhinoplasty and nasal reconstruction. They offer complete tissue immunogenicity and the lowest rates of resorption and extrusion [19]. Donor sites for grafts include septal, auricular (concha), and rib cartilage, as well as calvarial and iliac bones. Because of its structural rigidity and ease of harvest [20], septal cartilage is frequently preferred for reconstruction [21]. However, this often cannot be utilized in cases of revision rhinoplasty, when significant dorsal augmentation requires large grafts or in cases where prior trauma or surgery has compromised the amount of available cartilage. The ear and rib have been used extensively as secondary sources of cartilage [5, 20]. Conchal cartilage can be obtained without postsurgical deformity if one maintains the antihelical integrity; however, it lacks structural rigidity. In observance of this fact, the authors prefer to retain the use of auricular cartilage for cases that do not require extensive structural support.
Given the frequent lack of sufficient septal cartilage in rhinoplasty and the absence of rigidity of conchal cartilage, costal cartilage grafts provide an ample, readily available, and reliable source of cartilage for nasal dorsal augmentation. Rib is utilized for grafting material as a cartilaginous or as an osseocartilaginous graft.
The most common concern when using rib as a cartilaginous graft is its tendency to warp. This phenomenon has been noted since the early 1900s when Gilles noted the propensity for cartilage to warp toward the side where the perichondrium was left intact. This initially led to the belief that it was the perichondrial layer that induced warping of the cartilage [22]. This theory was disproven decades later when Gibson and Davis [23] reported that costal cartilage appears to be in a state of constant counterbalanced tension. They hypothesized that imprecise carving of the grafts could lead to an imbalance of these forces, which results in eventual disfigurement. Gibson and Davis have proposed four main configurations for sculpting the graft that balance the forces of tension and resist warping.
Despite Gibson’s initial reports of cross-balanced carving, he later states that the most critical factor in reducing warping is to minimize the amount of shaping required, which is still advocated today [24]. Gunter et al. [24, 25] report overcoming this by fixation of costal cartilage grafts using internal K-wires, using a 0.035-in. K-wire placed down the central aspect of the graft as a technique to resist warping. Studies have shown that the majority of cartilage warping takes place within 15–30 min after immersion in saline [23, 26], although some warping can continue for up to 4 weeks postoperatively [27].
The authors recommend immersing costal grafts in saline for at least 20 min prior to its use in order to allow any warping of the cartilage to take place before sculpting occurs. Moreover, the authors agree that concentrically carved cartilage grafts warp far less than eccentrically carved pieces [28, 29].
Osseocartilaginous costal grafts are an alternative to cartilaginous grafts for the nasal dorsum. Early reports of significant bony reabsorption lead to a tendency to avoid its use for nasal reconstruction [30, 31]. However, the nose has been shown to have low rates of resorption of bony grafts, such as calvarial and costal grafts when used for dorsal augmentation [32, 33]. Although the use of osseocartilaginous costal grafts avoids the potential for warping, the incision tends to be less concealed due to the more inferolateral position of the 10th and 11th ribs. This typically is an issue in females, where an inframammary incision provides the perfect concealment under a bra wire or bikini top.
5 Evaluation of the Patient
The overall evaluation of the rhinoplasty patient is a complex process and beyond the scope of this chapter. However, there are a few key points that require addressing when attempting to correct the nasal dorsum. A complete history of the patient should always be elicited to help identify the potential causes of deformities of the nose and the patient’s motivation for corrective surgery.
A variety of pathological conditions can lead to a dorsal deformity requiring augmentation, but trauma and prior surgical procedures account for the majority of causes in the reported literature [34–36]. Nasal trauma may result in mechanical disruption of the septum or in hematoma formation leading to necrosis of the cartilaginous septum and loss of support [37]. Surgical disruption of septal attachments to the nasal floor, bony septum, and nasal bones as well as injudicious resection of the septal cartilage may result in a loss of support of the nasal dorsum. Such effects may be delayed for months or years following the procedure [38]. Destruction of the septal mucoperichondrium and subsequent perforation of the septum by prolonged topical use of vasoconstrictive agents such as cocaine and oxymetazoline are also common causes of saddle nose deformity.
Septal perforations unrelated to above-mentioned etiologies require further workup. A thorough serological evaluation and nasal biopsy is required to exclude conditions such as Wegener’s granulomatosis, sarcoid, Crohn’s disease, and relapsing polychondritis [39, 40]. Such illnesses usually result in damage to the septal and middle vault cartilages while involving the bone to a lesser extent [41]. These conditions should be under medical control and in remission prior to reconstructive rhinoplasty. Despite fears of an immunosuppressive regimen’s effect on graft take rate, studies have failed to show increased rates of failure in this patient population and is not a contradiction to surgery [42]. Directed nasal biopsy permits evaluation for neoplastic processes such as inverted papillomas and squamous cell carcinomas in which direct growth of the lesion is locally destructive [20]. Prior to the popularization of septorhinoplasty, infectious processes were frequent causes of septal perforations and included syphilis, leprosy, or septal abscesses [38, 43].
In addition to dorsal contour and septal evaluation, tip support and functional integrity of the internal nasal valves must also be ascertained preoperatively in order to determine whether these areas need to be addressed simultaneously with dorsal augmentation. Finally, the skin-soft tissue envelope (S-STE) should always be examined to determine its thickness as grafting in thinner skin will be more transparent to irregularities, and thus more likely to require onlay camouflage material. Rigid costal grafting may also be untenable for patients who have S-STE with poor vascularity and/or significant cicatricial contracture.
The surgical approach for dorsal augmentation is dependent on the surgeon’s determination of the needs for dorsal reconstruction. Endonasal and external approaches need to be both utilized depending on the nature of the dorsal augmentation as well as the need for tip reconstruction.
6 Harvesting Grafts
6.1 Cartilaginous Rib Grafts
The ribs are marked by palpation of their medial articulation with the sternum starting with the manubrioclavicular joint, which marks the second rib. The fifth, sixth, and seventh ribs are typically chosen for harvesting, but one should be familiar with the overall anatomy of the ribs as certain ribs, such as the ninth rib, can provide two ample straight segments of grafts (Figs. 34.2 and 34.3). In females, an incision is marked at the inframammary fold centered just medial to the midclavicular line and measures approximately 2.5–5 cm in length. Care should be taken not to extend this line beyond the medial border of the inframammary fold in order to avoid an obvious scar when wearing low-cut clothing. In males, the scar is placed above the rib to be harvested, ideally within a hair-bearing area for better concealment.
Harvesting of the ninth rib cartilage takes advantage of the natural curvature of the rib cage. Both a dorsal graft and a dorsocaudal septal strut can be easily carved using this one rib. The disadvantage to harvesting this rib is due to its more inferolateral position and cannot be harvested from an inframammary incision
After ensuring a sterile field, the skin is injected with a lidocaine solution containing epinephrine. Adequate time is allowed for vasoconstriction, and the incision is made through the skin using a scalpel blade. Electrocautery is utilized to dissect the subcutaneous fat, fascia, and muscle layers. Muscle-sparing approach is almost always utilized in order to minimize postoperative pain. Maintaining the dissection directly over the rib targeted for harvesting is aided by direct palpation. The cartilaginous portion of the rib is isolated. The goal is to harvest the largest segment capable of producing long, straight segments. The bony-cartilaginous junction can be identified visually by the change in color from the off-white cartilage to the reddish-gray bone. The perichondrium is incised along the superior and inferior length of the rib. Blunt subperiosteal dissection then ensues around the superior, inferior, and posterior cartilaginous portion of the rib, thus minimizing the risk of violating the pleura and allowing perichondrium to be available for closure if required. Freer and pediatric doyen rib elevators are used to maintain a subperichondrial dissection. Once the cartilage is isolated, a #15 blade is used to make the medial and lateral cuts with freer elevator protecting the pleura to complete the harvesting of the graft. Using the same technique, osseocartilaginous grafts can also be harvested if desired. The internal oblique strongly adheres to the periosteum overlying the rib, and dissecting this layer requires spreading parallel to the direction of the muscle fibers to avoid inadvertent cautery of the underlying bone. If there is difficulty defining the osseocartilaginous junction, a 22-guage needle can be used to differentiate the softer cartilage from the bony rib. The graft is immediately immersed in saline for at least 20 min to account for any warping that may take place. The perichondrium/periosteum is harvested with the graft and can be separated from the bone and/or cartilage to take the place of temporalis fascia as a camouflage onlay graft [33].
The donor site is flooded with saline, and Valsalva maneuver is performed to check for pleural defects. If one is found, a 14-french red rubber catheter is threaded into the defect and connected to continuous suction. The closure is performed in layers to ensure a watertight closure. Once the muscular layers are closed, positive pressure up to 40 mmHg is maintained while the red rubber catheter is withdrawn. Failure to maintain appropriate ventilation volumes and pressures may require placement of a chest tube and appropriate postoperative care – although this is typically not needed. A long-acting local anesthetic is infiltrated in the surrounding area for pain management prior to closure of the skin with suture.
7 Determining the Needs of the Dorsum
7.1 Contour Deformities
The success of any nasal surgery lies in the ability to accurately diagnose the type of dorsal deformity and anticipate which type of grafts are required to attain the desired outcome. Onlay grafting will typically be necessary in a structurally stable nose with contour depression due to overresection of the dorsum. The restoration of the dorsal profile may proceed without concern for strengthening or rebuilding the septal/middle nasal vault. Injectable filler materials may be employed to correct relative supratip depressions, but lasting corrections generally require the use of onlay and support grafts. As previously described, allografts may be used successfully but can result in delayed infection and extrusion. In general, autografts are favored by the authors for dorsal augmentation.
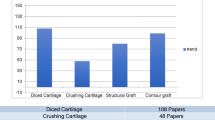
Bare diced cartilage grafts from the septum, concha, or rib have been used but are associated with the possibility of shifting despite placement in a secure pocket of tissue and of palpable irregularities, especially in thinner-skinned individuals (Fig. 34.4). Out of these drawbacks, Erol established the method of wrapping diced cartilage in Surgicel® (ETHICON, West Somerville, NJ) for correction of defects of the nasal dorsum – coined The Turkish Delight [44]. He published a series of 2,365 patients treated over the course of a 10-year period. In addition to the ability to utilize this graft in both endonasal and open approaches, the graft was moldable by manipulation for up to 3 weeks postoperatively. The need for revisions secondary to overcorrection and rate of resorption were both under 1%.
Daniel and Calvert attempts to duplicate these results, however, were unsuccessful due to significant resorption of the grafts [45]. Upon revision, the Surgicel® wrapped grafts were histologically compared to diced cartilage wrapped in temporalis fascia. The specimens wrapped in Surgicel® displayed evidence of significant foreign body reaction, the primary means of Surgicel® degradation, leading to the resorption of the underlying cartilage [46] In comparison, the temporalis fascia wrapped grafts had minimal evidence of resorption and retained the regenerative capacity of the cartilage [45]. A smooth contour was attained, and no evidence of mobility was observed. These grafts may be inserted into the dorsum through an intercartilaginous or external incision and do not require overcorrection. Furthermore, diced cartilage grafts may be the only alternative for patients with extremely compromised S-STE due to the lack of rigidity.
7.2 Contour Deformity with Middle Nasal Vault Collapse
Some patients present with contour deformities in conjunction with internal nasal valve collapse and loss of tip projection. In this setting, middle nasal vault reconstruction is required in addition to reestablishing the nasal dorsal contour [46–48]. In this setting, despite the possibility of the patient having adequate septal cartilage, the surgeon should anticipate the likelihood of having to harvest costal cartilage. The authors will always pre-consent the patient for costal cartilage grafting and maintain a separate set of instruments and surgical field for sterility.
Dorsal augmentation in conjunction with middle vault reconstruction will typically require the surgeon to utilize extended spreader grafts, consisting of two longitudinal struts of cartilage typically measuring 20–25 mm × 3 mm. These are placed between the upper lateral cartilages and the septum. They serve to widen the internal nasal valve, thereby improving the functionality of the internal nasal valve. The grafts are supported by the remaining dorsal septal cartilage and a septal/columellar strut caudally in a tongue-in-groove fashion (Fig. 34.5). This caudal strut is placed at the nasal spine with its maximal width and weight bearing strength at the columellar-labial angle [49]. This configuration will also provide lobular support and help increase tip projection as well as counter-rotate the tip if desired. Once the desired dorsal profile is set, the extended spreader grafts are secured to the existing ULCs to reconstitute the middle nasal vault and to the septal/columellar strut by 5-0 polydioxane sutures. The LLCs are also reattached to this new scaffolding in a tongue-in-groove fashion order to reset the nasal tip.
(a) Dorsal modification using two dorsal struts (dark green) secured to the remaining septal cartilage at the keystone area. This is secured to a caudal septal strut (light blue) anteriorly and to the nasal spine posteriorly. (b) The caudal septal strut placed in a tongue-in-groove fashion over the nasal spine and secured with sutures. This serves as support but can also be used to reset the lower lateral cartilages, thus adjusting tip height
7.3 Contour Deformities with Significant Loss of Structural Support
Significant dorsal contour deformity will almost always lead to significant functional deficits due to the loss of structural support in the middle nasal vault and tip. Augmenting these defects with camouflage onlay grafts without addressing the underlying framework will result in a poorly functioning nose. The dorsal contour should be restored with structurally supporting grafts.
Two alternative approaches can be utilized to address significant dorsal deformities. The most common approach involves utilizing a canoe-shaped dorsal cartilage or osseocartilaginous grafts secured to the bony dorsum and to a dorsocaudal septal strut. The upper lateral cartilages can be secured to the undersurface or lateral aspect of these dorsal grafts, thereby improving the internal nasal valve.
An alternative composite approach popularized by Daniel involves augmenting the dorsal contour after reestablishing of a stable middle nasal vault and tip support with extended spreader grafts cantilevered to septal/columellar struts and tip grafts. The extended spreader grafts described as “pistol” grafts by Gunter should be carved along the natural curvature of the rib and secured beneath the bony dorsum [50]. Caudally, the grafts are secured to a piece of rib cartilage carved to serve as a dorsocaudal septal strut and sutured directly to the nasal spine. The upper lateral cartilages may then be attached to this stable support wall. Adequate nasal lining is critical for the survival of these grafts. Advancing and securing the medial crura to the septal/columellar strut can place the nasal tip at its desired position. If additional projection is required, onlay or shield tip grafts are utilized [51].
Once the structural framework has been established and the tip work completed, dorsal contouring proceeds secondarily. Either fascia alone, diced cartilage, or fascia-wrapped diced cartilage grafts, fashioned from the remaining rib, may be placed along the dorsum in order to achieve the desired contour (Fig. 34.6) [47]. Lateral nasal wall collapse can be corrected through additional cartilage grafts designed to bolster the compromised internal and external nasal valve. Segments of cartilage as thin as 1 mm can be carved and provide adequate support and aesthetics [48].
When dealing with significant dorsal defects, the need for additional grafting should be anticipated. (a) A septal columellar strut may be utilized to lengthen the nose and elevate the tip. (b) Further contour deformities may be addressed through diced cartilage or fascia-wrapped diced cartilage placed upon the new established framework
7.4 Defects Encompassing the Bony Dorsum
Defects of the bony vault that accompanies the complete loss of dorsal septal support and contracture of the nasal lining represent a significant reconstructive undertaking. Composite reconstructions aimed at rebuilding a septal support wall are not possible due to the compromised nasal lining that usually accompanies this type of defect. A new framework must be fashioned from a cantilevered dorsal graft and a dorsocaudal septal/columellar cartilage strut. Tardy et al. reserves the use of autogenous iliac bone crest for reconstruction of these major defects [5]. However, iliac bone harvesting results in significant donor-site morbidity and pain [20]. Membranous calvarial bone grafts have been shown to exhibit improved resorption rates over the endochondral bone of the iliac crest. Thomassin et al. reported a 13.5% resorption rate of iliac versus none for calvarial bone over a mean follow-up of 4 years when correcting moderate and major saddle nose deformities [51]. Calvarial bone has also been utilized for creation of an L-shaped strut in reconstruction. Such a graft has advantages of harvesting generous graft material from the same region of the body, direct bone to bone contact improving graft take rate, and a minimal blood supply requirement [32]. This option is not ideal for patients who have thinning hair, are bald, or have a monocortical calvarium. In addition, iliac crest and calvarial bone grafts fail to address support of the ala and lateral nasal side wall, requiring further harvesting of cartilage from another donor site.
A cantilevered cartilaginous or osseocartilaginous dorsal graft carved from costal cartilage can also provide adequate structural support and aesthetic contour (Fig. 34.7) [47]. These grafts are harvested as previously described. If an osseocartilaginous graft is used, the osseous portion can be aggressively carved out to provide a smooth dorsal contour without the fear of warping. The native bony vault in the upper third of the nose is gently rasped down to accommodate the height of the bony rib, so as not to create a step-off deformity, and allow for an ample bone-to-bone union. If shifting is experienced intraoperatively, the graft can be secured cephalically with percutaneous Kirschner wires, 1.2-mm titanium lag screws, or a 1.2-mm X- or Y-shaped titanium fixation plate to the existing nasal bones (Fig. 34.8). The Kirschner wire, when utilized, is placed percutaneously and removed in the office 7 days after the procedure. Titanium plate fixation can be performed through a separate incision at a prominent rhytid at the nasion (Fig. 34.9).
Total nasal reconstruction with an autologous rib graft. The dorsal and caudal septal struts are supporting additional grafts formed from the remaining cartilage to reconstitute the upper and lower lateral cartilages. While the primary goal of this particular procedure is functional, the principles of structural support are best exemplified by these cases and should be maintained during cosmetic cases as well
A dorsocaudal septal strut is fashioned from the distal cartilaginous portion of the rib graft. This is secured with a 4-0 Prolene suture passed through a drill hole placed in the nasal spine. A hand drill can be utilized or, more practically accomplished, with an 18-guage needle twisted back and forth between the thumb and forefinger. The strut is also vertically incised at its base to permit it to straddle the nasal spine. Tip projection and lateral nasal wall reconstruction may proceed as described above, but results are often limited by extensive contracture of the skin and nasal lining [47–49]. To account for skin contracture, composite grafts from the triangular fossa or concha of the contralateral ear serve as excellent extenders at the alar rim.
8 Conclusions
Augmentation and reconstruction of the nasal dorsum is a challenging component of rhinoplasty. The role of the middle nasal vault in function and aesthetics is vital, and maintenance of the support mechanisms is paramount to the ideal dorsal profile. The interplay between the nasal pyramid, cartilaginous septum and upper lateral cartilages, and lower third of the nose must be taken into consideration during reconstruction. By first ascertaining the exact nature and extent of the defect, the surgeon should be able to anticipate the need for grafts preoperatively. Autologous material provides the most reliable source of graft material, with the most abundant source found in costal cartilage. Harvesting either a cartilaginous or osseocartilaginous graft can be accomplished without significant morbidity to the patient. Strict adherences to the basic principles surrounding nasal support will allow the surgeon to efficiently plan their reconstructive effort and lead to acceptable surgical outcomes.
References
Orten SS, Hilger PA (2008) Facial analysis of the rhinoplasty patient. In: Papel ID, Holt GR, Frodel GL, Larrabee WF Jr, Nachlas NE (eds) Facial plastic and reconstructive surgery, 3rd edn. Thieme Medical Publishing, New York, pp 361–368
Kim I, Chung Y, Lee Y (2008) An anatomic study on the overlap patterns of structural components in the keystone area in noses of Koreans. Clin Exp Otorhinolaryngol 1(3):158–160
Pribitkin EA, Ezzat WH (2009) Classification and treatment of the saddle nose deformity. Otolaryngol Clin North Am 42(3):437–461
Kim DW, Mau T (2006) Surgical anatomy of the nose. In: Bailey B, Johnson J, Newlands S (eds) Head and neck surgery – otolaryngology, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 2511–2532
Tardy ME, Schwartz M, Parras G (1989) Saddle nose deformity: autogenous graft repair. Facial Plast Surg 6(2):121–134
Lupo G (1997) The history of aesthetic rhinoplasty: special emphasis on the saddle nose. Aesthetic Plast Surg 21(5):309–327
Adamson PA (1995) The over-resected nasal dorsum. Facial Plast Surg Clin North Am 3:407–419
Romo T 3rd, Kwak ES (2006) Nasal grafts and implants in revision rhinoplasty. Facial Plast Surg Clin North Am 14(4):373–387
Tham C, Lai YL, Wend CJ, Chen YR (2005) Silicone augmentation rhinoplasty in an oriental population. Ann Plast Surg 54(1):1–5
Turegun M, Sengezer M, Guler M (1998) Reconstruction of saddle nose deformities using porous polyethylene implant. Aesthetic Plast Surg 22(1):38–41
Adams JS (1987) Grafts and implants in nasal and chin augmentation A rational approach to material selection. Otolaryngol Clin North Am 20(4):913–930
Sclafani A, Thomas J, Cox A, Cooper MH (1997) Clinical and histologic response of subcutaneous expanded polytetrafluoroethylene (Gore-Tex) and porous high-density polyethylene (Medpor) implants to acute and early infection. Arch Otolaryngol Head Neck Surg 123(3):328–336
Kridel RW, Konior RJ (1993) Irradiated cartilage grafts in the nose: a preliminary report. Arch Otolaryngol Head Neck Surg 119(1):24–31
Gunter JP, Clark CP, Robinson JB (1999) The rate of warping in irradiated and nonirradiated homograft rib cartilage: a controlled comparison and clinical implications. Plast Reconstr Surg 103(1):265–270
Welling DB, Maves MD, Schuller DE, Bardach J (1988) Irradiated homologous cartilage grafts. Long-term results. Arch Otolaryngol Head Neck Surg 114(3):291–295
Donald PJ (1986) Cartilage grafting in facial reconstruction with special consideration of irradiated grafts. Laryngoscope 96(7):786–807
Kridel RWH, Ashoori F, Liu ES, Hart CG (2009) Long-term use and follow-up of irradiated homologous costal cartilage grafts in the nose. Arch Facial Plast Surg 11(6):378–394
Sclafani AP, Romo T, Jacono AA, McCormick SA, Cocker R, Parker A (2001) Evaluation of acellular dermal graft (AlloDerm) sheet for soft tissue augmentation: a 1-year follow-up of clinical observations and histological findings. Arch Facial Plast Surg 3(2):101–103
Gunter JP, Rohrich RJ (1990) Augmentation rhinoplasty: dorsal onlay grafting using shaped autogenous septal cartilage. Plast Reconstr Surg 86(1):39–45
Dyer WK, Beaty MM, Prabhat A (1999) Architectural deficiencies of the nose: treatment of the saddle nose and short nose deformities. Otolaryngol Clin North Am 32(1):89–112
Marin VP, Landecker A, Gunter JP (2008) Harvesting rib cartilage grafts for secondary rhinoplasty. Plast Reconstr Surg 121(4):1442–1448
Chait LA, Becker H, Cort A (1980) The versatile costal osteochondrial graft in nasal reconstruction. Br J Plast Surg 33(2):179–184
Gibson T (1957–1958) The distortion of autogenous cartilage grafts: its cause and prevention. Br J Plast Surg 10:257–274
Gunter JP, Clark CP, Friedman RM (1997) Internal stabilization of autogenous rib cartilage grafts in rhinoplasty: a barrier to cartilage warping. Plast Reconstr Surg 100(1):161–169
Gunter J, Cochran C, Marin V (2008) Dorsal augmentation with autogenous rib cartilage. Semin Plast Surg 22(2):74–89
Abrahams M, Duggan TC (1964) The mechanical characteristics of costal cartilage. In: Kenedi RM (ed) Biomechanics and related bioengineering topics: proceedings of symposium held in Glasgow. Pergamon Press, New York, p 196
Adams WP, Rohrich RJ, Gunter JP, Clark CP, Robinson JB (1999) The rate of warping in irradiated and nonirradiated homograft rib cartilage: a controlled comparison and clinical implications. Plast Reconstr Surg 103(1):265–270
Harris S, Pan Y, Peterson R, Stal S, Spira M (1993) Cartilage warping: an experimental model. Plast Reconstr Surg 92(5):912–915
Kim DW, Shah AR, Toriumi DM (2006) Concentric and eccentric carved costal cartilage: a comparison of warping. Arch Facial Plast Surg 8(1):42–46
Chase SW, Herndon CH (1955) The fate of autogenous and homogenous bone grafts. J Bone Joint Surg Am 37-A(4):809–841
Mowlem R (1963) Bone grafting. Br J Plast Surg 16:293–304
Shipchandler TZ, Chung BJ, Alam DS (2008) Saddle nose deformity reconstruction with a split calvarial bone L-shaped strut. Arch Facial Plast Surg 10(5):305–311
Christophel JJ, Hilger PA (2011) Osseocartilaginous rib graft rhinoplasty: a stable, predictable technique for major dorsal reconstruction. Arch Facial Plast Surg 13(2):78–83
Bilen BT, Kilinc H (2007) Reconstruction of saddle nose deformity with three-dimensional costal cartilage graft. J Craniofac Surg 18(3):511–515
Kalogjera L, Bedekovic V, Baudoin T, Ivkic M (2003) Modified alar swing procedure in saddle nose correction. Aesthetic Plast Surg 27(3):209–212
Yabe T, Muraoka M (2004) Treatment of saddle type nasal fracture using Kirschner wire fixation of nasal septum. Ann Plast Surg 53(1):89–92
Beekhuis GJ (1974) Saddle nose deformity: etiology, prevention, and treatment; augmentation rhinoplasty with polyamide. Laryngoscope 84(1):2–42
Andrade M, Fernandes VS, Boleo-Tome JP (1999) Saddle nose: our approach to the problem. Aesthetic Plast Surg 23(6):403–406
Merkonidis C, Verma S, Salam MA (2005) Saddle nose deformity in a patient with Crohn’s disease. J Laryngol Otol 119(7):573–576
Shine NP, Hamilton S, McShane DP (2006) Takayasu’s arteritis and saddle nose deformity: a new association. J Laryngol Otol 120(1):59–62
Congdon D, Sherris DA, Specks U, McDonald T (2002) Long-term follow-up of repair of external nasal deformities in patients with Wegener’s granulomatosis. Laryngoscope 112(4):731–737
Vogt PM, Gohritz A, Haubitz M, Steiert A (2010) Reconstruction of nasal deformity in Wegener’s granulomatosis: contraindication or benefit? Aesthetic Plast Surg 35(2):156–161
Malaviya GN, Husain S (1994) Surgical correction of saddle nose deformity in leprosy – one stage procedure. Acta Leprol 9(2):76–82
Erol OO (2000) The Turkish Delight: a pliable graft for rhinoplasty. Plast Reconstr Surg 105(6):2229–2241
Daniel RK, Calvert JW (2004) Diced cartilage grafts in rhinoplasty surgery. Plast Reconstr Surg 113(7):2156–2171
Ertas NM, Hucumenoglu S, Bestalti O, Ozak A, Celebioğlu S (2000) The effects of oxidized, regenerated cellulose on diced cartilage xenograft: an experimental study. Ann Plast Surg 45(2):224–225
Daniel RK (2007) Rhinoplasty: septal saddle nose deformity and composite reconstruction. Plast Reconstr Surg 119(3):1029–1043
Daniel RK, Brenner KA (2006) Saddle nose deformity: a new classification and treatment. Facial Plast Surg Clin North Am 14(4):301–312
Emsen IM (2008) New and detailed classification of saddle nose deformities: step-by-step surgical approach using the current techniques for each group. Aesthetic Plast Surg 32(2):274–285
Gunter JP, Rohrich RJ, Adams WP (2002) Special emphasis on dorsal augmentation: autologous rib cartilage. In: Gunter JP, Rohrich RJ, Adams WP (eds) Dallas rhinoplasty. Quality Medical Publishing, St. Louis, pp 513–527
Thomassin JM, Paris J, Richard-Vitton T (2001) Management and aesthetic results of support grafts in saddle nose surgery. Aesthetic Plast Surg 25(5):332–337
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Ezzat, W.H., Azizzadeh, B. (2013). Costal Cartilage Grafting for Dorsal Augmentation. In: Shiffman, M., Di Giuseppe, A. (eds) Advanced Aesthetic Rhinoplasty. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-28053-5_34
Download citation
DOI: https://doi.org/10.1007/978-3-642-28053-5_34
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-28052-8
Online ISBN: 978-3-642-28053-5
eBook Packages: MedicineMedicine (R0)