Abstract
“Acute liver failure” (ALF) and “fulminant liver failure” are terms used interchangeably to describe severe and sudden onset of liver cell dysfunction leading on to synthetic and detoxification failure across all age groups. Considerable variations exist between ALF in children and adults, in terms of aetiology and prognosis. Encephalopathy is not essential to make a diagnosis of ALF in children but when present has a bad prognosis. Early recognition of ALF and initiation of supportive management improve the outcome. Liver transplantation remains the only definitive treatment when supportive medical management fails.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Acute liver failure
- Liver transplantation
- Hepatocyte transplantation
- Neonatal haemochromatosis
- Transplant listing
-
Encephalopathy is not essential in the diagnosis of ALF in children.
-
Coagulopathy is being used as a prognostic marker in paediatric ALF.
-
Role of liver assist devices and hepatocyte transplant is still limited.
-
Auxiliary liver transplantation if feasible should be offered where indicated as it provides a chance for native liver regeneration.
-
Surrogate markers of prognosis in ALF
-
Defining liver transplant criteria with improved sensitivity and specificity
-
Clinical trials in human hepatocyte transplantation
1 Definition
Trey and Davidson coined the term “fulminant liver failure” 40 years ago to define onset of altered mental status within 8 weeks of initial symptoms of liver dysfunction in an otherwise healthy individual with no previous history of liver disease [1]. This definition was difficult to apply in children with ALF as the disease process could start in utero and time quantification might not be possible and, also, encephalopathy might be difficult to diagnose. Trying to address this issue, Bhaduri and Vergani defined ALF in children as “a rare multisystem disorder in which severe impairment of liver function, with or without encephalopathy, occurs in association with hepatocellular necrosis in a patient with no recognized underlying chronic liver disease” [2]. This newer definition for children failed to differentiate between acute hepatitis and ALF as “severe impairment of liver function” is very subjective and can vary from person to person.
Paediatric Acute Liver Failure (PALF) study group has come up with practical definition to select cases for their multicentre study. They used the following criteria to define acute liver failure (ALF) in children: (1) hepatic-based coagulopathy defined as a prothrombin time (PT) ≥ 15 s or international normalized ratio (INR) ≥ 1.5 not corrected by vitamin K in the presence of clinical hepatic encephalopathy (HE) or a PT ≥ 20 s or INR ≥ 2.0 regardless of the presence or absence of clinical hepatic encephalopathy (HE), (2) biochemical evidence of acute liver injury and (3) no known evidence of chronic liver disease [3]. Due to its simplicity and objectivity, PALF definition is widely used in children.
1.1 Coagulopathy
PALF has used INR as a surrogate marker to denote overall liver synthetic inadequacy and an impending multiorgan failure. Coagulopathy is not only a key criterion in diagnosing paediatric ALF but also helps as prognostic marker. Due to short half of several liver-based clotting factors, PT/INR functions as a dynamic marker of synthetic inadequacy due to loss of functioning hepatocytes in ALF. Factors II, VII, IX and X depend on vitamin K for carboxylation of terminal glutamic acid residues to convert them into active form (Fig. 8.1). Correction of coagulopathy by intravenous vitamin K differentiates between vitamin K deficiency due to decreased absorption and synthetic liver failure. Isolated prolonged APTR is not due to liver disease, as factor VII in extrinsic pathway (Fig. 8.1) has the shortest half-life of the vitamin K-dependent factors; therefore, it is the first factor depleted in ALF and invariably affects INR. Due to defective synthesis and impaired clearance of procoagulant/anticoagulant factors, inflammatory mediators, infection, etc., there could be a degree of intravascular coagulation (IC) that invariably exists in ALF which can progress to fulminant disseminated intravascular coagulation. Haemostasis in liver disease is best assessed using thromboelastography (TEG). TEG is a point-of-care assay using a specialized machine that assesses clot formation in whole blood, including plasmatic and cellular components. TEG provides a graphical representation (Fig. 8.2) of assembly of a clot in whole blood and provides an assessment of overall haemostasis.
The liver is the major site for synthesis of clotting factors, except for von Willebrand factor and tissue plasminogen activator. Factors V and VII are theoretically more sensitive markers than INR (Reproduced with permission from Shanmugam et al., Coagulopathy in liver disease, manual of paediatric liver intensive care) (Springer publication in print)
Figure showing standard TEG in a normal person. Reaction time in minutes (r), time between beginning of the clotting cascade to the initial formation of fibrin; kinetic time in minutes (k), time between initial fibrin formation to reach a specific clot firmness; α-angle in degrees, deals with kinetics of clot formation, rate of fibrin formation and crosslinking of platelets. Maximum amplitude in mm, measures the maximum clot strength; clot lysis at 30 min (Ly-30; in percentage), percentage of clot dissolution within 30 min of maximum amplitude (Reproduced with permission from Shanmugam et al., Coagulopathy in liver disease, manual of paediatric liver intensive care) (Springer publication in print)
2 Aetiology
The causes of ALF vary with the age and geographical location. Infectious aetiology predominates as a cause of ALF in children in the developing countries, while drug-induced ALF predominates in adults and is indeterminate in children in Europe and North America [4]. Table 8.1 shows aetiology of 215 consecutive children with ALF, at King’s College Hospital, London. ALF occurring during neonatal period differs from the rest of the age group by means of aetiology and prognosis [5]. Though exact frequency of ALF in the paediatric age group is unknown, overall annual incidence of ALF in the USA was around 5.5 million population among all ages [6]. Investigation of ALF in children is outlined in Table 8.2.
3 Drugs and Toxins
In developed countries drugs and toxins have become the most common identifiable cause of drug-induced acute liver failure in adults and children. Drug-induced liver injury (DILI) can be a dose-dependent response, an idiosyncratic reaction or a synergistic reaction when two medications are given together. It is essential to enquire about any indigenous/herbal medicine intake as some are potentially hepatotoxic [7]. Acetaminophen is the most common drug associated with ALF and is normally a dose-dependent hepatotoxic agent. Acetaminophen is detoxified mainly by glucuronidation (40%), sulphation (20–40%) and N-hydroxylation (15%). A small fraction is metabolized via cytochrome P450 to yield N-acetyl-para-benzoquinone-imide (NAPQI), a toxic intermediate compound which irreversibly conjugates with the sulphhydryl group of glutathione and causes hepatocyte necrosis [8]. NAPQI forms acetaminophen-protein adducts, which acts as a specific biomarker for chronic acetaminophen-related toxicity. In acute acetaminophen poisoning, serum levels after 4 h of ingestion are useful in identifying high-risk patients. Genetic polymorphism of cytochrome P450 isoenzymes could predispose affected people to acetaminophen toxicity. Anti-tuberculosis drugs, particularly isoniazid, are associated with drug-induced ALF. The mechanism of toxicity is similar to acetaminophen; oxidation via cytochrome P450 pathway results in toxic metabolites.
The true incidence of idiosyncratic drug-induced liver injury (DILI) is unknown; reports have suggested to up to 14 new cases/100,000/year [9]. Around 8% of idiosyncratic DILI developed ALF [10]. DILI is unpredictable, but genetic susceptibility of an individual to certain drugs and underlying mitochondrial cytopathies are proposed causes [11]. The Councils for International Organizations of Medical Sciences/Roussel Uclaf Causality Assessment Method (CIOMS/RUCAM) scale is helpful in establishing causal relationship between offending drug and liver damage. Using the scoring system, suspected drug could be categorized into “definite or highly probable” (score > 8), “probable” (score 6–8), “possible” (score 3–5), “unlikely” (score 1–2) and “excluded” (score ≤ 0) [12]. This scale is helpful in identifying drug-induced hepatotoxicity even in newly marketed drugs and for a previously unreported older drug. Chemotherapy drugs are known to produce veno-occlusive disease leading on to ALF due to endothelial damage. Few of the common drugs that cause ALF are outlined in Table 8.2.
3.1 Viral Hepatitis
Water-borne viral hepatitis (hepatitis A and E) is the most common cause of ALF in developing countries with poor sanitation facilities. Following infection with hepatitis A virus, the risk of developing liver failure is 0.1–0.4%, and this further increases with underlying chronic liver disease. Usually the disease runs a benign course with spontaneous recovery, but some might require liver transplantation [13]. With hepatitis E infection, the risk of developing ALF in adults is 0.6–2.8% [14]. Recent evidence suggests that case fatality due to hepatitis E-induced ALF in pregnancy is similar to that of age-matched general population [15]. The ALF due to hepatitis B virus (HBV) can occur at the time of acute infection, reactivation of chronic HBV infection or seroconversion from a hepatitis B e antigen-positive to a hepatitis B e antibody (HBeAb)-positive state. Superinfection or co-infection of HBV-infected patients with hepatitis delta virus (HDV) can cause liver failure.
Hepatitis C virus (HCV) infection has not been reported as a cause of ALF, and herpes simplex virus can cause ALF, of which herpes simplex virus 1 and 2 (HSV) is the predominant cause of viral-induced ALF during the first month of life.
Babies presenting with fever, rash, lethargy, poor feeding and raised transaminase (in thousands) are usually suggestive of HSV hepatitis. Disseminated neonatal herpes with liver failure carries high mortality. In stable neonates with ALF due to HSV, liver transplantation has been successful. Treatment with high-dose acyclovir should be initiated in all neonates with ALF, until serology results are known. Other members of herpes virus family such as cytomegalovirus, Epstein-Barr virus and varicella-zoster virus can cause ALF. Dengue virus causing ALF is common in tropical countries, which was thought to be multifactorial due to direct viral injury, dysregulated immune response, hypoxic/ischemic injury secondary to shock, etc. [16].
4 Neonatal Haemochromatosis
Neonatal haemochromatosis (NH) is the single most common cause of ALF during the first month of life, due to massive iron deposition in the liver and extrahepatic tissues with sparing of the reticuloendothelial system. NH presents with jaundice, coagulopathy, moderately elevated alanine aminotransferase, high ferritin and raised iron saturation levels. The disease varies in severity; at one end of spectrum, it is associated with foetal death, while at the other end, spontaneous recovery is reported.
The pattern of iron overloading is similar to hereditary haemochromatosis, but NH is entirely different condition affecting newborn, and so far no specific genetic mutation has been identified [17]. Current hypothesis suggests NH to be an alloimmune process where maternal antibody is directed towards foetal liver cells resulting in hepatocyte loss [18, 19]. This hypothesis is supported by successful prevention of severe disease by antenatal and postnatal treatment with intravenous immunoglobulin. High serum ferritin is a non-specific marker and elevated in other causes of ALF and so should not be used a marker for diagnosis. The diagnosis could be safely confirmed by labial salivary gland biopsy, showing extrahepatic iron deposits with reticuloendothelial system sparing [20].
5 Metabolic Disorders
Metabolic disorders are important cause of ALF in paediatric population particularly during infancy. Galactosaemia, tyrosinaemia type I and fructosaemia are few of the metabolic disorders that could present as ALF. Tyrosinaemia type I is an inborn error of amino acid metabolism, due to absence of enzyme fumarylacetoacetase, the last enzyme in a series of five enzymes needed to break down tyrosine. This results in formation of intermediate compounds, maleylacetoacetic acid and fumarylacetoacetic acid, which is converted to succinylacetone, a toxin that damages the liver and kidneys. Oral NTBC (nitro-4-trifluoromethylbenzoyl-1,3-cyclohexanedione) and phenylalanine- and tyrosine-free diet could help liver recovery, but some children might require LT. Galactosaemia type 1 is autosomal recessive disorder with mutation in galactose-1-phosphate uridyl transferase (GALT) gene located on chromosome 9p13. Lactose-free diet should be started in any infant presenting with ALF or hepatitis until the quantitative GALT activity is available. Galactose-free diet and supportive treatment may allow recovery of ALF. Rarely inborn errors of bile acid synthesis can present as ALF.
Mitochondrial disorders are group of spontaneous or inherited disorders of mitochondrial proteins resulting in defective oxidative phosphorylation, fatty acid oxidation, urea cycle and other mitochondrial pathways [21]. Deficiencies of complexes I, III and IV, multiple complex deficiencies and mitochondrial DNA (mtDNA) depletion syndrome are associated with liver failure. Diagnosis might be difficult due to particularly (mtDNA) depletion syndrome where there is tissue-specific mitochondrial enzyme deficiency. These infants usually present with hypotonia, hypoglycaemia, feeding difficulties, seizures and deranged liver function. Liver transplantation could be done in isolated liver-based mitochondrial disorders, and it is usually contradicted in multisystemic involvement [22]. Sasaki et al. have reported 78% survival in a cohort of nine children with mitochondrial respiratory chain disorder, which included children with extrahepatic manifestation such as developmental delay and failure to thrive [23].
Medium-chain acyl-coenzyme A dehydrogenases (MCAD) are group of enzymes involved in β-oxidation of 6–12 carbon chain fatty acids in mitochondria. Affected children could present with hypoketotic hypoglycaemia and recurrent liver failure, precipitated by otherwise minor illness. Unless treated with dextrose supplementation, these episodes may quickly progress to coma and death.
Wilson’s disease, an autosomal recessive disorder, could present as ALF. The acute hepatic presentation is usually characterized by the presence of liver failure, Coombs-negative haemolytic anaemia and low serum alkaline phosphatase. Diagnosis might be difficult in acute presentation as blood test might show weakly positive autoantibodies, and tissue copper estimation might not be possible due to coagulopathy. New Wilson index proposed by Dhawan et al. used five parameters such as serum bilirubin, serum albumin, international normalized ratio, aspartate aminotransferase (AST) and white cell count (WCC) at presentation. Based on serum levels, each parameter is graded from 0 to 4, with a total maximum score of 20. They identified a cutoff score of more than 11 for death without transplantation and proved to be 93% sensitive and 98% specific, with a positive predictive value of 88% [24].
6 Malignancies
Haemophagocytic lymphohistiocytosis (HLH) is a type of haematological malignancy that could present as ALF in children. HLH is due to paradoxical overactivation of natural killer cells and of CD8+ T-cell lymphocytes resulting in destruction of own haemopoietic cells. It could be familial (inherited) or acquired. Familial HLH usually presents during infancy, while secondary HLH usually occurs after systemic infection or immunodeficiency, which can affect people at any age. Familial HLH is an autosomal recessive disease resulting in reduced or defective production of cytoplasmic granules such as perforin in cytotoxic cells resulting in paradoxical overactivation. HLH presents with fever, cutaneous rash, hepatosplenomegaly, pancytopenia and, in severe cases, ALF [25]. Though rare, leukaemia or lymphoma could present with ALF [26].
Other causes: Autoimmune hepatitis (AIH), particularly type 2 (positive liver-kidney microsomal (LKM) antibody), can present with ALF. ALF due to AIH with encephalopathy usually does not respond to any form of immunosuppression and needs urgent liver transplant [27]. In spite of extensive investigation, the diagnosis could not be found in some of the children (indeterminate). There is centre-to-centre variation in incidence of indeterminate ALF, probably due to incomplete investigations, which has been highlighted by Narkewicz et al. [28].
7 Investigations
General investigation should include liver function tests, serum electrolytes, uric acid, lactate, cholesterol/triglyceride, amylase, serum amino acids, blood gas analysis, blood glucose levels, full blood count, blood grouping, Coombs test coagulation studies (INR), urinary amino/organic acids and toxicology screen along with surveillance blood and urine cultures. In liver function tests, coagulation should be checked on regular basis that helps in monitoring the progression of disease. Investigations to establish the underlying aetiology are listed in Table 8.2. Detailed clinical history and physical examination give valuable clue of underlying diagnosis. This would provide guidance in choosing appropriate investigations.
8 Prognosis
Transplant-free survival is aetiology dependent. Age of patient was not associated with outcome in adults [29], while in children, neonates have worst prognosis (Fig. 8.2), probably due to predominance of certain aetiology in different age groups. Prognostic scoring helps in predicting mortality and helps in listing appropriate patients for transplantation.
For non-acetaminophen ALF, several prognostic scoring systems are available for adults, but in children there are no universally accepted criteria for listing. To date, INR and factor V concentration remain the best indicators of mortality without transplantation in paediatric ALF. Bhaduri and Mieli-Vergani showed that the maximum INR reached during the course of illness was the most sensitive predictor of the outcome, with 73% of children with an INR less than 4 surviving compared with only 4 of 24 (16.6%) with an INR greater than 4 [2]. In children, a factor V concentration of less than 25% of normal suggests a poor outcome. A prognostic score incorporating serum bilirubin, serum albumin, international normalized ratio, aspartate aminotransferase (AST) and white cell count (WCC) is available predicting the outcome of decompensated Wilson’s disease [24]. In acetaminophen overdose adult criteria of INR > 6.5, creatinine > 300 μmol/L and hyperphosphatemia or metabolic acidosis arterial pH less than 7.3, after the second day of overdose in adequately hydrated patients, is used to list children for liver transplantation [30].
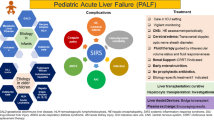
9 Management
Management of ALF and its complications still remains a challenge. Early diagnosis helps in initiation of investigation and safe transfer to a specialist centre. Diagnostic algorithm for any child with abnormal liver function test is outlined in Fig. 8.3.
Approach to children with biochemical evidence of liver injury (Reproduced with permission from Shanmugam et al., Neonatal liver failure: aetiologies and management state of the art. Eur J Pediatr. 2011 May; 170(5):573–81). # Raised alanine aminotransferase (ALT), bilirubin, gamma-glutamyltransferase (GGT). *Check prothrombin time (PT)/international normalized ratio (INR), activated partial thromboplastin ratio (APTR), fibrinogen and d-dimers. Isolated prolonged APTR is not due to liver disease. In disseminated intravascular coagulopathy (DIC), there will be low fibrinogen levels and increased d-dimers. **INR ≥ 1.5 with encephalopathy or INR ≥ 2.0 regardless of the presence or absence of encephalopathy
10 General Measures
All children with ALF should be closely monitored in a quiet setting. Vital parameters such as oxygen saturation, pulse, blood pressure and neurologic observations should be done on regular basis. Prophylactic broad-spectrum antibiotics and antifungals should be started in all children, and acyclovir should be added in infants and neonates. Hypoglycaemia should be avoided either by parenteral glucose or adequate enteral feeds. Children with encephalopathy or an INR > 4 (regardless of encephalopathy) should be admitted to an intensive care unit for continuous monitoring. Prophylactic histamine 2 blockers or proton-pump inhibitors should be started to all patients requiring mechanical ventilation [31]. Coagulopathy is corrected only if the patient is already listed for transplant or prior to an invasive procedure. To correct coagulopathy, fresh frozen plasma could be given at a dose of 10 mL/kg and cryoprecipitate at 5 mL/kg (if fibrinogen is <1 g/L). Factor VII concentrates improve the coagulopathy for a short period. Platelet count should be maintained above 50 × 109/dL, as thrombocytopenia is an important risk factor for haemorrhage.
N-acetylcysteine (NAC) is being increasingly used as a part of general supportive measure in non-acetaminophen-induced ALF, as it enhances circulation and improves oxygen delivery. In a prospective, double-blind trial in adults with non-acetaminophen ALF, NAC usage is associated with significant improvement in transplant-free survival in patients with early (stage I–II) coma [32]. A similar study in children failed to show any benefit, and Paediatric Acute Liver Failure study group does not recommend routine use of NAC in non-acetaminophen-induced ALF in children [33]. Bowel cleansing agents and benzodiazepine antagonists are of no proven benefit [34].
11 Airway and Ventilation
Elective intubation and mechanical ventilation should be considered for patients with grade 3/4 encephalopathy. Apart from providing secure airway, sedation and controlled ventilation help in reducing sudden variation of intracranial pressure (ICP). Induction using suxamethonium and fentanyl and combination of morphine or fentanyl with a hypnotic such as midazolam for sedation is usually safe in children. Normocapnia is to be maintained, as hypercapnia causes vasodilatation and increases cerebral congestion, while hypocapnia causes vasoconstriction and thus decreased blood flow to the brain.
12 Fluid Management and Renal Failure
Intravenous fluids should be restricted to two-thirds maintenance, with the idea of decreasing the possibility of development of cerebral oedema. Ultrasonic cardiac output monitor (USCOM), which is a non-invasive method to measure cardiac parameters, helps in decision-making regarding appropriate fluid regimens/inotropes even in small infants. In the presence of persistent hypotension, noradrenaline is the inotropic agent of choice. Continuous filtration or dialysis systems should be considered when the urine output is less than 1 mL/kg/h to prevent acidosis and volume overload.
13 Neurologic Complications
The most serious complications of ALF are cerebral oedema with resultant encephalopathy and intracranial hypertension, progressively leading on to brain herniation and death. Systemic hypertension, bradycardia, hypertonia, hyperreflexia and in extreme cases decerebrate or decorticate posturing are clinical features of raised ICP. Ammonia-lowering measures such as dietary protein restriction, bowel decontamination or lactulose are of limited or no value in rapidly advancing encephalopathy. Mannitol is an osmotic diuretic commonly used to treat intracranial hypertension. A rapid bolus of 0.5 g/kg as a 20% solution over a 15-min period is recommended, and the dose can be repeated if the serum osmolarity is less than 320 mOsm/L. Hypertonic saline could be also used in emergency situation, where there is impending brainstem herniation. Studies have shown mild cerebral hypothermia (32–35 °C), sodium thiopental and hypernatremia (serum sodium > 145 mmol/L) improves cerebral perfusion.
14 Disease-Specific Management
Disease-specific management is outlined in Table 8.2. Intravenous immunoglobulin (IVIG) at a dose of 1 g/kg body weight given weekly from the 18th week until the end of gestation as antenatal prophylaxis to mothers whose previous pregnancy/child was affected with NH has been associated with milder phenotypic expression of the disease and 100% survival of babies [35]. Evidence is accumulating towards the usefulness of high-dose IVIG (1 g/kg), in combination with exchange transfusion resulting in significant decrease in the need for liver transplantation in NH. Dietary intervention with restriction of phenylalanine and tyrosine together with oral medication, 2(2-nitro-4-trifluoromethylbenzoyl)-1,3-cyclohexenedione (NTBC), helps in normalization of liver function, but doesn’t prevent long-term risk for development of hepatocellular carcinoma in children started beyond infancy.
15 Plasmapheresis/Plasma Exchange in ALF
Plasmapheresis is the removal or exchange of blood plasma. Therapeutic plasmapheresis and therapeutic plasma exchange (TPE) are terms that are often used synonymously. TPE has been increasingly used over the past decade as a first-line and lifesaving treatment for various conditions classified by the American Society for Apheresis (ASFA). In acute fulminant Wilson’s disease, it can rapidly remove significant amount of copper and, thereby, reduce haemolysis, prevent progression to renal failure and provide clinical stabilization. It has been reported to be used as a bridge to LT or can lead to elimination of the need for urgent LT. TPE is also helpful in stabilizing ALF due to viral hepatitis, drug-induced hepatitis, etc. by removing albumin-bound toxins, large molecular weight toxins, aromatic amino acids, ammonia, endotoxin, indols, mercaptans, phenols, etc.
16 Liver Assist Devices
Simple liver assist devices detoxify blood by simple osmotic diffusion, while bioartificial liver support system which contains human or animal liver cells could perform complex synthetic function and detoxifying and detoxification. These devices have shown to decrease the toxins (ammonia, bilirubin, cytokines, etc.) but have no effect on mortality. Successful use of these devices in children with ALF as a bridge therapy, supporting liver function while the native liver regenerates, is not recommended outside research setting.
17 Liver Transplantation
Liver transplant remains the only proven treatment that has improved the outcome of ALF. Appropriate patient selection and timing of transplantation are essential for graft and patient survival. Several surgical techniques such split liver grafts, reduced grafts and auxiliary liver transplants are practiced, depending upon patient size, organ availability and surgical expertise available. Auxiliary liver transplant is a surgical technique where the donor liver is placed alongside of native liver and the allograft supports the entire liver function, while the native liver regenerates. Either left lateral segment or right lobe allograft could be used, based on recipient weight. Once native liver regeneration is optimal [36], then immunosuppression could be weaned and eventually stopped. In a series from King’s College Hospital, of the 20 children who received auxiliary liver transplantation for ALF, immunosuppression was withdrawn successfully in 11 patients at a median time of 23 months after transplantation [37]. This would be an ideal option in ALF due to indeterminate aetiology, as spontaneous regeneration of native liver remains a possibility.
Liver transplantation is indicated in ALF due to liver-based disorders while contraindicated in haematological malignancies, uncontrolled sepsis, systemic mitochondrial/metabolic disorders and severe respiratory failure (ARDS) [38]. Relative contraindications are increasing inotropic requirements, infection under treatment, cerebral perfusion pressure of less than 40 mmHg for more than 2 h and a history of progressive or severe neurologic problems.
Hepatocyte transplantation, where hepatocytes are infused intraportally into the patient’s liver, has been tried with variable success in certain liver-based metabolic disorders [39]. Research is underway to use alginate-encapsulated hepatocytes, which could be injected intraperitoneally. This could act as a bridge until native liver regenerates. Hepatocyte transplantation is not recommended outside research setting.
18 Conclusion
Improved intensive care management has greatly increased the ALF survival. When compared to adult ALF, the spectrum of underlying aetiology, management and outcome varies in paediatric ALF. Acyclovir should be started in all neonates with ALF along with prophylactic antibiotics, until viral cultures are negative. Liver transplantation is the only definitive treatment that improves survival in paediatric ALF. Wilson’s disease and autoimmune liver disease presenting as ALF usually do not respond to medical management and warrant liver transplantation. Liver assist devices and hepatocyte transplantation are potential emerging therapies in paediatric ALF.
References
Trey C, Davidson CS. The management of fulminant hepatic failure. Prog Liver Dis. 1970;3:282–98.
Bhaduri BR, Mieli-Vergani G. Fulminant hepatic failure: pediatric aspects. Semin Liver Dis. 1996;16(4):349–55.
Squires RH Jr, et al. Acute liver failure in children: the first 348 patients in the pediatric acute liver failure study group. J Pediatr. 2006;148(5):652–8.
Alam S, et al. Profile and outcome of first 109 cases of paediatric acute liver failure at a specialized paediatric liver unit in India. Liver Int. 2017;37(10):1508–14.
Shanmugam NP, et al. Neonatal liver failure: aetiologies and management—state of the art. Eur J Pediatr. 2011;170(5):573–81.
Bower WA, et al. Population-based surveillance for acute liver failure. Am J Gastroenterol. 2007;102(11):2459–63.
Larrey D. [Hepatotoxicity of drugs and chemicals]. Gastroenterol Clin Biol. 2009;33(12):1136–46.
Davis M. Protective agents for acetaminophen overdose. Semin Liver Dis. 1986;6(2):138–47.
Bjornsson E. Review article: drug-induced liver injury in clinical practice. Aliment Pharmacol Ther. 2010;32(1):3–13.
Idilman R, et al. The characteristics and clinical outcome of drug-induced liver injury: a single-center experience. J Clin Gastroenterol. 2010;44(6):e128–32.
Ghabril M, Chalasani N, Bjornsson E. Drug-induced liver injury: a clinical update. Curr Opin Gastroenterol. 2010;26(3):222–6.
Andrade RJ, et al. Assessment of drug-induced hepatotoxicity in clinical practice: a challenge for gastroenterologists. World J Gastroenterol. 2007;13(3):329–40.
Ciocca M, et al. Prognostic factors in paediatric acute liver failure. Arch Dis Child. 2008;93(1):48–51.
Krawczynski K, Kamili S, Aggarwal R. Global epidemiology and medical aspects of hepatitis E. Forum (Genova). 2001;11(2):166–79.
Bhatia V, et al. A 20-year single-center experience with acute liver failure during pregnancy: is the prognosis really worse? Hepatology. 2008;48(5):1577–85.
Samanta J, Sharma V. Dengue and its effects on liver. World J Clin Cases. 2015;3(2):125–31.
Hardy L, et al. Neonatal hemochromatosis. Genetic analysis of transferrin-receptor, H-apoferritin, and L-apoferritin loci and of the human leukocyte antigen class I region. Am J Pathol. 1990;137(1):149–53.
Whitington PF, Malladi P. Neonatal hemochromatosis: is it an alloimmune disease? J Pediatr Gastroenterol Nutr. 2005;40(5):544–9.
Pan X, et al. Novel mechanism of fetal hepatocyte injury in congenital alloimmune hepatitis involves the terminal complement cascade. Hepatology. 2010;51(6):2061–8.
Smith SR, et al. Minor salivary gland biopsy in neonatal hemochromatosis. Arch Otolaryngol Head Neck Surg. 2004;130(6):760–3.
Treem WR, Sokol RJ. Disorders of the mitochondria. Semin Liver Dis. 1998;18(3):237–53.
Dhawan A, Mieli-Vergani G. Liver transplantation for mitochondrial respiratory chain disorders: to be or not to be? Transplantation. 2001;71(5):596–8.
Sasaki K, et al. Liver transplantation for mitochondrial respiratory chain disorder: a single-center experience and excellent marker of differential diagnosis. Transplant Proc. 2017;49(5):1097–102.
Dhawan A, et al. Wilson’s disease in children: 37-year experience and revised King’s score for liver transplantation. Liver Transpl. 2005;11(4):441–8.
Henter JI, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48(2):124–31.
Kader A, et al. Leukaemia presenting with fulminant hepatic failure in a child. Eur J Pediatr. 2004;163(10):628–9.
Mieli-Vergani G, Vergani D. Autoimmune paediatric liver disease. World J Gastroenterol. 2008;14(21):3360–7.
Narkewicz MR, et al. Pattern of diagnostic evaluation for the causes of pediatric acute liver failure: an opportunity for quality improvement. J Pediatr. 2009;155(6):801–6.e1.
Ostapowicz G, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137(12):947–54.
O’Grady JG, et al. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology. 1989;97(2):439–45.
Polson J, Lee WM. AASLD position paper: the management of acute liver failure. Hepatology. 2005;41(5):1179–97.
Koch A, Trautwein C. N-acetylcysteine on its way to a broader application in patients with acute liver failure. Hepatology. 2010;51(1):338–40.
Squires RH, et al. Intravenous N-acetylcysteine in pediatric patients with nonacetaminophen acute liver failure: a placebo-controlled clinical trial. Hepatology. 2013;57(4):1542–9.
Cochran JB, Losek JD. Acute liver failure in children. Pediatr Emerg Care. 2007;23(2):129–35.
Whitington PF, Hibbard JU. High-dose immunoglobulin during pregnancy for recurrent neonatal haemochromatosis. Lancet. 2004;364(9446):1690–8.
Dhawan A. Clinical human hepatocyte transplantation: current status and challenges. Liver Transpl. 2015;21(Suppl 1):S39–44.
Faraj W, et al. Auxiliary liver transplantation for acute liver failure in children. Ann Surg. 2010;251(2):351–6.
Strom SC, et al. Hepatocyte transplantation as a bridge to orthotopic liver transplantation in terminal liver failure. Transplantation. 1997;63(4):559–69.
Forbes SJ, Gupta S, Dhawan A. Cell therapy for liver disease: from liver transplantation to cell factory. J Hepatol. 2015;62(1 Suppl):S157–69.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Shanmugam, N., Dhawan, A. (2019). Acute Liver Failure in Children. In: D'Antiga, L. (eds) Pediatric Hepatology and Liver Transplantation. Springer, Cham. https://doi.org/10.1007/978-3-319-96400-3_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-96400-3_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-96399-0
Online ISBN: 978-3-319-96400-3
eBook Packages: MedicineMedicine (R0)