Abstract
Background. In recent years, virtual reality (VR) has emerged as an efficient distraction technique to reduce procedural pain among both adults and children. However, the effectiveness of VR as a distraction technique remains scarcely evaluated during many painful procedures. In many countries, such as Italy, VR analgesia is hardly applied.
Aim. The current study aims to highlight the potentials and the limitations of VR analgesia for children’s pain management in clinical settings and to explore the feasibility and the effectiveness of VR distraction in Italy.
Methods. Studies that applied VR analgesia to children and adolescents undergoing painful procedures in clinical settings were included in the analysis. Factors influencing VR analgesia and the effectiveness of VR distraction for pain management were considered. The feasibility and the effectiveness of a low-cost VR system was evaluated for patients undergoing venipuncture in an Italian children’s hospital.
Results. Factors influencing VR analgesia are still sparsely investigated, particularly regarding the psychological variables, such as anxiety and coping strategies. Italian patients suffering from cancer and kidney diseases who used VR distraction reported lower levels of pain and higher levels of fun compared with the control group.
Discussion. VR analgesia is destined to be applied more in clinical settings; however, VR systems designed for the specific use of VR analgesia in clinical settings are needed. In the Italian context, VR systems are necessary to improve the knowledge of VR analgesia among physicians, nurses, and clinical psychologists and encourage further research in this field.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
1.1 Virtual Reality for Pain Management: How Does It Work?
In recent years, new technologies had a large expansion, not only for entertainment or pleasure, but also as versatile tools applied to improve people’s health. Virtual Reality (VR) has probably been one of the most important emerging technologies [1]; it lets people experiment with realistic experiences, overcome their fears, and relax by simply wearing a head-mounted display. The use of VR in clinical settings is not a recent novelty; however, only lately it has been applied in a more extended manner. Healthcare practitioners can use VR to promote patients’ health in different directions; one of these methods is VR analgesia, a non-pharmacological technique for pain management that has captured the interest of a growing number of researchers.
VR analgesia is a non-pharmacological technique for pain management based on distraction. Involving the most common distraction techniques (playing with a video game, reading a book, or listening to music), VR analgesia aims to capture the patient’s attention to a pleasant activity during painful medical procedures. Generally, the effectiveness of distraction techniques for pain reduction can be explained by Eccleston and Crombez’s interruption of attention and pain theory [2]. This interpretive model considers pain a stimulus, such as a sound or an image, that requires attention to be experienced. As personal attentional resources are limited, if a person focuses most of his or her attentive resources on a different stimulus, the person’s capability to feel pain would be reduced. This being the case, the techniques for pain management based on distraction should capture the patients’ attention by involving them in interesting, age-appropriate, and attention-demanding activities. Generally, the most common distraction techniques are easy to use and require the application of simple tools (i.e., books, toys, and video games) that are well known by patients. However, many other distraction techniques include specific professionals’ interventions that involve patients in pleasant activities, such as playing an instrument or having fun with dogs or clowns [3,4,5,6,7]. In this varied scenario, the factor that unifies the most common distraction techniques is that during the painful procedure, although the patient’s attention to the painful stimulus is reduced by the activity, the person continues to see and hear what is happening in the room. Indeed, the most widely used distraction techniques can only partially isolate the patient from the real environment (e.g., listening to music or talking with the nurse can occlude the sounds, and playing with video games or reading a book can reduce the visual attention to the painful procedure). On the contrary, while patients are interacting with VR distraction, they wear a head-mounted helmet that physically occludes the possibility to hear and watch the real environment. According to Eccleston and Crombez’s interpretive model [2], the high level of isolation from the painful stimulus and the possibility to interact with the VR video game (based on the characteristics of the software) would strongly reduce the attentional resources available to experience pain. Thus, the analgesic effect of VR would be hypothetically stronger compared with the analgesic effect of non-immersive distraction techniques. With respect to this aspect, the pieces of evidence presented in the literature are not uniform, and the superiority of VR analgesia over video games or other distraction techniques is not always supported by proof [8]. These inconsistent results could depend on methodological differences across studies and on individual differences among children.
1.2 Factors Influencing the Effectiveness of VR Analgesia
Presence, Immersion, and Interactivity.
Presence, described as the psychological illusion of being in the computer-generated world and feeling virtual experience as real [9, 10], seems to play a central role in the user’s response to VR stimuli and in the effectiveness of mediated environment applications. Another important factor connected with the effectiveness of VR analgesia is immersion, a concept often confused with presence and defined by Slater and Wilbur [11] as the quality of the system’s technology and capability to produce a vivid virtual environment. According to the two authors, a deep relationship exists between presence and immersion; the more immersive the system is, the more likely the user would feel present in the virtual world and the more likely the virtual environment would dominate physical reality in determining the person’s response. Regarding the specific field of pain management, it has been demonstrated that patients undergoing thermal pain stimulation while wearing a low-quality helmet reported higher levels of pain compared with patients undergoing the same stimulation but wearing a high-quality helmet and compared with the control group under the no-distraction condition [12]. In another study, Hoffman et al. [13] evaluated the pain ratings of adult volunteers undergoing thermal pain stimulation. The subjects in the “high-tech VR group” (multisensory distraction, helmet, and head-tracking system) reported lower levels of pain and higher levels of presence compared with the subjects in the “low-tech VR group” (only visual distraction, eyeglasses, and no head tracking), and the amount of pain reduction (worst pain) was positively and significantly correlated with VR presence levels. In contrast, in a study involving children with burn injuries undergoing a dressing change, the sense of presence showed no significant correlation with the patients’ pain ratings [14]. Age has been demonstrated to influence the sense of presence, as confirmed by Sharar et al. study [15]. According to their results, presence and realism scores were significantly higher among children (6–18 years) than among adults; however, younger patients did not report lower levels of pain compared with adults when interacting with VR. A recent review study that analyzed psychological variables associated with the effectiveness of VR analgesia highlighted that presence might not have a direct impact on pain experience per se, but it could allow VR to be distractive from a perceptual point of view [16]. However, only a few clinical studies have evaluated the sense of presence among patients undergoing medical procedures, and the role of presence in the effectiveness of VR analgesia remains unclear. Other studies comparing VR with video games highlighted better performance when users interacted in a non-immersive setup [17, 18], but these findings were not always confirmed [19]. As for presence, the role of immersion in the effectiveness of VR as a distraction technique for pain management is not completely clear. Some studies compared pain levels reported by young patients undergoing medical procedures with those under the control condition in which the group was distracted with a desktop video game. The results suggest that immersive systems can produce better analgesia compared with non-immersive systems [20,21,22]; however, no significant differences have been detected when compared with watching television [23].
Another variable connected with the effectiveness of VR analgesia is interactivity. The possibility to interact with the VR environment seems to promote higher pain reduction compared with passive distraction in a laboratory study [24]. This finding supports Eccleston and Crombez’s interpretive model [3] and has relevant implications for the realization of VR environments. Passive VR analgesia was compared with interactive VR non-interactive VR analgesia among pediatric-age patients in only one clinical study, which supported the results of the laboratory study. However, a significant pain reduction was detected by using a passive VR system compared with watching cartoons among patients undergoing dental care. These findings suggest that interactivity may not make a difference. However, more studies with a larger sample are needed to gain a better understanding of the role played by interactivity in the effectiveness of VR analgesia.
Anxiety and Distress.
Psychological factors, such as anxiety, could also influence the user’s experience during an interaction with VR. Indeed, in a recent study aimed to detect the main difference between VR and a non-immersive video game, significantly higher levels of anxiety emerged when the users interacted with VR compared with the video game [19]. In practical clinics, the deep connection between anxiety and pain is well known, and the literature confirms that anxiety can exacerbate pain perception [25]. For this reason, it can be hypothesized that VR distraction could have a minor analgesic effect if patients report high levels of anxiety. Moreover, high levels of anxiety could influence the patients’ capability to focus their attentional resources on the VR environment and limit the levels of presence. To date, no study has directly evaluated the role of anxiety with respect to the effectiveness of VR analgesia [16]; however, Jeffs et al. considered the relationship between anxiety and engagement in the intervention [26]. They highlighted that burn patients’ pain ratings were significantly lower in the VR distraction group compared with those in the group that was distracted by watching a video. Moreover, the patients’ trait anxiety was negatively correlated with distraction engagement, showing low levels of engagement in distraction when the patients reported high levels of trait anxiety. However, the results of Pallavicini et al. study [19] seemed unconfirmed by clinical studies that evaluated VR as a distraction technique for pain management among children. Indeed, VR analgesia was demonstrated as a useful tool to reduce children’s distress in two clinical studies with burn patients [21, 22], and significantly lower levels of anxiety were reported in another research by Hoffman et al. [20].
More studies are needed to understand the factors that can influence VR analgesia in order to evaluate its effectiveness and acceptability compared with other distraction techniques. Indeed, a recent review study highlighted that high-technology distraction techniques (video games and VR) were unable to produce a significantly higher analgesia compared with low-technology distraction techniques (reading a book, blowing bubbles…) during venipuncture [5]. However, these finding should be cautiously interpreted because the quality of the VR systems in the two included studies wasn’t indicated and one of the systems was passive [27, 28].
2 Virtual Reality for Children and Adolescents’ Pain Management: The State of the Art
VR analgesia has been applied in several clinical settings to improve children’s pain management during medical procedures. The first studies included burn patients, who needed numerous painful procedures (such as dressing changes and physical therapy) for the treatment of their wounds [20]. Currently, the evaluation of VR effectiveness for these patients remains the most investigated domain compared with other kinds of diseases and procedures [8]. Little is known about the effectiveness of VR distraction in other invasive procedures, such as needle-related procedures, that are described by young patients as among the most painful and fearful aspects in hospitals [29]. Gold et al. [27] compared VR analgesia to a topical analgesic spray among patients undergoing venipuncture for magnetic resonance. Their results noted a significantly higher satisfaction regarding pain management and lower levels of pain in the VR condition; however, the difference in the pain level was not significant. VR distraction has also been applied to children suffering from cancer during port access and lumbar puncture, two common medical procedures for oncological patients. Significantly lower levels of pain and distress were reported by patients who used VR during port access compared with the control group subjected to the non-distraction condition [30]. However, in Sander Wint’s study [28], patients undergoing lumbar puncture in an experimental condition (VR plus pharmacological analgesia) did not report lower levels of pain compared with patients who only received pharmacological analgesia. The inconsistency of these results could depend on the quality of the VR systems used in the studies. Indeed, Sander Wint et al. used a non-interactive VR system (no interactivity and narrow field of view through VR goggles), and the analgesic effect could be reduced for this reason [12, 24]. Moreover, the effectiveness of VR during dental procedures, which often generate anxiety and pain among children [31], is still under-investigated. Only a study involving children undergoing fluoride therapy and restorative treatment found that patients distracted with VR reported significantly lower levels of pain and anxiety compared with the control group that watched cartoons. Interestingly, this study used a passive VR system.
More recently, VR has also been introduced for chronic pain management, but few studies have evaluated its effectiveness among children [32]. In this field, VR could encourage patients to move and experience positive emotions despite their pain [33].
3 Applicability of Virtual Reality Analgesia in Clinical Settings: Specific Aspects, Limitations and Considerations
According to the literature, VR has immense potential as a distraction technique for pain management. However, when planning the use of VR in hospitals and other clinical settings, many aspects connected with the spaces, the hygienic norms, and the specific patients’ needs (based on their diseases and own abilities) should be considered. VR analgesia requires the use of at least three elements (a computer, a head-mounted helmet, and a joystick) that need to be connected with a power outlet. Therefore, the first limitation is that VR distraction can only be used in a room that is large enough and has power outlets Regarding the hygienic norms, the helmet (or the other types of VR goggles) can be easily cleaned with a sanitizing gel, so it can be safely worn by patients in hospitals.
The choice of the most suitable VR system is not easy, neither for the hardware component nor for the software component. On one hand, high-quality VR systems (wide field-of-view helmet, head tracking, and interactive software) should be preferred to promote more realistic experiences, higher levels of presence, and hypothetically better analgesia [12, 24]. On the other hand, low-quality systems (narrow field of view, eyeglasses, and passive software) have also been demonstrated to produce a significant analgesic effect in a limited number of studies. For example, significantly lower levels of pain were reported by pediatric patients who interacted with VR during routine dental care compared with the control group subjected to the no-distraction condition in Aminabadi et al. study [35]. In the VR analgesia condition, patients wore a passive VR system (eyeglasses, no interaction, and unknown diagonal field of view) to watch age-appropriate cartoons. These findings suggest that a low-cost system could be enough to produce an analgesic effect, at least for younger children. Moreover, in some circumstances, high-quality systems should not be recommended due to the characteristics of the procedure or specific limitations connected with the clinical environment. For example, patients undergoing dental procedures need to remain still, and a head-tracking system is not recommended because they should move their heads to interact with the system. The ideal VR system should let patients be isolated from the real environment and have multimodal possibilities to be worn and to interact with the virtual scenario. This aspect had been partly considered by Hoffman et al. [13] who implemented a water-friendly VR system that can be used during underwater procedures, such as for the wound care for burn patients. However, this revised VR system has never been used with pediatric patients and is more expensive than its classic counterpart.
Regarding the software component, the most applied VR game for pain reduction is Snow World (www.vrpain.com), an ice scenario specifically created for burn pain management. A limited number of other VR environments were used for pain management among children and adolescents, but all of them were designed for burn patients [22] or were not projected for pain reduction [27, 34]. To date, no evidence in the literature has indicated VR objects and scenarios that are more suitable than others for promoting better analgesia. The only suggestion is that age-appropriate software without violence should be preferred for children. In the past, the realization of VR software was expensive, and the availability of serious games (defined by Michael and Chen [34] as “games that do not have entertainment, enjoyment, or fun as their primary purpose”) was limited. Currently, it is easier to buy cheap VR video games (created for pleasure and entertainment), which could also be applied to pain management, or to obtain serious video games, specifically designed for health [33]. More studies comparing different VR environments could help deepen the understanding of how VR analgesia could depend on the kind of VR scenario. Moreover, for some procedures, such as dental ones, images that generate a sensation that is not referred to a cold environment could be preferred.
Psychological aspects should also be considered in the applicability of VR analgesia. One of the most relevant differences between VR and a classic distraction technique is that VR isolates the user from the real environment and blocks the possibility to see and listen to what is happening around the person. Patients undergoing a painful procedure would therefore focus their attentional resources on a pleasant stimulus and avoid watching the procedure. However, wearing the helmet, the patients are also isolated from potentially supporting elements in the real environment that could help them cope with the painful procedure. Indeed, children deal with pain by using different kinds of strategies; some children seek support from their parents during medical procedures, while other patients prefer to maintain their control of the environment rather than be distracted [36]. For patients who require social support or for those who prefer watching the procedure, VR distraction could produce a low analgesic effect, and in the worst case, it could also potentially generate an anxious and more painful experience. On the other hand, for patients who spontaneously use distraction to cope with pain, VR could be particularly indicated and efficient to control their pain. The literature has rarely investigated whether pain-coping strategies could influence the effectiveness of VR analgesia. Only one laboratory study reported that children’s coping style would not influence the VR efficacy and that this distraction technique was effective for children who reported both blunting and monitoring coping styles [37]. However, medical procedures are different from simulations in a laboratory setting and these results could in principle be disconfirmed in a clinical study performed during actually painful procedures.
The limitations regarding the applicability of VR distraction also include several contraindications, such as a diagnosis of epilepsy (because the use of VR could induce epileptic seizures) and physical or cognitive disabilities that could impede patients’ correct wearing of the helmet or interaction with the VR environment [8, 33]. According to these exclusion criteria, VR analgesia could not be usable by a large number of patients due to their diseases or the need to avoid hypothetical side effects. However, patients affected by different kinds of diseases and undergoing different procedures while distracted by VR did not report side effects in any of the studies [8]. Moreover, patients with intellectual disabilities should not be a priori excluded from the possibility to use VR analgesia. In fact, the effectiveness of VR for pain management involving this group of patients has never been investigated.
4 Clinical Applications of Virtual Reality: Our Italian Experience
The research on VR application is quite recent in Italy and has mostly focused on its use in psychotherapy [38, 39] and in training healthcare professionals [40] rather than on VR analgesia. The limited availability of VR systems and the difficulty to find VR head-mounted displays and software have probably made it difficult to introduce VR in Italian clinical settings. In recent years, VR systems have become available at reduced costs, and now, the user has the opportunity to choose among different kinds of VR goggles. However, high- and medium-quality helmets have only recently become accessible in Italy.
Thanks to the collaboration with Professor Hunter Hoffman, Director of the VR Analgesia Research Center at the Human Photonics Lab in the University of Washington, USA, and his collaborators, we recently obtained a VR system. We therefore started a research project aiming to evaluate the feasibility and the effectiveness of VR analgesia for pediatric and adolescent patients undergoing painful procedures in hospitals.
4.1 The Project
Introduction.
In our clinical experience, VR analgesia appears to be specifically indicated for pain management during venipuncture. Indeed, this common procedure is particularly fearful and painful for many children in hospitals, including those patients who need to repeat it due to their diseases [29, 41]. Moreover, in Piskorz et al. recent quasi-experimental study [42], VR analgesia emerged as an efficient distraction technique for pain management among patients undergoing blood draw in a pediatric nephrology clinic. Children distracted by VR reported significant lower levels of stress compared with the control group subjected to the no-distraction condition and a 59% reduction in pain intensity in the VR compared with the control group [42]. Our research group decided to promote the clinical use of VR analgesia at A. Meyer Children’s Hospital in Florence, Italy. Since 2014, we have introduced the use of VR distraction to the Service of Onco-hematology and the Service of Pediatric Nephrology, in collaboration with the Service of Pain Therapy and Palliative Care and the Department of Health Sciences, University of Florence.
Aim.
The project aims to explore the effectiveness of VR as a distraction technique for pain management among pediatric patients undergoing venipuncture and to promote the use of VR analgesia in clinical settings. According to the literature, we expect that patients distracted with VR will report lower levels of pain and will experience the procedure in a non-stressful manner, therefore reporting higher levels of fun in comparison with the control group.
Methods
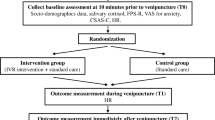
Study Design.
Patients undergoing venipuncture and availing of the Service of Onco-hematology at A. Meyer Children’s Hospital in Florence were recruited to participate in a study using a within-subjects randomized design. Patients undergoing venipuncture and availing of the Service of Nephrology were recruited to join a study using a between-subjects randomized design.
In both studies, the patients were selected with the help of a nurse of the hospital service, according to the following inclusion criteria based on the existent literature: children aged 7–17 years old, fluent in the Italian language, and without physical or psychological impediments to be able to use the VR system and complete the tests. Patients with a venous access already inserted in or with a port device, with a diagnosis of epilepsy, who were unaccompanied by parents, and who were over 17 years old or under 7 years old were excluded. Moreover, patients who wanted their own distraction tool (i.e., a book, a video game, or an MP3 player) during venipuncture in the control condition were excluded from the study.
Procedure.
The patients meeting the inclusion criteria were approached by a psychologist before the procedure in order to inform their families and obtain the informed consent forms signed by the patients’ caregivers. In the between-subjects design, the patients using the Service of Nephrology were randomly assigned to either the control group (No-VR), where they received the standard care pain management (non-medical conversation with the nurse) or the experimental group (Yes-VR), where they were distracted with VR. In the within-subjects design, the patients using the Service of Onco-hematology, who needed to undergo venipuncture twice a year, were assigned to either the control condition (non-medical conversation with the nurse) or the experimental condition (Yes-VR) and repeated the second venipuncture using the distraction technique (VR analgesia or non-medical conversation) that was not used the first time. In both designs, at the end of each procedure, the patients completed a self-report questionnaire to evaluate the quality of their VR experience, fun levels, and nausea.
Measures.
Pain levels, the quality of the VR experience, nausea, and fun were measured by using the Italian version of a self-report questionnaire adopted in previous international studies [8], based on the 0–10 graphic rating scale (GRS) [43]. Pain was evaluated in terms of its cognitive component (time spent thinking about pain), affective component (unpleasantness), and perceptive component (worst pain). The quality of the VR experience was investigated in terms of presence and the realism of VR objects.
The VR system. Our VR equipment consisted of a low-cost VR helmet and the Personal 3D Viewer Sony: HMZ T-2, supported by a laptop that allowed interaction with the VR environment. The helmet had a 45° diagonal field of view, with 1280 × 720 pixels per eye, and was suitable for both younger and older patients. The VR helmet had two miniature screens, one for each eye of the user, and latex-free earphones to provide acoustic isolation and promote escapism from reality. The VR software used was Snow World, one of the most frequently employed VR environments, specifically designed to promote distraction from procedural pain. In Snow World, patients virtually enter an icy canyon, where they throw snowballs at penguins, snowmen, and other characters in VR, using a wireless mouse with the hand that is not employed in the venipuncture.
4.2 Preliminary Results
In recent years, preliminary results have been presented in occasion of several national and international conferences regarding pain and the care of cancer patients [44]; however, the project is still ongoing.
Service of Onco-hematology
Eleven children suffering from cancer and blood diseases (7 males, 4 females; mean age = 10.64, SD = 2.58) underwent venipuncture twice. A t-test for paired samples was adopted to compare pain, nausea, and fun levels between the control and the experimental conditions. The patients reported significantly lower levels of pain unpleasantness and time spent thinking about pain while they underwent venipuncture plus VR analgesia (p < 0.05) compared with the group under the control condition, in which they were engaged in non-medical conversation by the nurse. Moreover, the children reported a “strong sense of going inside the computer-generated world” when interacting with VR and experienced significantly higher levels of fun compared with the group under the control condition (p < 0.05).
Service of Pediatric Nephrology.
The preliminary results were encouraging and followed the predicted direction. The nonparametric Mann–Whitney U test was adopted. Twelve patients (6 females and 6 females, mean age 12,25 years ±2,22) were distracted with VR and 12 patients (6 females and 6 males, mean age 10,42 years ±2,68) received the standard care during the venipuncture. The patients assigned to the experimental group reported significant lower levels of pain unpleasantness, and time spent thinking about pain (p < 0,05). No significant differences were noted for the levels of worst pain; however, the patients distracted by VR analgesia reported significantly higher levels of fun (p < 0.05) compared with their counterparts in the control group. The levels of nausea were negligible in both groups.
4.3 Discussion
This ongoing project represents a contribution to the growing literature that supports the effectiveness of VR as a distraction technique for pain management among children and adolescents. Our preliminary results highlight the huge potential of VR analgesia for pain management among children suffering from onco-hematological and kidney diseases as well. However, our sample, particularly in the study involving patients with kidney diseases, is still rather small. Future research with a larger sample is needed. VR analgesia has been positively evaluated by both the patients and the clinical staff of the hospital, who consider VR distraction a useful tool for pain and anxiety management. In one case, a male patient who used VR analgesia admitted that he had preferred watching the procedure; however, he reported high levels of fun and no pain during the venipuncture. This finding suggests that future studies should evaluate whether the desire to watch the procedure (and other pain-coping strategies) could influence the effectiveness of VR analgesia.
5 Conclusions and Future Perspectives
According to the literature and our clinical experience, VR has immense potential as a distraction technique and can be a useful non-pharmacological analgesic for children’s pain management. VR analgesia can help patients experience lower levels of pain and cope with the medical procedure in a non-stressful and safe manner, without side effects. However, more studies are needed to explore in depth the effectiveness of VR during several kinds of procedures and for different types of patients. For example, no study has evaluated the applicability of VR analgesia to patients with special needs or cognitive disabilities. Moreover, little is known about how psychological variables can influence the effectiveness of VR for pain management. Presence plays a central role in the quality of the experience in the VR environment; however, the relationship between presence levels and pain reduction by using VR has not been completely clarified. The analgesic effect of VR could also depend on the patient’s wish and capability to be isolated from the real environment. In principle, not all children could benefit from the isolation in a virtual world during a painful procedure.
The drop in the prices of VR systems has facilitated the diffusion of medium/high-quality VR helmets; however, specific VR software developed for children’s pain management are still rare. In future studies, different VR scenarios should be considered to evaluate whether specific environments could be preferable to others in order to improve the effectiveness of VR analgesia. Moreover, lightweight and wireless VR helmets should be developed for an easier application in a clinical setting with pediatric patients. Future research could also evaluate how the presence of more users in the same VR environment could improve the analgesic effect of VR. Indeed, a multiplayer software could help patients be isolated from the painful context, but at the same time, the social support of other VR players could improve the analgesic effect of VR. This solution could be particularly useful for those patients who use social support strategies to cope with painful procedures.
With respect to the Italian context, there is the need to improve the knowledge about VR analgesia among physicians, nurses, and clinical psychologists and to encourage research in this field in order to extend the use of VR distraction for pain management in clinical settings.
References
Heinemann, D.S.: Porting game studies research to virtual reality. New Media Soc. 18, 2793–2799 (2016)
Eccleston, C., Crombez, G.: Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychol. Bull. 125, 356–366 (1999)
Caprilli, S., Anastasi, F., Lauro Grotto, R., Scollo Abeti, M., Messeri, A.: Interactive music as a treatment for pain and distress in children during venipuncture: a randomized prospective study. J. Dev. Behav. Pediatr. 28, 399–403 (2007)
Koller, D., Goldman, R.D.: Distraction techniques for children undergoing procedures: a critical review of pediatric research. J. Pediatr. Nurs. 27, 652–681 (2012)
Birnie, K.A., Noel, M., Parker, J.A., Chambers, C.T., Uman, L.S., Kisely, S.R., McGrath, P.J.: Systematic review and meta-analysis of distraction and hypnosis for needle-related pain and distress in children and adolescents. J. Pediatr. Psychol. 39(8), 783–808 (2014)
Vagnoli, L., Caprilli, S., Vernucci, C., Zagni, S., Mugnai, F., Messeri, A.: Can presence of a dog reduce pain and distress in children during venipuncture? Pain Manag. Nurs. 16, 89–95 (2015)
Rezai, M.S., Goudarzian, A.H., Jafari-Koulaee, A., Bagheri-Nesami, M.: The effect of distraction techniques on the pain of venipuncture in children: a systematic review. J. Pediatr. Rev. 5(1), e9459 (2017). https://doi.org/10.17795/jpr-9459
Atzori, B., Hoffman, H.G., Vagnoli, L., Messeri, A., Lauro-Grotto, R.: Virtual reality as distraction technique for pain management in children and adolescents. In: Khosrow-Pour, M.: Encyclopedia of Information Science and Technology, 4th edn., Hershey, pp. 5955–5965 (2017)
Lee, K.M.: Presence, explicated. Commun. Theor. 14(1), 27–50 (2004)
Bulu, S.T.: Place presence, social presence, co-presence, and satisfaction in virtual worlds. Comput. Educ. 58, 154–161 (2012)
Slater, M., Wilbur, S.: A framework for immersive virtual environment (FIVE): speculations on the role of presence in virtual environments (1997)
Hoffman, H.G., Seibel, E.J., Richards, T.L., Furness III, T.A., Patterson, D.R., Sharar, S.R.: Virtual reality helmet display quality influences the magnitude of virtual reality analgesia. J. Pain 7, 843–850 (2006)
Hoffman, H.G., Sharar, S.R., Coda, B., Everett, J.J., Ciol, M., Richards, T., Patterson, D.R.: Manipulating presence influences the magnitude of virtual reality analgesia. Pain 111, 162–168 (2004)
Chan, E.A., Chung, J., Wong, T., Lien, A., Yang, J.Y.: Application of a virtual reality prototype for pain relief of pediatric burn in Taiwan. J. Clin. Nurs. 16, 786–793 (2007)
Sharar, S.R., Carrougher, G.J., Nakamura, D., Hoffman, H.G., Blough, D.K., Patterson, D.R.: Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: preliminary results from 3 ongoing studies. Archiv. Phys. Med. Rehab. 88, S43–S49 (2007)
Triberti, S., Repetto, C., Riva, G.: Psychological factors influencing the effectiveness of virtual reality–based analgesia: a systematic review. Cyberpsychol. Behav. Soc. Netw. 17(6), 335–345 (2014)
Swindells, C., Po, B.A., Hajshirmohammadi, I., Corrie, B., Dill, J.C., Fisher, B.D., Kellogs, S.B.: Comparing CAVE, wall, and desktop displays for navigation and wayfinding in complex 3D models. In: Proceedings of Computer Graphics International, pp. 420–427. IEEE, New York (2004)
Santos, B.S., Dias, P., Pimentel, A., Baggerman, J.W., Ferreira, C., Silva, S., Madeira, J.: Head-mounted display versus desktop for 3D navigation in virtual reality: a user study. Multimed. Tools Appl. 4, 161–181 (2009)
Pallavicini, F., Ferrari, A., Zini, A., Garcea, G., Zanacchi, A., Barone, G., Mantovani, F.: What distinguishes a traditional gaming experience from one in virtual reality? An exploratory study. In: Ahram, T., Falcão, C. (eds.) AHFE 2017. AISC, vol. 608, pp. 225–231. Springer, Cham (2018). https://doi.org/10.1007/978-3-319-60639-2_23
Hoffman, H.G., Doctor, J.N., Patterson, D.R., Carrougher, G.J., Furness III, T.A.: Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain 85, 305–309 (2000)
Gershon, J., Zimand, E., Pickering, M., Rothbaum, B.O., Hodges, L.: A pilot and feasibility study of virtual reality as a distraction for children with cancer. J. Am. Acad. Child Adolesc. Psychiatr. 43, 1243–1249 (2004)
Hua, Y., Qiu, R., Yao, W., Zhang, Q., Chen, X.: The effect of virtual reality distraction on pain relief during dressing changes in children with chronic wounds on lower limbs. Pain Manag. Nurs. 16(5), 685–691 (2015)
Van Twillert, B., Bremer, M., Faber, A.W.: Computer-generated virtual reality to control pain and anxiety in pediatric and adult burn patients during wound dressing changes. J. Burn Care Res. 28, 694–702 (2007)
Wender, R., Hoffman, H.G., Hunner, H.H., Seibel, E.J., Patterson, D.R., Sharar, S.R.: Interactivity influences the magnitude of virtual reality analgesia. J. Cybertherapy Rehab. 2, 27–33 (2009)
Ploghaus, A., Narain, C., Beckamm, C.F., Clare, S., Bantik, S., Wise, R., Matthews, P.M., Rawlins, J.N.P., Tracey, I.: Exacerbation of pain by anxiety is associated with activity of hippocampal network. J. Neurosci. 21, 9896–9903 (2001)
Jeffs, D., Dorman, D., Brown, S., Files, A., Graves, T., Kirk, E., Meredit-Neve, S., Danders, J., White, B., Swearingen, C.: Effect of virtual reality on adolescent pain during wound care. J. Burn Care Res. 35, 395–407 (2014)
Gold, J.I., Kim, S.H., Kant, A.J., Joseph, M.H., Rizzo, A.: Effectiveness of virtual reality for pediatric pain distraction during IV placement. Cyberpsychol. Behav. 9, 207–212 (2006)
Sander Wint, S., Eshelman, D., Steele, J., Guzzetta, C.E.: Effects of distraction using virtual reality glasses during lumbar punctures in adolescents with cancer. Oncol. Nurs. Forum 29, E8–E15 (2002)
Caprilli, S.: I bambini non devono provare dolore. Giornale Italiano di Scienze Infermieristiche e Pediatriche 2, 44 (2010)
Wolitzky, K., Fivush, R., Zimand, L.H., Hodges, L., Rothbaum, B.O.: Effectiveness of virtual reality distraction during a painful medical procedure in pediatric oncology patients. Psychol. Health 20, 817–824 (2005)
Guelman, M.: Dental fear in children may be related to previous pain experience during dental treatment. J. Evid. Based Dent. Pract. 5(3), 143–144 (2005)
Shahrbanian, S., Ma, X., Aghaei, N., Korner-Bitensky, N., Moshiri, K., Simmonds, M.J.: Use of virtual reality (immersive vs. non immersive) for pain management in children and adults: a systematic review of evidence from randomized controlled trials. Eur. J. Exp. Biol. 2, 1408–1422 (2012)
Won, A.S., Bailey, J., Bailenson, J., Tataru, C., Yoon, I.A., Golianu, B.: Immersive virtual reality for pediatric pain. Children 4(7), 52 (2017). https://doi.org/10.3390/children4070052
Michael, D., Chen, S.: Serious games: games that educate, train, and inform. Thomson Course Technology, Boston (2006)
Aminabadi, N.A., Erfanparast, L., Sohrabi, A., Oskouei, S.G., Naghili, A.: The impact of virtual reality distraction on pain and anxiety during dental treatment in 4–6 year-old children: a randomized controlled clinical trial. J. Dent. Res. Dent. Clin. Dent. Prospects 6, 117–124 (2012)
Axia, G., Bonichini, S.: La valutazione delle strategie di coping al dolore fisico nei bambini di età scolare. Psicologia Clinica dello Sviluppo 1, 97–123 (2000)
Sil, S., Dahlquist, L.M., Thompson, C., Hahn, A., Herbert, L., Wohlheiter, K., Horn, S.: The effects of coping style on virtual reality enhanced videogame distraction in children undergoing cold pressor pain. J. Behav. Med. 6(4), 117–124 (2012)
Riva, G., Bacchetta, M., Baruffi, M., Rinaldi, S., Molinari, E.: Virtual reality based experiential cognitive treatment of anorexia nervosa. J. Behav. Ther. Exp. Psychiatr. 30(3), 221–230 (1999)
Riva, G.: Virtual reality: an experiential tool for clinical psychology. Br. J. Guid. Counc. 37(3), 335–343 (2009)
Mantovani, F., Castelnuovo, G., Gaggioli, A., Riva, G.: Virtual reality training for health-care professionals. Cyberpsychol. Behav. 6(4), 389–395 (2003)
Bisogni, S., Dini, C., Olivini, N., Ciofi, D., Giusti, F., Caprilli, S., Lopez, J.R.G., Festini, F.: Perception of venipuncture pain in children suffering from chronic diseases. BMC Res. Notes 7, 735–739 (2014)
Piskorz, J., Czub, M.: Effectiveness of a virtual reality intervention to minimize pediatric stress and pain intensity during venipuncture. J. Spec. Pediatr. Nurs. 23, e12201 (2018). https://doi.org/10.1111/jspn.12201
Gracely, R.H., McGrath, F., Dubner, R.: Ratio scales of sensory and affective verbal pain descriptors. Pain 5, 5–18 (1978)
Atzori, B., Hoffman, H.G., Vagnoli, L., Messeri, A., Alhalabi, W., Patterson, D., Lauro Grotto, R.: Virtual Reality pain management for children with onco-hematological diseases undergoing venipuncture. In: 18th International Psycho-oncology Society Congress, 17th–21st October 2016, Dublin, Ireland (2016)
Acknowledgments
A special thanks to the Cassa di Risparmio Foundation and the Association ATCRUP.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this paper
Cite this paper
Atzori, B., Vagnoli, L., Messeri, A., Lauro Grotto, R. (2018). Virtual Reality for Pain Management Among Children and Adolescents: Applicability in Clinical Settings and Limitations. In: Antona, M., Stephanidis, C. (eds) Universal Access in Human-Computer Interaction. Virtual, Augmented, and Intelligent Environments . UAHCI 2018. Lecture Notes in Computer Science(), vol 10908. Springer, Cham. https://doi.org/10.1007/978-3-319-92052-8_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-92052-8_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92051-1
Online ISBN: 978-3-319-92052-8
eBook Packages: Computer ScienceComputer Science (R0)