Abstract
Demographers and social epidemiologists have widely recognized that determinants of health operate on different levels. Among all of the relational networks, the family deserves a special place as it is the context where lifestyles and health-related behaviors are generally developed and shared. Using data from the Italian Health Interview Survey 2004/2005 for ages 18 and above, this chapter aims to provide an estimation of the magnitude of influence that the household has on self-perceived health, controlling for individual characteristics and the geographical context. We select three outcome variables to investigate perceived health: Physical Component Summary, Mental Component Summary, and poor Self-Rated Health. We develop an index of homogeneity within households and explore to what extent mutual influences of health perception exist within a household, resulting in a high resemblance of health for people living together, independent of or in addition to the effect of household covariates. Eventually, we try to gain a better understanding of the pathways through which these mutual influences are spread between people in the same household.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Demographers and social epidemiologists have widely recognized that determinants of health operate on different levels (Kawachi and Subramanian 2005). Hence, a true comprehensive analysis of population health must not look only at the individual, but must also include contextual characteristics. However, only a handful of studies to date have taken the multilevel structure of health determinants properly into account and, as a consequence, findings about the impact of context on population health are sparse and inconclusive.
Existing literature has shown that, over and beyond individual characteristics, contextual factors affecting health are related to two main aspects: area of residence, i.e. macro-level (Stafford and McCarthy 2006; Kunst et al. 2005) and social proximity, i.e. meso-level (Schor et al. 1987; Cardol et al. 2005; Van Minh et al. 2010). However, a limited number of studies on population health have formally made use of a hierarchical structure accounting for both geographical and relational levels (Subramanian et al. 2003; Ferrer et al. 2005). The geographical area of residence has been studied as being potentially responsible for exposure to environmental risk factors (Martuzzi et al. 2002; Biggeri et al. 2004; Pearce and Dorling 2006), economic deprivation (Kennedy et al. 1998; Subramanian et al. 2001), social conflicts (Kawachi et al. 1999), and, in some cases, uneven health care provision (Joumard et al. 2008; Jagger et al. 2008), thus demonstrating that all of these factors have some influence on health outcomes. Less investigated is the meso-level, which typically refers to the network of relations binding the individual to the people close to him/her in everyday life (Agneessens et al. 2006; Rivellini 2006). This social/relational network influences individuals in terms of group identity, cultural background, and social support.
Among all of the relational networks, the family deserves a special place as it is the context where lifestyles and health-related behaviors (e.g. prevention, timely access to care, adherence to treatment) are generally developed and shared. Members of the same family are often found to be similar in terms of health-related lifestyles (Rice et al. 1998), help-seeking behaviors (Cardol et al. 2005), and utilization of health services (Sepheri et al. 2008). Having similar behaviors also exposes family members to similar risks (or protective factors) for health, directly deriving from those behaviors. For example, in a family where prevention is a common practice, all members share the protective effect of timely medical check-ups. Conversely, in a family where nutrition style is unbalanced in favor of consumption of fatty foods, members will be more exposed to the risk of being obese, and in turn exposed to an increased risks of cardiovascular diseases. This kind of result has been consistently illustrated in the epidemiological literature (Johnson et al. 1965; Monden 2007; Merlo et al. 2012).
Furthermore, the family is the predominant setting for the inter-exchange of resources finalized to satisfy an individual’s needs and to attain wellbeing. In this perspective, the family has always played a key role in supporting its members in those specific critical periods of their lifetime when they need assistance. In short, family affects health in two main areas: the occurrence of illness and the assistance thereof. In literature, family is generally identified with the household, first because it makes it easier to define the boundaries of the concept of “family”, and second because it is reasonable to assume that co-residence makes all the presented hypotheses about behaviors and assistance more intense.
Household characteristics that have been investigated in the literature as predictors of individual health include the socio-economic level of the family, housing conditions, living arrangements, and the burden of care for a cohabiting ill-health member. All of these characteristics can, to some extent, exercise influence on health as “household factors” because they operate simultaneously on all cohabiting members of the family. However, particularly when perceived health is the outcome, another hypothesis must be taken into consideration: poor health of a member can, by itself, operate as a factor influencing the perceived health status of other members. In other words, mutual influences of health perception can exist within a household, resulting in a high resemblance of health status for people living together, independent of (or in addition to) the effect of household covariates.
Research that has dealt with household influences on health perception (Ferrer et al. 2005; Van Minh et al. 2010) has not provided clear explanations of the mechanisms through which these influences occur. However, it is reasonable to suppose that household influences tend to be stronger in those countries where family has a strong impact on individual choices, such as Southern European Countries. Paradoxically, to the best of our knowledge, no studies of household contribution on health perception have been carried out in Italy, which is one of these familialistic countries.
Objective
The specific objectives of this study are:
-
to provide an estimation of the magnitude of influence that the household has on self-perceived health, controlling for individual characteristics and the geographical context;
-
to gain a better understanding of the pathways through which the household affects the perceived health of its members.
The Italian Setting
Italy is characterized by several peculiarities concerning both its territorial profile and the role of the family in an ample set of demographic and social phenomena. As a consequence, both territory and family are frequently found to have a larger influence on socio-demographic outcomes than in other countries.
Those territorial factors affecting health are closely linked to the provision of health care facilities, which have undergone profound changes in Italy in the last decades. The Italian National Health Service is currently structured on three hierarchical levels: two levels of governance (State and Regions) and one level of management (Local Health Units). It is financed through public taxation and presents centralized control together with strong federalized organization. The central governance rules the system through the national health program: it defines the priorities and guarantees homogeneity in the basic levels of assistance. At the same time, decentralization promotes regional autonomy in establishing, financing and managing health care facilities. The Region operates through the Local Health Units in transforming the economic resources in public health service for their population.
This final structure of NHS is the result of a long process of decentralization, which began in 1995 and has led Regions to contribute to their health expenses through autonomous taxation and to increase (according to resources available) the number of health services. The entire process of reform has alimented a heated debate concerning the risk of territorial health inequality. The hypothetical scenario in which health expenditures are entirely financed by Regions, without any relevant national adjustment, has further increased concerns about health equity (Egidi and Reynaud 2005).
What has been empirically observed is the existence of sharp heterogeneity between Italian Regions in both social and economic terms. Such heterogeneity is reflected also in the availability and quality of health services and it becomes apparent when viewing typical indicators of quality of care. Thirty-day mortality after a stroke, for example, varies from about 7% in Bolzano (in the North, on the Austrian border) to almost 20% in Molise (in the South). The proportion of patients receiving coronary angioplasty within 48 h ranges from 15% in Marche, Molise, and Basilicata to 50% in Valle d’Aosta (in the extreme north west part of Italy). The same indicator at the Local Health Units level reveals even more profound differences (spanning 5–60%). The waiting time for surgery after a hip fracture is 3 days in Valle d’Aosta and 7 days in Molise and Campania (South). More general indicators, commonly used as a proxy for quality in primary care, are potentially avoidable medical admissions, i.e. those medical conditions which are deemed fully manageable in primary care. These include conditions such as childhood asthma, for which age- and sex-adjusted hospital admissions are lowest in Toscana (0.21 per 1000 population) and highest in Sicilia (0.95) according to the data from National Outcome Programme (OECD 2014).
These variations in health provision correspond to a strong variation in health satisfaction and health outcomes. The proportion of patients who were “very satisfied” with hospital care in 2009 was about 50% in Trentino-Alto Adige and 20% in Sicilia and Puglia. This gap is reflected in the substantial flows across regional borders of patients who opt to receive health care assistance in a region other than their own.
This geography difference in health care offer is largely confirmed when we look directly at health outcomes. Differences in mortality according to Italian Regions and provinces have been extensively documented (Caselli and Egidi 1979; Divino et al. 2009), with studies consistently reporting very clear spatial trends changing over time and with minor differences according to gender. Male mortality is significantly lower in the Northern regions (especially in the eastern part of the country) and higher in the Southern regions and the Islands, with differences only slightly lower than 3 years of life expectancy at birth between the more and less favored regions. Women follow the same general trend, while showing a relative disadvantage in the northwestern part of the country. Territorial differences can be observed also for health conditions: e.g. prevalence of multiple chronic conditions, disability rates, and disability-free life expectancy have sharp geographical variations which depict the traditional North–South gradient (Fig. 1 males and Fig. 1 females).
In terms of the familial perspective, Italy is well-known as a characteristically familialistic country. Extensive research has documented the strong role of family ties on demographic phenomena, such as fertility, leaving the parental home, and economic conditions (Cook and Fustenberg 2002; Tomassini et al. 2003; Vignoli and Matysiak 2013). The same effects can be hypothesized as extendable to health issue.
Despite the immediacy of this hypothesis, the subject is rarely ever taken into consideration for the Italian context. In the international literature marital status and patterns of family disruption have been extensively analyzed and proven to be remarkable predictors of health; however, the family as a whole and its role on health has not yet appeared in the health demographer’s agenda.
One exception is the number of emerging studies that deal with the burden of care-giving on family members (Ory et al. 2000; Bookwala and Schulz 2000; Vlachantoni 2010; Egidi et al. 2013), which present a picture of economic and health consequences of care-giving activities, in terms of wellbeing and labor market participation of carers (Vlachantoni 2010) or psychological stressors (Bookwala and Shulz 2000). In other cases, they evaluated more specifically the consequences on health for people living with a person affected by dementia (Ory et al. 2000; Egidi et al. 2013). These studies give proof of a non-negligible impact on self-perceived health especially for people in the youngest age groups, up to age 64, when the demand for care of the demented conflicts with familial and social roles; and for couples living alone, for which the burden of care is faced by a single person. This kind of effect can be particularly strong in countries, such as Italy, where the family plays a relevant and often exclusive role in terms of care and assistance of an ill member. Moreover, this family-based assistance is usually not supported by the National Health System and the family is therefore left alone in the care of its ill member, with only limited external support. This condition is especially hard on smaller families, e.g. elderly couples, or for specific kinds of pathologies, such as mental disorders.
Given this context, we expected family members to be strongly affected by the emerging of poor health in one of them.
Data and Methods
Data come from the Italian Health Interview Survey carried out by the National Statistical Office (Istat) in 2004/2005. The survey used a cluster sample design based on households and uses Aggregated Local Health Units (ALHU). AHLU are aggregations of contiguous Local Health Units according to demographic and health planning criteria. They constitute the territorial level of our analysis. The reason we selected ALHU as the most appropriate territorial aggregation is that these represent the minimal territorial units granting health care facilities for which statistical data are available.
According to the Italian definition, a household is a group of people cohabiting and related by marriage, kinship, adoption, or sentiment. Institutionalized people are therefore not included in the analysis, neither are people living together with no sentimental relationship (e.g. cohabiting formal caregivers). People living alone were also excluded from the analysis, as they did not fit the research objective of investigating the effects of household on health.
Data have a hierarchical structure defined as individuals (level 1) living in different households (level 2), which are, in turns, located in different ALHU (level 3). Because these data were collected as a cluster survey, it is important to note that when a household is sampled all the household members are surveyed.
In order to provide reliable estimations of perceived health we selected only those respondents aged 18 or older.
After sample selection we had 91,391 individuals who satisfied the eligibility criteria. These resided in about 36,000 households which were, in turn, grouped into 68 ALHU. The household dimensions ranged from 2 to 8 individuals, with an average of 2.5 people per household. We selected three outcome variables to investigate perceived health: Physical Component Summary—PCS, Mental Component Summary—MCS, and poor Self-Rated Health—poor SRH. The first two measures are quantitative assessments of physical and mental health, positively oriented (the higher the score the better the health) derived from the Short Form-12 Health Survey—SF-12 included in the Italian survey. SRH is a binary variable derived from the single-item question recommended by the World Health Organization (WHO), which asks: “How is your health in general?” (De Bruin et al. 1996). Answers are distributed on a five point scale: very good, good, fair, bad, very bad. We grouped these five categories into two, creating a dummy variable (poor-SRH) of people reporting “poor” and “very poor” health conditions as opposed to those reporting “fair”, “good” or “very good” conditions. This aggregation is due to the very unbalanced frequency distribution of respondents in the five categories: only a very small proportion of the population were in the two extreme categories (very good/very poor), which would have produced unreliable estimations. The choice of aggregating the category “fair” together with the positive modalities (“good” and “very good”) is due to its Italian translation, which has a quite positive, rather than a neutral, connotation (Egidi and Spizzichino 2006).
We included individual and contextual (household) covariates in the analyses. As individual variables, we consider age, classified as <50, 50–64, 65–74, 75+; gender; education (low, i.e. primary education or lower; medium, i.e. lower secondary; and high, upper secondary education or higher); disability (yes/no), according to the highest limitation grade in at least one item of OECD Long-Care Disability Questionnaire; and multichronicity (yes/no), defined as having three or more chronic illnesses diagnosed by a medical doctor. Finally, we created a new variable from the dataset intended to capture the burden of disability of one household member on the rest of the family. It is labeled cohabitation with disabled and has value one when the individual cohabits with at least one disabled person.
Household covariates include: perceived economic status with categories good/satisfactory versus inadequate; housing conditions, which is based on the presence of very basic housing problems (e.g. absence of heating) and is classified as Good (no problems), Fair (1–2 problems), or Bad (more than 2 problems); household size with categories 2–3; 4; 5+ components; household structure with couple-headed families opposed to single-headed families; and city size with two classes based on the threshold of 50,000 inhabitants.
We adopted a multilevel approach with which we are able to disentangle the proportion of variability on different levels, i.e. the variability between individuals due to differences between individual themselves or due to household or ALHU communalities. According to the outcome characteristics, we ran linear or logistic multilevel models, with random intercepts at the household and ALHU levels. For each of the three outcomes we ran different multilevel models:
-
Empty model: the model without any covariates, to evaluate the proportion of variance to be accounted for at each level, by means of the Variance Partition Coefficient (VPC).
-
Model with individual covariates: to estimate the VPC controlled for compositional effects (i.e. differences due to the unequal distribution of individuals in the groups).
-
Complete model: with individual and household covariates.
What remained as residual variance at the household level is the variation of perceived health between households not explained by all of those individual and household factors already included in the analysis. We should consider that the total variance is composed of the variability of individuals within the households (variance within) and the variability between households (variance between). Thus, the proportion of variance at the household level (\( VPC_{H} \)), as measured by the VPC, will result from:
and therefore it will be the highest, approaching 100%, when the variance within (\( \sigma_{I} \)) is equal to zero, i.e. when all individuals in the same household have exactly the same perceived health, and the whole variation is due to the variation between households (\( \sigma_{H} \)).
From this perspective one can easily understand how a high proportion of residual variance at the household level indirectly reflects a strong degree of health homogeneity within a household. The same formula is in fact used to calculate the Intraclass Correlation Coefficient (ICC), which is a measure of health homogeneity that expresses the correlation between two units randomly drawn from the same cluster (Snijders and Bosker 2012).
Finally, we looked at this health homogeneity as being responsible for the strong variation registered at the household level and advanced the hypothesis that mutual influences between household members play a major role in explaining this phenomenon. We tested this hypothesis with an analysis of health homogeneity by household structure, as we expected that the homogeneity would have been significantly different according to different typologies of households, where mutual influences have diverse magnitude.
Results
Descriptive Analyses
Whatever the measure adopted or the context of study, health is primarily affected by age. The proportion of poor-SRH ranges from 1.6% in the youngest group of people (under 50), to 27.8% in the oldest group (75 and over), and PCS and MCS scores range from 53.6 to 38.1 and from 51.0 to 45.6, on the same age interval. Looking at the range of variation of PCS and MCS, we also detect extremely large intervals between minimum and maximum values (Table 1), demonstrating the large heterogeneity in the health of the study population.
Multilevel Analysis
We run three nested models: the first one empty (i.e. with no covariates), the second with progressively individual covariates, and the third, which we refer to as a complete model, with individual and household covariates. We start by reporting the effects of individual and household covariates on the three health outcomes in the complete models, as illustrated in Table 2.
Objective health conditions, i.e. disability and multichronicity, have the strongest negative impact on perceived health as assessed by all three indicators. A negative effect can be detected for gender, with women having worse perceived health conditions, especially if we look at MCS, which expresses the mental/emotional dimension of health. Education also shows a negative health gradient from the highest to the lowest school attainment. Age presents a more complex relation with perceived health, with different impacts between physical and mental dimensions: for PCS and SRH ageing is correlated with health deterioration; for MCS the worst condition is observed for people aged 50–64, whereas being older appears to be a protective factor. Not surprisingly, living together with a disabled person affects the emotional/mental dimensions of perceived health with a remarked deterioration for MCS and SRH.
Regarding household covariates, we can see that characteristics related to economic conditions (resources and housing) are those that have an impact on all three outcomes. Household size and structure impact more on MCS than PCS, with people living in larger, couple-headed households being more protected from poor mental health. Conversely, the dimension of the city is positively associated with better perceived physical health, whereas it shows no significant relationship to perceived mental health. Poor-SRH seems to be a synthesis of the other two indicators, as it is associated with all of the covariates included in the model, and in some cases (e.g. household size) with a clearer trend than the quantitative outcomes.
We then looked at the proportion of variability of health perception existing on the three levels of analysis (AHLU, Households, Individuals) as measured by the Variance Partition Coefficient reported in Table 3.
On the one hand, we documented a very limited, although always significant, impact of AHLU of residence of individuals on their self-perceived health (0.3% for PCS, 0.6% for MCS, and 2.3% for poor-SRH) net from the effect of individual characteristics. Although we observed this very small influence of ALHU on health, we retained this geographical level in all subsequent analyses in order to control for the effect of territorial differences in health care facilities on health perception.
On the other hand, in the same models, the relevance of household on perceived health was quite substantive. The 14.7% of variability in PCS was a result of household differences, and MCS and poor-SRH show an even greater impact with, respectively, 32.5 and 38% of variability attributable to the household level (Table 2).
Characteristics of the household show a very weak impact on PCS (unexplained variability decreases from 14.7 to 14.3%) and only a slightly higher impact on MCS (from 32.5 to 31.5%). For poor-SRH, household covariates play a more important role (explaining an additional 5% of the variability between households). However, when all available covariates are controlled for, wide shares of SRH and MCS variability remain unexplained (34 and 32%, respectively).Footnote 1
Seeking an explanation, we formulated the hypothesis that mutual influences between family members may play a major role. We hypothesized that this health homogeneity was due to mutual influences in health perception between family members, rather than exogenous factors operating on the household as a whole. It was not possible to test this hypothesis directly, therefore we designed an indirect strategy to check indirectly the robustness of the mutual influences hypothesis.
Our idea was that the hypothesis could be investigated indirectly by comparing the health status of individuals living in households of different sizes and structures. In fact, mutual influences should be different according to the tightness of links between household members: Where the link between members is expected to be tighter (two components, marriage-like link, mono-nucleus families) we should find also higher levels of health homogeneity.
Reciprocal Influences on Health: Evidence from the Household-Structure Analysis
We considered three main dimensions for defining the different kinds of family structures:
-
household size: as it shapes the strength of the ties and determines the degree to which problems, burdens, and mutual influences are shared by the cohabiting members of the household;
-
family ties: as understanding, affinity, and empathy vary greatly according to the type of familial relationship. The husband-wife relationship is expected to have a larger extent of reciprocal influence than the brother-sister relationship;
-
duration of the relationships: as the emotional closeness between people is stronger according to the length of life span spent together, especially if they are a couple. Having no direct information about the relationship duration we use age as a proxy, using the age of 50 as the threshold.
In the following we verify whether the perceived health homogeneity between family members is coherent with these expectations. Health homogeneity at the household level is estimated as the Intra-class Correlation Coefficient (ICC%) at the household level. We compared specific subgroups (e.g. household composed of only two components, couples with or without children, multi-nucleus families) and we always applied the full model, in order to obtain estimations of homogeneity adjusted for territorial effects and for all individual and household observed covariates. As health measurements we use only PCS and MCS as we need robust estimation of the variability components.
Because we analyzed health resemblance only for people older than 18 years, when we analyze the household size we consider only those families where all members were older than 18. Families with children younger than 18 years are treated separately.
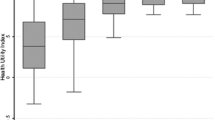
As expected, Fig. 2 shows that for both PCS and MCS the homogeneity is significantly higher in two-component households than in families with three or more cohabiting people. Moreover, homogeneity is higher for MCS, the indicator more sensitive to emotional influence, than for PCS.
The influence of household size on the level of homogeneity (i.e. the larger the groups the higher the probability of finding high variance) was evaluated by isolating the 2-component households and looking at the health homogeneity by family tie and duration of the relation (using age as a proxy). Our hypothesis was that homogeneity is highest for couples in a long-lasting relationship.
The hypothesis is entirely confirmed for PCS for which couples older than 50 have the highest level of homogeneity (25.1%), while their non-coupled peers have significantly lower homogeneity (11.4%) as well as young couples (14.6%) as clearly depicted in Fig. 3. People younger than 50 not in a couple were too small a group to produce reliable results.
For MCS homogeneity is not a matter of age/union duration, rather it depends on the type of relation between the two members: People in a couple have homogeneity over 36%, despite their age, while people not in a couple always have significantly lower levels of homogeneity (28.9% if younger than 50, 30% if older).
Focusing on couples, with and without children, our hypothesis was that the highest level of homogeneity characterizes couples without children, while it is expected to be weaker for couples with children because the ties are less tight and the network of relations wider. The duration of the link (once again approximated by the age of the individuals) should have the same effects as hypothesized before.
In the category “couple + children”, children themselves are included in the analysis of health resemblance if they are older than 18, whereas in the category “spouses in household with children” only the two partners are considered in the estimation of the homogeneity, regardless of the age of children. Our hypothesis is once again verified for PCS when we look at people over 50, while no differences are detectable for people younger than 50 (Fig. 4). This is not surprising, as in the young age group the PCS generally indicates good health and exhibits very limited variation.
For MCS, couples without children have the highest homogeneity, and this is significantly higher than that of couples with children. This result is independent of the partners’ age: the homogeneity differential between couples with and without children is about 6–7% points both for older couples (37% vs. 30%) and for younger couples (41% vs. 35%). However, if we select only the two spouses from families with children, their level of resemblance is not statistically different than that of the level of childless couples, as the confidence intervals overlap.
Households with three or more components exhibit a wide range of different structures, which we grouped into four broad categories: (1) couple without children and with aggregated members (couple + aggregated) which consist of the main family nucleous (couple) together with one or more isolated relatives not constituing a second family; (2) couple with adult children (couple + children); (3) single parent with adult children (single parent + children); (4) households with more than one family unit (multinuclear households). Once again we expect different levels of homogeneity corresponding to different tightness of the links between members. More precisely our hypotheses are:
-
mono-nuclear households will exhibit higher homogeneity than multi-nuclear ones (hypothesis 1);
-
among multi-nuclear households couples with adult children will have higher homogeneity than couples with aggregated members (hypothesis 2).
For single parent families with adult children two different hypotheses can be formulated:
-
they may have lower homogeneity than families headed by a couple due to the absence of the two partners (hypothesis 3) or a mechanism of compensation could take place. In this case the link (and mutual influences) between the single-parent and the offspring could become stronger as a response to the absence of a member of the couple. If this is the case, the homogeneity in a single-parent household would not differ significantly from that of couples with children (hypothesis 4). Hypothesis 3 and hypothesis 4 are alternatives. However, they both appeared to be theoretically reasonable, therefore we kept both and tested empirically which one prevails.
As Fig. 5 shows, hypothesis 2 and 3 are confirmed by PCS: couples with children have a higher resemblance than couples with aggregated members and much higher similarity than one-parent households. Non-nuclear households do not exhibit a level of homogeneity significantly different from the other groups according to PCS.
The picture given by MCS is entirely different: homogeneity is highest for households with adult children, despite the number of co-living parents (hypothesis 4). When the household comprises a couple (without children) living with relatives, the household members exhibit very different MCS, with significantly less resemblance than parents and children. People living in multinuclear households are the most heterogeneous group, confirming hypothesis 1.
Discussion
Heath is influenced not only by individual characteristics and behaviors but also by the different contexts in which the person lives. Of all of these contexts, our interest is focused on the role played by the family, which we defined as based on cohabitation. According to this definition we investigated the effects of household on health, after adjustment for available individual covariates, including age, gender, education, and objective health conditions.
In considering quantitative and qualitative perceived health outcomes, we were able to cross-validate the results, particularly those estimated for poor SRH, which could be affected by limitations related to the binary nature of the outcome. We documented an effect of household on health that ranges from 15 to 38% according to the health indicator in use.
We tried to corroborate this interpretation through an international comparison of household effects in contexts with different characteristics in terms of family role and health policy. Such a comparison is not easy, as to date only a handful of studies have looked at the issue of households influences on health, and across these studies the health outcome, the target population, and the country characteristics vary largely. Working on all-cause mortality in Sweden, Merlo et al. (2012) reported 18.6% of variability at the household level. Subramanian et al. (2003) found a very large effect of households on poor self-rated health in Chile (VPC of 47%), however they made use solely of the binary indicator (SRH). Van Minh et al. (2010) reported a share of only 15% of perceived good health variability among Vietnamese people over 50 which, however, is a different outcome and cannot simply be seen as the other side of the coin of our outcome (Benyamini et al. 2003; Kaplan and Baron-Epel 2003; Schüz et al. 2011). The only study concerning a developed country is based in the USA (Ferrer et al. 2005) and revealed a maximum variability share attributable to the family context of 9.9% for PCS and 15.4% for MCS, controlled for individual covariates The authors used census families, which include all persons related to the household’s head by blood or marriage, disregarding the co-residence requisite. This can partially explain the lower effect of family on health with respect to our findings.
We made a further step towards a better understanding of the household effect by introducing family-covariates (i.e. a household’s economic resources, size, and typology of household structure together with the size of the municipality of residence); however, we found that residual variance between households did not decrease substantially, i.e. these variables did not explain the difference in health between households. Aware of the strict dependence of variance between units at a higher level from the homogeneity of units within the groups themselves, we looked at the levels of homogeneity within households, and from this perspective we advanced the hypothesis that a major role can be played by mutual influences between members of the households, rather than exogenous factors. Actually, people living in the same households can have similar individual health determinants, such as nutritional choices, prevention attitude, health-seeking behavior, or health care utilization, which derive from a shared familial approach to health and care. These communalities can partially explain our results. However, there is another interpretation of mutual influences we found more stimulating and consistent with our data: the perceived health of one person can be directly affected by the perceived health of people living in the same household, especially in case of poor health. In this situation we observe mutual influences not related to similar determinants but related to the outcome itself, as happens when specific diseases or conditions affect household members asking for care from other members and altering their emotional status and subjective health (Egidi et al. 2013).
We expected these mutual influences to be of particular relevance in the Italian context, where the tightness of the links between family components and the limited support provided by the welfare state for the care of severe illnesses could emphasize the effects of “contagion” of poor health status.
It was not possible to test this hypothesis conclusively from our data; however, the analysis of homogeneity according to household structure did produce some insights in this direction. The effects of households were especially pronounced for small families and within couples.
In all, the results of homogeneity by household structure show a very clear pattern for 2-component households, while they appear more articulated when the household size increases. These results are in line with findings in social psychology, which have consistently documented a similarity in mental illness, depressive symptoms, and distress between spouses (Meyler et al. 2007; Monden 2007), and with those in sociology reporting a positive effect of partner interactions on well-being, happiness, and life satisfaction (Horwitz et al. 1998). We also documented that as the couples got older their concordance increases, which had already been noticed in studies of clinical medicine (Cheraskin et al. 1968; Johnson et al. 1965).
Furthermore, the family constellation has already been taken into consideration in relation to life satisfaction and well-being, suggesting that family structure and relations between family members are among the most important determinants of life satisfaction (Evans and Kelly 2004; Vignoli et al. 2012). Interpersonal relationships and social supports heavily shape an individual’s well-being. and the most detailed investigation revealed that the effects of social support on well-being vary depending on family structure and the person providing support. We expand this framework by hypothesizing that similar mechanisms are at play when individuals rate their health. The very limited role played by the geographical context on individual perceived health was rather unexpected based on previous work illustrating a health gradient for both objective and subjective health in Italy (Costa et al. 2003; Mazzuco 2009). However, research that adopted a multilevel approach to investigate the Italian Regional and ALHU heterogeneity came to the same conclusion as we did, recognizing a proportion of variability at the ALHU level less than 3% for poor self-perceived health (Pirani and Salvini 2012).
There are also some limitations to our study, the most important of which is due to the cross-sectional nature of our data preventing us from controlling for a possible selection effect in household composition and examining the “dynamic” of mutual influences. Analyses of longitudinal data could provide valuable information about how mutual influences on health take place, particularly whether deterioration in the health perception of one member worsens the health perception of others and how long it takes for this influence to occur. These kinds of mechanisms are especially interesting when we explore health contagion from a gendered perspective. Italy, like other southern European countries, has a remarkable gender role differentiation, especially for older cohorts. Not only does this differentiation have effects on health outcomes per se, but it also determines that some typologies of activities, among which are the assistance of an ill family member, are strongly assigned to women within the families.
This asymmetry of gender roles within the family can affect the intensity and direction of the health influence between members. For example, we could expect the “contagion” of poor health to be stronger from men to women, because in the traditional family it is the woman who is requested to provide assistance and to take on the burden of her partner’s disease. However, we could also expect the opposite: because the woman is used to this role of care-giver she would cope better with poor health of her partner than her partner would cope with hers.
Unfortunately, to better understand these mechanisms, longitudinal data are necessary because only if we look at temporal changes can we observe the direction of health influences; i.e. if the man or the woman worsen his/her health first and then affects the others.
Moreover, our data do not allow us to control for psychological variables, such as the personality traits of the household’s members, and health related behaviors, which are often shared by family members. In conjunction with the selection effect for couples (assortative mating), these aspects could explain our results about health homogeneity, at least partially. However, while putting into question the primacy of the mutual influence hypothesis in explaining perceived health homogeneity inside households, these limitations do not detract from the importance played by the household context on members’ health.
Conclusions
This research provides insights on the extent and the ways in which contextual factors shape subjective health. Within this general aim, we document three more specific results: (1) the geographical effect on health, examined by means of a multilevel approach, is dramatically resized compared to previous studies of the Italian case which used an ecological perspective; (2) household appears as a key-element in influencing the perceived health of individuals, with a clear gradient from physical to mental component; (3) the mechanism of the household effect on perceived health can reasonably rely on the reciprocal influences between family members.
When poor health enters into the family, even if solidarity is activated to cope with the need of the family member in poor health, cohabitation and emotional ties seem to act as a multiplier of poor health conditions, negatively altering the perceived health status of all family members. Health policies, traditionally targeted at single individuals, probably have positive effects that go far beyond the single recipient of the intervention. In fact, maintaining an individual in good health (and in good health perception) means that all of his/her family is protected from the process of health deterioration that could occur as a consequence of mutual influences on health. In this perspective, current evaluations of the benefits of social/health interventions are consistently underestimated, as we overlook the positive externalities that each intervention has also on the family of the targeted recipient.
Notes
- 1.
The value of the SRH variability, which could be overestimated due to the small cluster sizes, is perfectly in line with the value for MCS. Although we need to be cautious in interpreting the variance of SRH between households, the resemblance of this value with the correspondent value for MCS is a cross validation for the results of the binary outcome.
References
Agnessens, F., Waege, H., & Lievens, J. (2006). Diversity in social support by role relations: a typology. Social Networks, 28, 427–441.
Benyamini, Y., Leventhal, E. A., & Leventhal, H. (2003). Elderly people’s rating of the importance of health-related factors to their self-assessments of health. Social Science and Medicine, 56, 1661–1667.
Biggeri, A., Pasetto, R., Belli, S., Bruno, C., Di Maria, G., Mastrantonio, M., et al. (2004). Mortality from chronic obstructive pulmonary disease and pleural mesothelioma in an area contaminated by natural fiber (fluoro-edenite). Scandinavian Journal of Work Environment and Health, 30(3), 249–252.
Bookwala, J., & Schulz, R. (2000). A comparison of primary stressors, secondary stressors, and depressive symptoms between elderly caregiving husbands and wives: the caregiver health effects study. Psychology and Aging, 15(4), 607–616.
Caselli, G., & Egidi, V. (1979). La geographie de la mortalite italienne: differences territoriales et milieu. Genus, 35(1/2), 101–153.
Cardol, M., Groenewegen, P. P., de Bakker, D. H., Spreeuwenberg, P., van Dijk, L., & van den Bosch, W. (2005). Shared help seeking behavior within families: A retrospective cohort study. British Medical Journal, 330(7496), 882.
Cheraskin, E., Ringsdorf, W. M., Setyaadmadja, A. T. S. H., Barrett, R. A., Sibley, G. T., & Reid, R. W. (1968). Environmental factors in blood glucose regulation. Journal of the American Geriatrics Society, 16, 823–825.
Cook, T. D., & Furstenberg, F. F. (2002). Explaining aspects of the transition to adulthood in Italy Sweden, Germany, and the United States: A cross-disciplinary, case synthesis approach. The ANNALS of the American Academy of Political and Social Science, 580, 257–287.
Costa, G., Marinacci, C., Caiazzo, A., & Spadea, T. (2003). Individual and contextual determinants of inequalities in health: The Italian case. International Journal of Health Services, 33(4), 635–667.
De Bruin, A., Picavet, H. S. J., & Nossikov, A. (1996). Health interview surveys (p. 58). European Series: Towards International Harmonization of Methods and Instruments, WHO Regional Publications.
Divino, F., Egidi, V., & Salvatore, M. A. (2009). Geographical mortality patterns in Italy: A bayesian analysis. Demographic Research, 20(18), 432–466.
Egidi, V., & Reynaud, C. (2005). Le politiche sanitarie nell’Italia del dopoguerra. Popolazione e storia, 1, 45–85.
Egidi, V., & Spizzichino, D. (2006). Perceived health and mortality: A multidimensional analysis of ECHP Italian data. Genus, LXII(3–4).
Egidi, V., Salvatore, M. A., Gargiulo, L., Iannucci, L., Sebastiani, G., & Tinto, A. (2013). Dementia in the elderly: Health consequences on household members. In N. Torelli, F. Pesarin, & A. Bar-Hen (Eds.), Advances in theoretical and applied statistics. Berlin Heidelberg: Springer-Verlag.
Evans, M. D. R., & Kelly, J. (2004). Effects of family structure on life satisfaction: Australian evidence. Melbourne, Vic: Melbourne Institute of Applied Economic and Social Research, University of Melbourne.
Ferrer, R. L., Palmer, R., & Burge, S. (2005). The family contribution to health status: A population-level estimate. Annals of Family Medicine., 3(2), 102–108.
Horwitz, A. V., McLaughlin, J., & Raskin White, H. (1998). How the negative and positive aspects of partner relationships affect the mental health of young married people. Journal of Health and Social Behavior, 39(2), 124–136.
Jagger. C., Gillies, C., Moscone, F., Cambois, E., Van Oyen, H., & Nusselder, W., et al.(2008). Inequalities in healthy life expectancies in EU25: A cross-national meta-regression analysis. The Lancet, 9656(372), 2124–2131.
Johnson, B. C., Epstein, F. H., & Kjelsberg, M. O. (1965). Distributions and familial studies of blood pressure and serum cholesterol levels in a total community—Tecumseh, Michigan. Journal of Chronic Diseases, 18, 147–160.
Joumard, I., André, C., Nicq, C., & Chatal, O. (2008). Health status determinants: Lifestyle, environment, health care resources and efficiency. OECD Economics Department Working Papers, 627 (OECD Publishing).
Kaplan, G., & Baron-Epel, O. (2003). What lies behind the subjective evaluation of health status? Social Science and Medicine, 56, 1669–1676.
Kawachi, I., & Subramanian, S. V., (2005). Health demography. In Poston & Micklin (Eds.), Handbook of population—handbooks of sociology and social research (pp. 787–808). Springer.
Kawachi, I., Kennedy, B. P., & Glass, R. (1999). Social capital and self-rated health: A contextual analysis. American Journal of Public Health, 89(8), 1187–1193.
Kennedy, B. P., Kawachi, I., Glass, R., & Prothrow-Stith, D. (1998). Income distribution, socioeconomic status, and self-rated health in the United States: Multilevel analysis. British Medical Journal, 317, 917–921.
Kunst, A. E., Bos, V., Lahelma, E., Bartley, M., Lissau, I., Regidor, E., et al. (2005). Trends in socio-economic inequalities in self-assessed health in 10 European countries. International Journal of Epidemiology, 34(2), 295–305.
Martuzzi, M., Mitis, F., Biggeri, A., Terracini, B., & Bertollini, R. (2002). Ambiente e stato di salute nella popolazione delle aree ad alto rischio di crisi ambientale in Italia [Environment and health status of the population in areas with high risk of environmental crisis in Italy]. Epidemiologia e Prevenzione, 26(6), 1–53.
Mazzuco, S. (2009). Condizioni di salute nelle Regioni Italiane. In F. Ongaro & S. Salvini (Eds.), Rapporto sulla popolazione—Salute e sopravvivenza. Bologna: Gruppo di Coordinamento per la Demografia, Il Mulino.
Merlo, J., Viciana-Fernandez, F. J., & Ramiro-Farinas, D., Research Group of Longitudinal Database of Andalusian P. (2012). Bringing the individual back to small-area variation studies: A multilevel analysis of all-cause mortality in Andalusia, Spain. Social Science and Medicine, 75, 1477–1487.
Meyler, D., Stimpson, J. T., & Peek, M. C. (2007). Health concordance within couples: A systematic review. Social Science and Medicine, 64, 2297–2310.
Monden, C. (2007). Partners in health? Exploring resemblance in health between partners in married and cohabiting couples. Sociology of Health & Illness, 29(3), 391–411.
Ory, M. G., Yee, J. L., Tennestedt, S. L., & Schulz, R. (2000). The extent and impact of dementia care: Unique challenges experienced by family caregivers. In Handbook on dementia caregiving: evidence-based interventions for family caregivers. New York: Richard Schulz editor.
OECD. (2014). OECD reviews of health care quality: Italy 2014: Raising standard. Italy: OECD Publishing.
Pearce, J., & Dorling, D. (2006). Increasing geographical inequalities in health in New Zealand, 1980–2001. International Journal of Epidemiology, 35(3), 597–603.
Pirani, E., & Salvini, S. (2012). Socioeconomic inequalities and self-rated health: A multilevel study of Italian elderly. Population Research and Policy Review, 31, 97–117.
Rice, N., Carr-Hill, R., Dixon, P., & Sutton, M. (1998). The influence of households on drinking behaviour: A multilevel analysis. Social Science and Medicine, 46(8), 971–979.
Rivellini, G. (2006). Network analysis: From theory to applications. CLEUP, Padova (Italy): Atti della XLIII Riunione Scientifica della SIS.
Schor, E., Starfield, B., Stidley, C., & Hankin, J. (1987). Family health: Utilization and effects of family membership. Medical Care, 25(7), 616–626.
Schüz, B., Wurm, S., Schöllgen, I., & Tesch-Römer, C. (2011). What do people include when they self-rate their health? Differential associations according to health status in community-dwelling older adults. Quality of Life Research, 20, 1573–1580.
Sepehri, A., Moshiri, S., Simpson, W., & Sarma, S. (2008). Taking account of context: How important are household characteristics in explaining adult health-seeking behaviour? The case of Vietnam. Health Policy and Planning, 23(6), 397–407.
Snijders, T. A. B., & Bosker, R. J. (2012). Multilevel analysis (2nd ed.). SAGE Publications Ltd.
Stafford, M., & McCarthy, M. (2006). Neighbourhoods, housing, and health. In M. Marmot & R. G. Wilkinson (Eds.), Social determinants of health. Oxford University Press.
Subramanian, S. V., Kawachi, I., & Kennedy, B. P. (2001). Does the state you live in make a difference? Multilevel analysis of self-rated health in the US. Social Science and Medicine, 53(1), 9–19.
Subramanian, S. V., Delgado, I., Jadue, L., Vega, J., & Kawachi, I. (2003). Income inequality and health: Multilevel analysis of Chilean communities. Journal of Epidemiology and Community Health, 57, 844–848.
Tomassini, C., Wolf, D., & Rosina, A. (2003). Parental housing assistance and parent-child proximity in Italy. Journal of Marriage and the Family, 65, 700–715.
Van Minh, H., Byass, P., & Wall, S. (2010). Multilevel analysis of effects of individual characteristics and household factors on self-rated health among older adults in rural Vietnam. Geriatrics and Gerontology International, 14, 209–215.
Vignoli, D., & Matysiak, A. (2013). Diverse effects of women’s employment on fertility: Insights from Italy and Poland. European Journal of Population, 29, 273–302.
Vignoli, D., Pirani, E., & Salvini, S. (2012). Family constellation and life satisfaction in Europe. In Paper Presented at the International Society for Quality of Life Studies (ISQOLS) XI World Conference. Venice (Italy). November 1–4.
Vlachantoni, A. (2010). The demographic characteristics and economic activity patterns of carers over 50: Evidence from the english longitudinal study of ageing. Population Trend 2010. Office for National Statistics (UK).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2018 The Author(s)
About this chapter
Cite this chapter
Giannantoni, P., Egidi, V. (2018). Similarity of Perceived Health Between Household Members: The “Mutual Influences” Hypothesis. In: Doblhammer, G., Gumà, J. (eds) A Demographic Perspective on Gender, Family and Health in Europe. Springer, Cham. https://doi.org/10.1007/978-3-319-72356-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-72356-3_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-72355-6
Online ISBN: 978-3-319-72356-3
eBook Packages: Social SciencesSocial Sciences (R0)