Abstract
The treatment of rheumatoid arthritis (RA) has undergone considerable changes over the last 15–20 years. With an expansion in the armamentarium of therapies available for RA comes a wider choice in selecting the best treatment in terms of comparative safety in the presence of comorbidities. Clinicians frequently encounter patients with RA-associated interstitial lung disease with uncontrolled joint disease and have to make decisions about the safest treatments in this context with the eventual goal of joint remission. In this chapter, available evidence is reviewed on the comparative pulmonary safety of non-biologic disease-modifying antirheumatic drugs (nbDMARDs), biologic DMARDs, biosimilars and targeted synthetic DMARDs in RA-ILD. In addition, the potential role for additional immunosuppression in RA-ILD is reviewed as well as overarching recommendations proposed for patient assessment to guide treatment decisions and management.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Rheumatoid arthritis
- Interstitial lung disease
- Non-biologic DMARDs
- Biologic DMARDs
- Targeted synthetic DMARDs
- TNF inhibitors
Introduction
The management of rheumatoid arthritis (RA) has changed dramatically over the past 15–20 years. New classification criteria for RA have been introduced [1] that allow the study of patients earlier in their disease course, and recommendations have been developed to treat patients with RA using a strategic approach by targeting an optimal outcome, with the primary goal of joint disease remission [2, 3]. The armamentarium of treatments available for the treatment of RA has also expanded. However, with the introduction of novel therapies comes a wider choice in selecting the best treatment for the individual patient not only in terms of comparative efficacy but also safety in the presence of comorbidities.
Interstitial lung disease (ILD) is one of the most common respiratory manifestations in patients with RA and is a major cause of morbidity and mortality. RA-ILD encompasses several histopathologic patterns; the most frequent considered here are usual interstitial pneumonia (UIP), nonspecific interstitial pneumonia (NSIP), and obstructive pneumonia (OP). The development of respiratory complications of treatment is thus particularly problematic in patients with such coexistent lung disease, and there have been many reports of respiratory complications of both non-biologic disease-modifying antirheumatic drugs (nbDMARDs) and biologic DMARD (bDMARD) therapy. Clinicians are frequently encountered with decisions about balancing risk and benefit of treatments in patients with RA-ILD who have active articular disease. Serious respiratory adverse events (SRAEs) in the patient with RA on treatment for their joint disease may be due to induction of ‘pneumonitis’ or idiosyncratic adverse drug reactions (ADRs), acceleration of pre-existing ILD or increased predisposition to infection in a susceptible host. Several nbDMARDs and bDMARDs have been implicated in the development of ILD. Conversely, treatment of the underlying disease process may be beneficial in halting the progression of the lung disease. This chapter first considers methods for assessing drug safety and then reviews the available evidence for respiratory outcomes of nbDMARDs and bDMARDs in RA-ILD and the role of additional immunosuppression and overarching recommendations for patient assessment and management of ILD.
Detection Safety Assessment Methods
Clinical Trials
Whilst randomised controlled trials (RCTs) are considered the gold standard in assessing efficacy of treatments, they have limited utility in terms of assessing safety. Although safety has been evaluated as part of a number of RCTs, uncommon events such as new-onset ILD may not be captured. RCTs often have restrictive eligibility criteria to ensure a homogenous population (leading to exclusion of patients with known RA-ILD), small numbers of patients and a short follow-up period. This also limits their external validity, as real-life patients may be older and have multiple comorbidities compared to trial patients. Open-label extension (OLE) studies are often an adjunct to double-blind RCTs, and although they do allow surveillance of participants for a longer duration, patients who are intolerant to the drug during the previous study will not be able to participate in the extension period, therefore potentially leading to underreporting of adverse events (AEs). OLE studies also lack a comparator group and are prone to loss to follow-up, making it difficult to interpret the rate of AEs.
Spontaneous Pharmacovigilance
Post-marketing spontaneous pharmacovigilance involves the reporting of suspected adverse drug reactions by healthcare professionals or patients. This is done either in the form of case reports/series to medical journals or to national or international monitoring centres, such as the UK Medicines and Healthcare products Regulatory Agency (MHRA) ‘Yellow Card Scheme’, European Medicines Agency EudraVigilance database and the US Food and Drug Administration (FDA) MedWatch programme. Whilst these are useful for drug safety signal detection, there is no available denominator to calculate rates of AE or to determine whether these reported cases represent an increased incidence above the background population rate.
Observational Cohort Studies
Observational cohorts have the advantage of being able to examine drug safety in a ‘real-world’ setting and can follow large numbers of patients for long periods of time. They can therefore study the medium- to long-term side effects of a drug that might otherwise be missed in clinical trials or spontaneous pharmacovigilance. However these come with the challenge of interpreting results in the context of clinical decisions, with their consequent biases and confounding.
Each of these methods can employ a wide array of terminology to describe various forms of respiratory AEs. For example, parenchymal lung disorders are called many things from ‘pulmonary fibrosis’ to ‘allergic pneumonitis’. There are also challenges in differentiating between respiratory conditions with different aetiologies but similar clinical presentations. RCTs, for example, can report on culture-negative pneumonias or ‘community-acquired pneumonitis’, which may indeed be idiosyncratic drug reactions or pneumonias secondary to a resistant microorganism: often patients are administered a combination of glucocorticoids and antibiotics due to initial uncertainty of the diagnosis.
The data available for this chapter come from all of the above study designs. Having been in use for RA for the longest duration, nbDMARDs and tumour necrosis factor inhibitors (TNFis) have the most observational evidence, but not in all cases. Newer TNFis, nbDMARD and emerging novel therapies recently licensed for RA have not had the opportunity for longer follow-up; therefore, experience about pulmonary safety may be restricted to clinical trials and spontaneous pharmacovigilance.
Respiratory Safety of Non-Biologic Disease-Modifying Antirheumatic Drugs
Methotrexate
Methotrexate (MTX) has been described as the anchor drug in RA treatment, as it is often used first line at diagnosis, in combination with other nbDMARDs and concomitantly with biologics, following failure of traditional nbDMARDs for controlling articular disease. It inhibits folic acid and purine metabolism along with T-cell activation. MTX-induced pulmonary injury was initially reported in children with leukaemia in the 1960s [4], followed by a case series in treated patients with RA in 1983 [5]. Following a review of 123 cases of methotrexate pneumonitis in the year 2000, 63% of cases arose in patients with RA (dose range 2.5–15 mg/week), 23% occurred during intensification/consolidation treatment for leukaemia (dose range 20–80 mg/week), and 8% were in patients treated for other malignancies (dose range 15–1400 mg/week) [6]. Whilst mortality rates have been reported up to 17%, hypersensitivity pneumonitis is reported to be a rare AE in RA patients. In a systematic literature review of 3463 patients with RA on MTX, 84 patients (2%) had some type of lung toxicity, but only 15 patients were felt to be definitive cases of pneumonitis attributable to methotrexate (0.43%) [7]. Estimates of reported incidence vary between 0.43 and 1% of treated patients (in up to 3-year follow-up) [8, 9].
Classification of MTX Pneumonitis
The clinical presentation of acute MTX pneumonitis is generally nonspecific, with symptoms (fever, rigors, malaise, nonproductive cough, dyspnoea, chest pain) that can be progressive over several days. Criteria proposed by Searles and McKendry [10] and Carson et al. [11] are generally accepted for defining MTX pneumonitis and can sometimes help in differentiating the disease from RA-ILD and respiratory infections, although it is possible to fulfil the criteria with conditions other than pneumonitis, for example, infection or a progression of pre-existing RA-ILD (Table 9.1). Searles and McKendry criteria have since been adapted by Kremer et al. [12] categorising them into major and minor. All rely on a combination of clinical features, radiological, histology and exclusion of infection.
Studies have explored other factors that might differentiate these clinically similar respiratory diseases. Histological findings in MTX pneumonitis such as cellular interstitial infiltrates, diffuse alveolar damage, tissue eosinophils and granuloma formation are nonspecific and have all been seen in RA lung disease [6]. High-resolution computer tomography (HRCT) studies in MTX pneumonitis typically show ground-glass changes, centrilobular nodules +/− diffuse parenchymal opacification [13]. Bronchoalveolar lavage (BAL) cell profiles in MTX pneumonitis show a lymphocyte alveolitis with a preferential increase in CD4+ cells compared to normal RA controls [14, 15], though comparisons have not been made between BAL in MTX pneumonitis and RA-ILD. A challenge with all these studies is the problem of measuring the accuracy of a test against no accepted gold standard.
Prevalent RA-ILD and MTX Pneumonitis
It has been argued on several counts that MTX hypersensitivity pneumonitis is a unique hypersensitivity reaction rather than the development or progression of RA-ILD. Firstly, MTX-associated lung injury tends to occur early in the course of MTX therapy [16], the close temporal relationship arguing in favour of causality. Secondly, acute lung injury has resolved after discontinuation of the drug and treatment with high-dose glucocorticoids [5]. Lastly, case reports of ILD have been reported in other conditions including psoriatic patients treated with MTX [6, 17] as well as in other conditions not typically associated with ILD.
However, there are issues with each of these arguments. Clinicians are more likely to diagnose and report MTX pneumonitis if there is a close temporal relationship. If cases in question are identified by asking rheumatologists to identify them [16], it is inevitable that a strong temporal relationship will be found. The second argument of resolution on drug withdrawal would be more convincing if there were no concurrent glucocorticoid treatment. Acute exacerbations of ILD, which may resemble drug pneumonitis, tend to be responsive to glucocorticoids. That said, there are cases of improvement on MTX withdrawal with no increase in pre-existing glucocorticoid dose [14]. Third, dose and duration of MTX treatment does not appear to be associated with pulmonary toxicity in the reported literature [6]. Furthermore a recent systematic review and meta-analysis evaluating the risk of pulmonary disease amongst MTX-treated patients with psoriasis, psoriatic arthritis and inflammatory bowel disease in RCTs concluded no increased risk [18].
It is not clear whether pre-existing RA-ILD increases the risk of MTX pneumonitis with studies both supporting and opposing this view. The largest study was a multicentre case-control study from the USA [12, 19], which identified 29 cases and 82 controls matched for MTX use. The strongest predictors of lung injury were diabetes, hypoalbuminaemia, previous use of nbDMARDs, rheumatoid pleuropulmonary involvement (OR 7.1 (95% CI 1.1–45.4)) and older age (>60). A history of COPD was modestly associated with MTX-induced lung injury. Since all the cases were identified following clinical presentation, the observed association between pre-existing lung disease and MTX pneumonitis may represent an increased likelihood of presentation (because of a reduced physiological lung reserve) or a surveillance bias rather than an increased predisposition to pneumonitis. Meta-analysis of six studies that suggested an association between pre-existing lung disease (of varying definitions) and an increased risk of MTX pneumonitis found a pooled odds ratio of 7.5 (95% CI 3.6, 15.8) [20]. However, two studies that suggested no such association [11, 21] were not included in the meta-analysis for reasons that are not clear. Howes et al. [22] followed 120 patients who received MTX for RA for a median treatment duration of 15 months, all of whom had baseline PFTs. Three patients developed pulmonary toxicity according the established criteria [5], all of whom had abnormal baseline PFTs. Of the patients studied, 3/120 patients had a transfer factor of <70% at baseline, one of whom developed pulmonary toxicity. The authors report a relative risk for pneumonitis of 10, though this estimate is not robust given the small numbers.
Progression of RA-ILD on MTX
There is currently no conclusive evidence that lung function is likely to decline faster in patients with RA-ILD on MTX who do not develop pneumonitis. In a retrospective cohort analysis, following 6 weeks of high-dose glucocorticoid treatment, one study reported treatment with MTX vs. leflunomide or azathioprine was associated with an improvement in FVC at 6 months in patients with less fibrosis at baseline, although there were no another differences in other major outcomes such as mortality [23]. Another study by Dawson et al. [7] followed 128 patients with RA for 2 years, 43% of whom were on low-dose MTX (mean 10.7 mg/week), with HRCT in all patients at baseline and pulmonary function tests (PFTs) at baseline and at 4-month follow-up intervals. There was no significant difference in the change in PFTs over the follow-up period either between the MTX and non-MTX patients or between MTX and non-MTX patients with proven ILD on HRCT at baseline. The authors concluded that they found no association between MTX therapy and progression of chronic pulmonary fibrosis.
Current guidelines on the use of MTX recommend that all patients should have a baseline chest radiograph with or without PFTs. There appears to be little evidence to support this; however, PFTs may be useful in patients with RA deemed to be at high risk of ILD or known to have RA-ILD to assess for progression (discussed further in section “Patient Management and Treatment”). In summary, diagnostic uncertainty and the lack of any gold standard test for MTX pneumonitis leaves ambiguity about the true pattern of disease. However MTX has not been shown to consistently accelerate the progression of underlying RA-ILD. Whilst few studies have been conducted in pre-existing RA-ILD stratified by severity of lung disease, the risk of pneumonitis means that it may not always be the safest first-line nbDMARD in patients with RA who have severe pre-existing lung disease.
Leflunomide
Leflunomide is an isoxazole derivative, which inhibits de novo pyrimidine synthesis, resulting in several downstream anti-inflammatory effects such as suppression of TNF-induced cellular responses and inhibition of matrix metalloproteinases and osteoclasts. Leflunomide-induced pneumonitis is rare but well reported. A signal of concern was raised in 2004 after an investigation by the Japanese Ministry of Health following post-marketing surveillance in 16 (0.5%) of the first 3000 Japanese patients treated with leflunomide, resulting in five fatalities [24, 25] and the Committee on the Safety of Medicines also reporting 17 cases in the UK of which five were fatal.
Further case reports have subsequently been reported especially in the Japanese and Korean populations [26,27,28]. However leflunomide is often used second line after MTX exposure or in combination with MTX in patients with active articular disease, which make studies evaluating leflunomide-induced pneumonitis difficult to interpret. In a report of 14 such cases from Australia and New Zealand, 12 were co-prescribed MTX [29]. Chikura et al. [30] reported on 32 pneumonitis cases following leflunomide exposure, classified using Searles and McKendry criteria (Table 9.1), and found 97% had a history of MTX exposure, whilst 41% were on concomitant MTX at the onset of ILD. The majority presented within 20 weeks of initiation. Clinical features of those who died were pre-existing ILD and diffuse alveolar damage on histology (n = 6/32). Pre-existing ILD was also shown to be a risk factor for leflunomide-induced pneumonitis in a large case-control study using a Canadian claims database [31]. The risk of ILD was increased with the use of leflunomide (adjusted RR 1.9 [95% CI 1.1–3.6]); however, in patients without previous MTX exposure or ILD history, the risk associated with leflunomide treatment was not elevated (RR 1.2 [95% CI 0.4–3.1]). However, it was acknowledged given the probable association between prior ILD and MTX pneumonitis; clinicians may be more likely to prescribe leflunomide than MTX to patients with prevalent ILD, leading to channelling bias explaining the increased risk observed.
Leflunomide-induced pneumonitis appears to occur more frequently in Japanese and Korean population (reported rate ~1%) [26, 32], whilst in the Western Caucasian population, a rate of <0.1% is reported [33]. Genetic susceptibility in Japanese patients has been described in a study which investigated human leukocyte antigen (HLA) class I associations with MTX pneumonitis in Japanese patients with RA and found HLA-A × 31:01 as a possible predictor. The prevalence of this allele is proportionally higher in the Japanese population (8.7%) than in the Caucasian population (3.9%) [34]. Therefore such genetic differences and undiscovered genetic predictors may explain some of the differences in frequency observed in such populations.
Several risk factors of leflunomide-induced pneumonitis have been reported in small numbers of patients in case series and retrospective studies including pre-existing lung disease [32, 35, 36], a prescribed loading dose, smoking, low body weight [32] and increased C-reactive protein, hypoalbuminaemia, hypoxia and lymphopaenia [36]. Treatment includes cessation of the drug, treatment with glucocorticoids with some benefit reported with activated charcoal and cholestyramine as washout treatments. Whilst conclusions of use in RA-ILD are limited from studies due to channelling bias, leflunomide should be avoided in patients with previous MTX pneumonitis and should be used with caution in patients with pre-existing ILD.
Sulphasalazine
Sulphasalazine is a 5-aminosalicyclic acid (5-ASA) derivative metabolised to sulphapyridine, which is the active moiety in RA. Pulmonary hypersensitivity reactions such as eosinophilic pneumonias [37, 38], fibrosing alveolitis and bronchiolitis obliterans have been well described, with over 50 case reports in the literature [39, 40]. Drug reaction with eosinophilia and systemic symptoms (DRESS) is also reported [41, 42]. Typical presentation of sulphasalazine-induced lung disease reported is with new-onset dyspnoea and infiltrates on chest radiograph (with or without peripheral eosinophilia with eosinophilic pneumonitis). Cough and fever are the most common symptoms with sputum production, whilst allergy history, rash, chest pain and weight loss were inconsistent findings [40]. Histology is often variable; the most frequent appears to eosinophilic pneumonia with interstitial inflammation with or without fibrosis. Drug cessation often results in resolution of symptoms in patients who develop eosinophilic pneumonia [43]. The role of systemic glucocorticoids is not well-studied, as most patients improve with withdrawal of sulphasalazine. There are no studies that have systematically evaluated the safety of sulphasalazine in pre-existing RA-ILD; however, it is worth observing that the rates of SRAEs with sulphasalazine appear much lower than those seen with methotrexate and leflunomide in the literature.
Hydroxychloroquine
Hydroxychloroquine is an antimalarial drug and is a 4-aminoquinoline derivative, often used in combination with other nbDMARDS. It is usually well tolerated and serious AEs are rare. Few cases of drug-induced pneumonitis exist [44], with some reports in association with drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome [45, 46]. Hydroxychloroquine has been tried in childhood ILD (diffuse parenchymal lung diseases) in case reports given the lack of therapeutic options. In a systematic review from 1984 to 2013 [47], 85 case reports were identified: a favourable response to hydroxychloroquine was reported in 35 cases (41%), with an unclear effect in the rest. Whilst idiosyncratic reactions leading to lung toxicity have been reported, no studies have demonstrated a benefit or harm of this drug in RA-ILD.
In summary, case report evidence for drug-induced pneumonitis exists for all nbDMARDs commonly used to treat joint disease; therefore, incident ILD may be a theoretical risk in most treated patients. With treat-to-target guidelines [2] and the eventual aim of abrogation of joint inflammation as soon as possible, most patients with RA are likely to be treated with a nbDMARD early in the course of their disease. Whether the risk of progression of RA-ILD or SRAEs increases with nbDMARDs is not clear and may vary according to the individual patient profile including their comorbidities, concomitant treatments, severity of ILD at the outset of treatment and their genotype. Evidence to date suggests caution should be exercised whilst treating patients with pre-existing RA-ILD with all nbDMARDs, particularly MTX and leflunomide, with careful monitoring of disease progression and vigilance for (sometimes rare) SRAEs associated with such treatments (summarised in Table 9.4).
Respiratory Safety of Biologic Disease-Modifying Antirheumatic Drugs
Tumour Necrosis Factor Inhibitors (TNFis)
Five TNFi agents have been approved for treating patients with RA: three monoclonal antibodies (infliximab, adalimumab and golimumab), the recombinant soluble TNF receptor etanercept and pegylated certolizumab. As biologic therapies such as TNFis target key cytokines and cells in the inflammatory cascade with pleiotropic effects on the immune system, there have been particular concerns regarding their long-term safety profile. Although these drugs are highly effective in controlling joint disease, and often are used as first-line biologics in combination with MTX, they are reported to be associated with various autoimmune AEs [48]. Whilst the most common of these appear to be lupus- and vasculitis-like events, TNFi-associated lung injury has been reported [49]. The safety of these drugs in patients with established RA-ILD continues to be scrutinised.
Conversely elevated levels of TNF-α have been detected in the lungs of both experimental animal models [50] and patients with idiopathic pulmonary fibrosis (IPF) [51]. Interestingly serum levels of TNF-α have also been found to be elevated in patients with rituximab-induced ILD [52]. Etanercept has been used in a randomised double-blind placebo-controlled exploratory trial in clinically progressive IPF subjects, however failed to show a difference in primary endpoint of improvement in FVC over 48 weeks. The study was underpowered; however, a non-significant reduction in disease progression was seen in several physiologic (including transfer factor), functional and quality-of-life endpoints amongst participants receiving TNFi. Importantly there was no decline in lung function or higher incidence of SRAEs in the etanercept group compared to placebo. Therefore whilst legitimate concerns about pulmonary toxicity have been highlighted, TNFi treatments may have plausible bidirectional effects. The next section will review the levels of evidence for both incident ILD and safety in pre-existing RA-ILD.
Randomised Clinical Trials and Case Reports
Clinical trials of TNFi therapy have been significantly underpowered to detect even a large increase in the incidence of serious RA-ILD. The original RCTs leading to eventual approval of TNFi provided no RA-ILD safety signals. In the first reported phase III trial of infliximab and MTX versus placebo and MTX over 30 weeks, there was a death in both the placebo arm due to ILD and the infliximab arm due to cardiopulmonary failure as a result of suspected pulmonary embolism or ILD [53]. In a two-year extension of this trial, there was a single death attributed to ILD in the infliximab arm; however, it was not clear whether this is the same patient reported in the previous paper.
A clinical trial of etanercept versus MTX in early RA reported three cases of pneumonitis in the MTX group at 1 year follow-up [54] and four cases at 2 year follow-up [55] with no reported cases in the etanercept arm despite a ratio of etanercept/MTX of 2:1. There was one case of death from respiratory failure in the 5-year OLE of this study in the etanercept arm [56]. No cases of ILD were reported in the 7-year OLE of etanercept [57]. ILD was not reported in any of the initial adalimumab clinical trials, in either the adalimumab or placebo arms [58]. However, within an adalimumab OLE study [59], SAEs coded as ‘parenchymal lung disorders’ occurred at a rate of 0.2–0.3/100 patient-years, accounting for 20% of all SAE’s. In this trial, however, there was no placebo-controlled or nbDMARD-exposed arm, making the interpretation of these figures challenging. Similarly no signal of concern for incident ILD was observed in the initial golimumab-RA trials [60, 61] in the two-year [62] or five-year [63] extension studies. In the certolizumab RAPID 1 and RAPID 2 trials [64, 65], and subsequent OLEs [66], no cases of drug-induced pneumonitis were reported in any arms.
Therefore original RCTs of TNFi agents did not raise concern over the potential development of ILD. These trials typically had short duration, included between 210 and 340 patients in the TNFi arm each and excluded patients with RA-ILD at baseline. Concerns regarding the respiratory safety of TNFi agents arose initially following three case reports of rapid fatal exacerbations of RA-associated fibrosing alveolitis following commencement of infliximab in 2004 [67], which was extended in a later publication to five cases [68]. Of these cases, three patients were taking concomitant azathioprine, and one taking leflunomide developed rapid progression of RA-ILD (known UIP preceding treatment). The fifth patient did not have a history of lung disease pretreatment and, following infliximab, developed nonfatal cryptogenic organising pneumonia (COP or bronchiolitis obliterans organising pneumonia [BOOP]) [68]. In a case series of autoimmune diseases associated with TNFi, 24/226 (~10%) were reported to develop ILD (interstitial pneumonitis in 18 patients, sarcoidosis in three, pulmonary haemorrhage in two and BOOP in one patient) [49]. Exacerbation of previous ILD was reported in four patients. Perez-Alvarez et al. described a further series of 122 patient case reports from the literature (89% with RA), with incident ILD or exacerbation of pre-existing ILD (20 patients, 38%) [69]. The outcome was available in 52 of the described cases: 21 (40%) had complete resolution, improvement or partial resolution in 13 (25%) and no resolution reported in 18 (35%). Case reports of incident ILD have been reported with newer TNFis such as certolizumab [70,71,72,73] and golimumab [74], including possible deterioration of pre-existing ILD in a patient with RA treated with certolizumab and leflunomide after 3 months of therapy [75]. Whilst the temporal association with onset of ILD and repeated reporting of such events provides a signal of concern, the interpretation of such data for extrapolation into clinical practice is limited by a likely reporting bias, a possible ‘bandwagon’ effect (a phenomenon where following the publication of an index case, further cases are consequently more likely to be reported), and lack of an adequate denominator. Furthermore, reports of stabilisation of RA-ILD in patients exposed to TNFi therapy have also been published [76,77,78], suggesting a further bidirectional influence of TNFi on ILD.
Observational Studies
To accurately evaluate the risk of incident ILD or exacerbation in patients with RA-ILD on TNFi in patients who are most likely to receive them in the real world, observational studies offer the best design to examine rare outcomes. However all studies evaluating such events have faced methodological issues, namely, with channelling bias and challenges with classification. Using the National Databank for Rheumatic Diseases, Wolfe et al. used a combination of hospital records, patient descriptive reports and physician and mortality records to classify patients who had severe RA-ILD (requiring hospitalisation or who died) [79]. They reported a significant association with previous use of infliximab (HR 2.1, 95% CI 1.1–3.8) and etanercept (HR 1.7, 95% CI 1.0–3.0). However the study was confounded by the fact that physicians were, at the time, prescribing TNFis for treatment of RA-ILD, possibly accounting for such an association. The incidence of hospitalisation for ILD requiring hospitalisation was reported 260 per 100,000 patient-years with a 27% mortality, likely reflecting the types of patients included in this analysis. Whilst the authors concluded that there was no evidence of an association between TNFi and hospitalisation for ILD as the observed effect with TNFi was likely to be due to confounding by indication, the specific effect of TNFi on patients with RA-ILD at baseline was not assessed [79].
Two claims database studies have evaluated ILD incidence in patients treated with biologics including TNFis. To assess the risk of incident ILD in 8417 patients with autoimmune diseases who were members of Kaiser Permanente, Northern California, Herrington and colleagues compared new users of TNFi and nbDMARDs [80]. ILD cases were identified using ICD codes, with a pilot of the first 100 cases verified using CT reports. The study demonstrated no increased risk in the TNFi-exposed group of new ILD; however, patients with known ILD at baseline were systematically excluded. Using data from the commercial claims and benefit (Medicare) databases, Curtis et al. assessed the ILD incidence and exacerbation amongst users of rituximab, abatacept and tocilizumab to TNFi agents [81]. Two definitions of ILD were used (one more sensitive, the other more specific in the absence of CT results and lung histology). There were no significant differences in the risk of ILD and its related complications between patients with RA receiving TNFis and those on non-TNFis. Of the patients’ studies, 419 patients had a history of ILD, of which 232 were put on TNFi agents [81]. However there were clear baseline differences between the groups receiving the different drugs, which were not adjusted in the analysis. Therefore the true risk in the TNFi group may be confounded if patients with higher levels of RA joint disease or ILD disease severity were channelled to specific therapies, which may have led to an overall underrepresentation of risk in this group.
In a recent single-centre retrospective evaluation from Japan, Nakashita et al. described up to one-year outcomes of 163 RA patients with (n = 58) or without (n = 105) established ILD on a biologic drug [82]. In patients with established RA-ILD, 14 (24%) had an exacerbation of ILD, which the authors concluded was greater in patients exposed to TNFi agents using descriptive statistics. None of the patients on tocilizumab (n = 9) or abatacept (n = 3) were reported to have an exacerbation; however, conclusions were limited due to low numbers. Similar to Curtis et al.’s study [81], it did not adjust for severity of RA or any confounders potentially introducing channelling bias. In this case, it is likely that patients on TNFi (approved earlier than the non-TNFi drugs in this study) had more severe disease at the outset, in turn is known to be associated with the outcome.
Data from the British Society for Rheumatology Biologics Register for RA (BSRBR-RA) evaluated the effect of TNFi in patients with RA who have established ILD [83] and reported no difference in all-cause mortality between patients on TNFis and nbDMARDs. However RA-ILD as an underlying cause of death was reported in a higher proportion of TNFi-treated patients than nbDMARD-treated patients (21 vs. 7%), suggesting a signal for concern. Methodological challenges included potential for misclassification, as prevalent ILD was identified from clinician questionnaires since attempts to retrospectively verify such cases were unsuccessful. Whilst it could be that TNFi truly increased the proportion of deaths attributable to RA-ILD, given the well-publicised respiratory concerns with TNFi, it may be that physicians at that time were more inclined to report RA-ILD on death certificates of patients exposed to TNFis leading to the observed relationship. PFTs, imaging or nonfatal exacerbation of ILD details were not available to examine the effect of treatment on such outcomes.
Challenges in interpreting the data common to all studies is delineating the effect of TNFi on RA-ILD in the presence of nbDMARDs, the majority of which are linked to reports of pneumonitis or exacerbation of RA-ILD. Furthermore, it can be difficult to ascertain if severity of RA associated with both development of ILD and also being the indication for TNFi could explain the association between TNFi and RA-ILD exacerbation. However, no studies have completely excluded a clinically meaningful risk, and the multiple case reports, observational evidence and possible increase in ILD-specific mortality in patients with known RA-ILD indicate that careful monitoring and caution is required when considering use in this setting.
Biosimilar Drugs
With several biologics approaching patent expiration, substantial interest has been in the development of biosimilar products that are not bioidentical but highly similar to already approved reference products listed above [84]. To date, biosimilar infliximab CT-P13 (marketed as Remsima and Inflectra) and biosimilar etanercept SB4 (marketed as Benepali) have been approved for use by the FDA and EMA. There were no cases of pneumonitis or ILD in the biosimilar infliximab CT-P13 trials in RA [85, 86] or ankylosing spondylitis [87], although there was a case of non-infective dyspnoea reported within the CT-P13 arm of the latter trial felt to be related to the drug by the investigators. Open-label extensions of these trials have not suggested a signal for concern [88, 89]. Similarly no cases of new ILD were reported with biosimilar etanercept SB4, albeit treatment-emergent AEs in ≥2% of patients were reported only [90]. One patient in the SB4 arm died due to cardiorespiratory failure (felt to be unrelated to the drug by the investigators), and further details of the event were not provided [90]. Whilst this provides some initial reassurance, biosimilars should be considered as having similar risks to the originator reference products and therefore be used with vigilance in the context of established RA-ILD.
Non-tumour Necrosis Factor Inhibitor Biologics
Rituximab
Rituximab is a monoclonal chimeric anti-CD20 antibody licensed for the treatment of non-Hodgkin lymphoma and RA in TNFi nonresponders. Rituximab-induced ILD has been a well-described AE in haematology patients often presenting as acute/subacute hypoxaemic organising pneumonia, NSIP or hypersensitivity pneumonitis [91,92,93]. Whilst its pathogenesis is unknown, it may involve induction and release of cytokines, and it has been reported to occur in patients receiving rituximab for several months [94]. In RA, a number of rituximab trials have reported incident ILD [95,96,97], including subsequent deaths from acute respiratory distress syndrome (ARDS) [98] and culture-negative (non-infective) bronchopneumonia [99]. Hadjinicolaou et al. identified >120 cases of rituximab-associated ILD up to June 2010 in a systematic review of published studies and reports to the FDA and EMA [100]. In addition, UK spontaneous pharmacovigilance reporting systems (via its Yellow Card system) have recorded hundreds of rituximab-associated cases of non-infectious respiratory disorders till March 2016 (Table 9.2). Of the patients with possible rituximab-associated ILD/pneumonitis, 15 deaths have been reported (Table 9.2). Further observational evidence has been discussed in section “Other Agents with Limited Agents in RA-ILD”).
Abatacept
Abatacept is a selective T-cell costimulation modulator. It is a fully human recombinant protein that comprises of the extracellular domain of CTLA4 and the Fc portion of an IgG1 molecule that has been modified to prevent complement activation. Pooled safety data from eight trials of abatacept involving 3173 patients with RA reported incident ILD in 11 patients (0.11 cases per 100 person-years), with no events reported in the placebo control groups [101]. Patients with pre-existing RA-ILD were excluded from all of the initial abatacept trials [101]. Therefore limited conclusions can be drawn from existing trial data, which may suggest a small increase in incident ILD in patients with RA.
Despite its FDA licence back in 2005, few case reports exist describing abatacept-induced lung injury. One case reported drug-induced respiratory failure, 2 weeks after the second abatacept dose [102], however was unable to distinguish if infection was the reason for deterioration by the time of death. Relatively few respiratory ADRs have been reported to the regulatory agencies after treatment with abatacept compared with other biologic agents (Table 9.2). Indeed, only one case of pneumonitis and 23 cases of non-infectious respiratory events had been reported through the UK Medicines and Healthcare Products Regulatory Agency (MHRA) ‘Yellow Card’ system by March 2016. However it is worth noting at exposure to abatacept may be limited in the UK due to lack of its initial approval by the National Institute of Health and Care Excellence (NICE) until 2010 as a second-line biologic (following TNFi failure and if rituximab was contraindicated) and first-line biologic approved in 2013.
Whilst experience of using abatacept in the context of pre-existing ILD is limited, a case report of rapid-onset interstitial pneumonia 2 days post initiation of treatment has been described in a Japanese patient [103]. Conversely, there are reports of stabilisation of RA-ILD on abatacept [104] and improvement in some patients [105]. In a case series of 16 patients with RA-ILD (with varying grades of severity at baseline), all patients completed 52 weeks of abatacept treatment, and no one was reported to have an exacerbation of their pulmonary disease [105]. In the three patients with RA-ILD on abatacept, as part of Nakashita and colleagues’ retrospective study [82], none had ILD-related complications reported by one-year follow-up. However using claims data, in the Curtis et al. study [81], of the 102 patients with RA-ILD on abatacept, there was no significant decreased risk of ILD events compared to TNFis.
In comparison with other biologic agents introduced to the market at around the same time, the spontaneous pharmacovigilance and case report figures are cautiously encouraging. The lack of a clear denominator or the number of patients treated with each drug in these settings makes accurate interpretation challenging. Whilst experience in baseline RA-ILD is limited, emerging observational data thus far appears tentatively reassuring. Additionally patients on abatacept may have a more favourable infection profile in comparison to other biologics in those who have experienced a hospitalised infection previously [106]. This study also forms the basis of its use as a conditional recommendation in the context of prior serious infection in the ACR 2015 guidelines for RA [107]. Therefore given the limitations of spontaneous pharmacovigilance and inconsistent findings from observational data, more observational data is required before robust conclusions can be formed regarding safety of abatacept in RA-ILD. However, there may be a role for abatacept particularly in patients in whom serious infection is a concern.
Tocilizumab
Tocilizumab is a humanised monoclonal antibody that inhibits IL-6 receptor signalling through its membrane-bound and soluble forms. In the treatment of active joint disease, where MTX is contradicted or not tolerated, tocilizumab monotherapy has been shown to be as effective as combination treatment with MTX [108, 109]. Given the potential concerns regarding the respiratory safety profile of MTX, there may be a preference for using this drug over other biologics in RA-ILD by some physicians. Experimental work has demonstrated profibrotic effects of IL-6 on lung fibroblasts, which may have the potential to be antagonised by blocking the IL-6/IL-6 receptor pathway, suggesting a potential benefit of tocilizumab in RA-ILD [110]. However, clinical data on the use of tocilizumab in pre-existing RA-ILD is sparse and inconclusive.
Unlike other biologics, early RCTs of this biologic agent have raised some concerns regarding an association with development of ILD. A single case of ‘allergic pneumonitis’ after tocilizumab monotherapy exposure in 109 patients with RA was reported in 2004 by Nishimoto et al. [111]. In 2008, two of 419 patients treated with tocilizumab and MTX in the OPTION study [112] developed ILD at weeks 9 and 13, with a further two cases of ‘culture-negative pneumonia’. A similar case was also reported in the SATORI [113] trial, which included patients on tocilizumab monotherapy. In one of the few head-to-head biologics studies, the 2013 ADACTA trial compared tocilizumab monotherapy with adalimumab monotherapy and reported two deaths in the tocilizumab arm, one of which occurred suddenly in a 56-year-old man with multiple comorbidities, including pre-existing ILD [114]. Further deaths due to interstitial pneumonitis have been reported in tocilizumab-exposed arms in recent trials such as the SURPRISE (tocilizumab + MTX arm) [109], as well as the SUMMACTA trial, the latter reporting one death due to ILD and ARDS each [115]. Of note other anti-IL-6 drugs being evaluated for RA, such as sarilumab (a fully human anti-IL-6Rα mAb that binds membrane-bound and soluble human IL-6Rα), have also reported SRAEs within trials. Of the two deaths reported in the SARIL-RA-MOBILITY trial (sarilumab +MTX), one was due to ARDS (investigator felt was drug-related) [116]. Within the phase III study published to date, four deaths in the sarilumab arms were described [117], one due to unspecified respiratory complications post surgery.
Whilst the consequences of such reports are not clear at present for the patient with pre-existing ILD, such observations suggest the need for alertness especially since most trials exclude patients with multimorbidity. Case reports have suggested an association between incident ILD and tocilizumab exposure in patients on a concurrent nbDMARDs both in RA [118,119,120] and adult-onset Still’s disease [121]. Spontaneous pharmacovigilance figures from the UK have reported five deaths due to SRAEs in tocilizumab-exposed patients to date, four due to ILD and one secondary to ARDS (Table 9.2). Whilst the total number of patients exposed to treatment (denominator) is not available, cautious comparison of these figures with abatacept, which was approved earlier than tocilizumab by FDA and EMA, is of interest. Furthermore, the REACTION study, a retrospective study of 229 tocilizumab-exposed patients with RA in Japan, reported interstitial pneumonia in two of the 229 patients followed up over 6 months and an additional six discontinuations for pneumonia (presumed infective), raising further concerns of pulmonary toxicity in this population.
RA-ILD was found to have improved in one patient with pre-existing RA-ILD within 16 weeks after administration of tocilizumab [122], whereas another patient with biopsy-proven UIP and emphysema developed a fatal exacerbation of ILD after treatment with tocilizumab [119]. Of the 23 ILD events reported in 3881 patients who received tocilizumab every 4 weeks over 28 weeks (1.28 per 100 patient-years) in a post-marketing surveillance programme in Japan, the presence of a known ILD was a risk factor for acute presentation with ILD exacerbation and serious infections [123]. Recent small retrospective observational studies demonstrate limited reassurance. In the nine patients with RA-ILD selected to receive tocilizumab treatment over 1 year in the Nakashita et al. study [82], no patients were reported to have an ILD exacerbation. However patients who did not complete at least 1 year of follow-up lacked imaging data or discontinued treatment because infections were excluded from the study leading to a likely selection bias of reported outcomes. In a retrospective case-control study in RA, patients were stratified according to the presence of baseline RA-ILD (n = 78) or without (n = 317) [124]. During observation period of 148.8 patient-years and 629.7 patient-years for the RA-ILD and non-ILD groups, respectively, six patients developed an acute exacerbation in the RA-ILD group (none in the non-ILD group). Interesting all the patients who developed an exacerbation of ILD were on tocilizumab monotherapy, and there was a suggestion that all patients who developed an exacerbation had more uncontrolled articular disease that may in turn be associated with the outcome [124]. The administrative data study by Curtis et al. concluded no significant differences between tocilizumab and other biologic drugs in the risk of ILD or its exacerbation [81]. However exacerbation of ILD can be difficult to define in such databases as recognised by the authors. Hence surrogate measures such as hospitalisations for ILD, pneumonia or lung transplant were used, which as expected were observed infrequently and capture a heterogeneous overall outcome that includes infection. Therefore, whilst current evidence does not allow robust conclusions about the pulmonary safety of tocilizumab in RA-ILD, ongoing vigilance is recommended if used in this context in the absence of clear predictors of ILD exacerbation.
Anakinra
Anakinra is a recombinant IL-1 antagonist, which binds competitively to the type I IL-1 receptor and therefore acts as a competitive antagonist to IL-1. Initial trials that supported the licensing in RA did not demonstrate a signal of concern in relation to incident ILD either as monotherapy [125,126,127] or in combination with MTX [128]. Whilst such data supported the initial licensing of anakinra in RA, in clinical practice, it is not widely used in RA for active joint disease as it appears less efficacious than TNFi agents and of no additional value in early RA [129]. Moreover, combination of anakinra and etanercept provided no added benefit compared to etanercept monotherapy, and indeed increased serious safety concerns were reported including two patients with new ILD and pneumonitis in the combination biologic arms [130]. There are sparse reports of non-infective SRAEs on anakinra from spontaneous pharmacovigilance (Table 9.2), possibly reflecting fewer exposed patients with RA. Therefore apart from one case of improvement in tocilizumab-induced pneumonitis following anakinra in a patient with adult-onset Still’s disease [121], there is no further literature indicative of non-infective SRAEs with its use [33] but also minimal evidence to suggest a potential beneficial role in RA-ILD.
Janus Kinase Inhibitors
Janus kinase (JAK) inhibitors , such as tofacitinib and baricitinib, are synthetic orally administered compounds that block JAK, a protein that mediates signal transduction of multiple cytokines. Although these are not biologic drugs, though they interact with biological pathways, they have been classed as targeted synthetic DMARDs (tsDMARDs) for use in moderate to severe RA, who are nonresponders or intolerant to MTX [3, 131]. Tofacitinib has been approved in several countries, such as in the USA, Latin America and Asia although not in the European Union or UK. Baricitinib has completed phase III trials, and early results from head-to-head trials even suggest that it may be more efficacious than a TNF inhibitor [132].
RCT data thus far with regard to respiratory safety of JAK inhibitors are inconclusive. Phase III trials of tofacitinib with concomitant MTX in patients with RA have reported cases of new-onset ILD and pulmonary sarcoidosis [133]. Other SRAEs reported in tofacitinib-treated arms in RCTs include bronchopneumonia [134] and a death due to ARDS [135]. A combination of pulmonary fibrosis and chronic obstructive pulmonary disease has been observed in such trials using tofacitinib monotherapy [136]. However data from two long-term extension studies from Japan following up 4102 tofacitinib-treated patients over 5963 patient-years reported no additional ILD events [137], nor did subsequent meta-analysis of tofacitinib trials [138]. In addition phase IIb studies and phase III studies of baricitinib also have not reported incident ILD cases [139, 140] and is currently under regulatory review. In 2015, the FDA released a Risk Evaluation and Mitigation Strategy (REMS) document highlighting the known concerns with tofacitinib, instructing the pharmaceutical company to send information out to healthcare professionals regarding the risk of serious infections, malignancies, decreases in peripheral lymphocyte counts, neutrophil counts and haemoglobin and derangement in lipid profiles [141]; lung toxicity was not mentioned. No case reports or regulatory reports of ILD have been published to date, although tofacitinib was licensed for the treatment of RA a few years ago in November 2012 in the USA and remains unlicensed in most of Europe, limiting the numbers of exposed patients. Conclusions drawn regarding the association between JAK inhibitors and ILD in patients with RA are therefore restricted, given limited data and further observational evidence are required to assess its effect on pre-existing RA-ILD.
Immunosuppressive Agents to Treat Rheumatoid Arthritis-Related Interstitial Lung Disease
Although RA-ILD is a fairly heterogeneous extra-articular manifestation of RA, the majority of cases mimic the two idiopathic interstitial pneumonia patterns of NSIP and UIP. Whilst NSIP and organising pneumonia appear to be more responsive to glucocorticoid treatment, the presence of the UIP pattern on HRCT in patients with RA may be associated with a significantly shorter survival compared to other forms of interstitial disease [142]. As a general clinical guidance, lung disease features that may be predictive of treatment benefit include histopathologic patterns other than UIP (especially NSIP and OP, younger age of the patient and worsening of symptoms, PFTs or finding on HRCT over the preceding 3–6 months [143,144,145]. A DLCO of less than 54% is associated with progression and poor prognosis and may identify patients who could be considered for treatment [7]. Numerous medications have been described for potential therapies for RA-ILD, but currently there are no large RCTs to help guide physicians specifically in the management of the pulmonary manifestations of RA-ILD. In addition to immunosuppressive treatments, general considerations for management of RA-ILD include smoking cessation and age-appropriate vaccinations for pneumonia and influenza, as well as prophylaxis for Pneumocystis jirovecii pneumonia in patients who are profoundly immunosuppressed [145].
Glucocorticoids and Azathioprine
Typically glucocorticoids were used as first-line therapies in an attempt to stabilise and improve the disease course of RA-ILD based on limited evidence from IPF. Because RA-ILD is a heterogeneous spectrum of histopathologic patterns beyond UIP (IPF), experience extrapolated from management of idiopathic ILD suggests that some forms, including NSIP and OP, may respond to glucocorticoid therapy [145]. Given the paucity of evidence in RA-ILD, it was felt that the addition of azathioprine maybe beneficial in glucocorticoid-responsive patients and could result in improved survival compared to glucocorticoids alone, again based on historic data from IPF studies [146]. However, the 2012 multicentre Prednisone, Azathioprine, and (N) acetylcysteine [NAC]: A Study That Evaluates Response in IPF (PANTHER-IPF) trial had to be prematurely stopped as it is found that combination of prednisone, azathioprine and NAC was associated with greater mortality (eight vs. one death), more hospitalisations (23 vs. 7) and more serious AEs (24 vs. 8) compared to placebo in IPF patients with mild to moderate disease [147]. A large proportion of deaths were due to pulmonary infection, highlighting the need for adequate precautions to be taken against respiratory infections in patients with RA-ILD who are susceptible to serious infections [148]. Indeed in elderly patients with RA, prednisolone has been shown to have a dose-dependent risk of infection, with current/recent glucocorticoid therapy demonstrating the greatest impact on infection risk [149]. Therefore use of glucocorticoids specifically for ILD in RA is best performed after liaison with respiratory colleagues, with use of the lowest possible dose prescribed for the shortest duration.
Anti-Fibrotic Treatments
Pirfenidone is an anti-fibrotic drug that inhibits transforming growth factor beta (TGF-β)-stimulated collagen synthesis, decreases the extracellular matrix and blocks fibroblast proliferation. It has demonstrated efficacy in IPF [150,151,152] and has been approved by the National Institute of Health and Care Excellence in the UK and the FDA in the USA for use in patients with mild or moderate IPF. In CTD-ILD, specifically secondary to systemic sclerosis, case reports and small retrospective studies have suggested modest benefit [153,154,155,156], whilst a recent open-label study in systemic sclerosis demonstrated acceptable tolerability of pirfenidone, especially important since 63.5% of patients were on concomitant mycophenolate mofetil [157]. Currently there is no evidence for its use in RA-ILD. Theoretically, however, given its action on TGF-β and fibroblast proliferation, there may be justification of its use in the fibrotic NSIP pattern and fibrotic stages of other RA-ILD subtypes [158, 159]. Currently there is a phase II trial underway to assess the safety and tolerability of pirfenidone 2403 mg/day for the treatment of RA-ILD [160], with a need for more RCTs the effect on respiratory function in this setting. Other anti-fibrotic agents such as nintedanib, a tyrosine kinase inhibitor that targets multiple tyrosine kinases, including vascular endothelial growth factor, fibroblast growth factor and platelet-derived growth factor receptors, have been recommended by the international thoracic guidelines for its use in IPF [144]. It was recently found in various murine systemic sclerosis models to effectively inhibit the endogenous as well as cytokine-induced activation of fibroblasts and exert potent anti-fibrotic effects [161]. Whilst there is currently no clinical evidence to date in CTD/RA-ILD, there may be potential for future clinical trials with this drug.
Other Agents with Limited Evidence in RA-ILD
Cyclophosphamide has been commonly used to treat ILD unresponsive to glucocorticoids. However evidence of its use in IPF is lacking [162]. Conflicting data exist regarding its use in scleroderma-related ILD [163], with additional concerns regarding its toxicity profile. RCTs using cyclophosphamide suggest moderate benefit in scleroderma-ILD patients with early disease [164,165,166], although a previous meta-analysis concluded no improvement in pulmonary function following 12 months of treatment [167]. No RCTs have been performed assessing the use of cyclophosphamide in RA-ILD. Limited evidence suggests that there may be some role in rapidly progressing patients with restricted therapeutic options in the acute or subacute setting [168] or in refractory drug-induced pneumonitis unresponsive to glucocorticoids [169]. The use of this agent is not recommended for mild/moderate stable RA-ILD disease.
Experience of using cyclosporine in the treatment of RA-ILD is limited and not recommended currently due to its poor safety profile and absence of proven benefit on pulmonary or joint disease. Few publications in IPF have been less than encouraging [170, 171]; however, it appears to yield some benefits according to anecdotal reports in myositis-related ILD particularly anti-synthetase syndrome [172,173,174]. Mycophenolate mofetil often used in the treatment of scleroderma-ILD is an inhibitor of lymphocyte proliferation and additionally targets nonimmune cells such as fibroblasts and smooth muscle cells. The majority of the evidence for use has been derived from small prospective case series and retrospective reviews and has been shown to stabilise scleroderma-ILD [175,176,177] and CTD-ILD [178]. In the latter series, 18 patients with RA-ILD were included; mycophenolate was associated with modest improvements in forced vital capacity (FVC), diffusing capacity and reductions in the prednisone dose [178]. A head-to-head RCT assessing the use of a two-year course of mycophenolate compared to oral cyclophosphamide for 12 months in SSc-ILD has recently been published, demonstrating a more favourable safety profile with mycophenolate; however, both treatment arms demonstrate similar efficacy on lung function [179]. In the treatment of RA-ILD, mycophenolate has been prescribed at doses of 1–2 g per day in patients with RA who have limited pulmonary disease with some benefit [175, 180]. However it is not effective in the treatment of active articular disease on RA, requiring the use of concomitant nbDMARDs, which may have additional consequences on tolerability. Whilst studies supporting the use of mycophenolate in RA-ILD represent a relatively small number of patients, further work on tolerability and safety in the context of active RA is required, and if promising well-designed trials may be helpful before advocating its use in this area.
Of the biologics having potential utility for treatment of RA and other connective tissue disease-related ILD, perhaps rituximab has had the most interest and shown some promising results in published case reports and case series, not inclusive of RA [181,182,183,184]. A recent retrospective review of CTD-ILD cases treated with rituximab, which included anti-synthetase syndrome (n = 10), dermatomyositis (n = 3), systemic sclerosis (n = 3), systemic lupus erythematosus (n = 2) and unclassifiable CTD-ILD (n = 4), suggested stabilisation of lung disease in 11 patients and worsening in nine patients. Four patients with myositis had a reported clinically significant improvement with an FVC of >10% post treatment. Whilst encouraging in a CTD-ILD setting, most published work is in the form of case reports, subject to reporting bias, or retrospective case series.
Evidence of rituximab use for the treatment of RA-ILD has not been encouraging and studies to date have been small or inconclusive. In an open-label pilot study of rituximab in RA-ILD [185] of seven patients who completed a 48-week follow-up, one showed improvement in respiratory function, five were stable and one deteriorated. The study initially recruited ten patients, and of the three who did not complete the study, one patient died of ARDS/possible pneumonia, 6 weeks post treatment (no infective source identified). Four small retrospective observational studies assessing the use of rituximab in RA-ILD have been inconclusive (all still in abstract form, full papers not published). Dass and colleagues in 2011 [186] presented data from 48 patients with baseline RA-ILD; three deaths were reported in patients with RA-ILD following rituximab treatment, one due to pneumonia and possible acute progression of ILD, 4 weeks after the first cycle of rituximab therapy. Furthermore, five patients had a decline in transfer factor of >10% over an unspecified time in the presented results of this study. The same group reported their rituximab experience in RA-ILD over 10 years (January 2004–July 2014) in 2015 [187]. Of the 53 patients with RA-ILD on rituximab with a total of 171 patient-years, the authors concluded there was no significant improvement or deterioration in the majority (as measured using FVC/ DLCO; actual data not available in abstract). However there were 12 deaths reported, nine of which were attributed to progressive ILD (median DLCO of 41% [range 35–64%] pre-rituximab). Other reasons for death were lung cancer, colon cancer and infection post surgery (n = 1 each).
Becerra et al. [188] reported on a single-centre retrospective review of 38 patients with RA and known lung involvement who were undergoing therapy with rituximab, of whom 19 had established RA-ILD. Progression of ILD over 4 years was described in one patient with severe UIP at baseline. Improvement in lung function was observed in none of the patients, 66% (n = 25) reporting respiratory infections, two of which required hospitalisation. Recent work from the BSRBR-RA compared mortality of 353 patients with physician-reported RA-ILD, of whom 310 were treated with TNFi and 43 on rituximab [189]. The differences in mortality between the two groups were not statistically significant, and adjustment for baseline confounders made little difference to the estimates (HRadj 0.51, 95% CI 0.25–1.06). However, methodological issues included inherent differences in the two treated groups (the TNFi group being a more historic cohort, therefore likely to have more severe disease), low numbers of deaths and no information on baseline RA-ILD severity. The results of all four of these studies are difficult to interpret often due to a lack of well-matched comparator groups and uncertainty about the natural history of RA-ILD.
Therefore, currently, few data exists that suggest that rituximab can markedly improve RA-ILD. In comparison to other biologics, there did not seem to be a significantly lower risk of complications related to ILD in the Curtis et al. study [81], although channelling bias may exist. Furthermore rituximab is known to reduce IgG levels, which in turn may be associated with an increased infection risk, which bears consideration whilst making such treatment decisions [190]. In the context of RA overlap with another CTD, however, RTX may have a role in stabilising ILD, especially with other extra-pulmonary manifestations of CTD which exist that may benefit from B-cell depletion. A clinical trial is currently underway comparing rituximab versus cyclophosphamide in patients with systemic sclerosis, myositis and mixed connective tissue disease (RECITAL, ClinicalTrials.gov Identifier: NCT01862926). Currently, therefore, the evidence does not support preferentially switching to rituximab in all patients with RA-ILD who have active joint disease, regardless of the severity of lung disease.
Lung Transplant
In end-stage refractory RA-ILD, single lung transplantation may be considered. However there are limited data on long-term outcomes for lung transplant in RA-ILD. Amongst ten patients with RA-ILD who underwent transplantation, survival at 1 year was similar to IPF lung transplant recipients (67 and 69%, respectively), although higher for scleroderma-ILD at 82% [191]. Eligibility for lung transplantation may be restricted due to age (typically <65 years), contraindicated with certain comorbidities common in RA including osteoporosis, whilst other extra-articular manifestations of RA may in turn complicate transplantation. Nonetheless, comparable survival outcomes of RA-ILD with IPF are somewhat reassuring.
In summary at present, there are no current treatments available that have appeared to consistently stabilise RA-ILD as well as adequately treat joint symptoms. The risks and limited benefits of such medications bear consideration, especially since most evidence for efficacy has been demonstrated in IPF and CTD-ILD. Glucocorticoids may be used in RA-ILD, however, with the lowest effective dose for the shortest possible duration to minimise risk of infection amongst others. Robust RCTs are required to support the use of novel antfibrotic agents or immunosuppressive therapies directed towards treatment of RA-ILD. However, at present there is a paucity of evidence to support the routine use of these strategiest.
Patient Assessment and Management
Evidence to guide management and treatment of RA-ILD is of low quality or absent, hence extrapolated from systemic sclerosis-ILD or IPF. However, despite the lack of robust data, clinicians are required to advise patients on the comparative safety of treatment and strategies to minimise complications of RA-ILD such as infection and reduce the overall burden of morbidity to prolong survival. In addition RA management has become increasingly complex over the last decade. Several effective DMARDs are available, and treat-to-target strategies support the use of early, rapidly escalating treatment often in combination with each other. As discussed earlier, there are no treatments that conclusively improve both joint and pulmonary disease in all patients; therefore, careful baseline assessment, adequate risk assessment for adverse outcomes and regular monitoring and vigilance whilst using the majority of DMARD strategies are essential.
Baseline Assessment of Pre-Existing RA-ILD
To enable guidance of management strategies, a recent approach in idiopathic interstitial pneumonias (IIP) has been to classify pulmonary disease as self-limiting, reversible, stable, progressive or irreversible [143, 192, 193]. A thorough assessment of baseline RA-ILD severity should consider clinical features, PFTs and imaging pattern/extent on HRCT, low DLCO and a high radiological fibrosis score on HRCT being predictors of poor survival [194,195,196]. Such information in combination with monitoring disease progression over time allows mapping of the disease trajectory and may better inform management decisions in the face of poor evidence.
Clinical assessment including quantification of exercise tolerance using instruments such as the five-point Medical Research Council (MRC) breathlessness scale [197] can help aid serial assessment of the symptoms of RA-ILD (Table 9.3). Bibasilar crepitations are an associated feature that may help trigger detection of asymptomatic ILD, but have limited value in assessing severity or monitoring progression. The 6-min walk test is a commonly used instrument for assessing IPF and can be performed easily. Reduced walk distance and oxygen desaturation below 88% are poor prognostic factors in IPF [144, 198]; however, practically this may be challenging to perform in RA patients with poor mobility. PFTs provide objective measures of lung function and should be performed in all patients with respiratory clinical features, or confirmed RA-ILD, prior to decisions about therapy. ILDs share a restrictive pattern, with reductions in lung volumes and a reduced DLCO [199]. Low baseline FVC and DLCO (FVC <60% and DLCO <40% of predicted values) are independent predictors of early death in patients with IPF [195, 196]. Importantly, a 6–12-month decline in FVC of ≥10%, or a decline in DLCO of ≥15%, is associated with increased mortality in IPF [200]; this association might also exist in patients with idiopathic fibrotic NSIP.
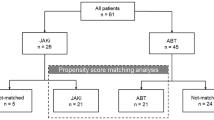
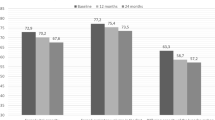
HRCT imaging is indicated in patients with RA-ILD clinical features or in asymptomatic patients with a DLCO of <70% of predicted [201]. Individuals with HRCT findings consistent with UIP, such as basally dominant honeycomb cysts with little or no ground-glass change, have poorer prognosis than those with HRCT-detected features indicative of other types of IIP [142, 202]. In SSc-ILD, an HRCT-based prognostic staging system has been developed, categorising patients as having limited (<20% lung involvement) or extensive (>20% lung involvement) SSc-ILD, with extensive disease found to be a strong predictor of mortality [203]. Similarly quantifying the extent of fibrosis and disease on HRCT has been shown to predict disease progression in IPF [204]. No comparable studies have assessed the use of similar HRCT-based scoring in RA-ILD, although a small study suggested that the degree of interstitial changes detected using HRCT imaging was predictive of prognosis [205]. On the basis of these factors, the authors have previously proposed a framework for assessment of RA-ILD, risk assessment before initiation of biologic therapy and post-treatment monitoring [206] (Fig. 9.1). The proposed approach is designed to help predict short-term progression of ILD irrespective of biologic therapy. In patients at higher risk of progression, even in patients who appear to have stable lung disease over a one- or two-year period, treatment decisions should involve a multidisciplinary approach including a respiratory physician as well as a careful discussion with the patient regarding the benefits and risks of treatment options available.
Suggested algorithm for assessment, monitoring and management of patients with RA- ILD on biologic therapy. Case-by-case decisions about commencing biologic therapy are required, informed by baseline assessments. For example, a patient with HRCT-detected UIP affecting 30% of lung fields and with a DLCO 40% of predicted is likely to experience disease progression and to have limited capacity to withstand a respiratory insult. Conversely, a clinician might be more reassured if their patient has 5% of lung fields involved, with NSIP detected using HRCT, and a 12-month decline in DLCO of only 5%. Abbreviations: AFB acid-fast bacilli; DLCO diffusion capacity of the lung for carbon monoxide; FVC forced vital capacity; HRCT high-resolution CT; NSIP nonspecific interstitial pneumonia; PFTs pulmonary function tests; RA-ILD rheumatoid arthritis-associated interstitial lung disease; UIP usual interstitial pneumonia. Initially published in Nature Reviews Rheumatology 2014. Jani M, Hirani N, Matteson EL, Dixon WG. The safety of biologic therapies in RA-associated interstitial lung disease. Nat Rev Rheumatol. 2014;10(5):284–94 [206]
Considerations of Post-Treatment
In all patients, including those with self-limiting and stable RA-ILD on treatment for their joint disease, rheumatologists should prompt questioning of new or evolving respiratory symptoms at follow-up, as patients may not spontaneously disclose such information. All patients who smoke should be educated about the important associated risks. Whilst being implicated in the pathogenesis of RA-ILD, it may also lead to deterioration of lung disease and is associated with higher joint disease activity and reduction in the effectiveness of medications such as MTX and TNFi drugs [207]. Smoking cessation advice and further support such as nicotine replacement therapy should be made available for all patients with RA-ILD [159]. Following an adequate period of monitored observation, classification of the trajectory of RA-ILD may be possible in the individual patient. In patients in whom a 12–24-month period of stability is observed, PFT follow-up intervals can be extended to 12 monthly.
Responses to Decreasing Lung Function
Routine monitoring of PFTs is suggested every 3–6 months in individuals at high risk of progression of RA-ILD or on any biologic drug [206]. An observed decline following serial PFTs could be due to progression of RA-ILD, either its natural history or accelerated by therapy or attributable to other causes that may or may not have an association with the DMARD prescribed. ‘Reversible’ decline has been categorised into potentially reversible with risk of irreversible disease (e.g. cases of drug-induced lung disease) or reversible disease with risk of progression (e.g. RA-cellular NSIP, some RA-fibrotic NSIP, RA-organising pneumonia) [143]. Management strategy for the former would involve cessation of the putative drug with or without further treatment with glucocorticoids if required, whilst the latter may require more prolonged therapy and monitoring. In practice, the two are difficult to delineate given their similar presentations, and therefore rheumatologists faced with such patients demonstrating worsening respiratory symptoms or lung function should consult with respiratory colleagues early. If the deterioration in clinical picture is found to be due to progression of RA-ILD, the decision to continue any DMARD, but especially bDMARDs or tsDMARDs, necessitates clinical decisions on a case-to-case basis. The choice of whether to continue with effective DMARD therapy for joint disease or the risk of potential pulmonary toxicity may be based on the perceived likelihood that the DMARD in question is driving deterioration (e.g. temporal relationship of starting the drug with the clinical scenario). Currently there is no observational evidence that preferentially switching between biologics, for instance, helps prolong survival or stabilises the disease; however, this may be tried in individuals that require management of their articular disease following careful discussion. In patients deemed to have progressive, irreversible disease, management of patients with RA-ILD in a joint pulmonary and rheumatology clinic should be especially considered where possible, with attempts made at stabilisation. In all patients, and especially in those with multimorbidity, conservative and nonpharmacological options that may be worth exploring include education, psychological support, pulmonary rehabilitation and supplemental oxygen if appropriate [143, 159, 208].
Serious Respiratory Adverse Events Following Treatment
SRAEs following treatments for RA may be due to incidence/exacerbation of RA-ILD or due to other reported pulmonary complications summarised in Table 9.4. Careful consideration of the underlying aetiology of SRAEs is essential, as deterioration in chest symptoms may not be due to pneumonitis or progression of ILD, which has been the focus of review in this chapter. A thorough investigation of common and opportunistic infections is imperative in patients with RA, especially on high glucocorticoid doses, certain nbDMARDs, bDMARDs and tsDMARDs. A full review of infection risk and biologics is beyond the scope of this chapter, as has been extensively reviewed recently [209, 210]. Rare reports of pulmonary manifestations of certain drugs have also been reported in the literature and are summarised in Table 9.4. For instance, lymphoproliferative disease (including non-Hodgkin lymphoma) have been described during treatment with MTX and may regress following cessation [211, 212]. TNFis have been associated with paradoxical AEs (associated with the treatment and possible induction of the same event) such as sarcoidosis and vasculitis [48]. The authors recommend a low threshold for withholding treatment with such cases, close liaison with respiratory and infectious disease physicians and imaging using HRCT, which in turn may help determine the cause of the deterioration.
Conclusions
The respiratory safety of RA therapy is an important consideration whilst deciding on the best treatment for patients with RA with active joint disease and coexisting ILD. This chapter summarises the current evidence available of the use of DMARDs in the context of pulmonary toxicity. However several limitations of the existing literature exist. Whilst RA-ILD is increasingly recognised, its natural history is still poorly understood. With newer treatments, case reports are helpful to identify a signal for concern, although such case reports are insufficient alone to provide a clear picture of drug toxicity. Where observational evidence is available, confounding by indication and channelling to certain treatments may limit robust conclusions. The lack of adequate comparator groups in several retrospective studies may further limit inferences drawn from the evidence. It appears that legitimate concerns are associated with several therapies; therefore, involving patients and multidisciplinary teams in such decisions is important. Careful discussion of the benefits and harms of treatments is encouraged, although this is made more challenging by the uncertainty of the current safety profile.
Systematic pre- and post-treatment assessment can help identify the trajectory of patients with RA-ILD and enable more effective risk stratification, enabling clinicians and patients to make better-informed decisions. Unfortunately at present, there are limited therapeutic options for additional treatment for specifically stabilising or reversing established fibrosis; however, emerging treatments such as novel anti-fibrotics may hold promise. Given the current evidence base, the decision to start an DMARD in patients with RA who have ILD should be based on its potential for improving joint disease, individual patient characteristics, patient education about the known risks and benefits of treatment and multidisciplinary team input.
References
Aletaha D, Neogi T, Silman AJ, et al. Rheumatoid arthritis classification criteria: an American College of Rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580–8.
Smolen JS, Breedveld FC, Burmester GR, et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis. 2016;75:3–15.
Smolen JS, Landewé R, Breedveld FC, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis. 2014;73:492–509.
Acute lymphocytic leukemia in children: maintenance therapy with methotrexate administered intermittently. Acute Leukemia Group B. JAMA. 1969;207:923–8.
Cannon GW, Ward JR, Clegg DO, et al. Acute lung disease associated with low-dose pulse methotrexate therapy in patients with rheumatoid arthritis. Arthritis Rheum. 1983;26:1269–74.
Imokawa S, Colby TV, Leslie KO, et al. Methotrexate pneumonitis: review of the literature and histopathological findings in nine patients. Eur Respir J. 2000;15:373–81.
Dawson JK, Graham DR, Desmond J, et al. Investigation of the chronic pulmonary effects of low-dose oral methotrexate in patients with rheumatoid arthritis: a prospective study incorporating HRCT scanning and pulmonary function tests. Rheumatology (Oxford). 2002;41:262–7.
Salliot C, van der Heijde D. Long-term safety of methotrexate monotherapy in patients with rheumatoid arthritis: a systematic literature research. Ann Rheum Dis. 2009;68:1100–4.
Sathi N, Chikura B, Kaushik VV, et al. How common is methotrexate pneumonitis? A large prospective study investigates. Clin Rheumatol. 2012;31:79–83.
Searles G, McKendry RJ. Methotrexate pneumonitis in rheumatoid arthritis: potential risk factors. Four case reports and a review of the literature. J Rheumatol. 1987;14:1164–71.
Carson CW, Cannon GW, Egger MJ, et al. Pulmonary disease during the treatment of rheumatoid arthritis with low dose pulse methotrexate. Semin Arthritis Rheum. 1987;16:186–95.
Kremer JM, Alarcón GS, Weinblatt ME, et al. Clinical, laboratory, radiographic, and histopathologic features of methotrexate-associated lung injury in patients with rheumatoid arthritis: a multicenter study with literature review. Arthritis Rheum. 1997;40:1829–37.
Arakawa H, Yamasaki M, Kurihara Y, et al. Methotrexate-induced pulmonary injury: serial CT findings. J Thorac Imaging. 2003;18:231–6.
Fuhrman C, Parrot A, Wislez M, et al. Spectrum of CD4 to CD8 T-cell ratios in lymphocytic alveolitis associated with methotrexate-induced pneumonitis. Am J Respir Crit Care Med. 2001;164:1186–91.
Schnabel A, Richter C, Bauerfeind S, et al. Bronchoalveolar lavage cell profile in methotrexate induced pneumonitis. Thorax. 1997;52:377–9.
Carroll GJ, Thomas R, Phatouros CC, et al. Incidence, prevalence and possible risk factors for pneumonitis in patients with rheumatoid arthritis receiving methotrexate. J Rheumatol. 1994;21:51–4.
Ameen M, Taylor DA, Williams IP, et al. Pneumonitis complicating methotrexate therapy for pustular psoriasis. J Eur Acad Dermatol Venereol. 2001;15:247–9.
Conway R, Low C, Coughlan RJ, et al. Methotrexate use and risk of lung disease in psoriasis, psoriatic arthritis, and inflammatory bowel disease: systematic literature review and meta-analysis of randomised controlled trials. BMJ. 2015;350:h1269.
Alarcon GS, Kremer JM, Macaluso M, et al. Risk factors for methotrexate-induced lung injury in patients with rheumatoid arthritis: a multicenter, case-control study. Ann Intern Med. 1997;127:356.
Saravanan V, Kelly CA. Reducing the risk of methotrexate pneumonitis in rheumatoid arthritis. Rheumatology. 2003;43:143–7.
Cottin V, Tébib J, Massonnet B, et al. Pulmonary function in patients receiving long-term low-dose methotrexate. Chest. 1996;109:933–8.
Howes M, Tose J, White C, et al. Can baseline pulmonary function tests predict pulmonary toxicity in patients receiving methotrexate for rheumatoid arthritis? Intern Med. 1999;7:51–4.
Rojas-Serrano J, González-Velásquez E, Mejía M, et al. Interstitial lung disease related to rheumatoid arthritis: evolution after treatment. Reumatol Clin. 2012;8:68–71.
Ito S, Sumida T. Interstitial lung disease associated with leflunomide. Intern Med. 2004;43:1103–4.
McCurry J. Japan deaths spark concerns over arthritis drug. Lancet. 2004;363:461.
JH J, Kim S-I, Lee J-H, et al. Risk of interstitial lung disease associated with leflunomide treatment in Korean patients with rheumatoid arthritis. Arthritis Rheum. 2007;56(6):2094.
Kamata Y, Nara H, Kamimura T, et al. Rheumatoid arthritis complicated with acute interstitial pneumonia induced by leflunomide as an adverse reaction. Intern Med. 2004;43:1201–4.
Ochi S, Harigai M, Mizoguchi F, et al. Leflunomide-related acute interstitial pneumonia in two patients with rheumatoid arthritis: autopsy findings with a mosaic pattern of acute and organizing diffuse alveolar damage. Mod Rheumatol. 2006;16:316–5.
Savage RL, Highton J, Boyd IW, et al. Pneumonitis associated with leflunomide: a profile of New Zealand and Australian reports. Intern Med J. 2006;36:162–9.
Chikura B, Lane S, Dawson JK. Clinical expression of leflunomide-induced pneumonitis. Rheumatology (Oxford). 2009;48:1065–8.
Suissa S, Hudson M, Ernst P. Leflunomide use and the risk of interstitial lung disease in rheumatoid arthritis. Arthritis Rheum. 2006;54:1435–9.
Sawada T, Inokuma S, Sato T, et al. Leflunomide-induced interstitial lung disease: prevalence and risk factors in Japanese patients with rheumatoid arthritis. Rheumatology (Oxford). 2009;48:1069–72.
Roubille C, Haraoui B. Interstitial lung diseases induced or exacerbated by DMARDS and biologic agents in rheumatoid arthritis: a systematic literature review. Semin Arthritis Rheum. 2014;43:613–26.
Furukawa H, Oka S, Shimada K, et al. HLA-A*31:01 and methotrexate-induced interstitial lung disease in Japanese rheumatoid arthritis patients: a multidrug hypersensitivity marker? Ann Rheum Dis. 2013;72:153–5.
Hyeon Ju J, Kim S-I, Lee J-H, et al. Risk of interstitial lung disease associated with leflunomide treatment in Korean patients with rheumatoid arthritis. Arthritis Rheum. 2007;56(6):2094.
Sato T, Inokuma S, Sagawa A, et al. Factors associated with fatal outcome of leflunomide-induced lung injury in Japanese patients with rheumatoid arthritis. Rheumatology (Oxford). 2009;48:1265–8.
Nadarajan P, Fabre A, Kelly E. Sulfasalazine: a rare cause of acute eosinophilic pneumonia. Respir Med Case Rep. 2016;18:35–6.
Haroon M, Harney S. A case of severe pulmonary infiltration with eosinophilia (PIE) syndrome induced by sulphasalazine. Int J Rheum Dis. 2012;15:e150–2.
Yamakado S, Yoshida Y, Yamada T, et al. Pulmonary infiltration and eosinophilia associated with sulfasalazine therapy for ulcerative colitis: a case report and review of literature. Intern Med. 1992;31:108–13.
Parry SD, Barbatzas C, Peel ET, et al. Sulphasalazine and lung toxicity. Eur Respir J. 2002;19:756–64.
Michel F, Navellou J-C, Ferraud D, et al. DRESS syndrome in a patient on sulfasalazine for rheumatoid arthritis. Joint Bone Spine. 2005;72(1):82–5.
Gutierrez M, Filippucci E, Bugatti L, et al. Severe drug hypersensitivity syndrome due to sulphasalazine in patient with rheumatoid arthritis. Reumatismo. 2009;61:65–8.
de Lauretis A, Veeraraghavan S, Renzoni E. Review series: aspects of interstitial lung disease: connective tissue disease-associated interstitial lung disease: how does it differ from IPF? How should the clinical approach differ? Chron Respir Dis. 2011;8:53–82.
Català Pérez R, Azón Masoliver A, Hernández Flix S. Interstitial lung disease induced by hydroxychloroquine. Med Clín. 2015;145:415–6.
Schmutz J, Barbaud A, Tréchot P. Hydroxychloroquine and DRESS. Ann Dermatol Venereol. 2008;135:903.
Volpe A, Marchetta A, Caramaschi P, et al. Hydroxychloroquine-induced DRESS syndrome. Clin Rheumatol. 2008;27:537–9.
Braun S, Ferner M, Kronfeld K, et al. Hydroxychloroquine in children with interstitial (diffuse parenchymal) lung diseases. Pediatr Pulmonol. 2015;50:410–9.
Perez-Alvarez R, Pérez-de-Lis M, Ramos-Casals M. Biologics-induced autoimmune diseases. Curr Opin Rheumatol. 2013;25:56–64.
Ramos-Casals M, Brito-Zerón P, Muñoz S, et al. Autoimmune diseases induced by TNF-targeted therapies: analysis of 233 cases. Medicine (Baltimore). 2007;86:242–51.
Thrall RS, Vogel SN, Evans R, et al. Role of tumor necrosis factor-alpha in the spontaneous development of pulmonary fibrosis in viable motheaten mutant mice. Am J Pathol. 1997;151:1303–10.
Piguet PF, Ribaux C, Karpuz V, et al. Expression and localization of tumor necrosis factor-alpha and its mRNA in idiopathic pulmonary fibrosis. Am J Pathol. 1993;143:651–5.
Hiraga J, Kondoh Y, Taniguchi H, et al. A case of interstitial pneumonia induced by rituximab therapy. Int J Hematol. 2005;81:169–70.
Maini R, St Clair EW, Breedveld F, et al. Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial. ATTRACT study group. Lancet. 1999;354:1932–9.
Bathon JM, Martin RW, Fleischmann RM, et al. A comparison of etanercept and methotrexate in patients with early rheumatoid arthritis. N Engl J Med. 2000;343:1586–93.
Genovese MC, Bathon JM, Martin RW, et al. Etanercept versus methotrexate in patients with early rheumatoid arthritis: two-year radiographic and clinical outcomes. Arthritis Rheum. 2002;46:1443–50.
Genovese MC, Bathon JM, Fleischmann RM, et al. Longterm safety, efficacy, and radiographic outcome with etanercept treatment in patients with early rheumatoid arthritis. J Rheumatol. 2005;32:1232–42.
Moreland LW, Weinblatt ME, Keystone EC, et al. Etanercept treatment in adults with established rheumatoid arthritis: 7 years of clinical experience. J Rheumatol. 2006;33:854–61.
Breedveld FC, Weisman MH, Kavanaugh AF, et al. The PREMIER study: a multicenter, randomized, double-blind clinical trial of combination therapy with adalimumab plus methotrexate versus methotrexate alone or adalimumab alone in patients with early, aggressive rheumatoid arthritis who had not had previo. Arthritis Rheum. 2006;54:26–37.
Burmester GR, Mariette X, Montecucco C, et al. Adalimumab alone and in combination with disease-modifying antirheumatic drugs for the treatment of rheumatoid arthritis in clinical practice: the research in active rheumatoid arthritis (ReAct) trial. Ann Rheum Dis. 2007;66:732–9.
Emery P, Fleischmann RM, Moreland LW, et al. Golimumab, a human anti-tumor necrosis factor alpha monoclonal antibody, injected subcutaneously every four weeks in methotrexate-naive patients with active rheumatoid arthritis: twenty-four-week results of a phase III, multicenter, randomized, double-bli. Arthritis Rheum. 2009;60:2272–83.
Keystone EC, Genovese MC, Klareskog L, et al. Golimumab, a human antibody to tumour necrosis factor {alpha} given by monthly subcutaneous injections, in active rheumatoid arthritis despite methotrexate therapy: the GO-FORWARD study. Ann Rheum Dis. 2009;68:789–96.
Smolen JS, Kay J, Landewé RBM, et al. Golimumab in patients with active rheumatoid arthritis who have previous experience with tumour necrosis factor inhibitors: results of a long-term extension of the randomised, double-blind, placebo-controlled GO-AFTER study through week 160. Ann Rheum Dis. 2012;71:1671–9.
Smolen JS, Kay J, Doyle M, et al. Golimumab in patients with active rheumatoid arthritis after treatment with tumor necrosis factor α inhibitors: findings with up to five years of treatment in the multicenter, randomized, double-blind, placebo-controlled, phase 3 GO-AFTER study. Arthritis Res Ther. 2015;17:14.
Keystone E, Van Der HD, Mason D, et al. Certolizumab pegol plus methotrexate is significantly more effective than placebo plus methotrexate in active rheumatoid arthritis: findings of a fifty-two-week, phase III, multicenter, randomized, double-blind, placebo-controlled, parallel-group study. Arthritis Rheum. 2008;58:3319–29.
Smolen J, Landewé RB, Mease P, et al. Efficacy and safety of certolizumab pegol plus methotrexate in active rheumatoid arthritis: the RAPID 2 study. A randomised controlled trial. Ann Rheum Dis. 2009;68:797–804.
Keystone E, Landewé R, van Vollenhoven R, et al. Long-term safety and efficacy of certolizumab pegol in combination with methotrexate in the treatment of rheumatoid arthritis: 5-year results from the RAPID 1 trial and open-label extension. Ann Rheum Dis. 2014;73:2094–100.
Ostor AJK, Crisp AJ, Somerville MF, et al. Fatal exacerbation of rheumatoid arthritis associated fibrosing alveolitis in patients given infliximab. BMJ. 2004;329:1266.
Ostör AJK, Chilvers ER, Somerville MF, et al. Pulmonary complications of infliximab therapy in patients with rheumatoid arthritis. J Rheumatol. 2006;33:622–8.
Perez-Alvarez R, Perez-de-Lis M, Diaz-Lagares C, et al. Interstitial lung disease induced or exacerbated by TNF-targeted therapies: analysis of 122 cases. Semin Arthritis Rheum. 2011;41:256–64.
Pearce F, Johnson SR, Courtney P. Interstitial lung disease following certolizumab pegol. Rheumatology. 2012;51:578–80.
Glaspole IN, Hoy RF, Ryan PF. A case of certolizumab-induced interstitial lung disease in a patient with rheumatoid arthritis. Rheumatology. 2013;9:9.
Lager J, Hilberg O, Lokke A, et al. Severe interstitial lung disease following treatment with certolizumab pegol: a case report. Eur Respir Rev. 2013;22:414–6.
Migita K, Tsuji Y, Hisatomi K, et al. Acute exacerbation of rheumatoid interstitial lung disease during the maintenance therapy with certolizumab pegol. Mod Rheumatol. 2015;27:1079–82.
Hadjinicolaou AV, Nisar MK, Bhagat S, et al. Non-infectious pulmonary complications of newer biological agents for rheumatic diseases—a systematic literature review. Rheumatology. 2011;50:2297–305.
Millar A, McKew J, Taggart A. Fatal fibrosing alveolitis with certolizumab. Rheumatology (Oxford). 2012;51(5):953.
Bargagli E, Galeazzi M, Rottoli P. Infliximab treatment in a patient with rheumatoid arthritis and pulmonary fibrosis. Eur Respir J. 2004;24:708.
Vassallo R, Matteson EL, Thomas CJ. Clinical response of rheumatoid arthritis-associated pulmonary fibrosis to tumor necrosis factor-alpha inhibition. Chest. 2002;122:1093–6.
Antoniou KM, Mamoulaki M, Malagari K, et al. Infliximab therapy in pulmonary fibrosis associated with collagen vascular disease. Clin Exp Rheumatol. 2007;25:23–8.
Wolfe F, Caplan L, Michaud K. Rheumatoid arthritis treatment and the risk of severe interstitial lung disease. Scand J Rheumatol. 2007;36:172–8.
Herrinton LJ, Harrold LR, Liu L, et al. Association between anti-TNF-alpha therapy and interstitial lung disease. Pharmacoepidemiol Drug Saf. 2013;22:394–402.
Curtis JR, Sarsour K, Napalkov P, et al. Incidence and complications of interstitial lung disease in users of tocilizumab, rituximab, abatacept and anti-tumor necrosis factor α agents, a retrospective cohort study. Arthritis Res Ther. 2015;17:319.
Nakashita T, Ando K, Kaneko N, et al. Potential risk of TNF inhibitors on the progression of interstitial lung disease in patients with rheumatoid arthritis. BMJ Open. 2014;4:e005615.
Dixon WG, Hyrich KL, Watson KD, et al. Influence of anti-TNF therapy on mortality in patients with rheumatoid arthritis-associated interstitial lung disease: results from the British Society for Rheumatology biologics register. Ann Rheum Dis. 2010;69:1086–91.
Dörner T, Strand V, Castañeda-Hernández G, et al. The role of biosimilars in the treatment of rheumatic diseases. Ann Rheum Dis. 2013;72:322–8.
Yoo DH, Hrycaj P, Miranda P, et al. A randomised, double-blind, parallel-group study to demonstrate equivalence in efficacy and safety of CT-P13 compared with innovator infliximab when coadministered with methotrexate in patients with active rheumatoid arthritis: the PLANETRA study. Ann Rheum Dis. 2013;72:1613–20.
Yoo DH, Racewicz A, Brzezicki J, et al. A phase III randomized study to evaluate the efficacy and safety of CT-P13 compared with reference infliximab in patients with active rheumatoid arthritis: 54-week results from the PLANETRA study. Arthritis Res Ther. 2015;18:82.
Park W, Hrycaj P, Jeka S, et al. A randomised, double-blind, multicentre, parallel-group, prospective study comparing the pharmacokinetics, safety, and efficacy of CT-P13 and innovator infliximab in patients with ankylosing spondylitis: the PLANETAS study. Ann Rheum Dis. 2013;72:1605–12.
Yoo DH, Prodanovic N, Jaworski J, et al. Efficacy and safety of CT-P13 (biosimilar infliximab) in patients with rheumatoid arthritis: comparison between switching from reference infliximab to CT-P13 and continuing CT-P13 in the PLANETRA extension study. Ann Rheum Dis. 2016;13:2015–208786.
Park W, Yoo DH, Miranda P, et al. Efficacy and safety of switching from reference infliximab to CT-P13 compared with maintenance of CT-P13 in ankylosing spondylitis: 102-week data from the PLANETAS extension study. Ann Rheum Dis. 2016;76(2):346–54.
Emery P, Vencovský J, Sylwestrzak A, et al. A phase III randomised, double-blind, parallel-group study comparing SB4 with etanercept reference product in patients with active rheumatoid arthritis despite methotrexate therapy. Ann Rheum Dis. 2015;2015:207588.
Liote H, Liote F, Seroussi B, et al. Rituximab-induced lung disease: a systematic literature review. Eur Respir J. 2010;35:681–7.
Wagner SA, Mehta AC, Laber DA. Rituximab-induced interstitial lung disease. Am J Hematol. 2007;82:916–9.
Naqibullah M, Shaker SB, Bach KS, et al. Rituximab-induced interstitial lung disease: five case reports. Eur Clin Respir J. 2015;21:2.
Atzeni F, Boiardi L, Sallì S, et al. Lung involvement and drug-induced lung disease in patients with rheumatoid arthritis. Expert Rev Clin Immunol. 2013;9:649–57.
Haraoui B, Bokarewa M, Kallmeyer I, et al. Safety and effectiveness of rituximab in patients with rheumatoid arthritis following an inadequate response to 1 prior tumor necrosis factor inhibitor: the RESET trial. J Rheumatol. 2011;38:2548–56.
Emery P, Fleischmann R, Filipowicz-Sosnowska A, et al. The efficacy and safety of rituximab in patients with active rheumatoid arthritis despite methotrexate treatment: results of a phase IIB randomized, double-blind, placebo-controlled, dose-ranging trial. Arthritis Rheum. 2006;54:1390–400.
Emery P, Deodhar A, Rigby WF, et al. Efficacy and safety of different doses and retreatment of rituximab: a randomised, placebo-controlled trial in patients who are biological naive with active rheumatoid arthritis and an inadequate response to methotrexate. Ann Rheum Dis. 2010;69:1629–35.
Mease PJ, Cohen S, Gaylis NB, et al. Efficacy and safety of retreatment in patients with rheumatoid arthritis with previous inadequate response to tumor necrosis factor inhibitors: results from the SUNRISE trial. J Rheumatol. 2010;37:917–27.
Edwards JC, Szczepanski L, Szechinski J, et al. Efficacy of B-cell-targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med. 2004;350:2572–81.
Hadjinicolaou AV, Nisar MK, Parfrey H, et al. Non-infectious pulmonary toxicity of rituximab: a systematic review. Rheumatology. 2012;51:653–62.
Weinblatt ME, Moreland LW, Westhovens R, et al. Safety of abatacept administered intravenously in treatment of rheumatoid arthritis: integrated analyses of up to 8 years of treatment from the abatacept clinical trial program. J Rheumatol. 2013;40:787–97.
Doğu B, Atilla N, Çetin G, et al. A case of acute respiratory failure in a rheumatoid arthritis patient after the administration of abatacept. Eur J Rheumatol. 2015;3(3):134–5.
Takuma WADA, Yuji A, Kazuhiro Y, Kojiro S, et al. A case of rheumatoid arthritis complicated with deteriorated interstitial pneumonia after the administration of abatacept. J Clin Immunol. 2012;35:433–8.
Hayes F, Ostor A. Refractory rheumatoid arthritis with interstitial lung disease: could abatacept be the answer? Rheumatology. 2014;53((Suppl 1)):i65.
Motojima S, Nakashita T, Jibatake A, et al. Abatacept can be used safely for RA patients with interstitial lung disease. Arthritis Rheum. 2014;66(10 Suppl.) Abstract 472.
Yun H, Xie F, Delzell E, et al. Risk of hospitalised infection in rheumatoid arthritis patients receiving biologics following a previous infection while on treatment with anti-TNF therapy. Ann Rheum Dis. 2015;74:1065–71.
Singh JA, Saag KG, Bridges SL, et al. American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol. 2015;68(1):1–26.
Dougados M, Kissel K, Sheeran T, et al. Adding tocilizumab or switching to tocilizumab monotherapy in methotrexate inadequate responders: 24-week symptomatic and structural results of a 2-year randomised controlled strategy trial in rheumatoid arthritis (ACT-RAY). Ann Rheum Dis. 2013;72:43–50.
Kaneko Y, Atsumi T, Tanaka Y, et al. Comparison of adding tocilizumab to methotrexate with switching to tocilizumab in patients with rheumatoid arthritis with inadequate response to methotrexate: 52-week results from a prospective, randomised, controlled study (SURPRISE study). Ann Rheum Dis. 2016;0:1–7.
Moodley YP, Misso NLA, Scaffidi AK, et al. Inverse effects of interleukin-6 on apoptosis of fibroblasts from pulmonary fibrosis and normal lungs. Am J Respir Cell Mol Biol. 2003;29:490–8.
Nishimoto N, Yoshizaki K, Miyasaka N, et al. Treatment of rheumatoid arthritis with humanized anti-interleukin-6 receptor antibody: a multicenter, double-blind, placebo-controlled trial. Arthritis Rheum. 2004;50:1761–9.
Smolen JS, Beaulieu A, Rubbert-Roth A, et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet. 2008;371:987–97.
Nishimoto N, Miyasaka N, Yamamoto K, et al. Study of active controlled tocilizumab monotherapy for rheumatoid arthritis patients with an inadequate response to methotrexate (SATORI): significant reduction in disease activity and serum vascular endothelial growth factor by IL-6 receptor inhibition. Mod Rheumatol. 2009;19:12–9.
Gabay C, Emery P, van Vollenhoven R, et al. Tocilizumab monotherapy versus adalimumab monotherapy for treatment of rheumatoid arthritis (ADACTA): a randomised, double-blind, controlled phase 4 trial. Lancet. 2013;381:1541–50.
Burmester GR, Rubbert-Roth A, Cantagrel A, et al. Efficacy and safety of subcutaneous tocilizumab versus intravenous tocilizumab in combination with traditional DMARDs in patients with RA at week 97 (SUMMACTA). Ann Rheum Dis. 2016;75:68–74.
Huizinga TWJ, Fleischmann RM, Jasson M, et al. Sarilumab, a fully human monoclonal antibody against IL-6Rα in patients with rheumatoid arthritis and an inadequate response to methotrexate: efficacy and safety results from the randomised SARIL-RA-MOBILITY part a trial. Ann Rheum Dis. 2014;73:1626–34.
Genovese MC, Fleischmann R, Kivitz AJ, et al. Sarilumab plus methotrexate in patients with active rheumatoid arthritis and inadequate response to methotrexate: results of a phase III study. Arthritis Rheumatol. 2015;67:1424–37.
Ikegawa K, Hanaoka M, Ushiki A, et al. A case of organizing pneumonia induced by tocilizumab. Intern Med. 2011;50:2191–3.
Kawashiri SY, Kawakami A, Sakamoto N, et al. A fatal case of acute exacerbation of interstitial lung disease in a patient with rheumatoid arthritis during treatment with tocilizumab. Rheumatol Int. 2012;32:4023–6.
Wendling D, Vidon C, Godfrin-Valnet M, et al. Exacerbation of combined pulmonary fibrosis and emphysema syndrome during tocilizumab therapy for rheumatoid arthritis. Joint Bone Spine. 2013;22:71–9.
Sangüesa G, Flores R, Jara C, et al. Acute pneumonitis in a patient with adult-onset disease after toclizumab treatment with good response to anakinra. Reumatol Clin. 2016;12(6):345–7. [Epub ahead of print].
Mohr M, Jacobi AM. Interstitial lung disease in rheumatoid arthritis: response to IL-6R blockade. Scand J Rheumatol. 2011;40:400–1.
Koike T, Harigai M, Inokuma S, et al. Postmarketing surveillance of tocilizumab for rheumatoid arthritis in Japan: interim analysis of 3881 patients. Ann Rheum Dis. 2011;70:2148–51.
Akiyama M, Kaneko Y, Yamaoka K, et al. Association of disease activity with acute exacerbation of interstitial lung disease during tocilizumab treatment in patients with rheumatoid arthritis: a retrospective, case–control study. Rheumatol Int. 2016;36:881–9.
Drevlow BE, Lovis R, Haag MA, et al. Recombinant human interleukin-1 receptor type I in the treatment of patients with active rheumatoid arthritis. Arthritis Rheum. 1996;39:257–65.
Campion GV, Lebsack ME, Lookabaugh J, et al. Dose-range and dose-frequency study of recombinant human interleukin-1 receptor antagonist in patients with rheumatoid arthritis. The IL-1Ra arthritis study group. Arthritis Rheum. 1996;39:1092–101.
Bresnihan B, Alvaro-Gracia JM, Cobby M, et al. Treatment of rheumatoid arthritis with recombinant human interleukin-1 receptor antagonist. Arthritis Rheum. 1998;41:2196–204.
Cohen S, Hurd E, Cush J, et al. Treatment of rheumatoid arthritis with anakinra, a recombinant human interleukin-1 receptor antagonist, in combination with methotrexate: results of a twenty-four-week, multicenter, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2002;46:614–24.
Scott IC, Ibrahim F, Simpson G, et al. A randomised trial evaluating anakinra in early active rheumatoid arthritis. Clin Exp Rheumatol. 2016;34:88–93.
Genovese MC, Cohen S, Moreland L, et al. Combination therapy with Etanercept and Anakinra in the treatment of patients with rheumatoid arthritis who have been treated unsuccessfully with methotrexate. Arthritis Rheum. 2004;50:1412–9.
Smolen JS, van der Heijde D, Machold KP, et al. Proposal for a new nomenclature of disease-modifying antirheumatic drugs. Ann Rheum Dis. 2014;73:3–5.
Taylor P, Keystone E, Vanderheijde D. Baricitinib versus placebo or adalimumab in patients with active rheumatoid arthritis (RA) and an inadequate response to background methotrexate therapy: results of a phase 3 study. Arthritis Rheumatol. 2015;67(Suppl:L2).
van Vollenhoven RF, Fleischmann R, Cohen S, et al. Tofacitinib or adalimumab versus placebo in rheumatoid arthritis. N Engl J Med. 2012;367:508–19.
Burmester GR, Blanco R, Charles-Schoeman C, et al. Tofacitinib (CP-690,550) in combination with methotrexate in patients with active rheumatoid arthritis with an inadequate response to tumour necrosis factor inhibitors: a randomised phase 3 trial. Lancet. 2013;381:451–60.
Van Der Heijde D, Tanaka Y, Fleischmann R, et al. Tofacitinib (CP-690,550) in patients with rheumatoid arthritis receiving methotrexate: twelve-month data from a twenty-four-month phase III randomized radiographic study. Arthritis Rheum. 2013;65:559–70.
Fleischmann R, Kremer J, Cush J, et al. Placebo-controlled trial of tofacitinib monotherapy in rheumatoid arthritis. N Engl J Med. 2012;367:495–507.
Wollenhaupt J, Silverfield J, Lee EB, et al. Safety and efficacy of tofacitinib, an oral janus kinase inhibitor, for the treatment of rheumatoid arthritis in open-label, longterm extension studies. J Rheumatol. 2014;41:837–52.
He Y, Wong AY, Chan EW, et al. Efficacy and safety of tofacitinib in the treatment of rheumatoid arthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2013;14:298.
Keystone EC, Taylor PC, Drescher E, et al. Safety and efficacy of baricitinib at 24 weeks in patients with rheumatoid arthritis who have had an inadequate response to methotrexate. Ann Rheum Dis. 2015;74:333–40.
Genovese MC, Kremer J, Zamani O, et al. Baricitinib in patients with refractory rheumatoid arthritis. N Engl J Med. 2016;374:1243–52.
Food Drug Administration (FDA). Risk evaluation and mitigation strategy (REMS) NDA 203,214 XELJANZ® (Tofacitinib) 2015; http://www.fda.gov/downloads/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/UCM330290.pdf.
Kim EJ, Elicker BM, Maldonado F, et al. Usual interstitial pneumonia in rheumatoid arthritis-associated interstitial lung disease. Eur Respir J. 2010;35:1322–8.
Lake FR, Proudman SM. Rheumatoid arthritis and lung disease: from mechanisms to a practical approach. Semin Respir Crit Care Med. 2014;35:222–38.
Raghu G, Rochwerg B, Zhang Y, et al. An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis: an update of the 2011 clinical practice guideline. Am J Respir Crit Care Med. 2015;192:e3–19.
Krause LM, Zamora C, Vassallo R, et al. The lung disease of rheumatoid arthritis. Curr Respir Med Rev. 2015;11:119–29.
Raghu G, Depaso WJ, Cain K, et al. Azathioprine combined with prednisone in the treatment of idiopathic pulmonary fibrosis: a prospective double-blind, randomized, placebo-controlled clinical trial. Am Rev Respir Dis. 1991;144:291–6.
Idiopathic Pulmonary Fibrosis Clinical Research Network, Raghu G, Anstrom KJ, et al. Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med. 2012;366:1968–77.
Zamora-Legoff JA, Krause ML, Crowson CS, et al. Risk of serious infection in patients with rheumatoid arthritis-associated interstitial lung disease. Clin Rheumatol. 2016;35(10):2585–9.
Dixon WG, Abrahamowicz M, Beauchamp M-E, et al. Immediate and delayed impact of oral glucocorticoid therapy on risk of serious infection in older patients with rheumatoid arthritis: a nested case-control analysis. Ann Rheum Dis. 2012;71:1128–33.
Noble PW, Albera C, Bradford WZ, et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet. 2011;377:1760–9.
Taniguchi H, Ebina M, Kondoh Y, et al. Pirfenidone in idiopathic pulmonary fibrosis. Eur Respir J. 2010;35:821–9.
Noble PW, Albera C, Bradford WZ, et al. Pirfenidone for idiopathic pulmonary fibrosis: analysis of pooled data from three multinational phase 3 trials. Eur Respir J. 2016;47:243–53.
Nagai S, Hamada K, Shigematsu M, et al. Open-label compassionate use one year-treatment with pirfenidone to patients with chronic pulmonary fibrosis. Intern Med. 2002;41:1118–23.
Miura Y, Saito T, Fujita K, et al. Clinical experience with pirfenidone in five patients with scleroderma-related interstitial lung disease. Sarcoidosis Vasc Diffuse Lung Dis. 2014;31:235–8.
Udwadia ZF, Mullerpattan JB, Balakrishnan C, et al. Improved pulmonary function following pirfenidone treatment in a patient with progressive interstitial lung disease associated with systemic sclerosis. Lung India. 2015;32:50–2.
Huang H, Feng RE, Li S, et al. A case report: the efficacy of pirfenidone in a Chinese patient with progressive systemic sclerosis-associated interstitial lung disease: a CARE-compliant article. Medicine (Baltimore). 2016;95:e4113.
Khanna D, Albera C, Fischer A, et al. An open-label, phase II study of the safety and tolerability of pirfenidone in patients with scleroderma-associated interstitial lung disease: the LOTUSS trial. J Rheumatol. 2016;43(9):1672–9.
Dhooria S, Agarwal R, Gupta D. Is pirfenidone ready for use in non-idiopathic pulmonary fibrosis interstitial lung diseases? Lung India. 2015;32:4–5.
Iqbal K, Kelly C. Treatment of rheumatoid arthritis-associated interstitial lung disease: a perspective review. Ther Adv Musculoskelet Dis. 2015;7:247–67.
Phase ll Study of Pirfenidone in patients with RA-ILD. ClinicalTrials.gov Identifier: NCT02808871. 2016.
Huang J, Beyer C, Palumbo-Zerr K, et al. Nintedanib inhibits fibroblast activation and ameliorates fibrosis in preclinical models of systemic sclerosis. Ann Rheum Dis. 2016;75:883–90.
Collard HR, Ryu JH, Douglas WW, et al. Combined corticosteroid and cyclophosphamide therapy does not alter survival in idiopathic pulmonary fibrosis. Chest. 2004;125:2169–74.
Martinez FJ, McCune WJ. Cyclophosphamide for scleroderma lung disease. N Engl J Med. 2006;354:2707–9.
Tashkin DP, Elashoff R, Clements PJ, et al. Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med. 2006;354:2655–66.
Hoyles RK, Ellis RW, Wellsbury J, et al. A multicenter, prospective, randomized, double-blind, placebo-controlled trial of corticosteroids and intravenous cyclophosphamide followed by oral azathioprine for the treatment of pulmonary fibrosis in scleroderma. Arthritis Rheum. 2006;54:3962–70.
Roth MD, Tseng C-H, Clements PJ, et al. Predicting treatment outcomes and responder subsets in scleroderma-related interstitial lung disease. Arthritis Rheum. 2011;63:2797–808.
Nannini C, West CP, Erwin PJ, et al. Effects of cyclophosphamide on pulmonary function in patients with scleroderma and interstitial lung disease: a systematic review and meta-analysis of randomized controlled trials and observational prospective cohort studies. Arthritis Res Ther. 2008;10:R124.
Ota M, Iwasaki Y, Harada H, et al. Efficacy of intensive immunosuppression in exacerbated rheumatoid arthritis-associated interstitial lung disease. Mod Rheumatol. 2017;27(1):22–8.
Suwa A, Hirakata M, Satoh S, et al. Rheumatoid arthritis associated with methotrexate-induced pneumonitis: improvement with i.v. cyclophosphamide therapy. Clin Exp Rheumatol. 1999;17:355–8.
Moolman JA, Bardin PG, Rossouw DJ, et al. Cyclosporin as a treatment for interstitial lung disease of unknown aetiology. Thorax. 1991;46:592–5.
Grgic A, Lausberg H, Heinrich M, et al. Progression of fibrosis in usual interstitial pneumonia: serial evaluation of the native lung after single lung transplantation. Respiration. 2008;76:139–45.
Cavagna L, Caporali R, Abdì-Alì L, et al. Cyclosporine in anti-Jo1-positive patients with corticosteroid-refractory interstitial lung disease. J Rheumatol. 2013;40:484–92.
Kurita T, Yasuda S, Amengual O, et al. The efficacy of calcineurin inhibitors for the treatment of interstitial lung disease associated with polymyositis/dermatomyositis. Lupus. 2015;24:3–9.
Go DJ, Park JK, Kang EH, et al. Survival benefit associated with early cyclosporine treatment for dermatomyositis-associated interstitial lung disease. Rheumatol Int. 2016;36:125–31.
Saketkoo LA, Espinoza LR. Experience of mycophenolate mofetil in 10 patients with autoimmune-related interstitial lung disease demonstrates promising effects. Am J Med Sci. 2009;337:329–35.
Mendoza FA, Nagle SJ, Lee JB, et al. A prospective observational study of mycophenolate mofetil treatment in progressive diffuse cutaneous systemic sclerosis of recent onset. J Rheumatol. 2012;39:1241–7.
Shenoy PD, Bavaliya M, Sashidharan S, et al. Cyclophosphamide versus mycophenolate mofetil in scleroderma interstitial lung disease (SSc-ILD) as induction therapy: a single-centre, retrospective analysis. Arthritis Res Ther. 2016;18:123.
Fischer A, Brown KK, Du Bois RM, et al. Mycophenolate mofetil improves lung function in connective tissue disease-associated interstitial lung disease. J Rheumatol. 2013;40:640–6.
Tashkin DP, Roth MD, Clements PJ, et al. Mycophenolate mofetil versus oral cyclophosphamide in scleroderma-related interstitial lung disease (SLS II): a randomised controlled, double-blind, parallel group trial. Lancet Respir Med. 2016;4(9):708–19.
Swigris JJ, Olson AL, Fischer A, et al. Mycophenolate mofetil is safe, well tolerated, and preserves lung function in patients with connective tissue disease-related interstitial lung disease. Chest. 2006;130:30–6.
Eissa K, Palomino J. B-cell depletion salvage therapy in rapidly progressive dermatomyositis related interstitial lung disease. J La State Med Soc. 2016;168:99–100.
Sumida H, Asano Y, Tamaki Z, et al. Successful experience of rituximab therapy for systemic sclerosis-associated interstitial lung disease with concomitant systemic lupus erythematosus. J Dermatol. 2014;41:418–20.
Keir GJ, Maher TM, Hansell DM, et al. Severe interstitial lung disease in connective tissue disease: rituximab as rescue therapy. Eur Respir J. 2012;40:641–8.
Bosello SL, De Luca G, Rucco M, et al. Long-term efficacy of B cell depletion therapy on lung and skin involvement in diffuse systemic sclerosis. Semin Arthritis Rheum. 2015;44:428–36.
Matteson E, Bongartz T, Ryu JH, et al. Open-label, pilot study of the safety and clinical effects of rituximab in patients with rheumatoid arthritis associated interstitial pneumonia. Open J Rheumatol Autoimmune Dis. 2012;2:53–8.
Dass S, Atzeni F, Vital E, et al. Safety of rituximab in patients with rheumatoid arthritis and concomitant lung disease. Rheumatology. 2011;50:iii121. [abstract 205]
Kabia A, Yusof M, Dass S, et al. Efficacy and safety of rituximab in rheumatoid arthritis patients with concomitant interstitial lung disease: 10-year experience at single centre. Rheumatology. 2015;54:i86–suppl:1. [abstract 092]
Becerra E, Cambridge G, Leandro M. Safety and efficacy of rituximab in patients with rheumatoid arthritis and lung involvement. Arthritis Rheum. 2013;64:502. [abstract 502]
Druce K, Iqbal K, Watson K, et al. Mortality in patients with rheumatoid arthritis and interstitial lung disease treated with first line TNFi or rituximab therapies: results from the BSRBR-RA. Arthritis Rheumatol. 2016; [ACR abstract] Personal communication.
Buch MH, Smolen JS, Betteridge N, et al. Updated consensus statement on the use of rituximab in patients with rheumatoid arthritis. Ann Rheum Dis. 2011;70:909–20.
Yazdani A, Singer LG, Strand V, et al. Survival and quality of life in rheumatoid arthritis-associated interstitial lung disease after lung transplantation. J Heart Lung Transplant. 2014;33:514–20.
Cottin V. Pragmatic prognostic approach of rheumatoid arthritis-associated interstitial lung disease. Eur Respir J. 2010;35:1206–8.
Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733–48.
Ryerson CJ, Urbania TH, Richeldi L, et al. Prevalence and prognosis of unclassifiable interstitial lung disease. Eur Respir J. 2013;42:750–7.
Egan JJ, Martinez FJ, Wells AU, et al. Lung function estimates in idiopathic pulmonary fibrosis: the potential for a simple classification. Thorax. 2005;60:270–3.
Ley B, Ryerson CJ, Vittinghoff E, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med. 2012;156:684–91.
Stenton C. The MRC breathlessness scale. Occup Med. 2008;58:226–7.
Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824.
Danoff SK, Terry PB, Horton MR. A clinician’s guide to the diagnosis and treatment of interstitial lung diseases. South Med J. 2007;100:579–87.
Latsi PI, du Bois RM, Nicholson AG, et al. Fibrotic idiopathic interstitial pneumonia: the prognostic value of longitudinal functional trends. Am J Respir Crit Care Med. 2003;168:531–7. Epub 2003 Jun 5.
Hamblin MJ, Horton MR. Rheumatoid arthritis-associated interstitial lung disease: diagnostic dilemma. Pulm Med. 2011;2011:872120.
Flaherty KR, Thwaite EL, Kazerooni EA, et al. Radiological versus histological diagnosis in UIP and NSIP: survival implications. Thorax. 2003;58:143–8.
Goh NS, Desai SR, Veeraraghavan S, et al. Interstitial lung disease in systemic sclerosis: a simple staging system. Am J Respir Crit Care Med. 2008;177:1248–54.
Wells AU, Hogaboam CM. Update in diffuse parenchymal lung disease 2007. Am J Respir Crit Care Med. 2008;177:580–4.
Sathi N, Urwin T, Desmond S, et al. Patients with limited rheumatoid arthritis-related interstitial lung disease have a better prognosis than those with extensive disease. Rheumatology. 2011;50:620.
Jani M, Hirani N, Matteson EL, Dixon WG. The safety of biologic therapies in RA-associated interstitial lung disease. Nat Rev Rheumatol. 2014;10(5):284–94.
Saevarsdottir S, Wedrén S, Seddighzadeh M, et al. Patients with early rheumatoid arthritis who smoke are less likely to respond to treatment with methotrexate and tumor necrosis factor inhibitors: observations from the epidemiological investigation of rheumatoid arthritis and the Swedish rheumatology register cohorts. Arthritis Rheum. 2011;63:26–36.
O’Dwyer DN, Armstrong ME, Cooke G, et al. Rheumatoid arthritis (RA) associated interstitial lung disease (ILD). Eur J Intern Med. 2013;24:597–603.
Winthrop KL, Novosad SA, Baddley JW, et al. Opportunistic infections and biologic therapies in immune-mediated inflammatory diseases: consensus recommendations for infection reporting during clinical trials and postmarketing surveillance. Ann Rheum Dis. 2015;74(12):2107–16.
Lahiri M, Dixon WG. Risk of infection with biologic antirheumatic therapies in patients with rheumatoid arthritis. Best Pract Res Clin Rheumatol. 2015;29:290–305.
Hoshida Y, J-X X, Fujita S, et al. Lymphoproliferative disorders in rheumatoid arthritis: clinicopathological analysis of 76 cases in relation to methotrexate medication. J Rheumatol. 2007;34:322–31.
Rizzi R, Curci P, Delia M, et al. Spontaneous remission of ‘methotrexate-associated lymphoproliferative disorders’ after discontinuation of immunosuppressive treatment for autoimmune disease. Review of the literature. Med Oncol. 2009;26:1–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Jani, M., Dixon, W.G., Matteson, E.L. (2018). Management of the Rheumatoid Arthritis Patient with Interstitial Lung Disease. In: Fischer, A., Lee, J. (eds) Lung Disease in Rheumatoid Arthritis. Respiratory Medicine. Humana Press, Cham. https://doi.org/10.1007/978-3-319-68888-6_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-68888-6_9
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-68887-9
Online ISBN: 978-3-319-68888-6
eBook Packages: MedicineMedicine (R0)