Abstract
Coronary computed tomographic angiography (CCTA) is a powerful, noninvasive tool to evaluate coronary anatomy, plaque, and areas of stenosis in the coronary arteries. Technological advancements have now given CCTA diagnostic capabilities that approach those of invasive coronary angiography, which remains the gold standard for coronary artery imaging. CCTA is often used in an outpatient setting to evaluate for coronary artery disease as well as graft patency following coronary artery bypass. Recent studies have shown that CCTA can effectively rule out acute coronary syndrome in low to intermediate-risk patients, who present with suspicious chest pain. The use of CCTA is on the rise, and it is important to recognize its diagnostic capabilities not only related to the coronary arteries and heart, but also with respect to extracardiac structures.
Similar content being viewed by others
Keywords
- Pulmonary nodules
- Lung cancer
- Pneumonia
- Pulmonary emboli
- Pleural effusion
- Pericardial effusion
- Pericardial cyst
- Left atrial appendage
- Left atrial myxoma
- Aortic stenosis
- Aortic root aneurysm
- Sarcoidosis
- Thymic hyperplasia
- Hiatal hernia
- Thoracic aortic dissection
- Chronic transmural left ventricular MI
- Hepatic hemangioma
- Adrenal adenoma
- Abdominal aortic aneurysm
- Hepatic steatosis
- Thoracic fracture
11.1 Introduction
Coronary computed tomographic angiography (CCTA) is a powerful, noninvasive tool to evaluate coronary anatomy, plaque, and areas of stenosis in the coronary arteries. Technological advancements have now given CCTA diagnostic capabilities that approach those of invasive coronary angiography, which remains the gold standard for coronary artery imaging. CCTA is often used in an outpatient setting to evaluate for coronary artery disease as well as graft patency following coronary artery bypass. Recent studies have shown that CCTA can effectively rule out acute coronary syndrome in low to intermediate-risk patients, who present with suspicious chest pain. The use of CCTA is on the rise, and it is important to recognize its diagnostic capabilities not only related to the coronary arteries and heart, but also with respect to extracardiac structures.
To visualize each of the coronary vessels on CCTA, z-axis coverage must extend from the upper mediastinum to the upper abdomen. Depending on use of a wide or narrow field of view, this will include variable portions of the lungs, mediastinum, chest wall, thoracic spine, and abdomen. Not surprisingly, incidental findings will often be identified that may or may not be clinically significant. An incidental finding is classified as significant if it requires subsequent radiographic evaluation or therapeutic intervention.
Patients undergoing cardiac imaging are not necessarily representative of the general population because of the presence of cardiac disease, additional associated risk factors, and ongoing symptoms, all of which may affect the prevalence and types of clinically significant incidental findings.
In one of the earliest large studies to analyze incidental findings on cardiac electron beam CT in the context of calcium scoring, investigators found that 53% of all patients had one or more incidental findings [1]. Most incidental findings were limited to the heart or pericardium (38%). Extracardiac incidental findings included pneumonia (1.7%), pulmonary malignancy (0.1%), pleural disease (8.9%), esophageal carcinoma (0.06%), lymphadenopathy (4%), hiatal hernia (1%), hepatic tumors (2%), and spinal degenerative disease (5.4%). Regarding clinical significance, 9% of these findings required further evaluation, and only 1% resulted in therapeutic intervention.
More recent investigations with modern multi-detector CT scanners have found similar results, with a prevalence of significant findings as high as 23%. One important difference is that CCTA requires contrast administration, which enhances the ability to detect additional pathology such as pulmonary embolism and aortic dissection. For example, in a study looking at patients who underwent CCTA after coronary artery bypass grafts, incidental pulmonary embolism was found in 1.9% of patients in the immediate postoperative period.
There has been considerable debate about the necessity to look for and report incidental findings. Many studies have confirmed that incidental findings are common and have the potential to influence treatment; identifying such findings should be a component of the image interpretation.
11.2 Case 11.1
11.2.1 History
A 56-year-old male screened for coronary artery disease . History is significant for hypertension, hyperlipidemia, and family history of coronary artery disease.
11.2.2 Findings
There is a solitary pulmonary nodule in the left upper lobe of the lung measuring approximately 1 cm in diameter. There is no associated lymphadenopathy or calcification (Fig. 11.1).
11.2.3 Diagnosis
Incidental solitary pulmonary nodule.
11.2.4 Discussion
Solitary pulmonary nodules (SPN) are relatively common findings that must not be overlooked because they may represent malignancy. Most often, patients are asymptomatic, and these lesions are found incidentally or in screening studies for lung cancer in high-risk populations.
By definition, a pulmonary nodule is a discrete opacity that is less than 3 cm; any lesion that is greater than 3 cm is termed a mass. The differential diagnosis of a SPN is large and can be divided into benign and malignant etiologies. Benign causes include infection or abscess, inflammatory disease (e.g., sarcoidosis), vascular abnormalities (e.g., AVM, aneurysm), and benign neoplasms (e.g., hamartoma, lipoma, fibroma). Malignant causes include primary lung cancer or metastasis.
Certain radiographic features help to distinguish a benign versus malignant etiology of SPN. Several patterns of calcification are associated with a benign SPN including complete calcification, laminated calcification, popcorn calcification, and central calcification. Margins that are smooth and well defined are more likely benign. The growth rate of a SPN can be highly predictive of a benign or malignant cause. SPNs that double in less than 1 month usually have an infectious etiology. SPNs that are stable over 2 years are usually benign although ground glass nodules may have longer doubling times and those that double in less than 2 years (and greater than 1 month) are usually malignant.
Management of SPNs can be difficult because physicians must consider risks of further radiation from follow-up imaging and possible tissue sampling versus the likelihood of diagnosing or missing a lung cancer. The predictable growth rate of malignant and benign SPNs is the basis for the Fleischner Society recommendations for follow-up of lung nodules [2]. These recommendations outline scheduled CT follow-up, PET imaging, and/or biopsy based on the size of the SPN and risk stratification of the patient.
11.2.5 Pearls and Pitfalls
When available, prior imaging studies should be carefully studied to assess for changes in the size or morphology of any nodules. Solid nodules that are stable over 2 years or those that are completely calcified can be considered benign.
11.3 Case 11.2 Contributed by J. Lee and C. Smuclovisky
11.3.1 History
A 75-year-old male presented with new onset of left-sided chest pain.
11.3.2 Findings
There is a mass in the left upper lobe of the lungs infiltrating the adjacent mediastinum and with adenopathy (Fig. 11.2a–c).
(a) Axial. Left upper lobe adenocarcinoma infiltrating the mediastinum (double arrows). Left hilar metastatic lymph node (single arrow). (b) Axial. Delayed images again demonstrating the infiltrating tumor (arrows). (c) Axial. Metastatic adenopathy adjacent to the left subclavian artery and vein (arrow). (d) Axial. Incidental small lung cancer (different patient) adjacent to the right hilum with a metastatic lymph node (arrows). (e and f) Axial. Incidental 13-mm lung cancer (different patient) in the left upper lobe adjacent to the aortic arch. Lung window (f) demonstrating spiculated borders of the tumor (arrows). (g) Axial. Incidental 5.5-cm left upper lobe lung cancer (different patient) incidentally found on the cardiac CTA and previously missed on plain radiographs over a period of 3 years. Note that the tumor is posterior to a cardiac pacemaker and would be difficult to suspect on a plain radiograph (Murphy’s law)
11.3.3 Diagnosis
The diagnosis is adenocarcinoma of the lung.
11.3.4 Discussion
Lung cancer is the leading cause of cancer-related mortality in both men and women. The prevalence of lung cancer is second only to that of prostate cancer in men and breast cancer in women. Non-small cell lung cancer (NSCLC) accounts for approximately 75% of all lung cancers. NSCLC is divided further into adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Extracardiac findings are frequently encountered on cardiac CTA. Primary lung cancer typically appears as a noncalcified soft tissue mass with irregular or spiculated borders. The tumors have variable size and may be located anywhere in the thorax.
11.3.5 Pearls and Pitfalls
Careful attention to the extracardiac structures is of paramount importance in order not to miss reporting a neoplasm in the field of view.
11.4 Case 11.3
11.4.1 History
A 40-year-old male, who presented with chest pain after using cocaine .
11.4.2 Findings
There is a focal consolidation in the right middle lobe (Fig. 11.3).
11.4.3 Diagnosis
Pneumonia , possibly secondary to aspiration given patient’s history of drug abuse.
11.4.4 Discussion
Pneumonia develops when pathologic organisms invade lung parenchyma and initiate a host immune response. This manifests as inflammatory exudate in the airspaces, which causes the radiographic appearance of consolidation. Spread of organisms can occur through the airways via inhalation or aspiration, through vasculature (hematogenous spread) or by direct contact with infected adjacent structures such as the mediastinum or abdomen. Pneumonia can be caused by bacteria, viruses, fungi, and parasites. The integrity of the immune system plays an important role in the susceptibility of infections from various organisms.
There are three radiographic patterns of pneumonia : lobar, lobular or bronchopneumonia, and interstitial. Lobar pneumonia usually involves inflammation in the distal airways first, which then spreads proximally along the airways to involve the whole lobe. S. pneumoniae and Klebsiella pneumoniae often produce lobar pneumonia.
Lobular or bronchopneumonia is caused by inflammation in the bronchi, which then spreads distally to involve the pulmonary lobule. S. aureus and H. influenza often produce bronchopneumonia.
Interstitial pneumonia is caused by inflammation in the bronchioles and pulmonary interstitium, which causes radiographic thickening of airways and reticulonodular opacities. Viral infections and mycoplasma often produce interstitial pneumonia.
Although each organism has predilection for a specific radiographic appearance, there is considerable overlap. Other complications of infection that can occur with pneumonia are abscess and empyema.
11.4.5 Pearls and Pitfalls
In an erect patient, aspiration pneumonia is most common in the right middle lobe or bilateral lower lobes because the bronchi are oriented more vertically.
A chest radiograph may require 4–6 weeks to normalize after pneumonia.
11.5 Case 11.4
11.5.1 History
A 59-year-old female presented to the emergency department with chest pain and shortness of breath.
11.5.2 Findings
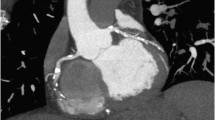
There are pulmonary emboli and bilateral main pulmonary arteries and segmental arteries. There is right ventricular strain (Figs. 11.4 and 11.5).
(a) Axial. Massive pulmonary embolism with a large saddle embolus in the main pulmonary artery (arrows). (b) Axial. Extensive bilateral thrombus in the proximal pulmonary arteries (arrows). (c and d) Axial and sagittal. Arrows pointing to a partial filling defect in an arterial branch to the right lower lobe (c) and proximal right pulmonary artery (d), which sometimes can have the appearance of an eyeball defect—Contributed by J. Lee & C. Smuclovisky
11.5.3 Diagnosis
The diagnosis is extensive pulmonary emboli with right ventricular strain .
11.5.4 Discussion
Pulmonary embolism (PE) is a common yet deadly disease that is responsible for 100,000 deaths in the USA annually. Risk factors for PE are similar to those for DVT and include malignancy, surgery, joint replacements, prolonged immobilization, pregnancy, and hypercoagulable disorders.
Common symptoms of PE are dyspnea, chest pain, and cough. The most common sign on physical exam is tachycardia. Because many patients may be asymptomatic, a high level of suspicion must be maintained among those who are at high risk. PE is often a lethal disease because it may cause right heart failure and subsequent death due to arrhythmias or cardiac shock in up to 30% of patients if not treated. Typical treatment is immediate anticoagulation and supportive therapy although more invasive therapy may be necessary in patients with hemodynamic compromise.
The presence of right ventricular strain , which can be assessed by right ventricular dilation and flattening of the intraventricular septum, is a negative prognostic indicator in patients with PE.
Historically, the gold standard for diagnosis was pulmonary angiography. However, today similar diagnostic results are achieved with CT angiography.
11.5.5 Pearls and Pitfalls
Timing of the contrast injection is crucial. Opacification extending from the main pulmonary arteries to the subsegmental arteries must be achieved to confidently rule out PE.
11.6 Case 11.5
11.6.1 History
A 65-year-old male underwent a preoperative study for aortic valve replacement. He has history of coronary artery disease and prior coronary artery bypass graft.
11.6.2 Findings
There is right-sided pleural effusion with septal thickening and ground glass opacities in both lung bases (Fig. 11.6).
11.6.3 Diagnosis
Pleural effusion due to volume overload.
11.6.4 Discussion
Pleural effusions can be classified as either transudative or exudative. Transudative effusions are caused by increased plasma hydrostatic pressure, decreased plasma oncotic pressure, or a combination of the two. The most common cause of transudative effusions is left heart failure, which causes increased plasma hydrostatic pressure from vascular congestion. Other causes include volume overload and diseases characterized by hypoalbunemia, such as hepatic disease or nephrotic syndrome. Exudative effusions are caused by infection, inflammation, and malignancy.
Pulmonary edema can develop in setting of volume overload or congestive heart failure. Radiographically, this is demonstrated by the presence of septal lines due to increased interstitial fluid as well as ground glass opacities due to increased fluid in the alveoli.
Thoracentesis can be performed to sample the pleural fluid, which can then be analyzed to help distinguish transudative effusions from exudative effusions. Typically, a transudative effusion has a pleural/serum protein ratio less than 0.5, pleural/serum LDH ratio less than 0.6, and pleural LDH less than 200 IU/L.
11.6.5 Pearls and Pitfalls
Transudative effusions usually have density on CT of 0–20 HU. Exudative effusions tend to have density greater than 20 HU.
11.7 Case 11.6 Contributed by J. Lee and C. Smuclovisky
11.7.1 History
An 89-year-old male presented with a history of increasing shortness of breath and atypical chest pain.
11.7.2 Findings
There is a pericardial effusion (Fig. 11.7a, b). There was multivessel non-obstructive calcified plaques in the coronary arteries (not shown).
(a and b) Axial and sagittal. Pericardial effusion (arrows). (c and d) Axial and sagittal. Thickened pericardium with scattered calcifications (arrows). (e) Axial: Constrictive pericarditis (arrows). Thickened and partially calcified pericardium causing compression of the ventricles with secondary dilatation of the atria (LA left atrium; RA right atrium)
11.7.3 Diagnosis
The diagnosis is pericardial effusion .
11.7.4 Discussion
The pericardial space normally contains up to 50 mL of fluid, which serves as lubrication for the visceral and parietal layers of the pericardium. Pericardial effusion is defined as an abnormal amount fluid or density in the pericardium. Etiologies include infectious, noninfectious, and autoimmune. The cause in this case was idiopathic.
The cause of increased fluid production depends on the underlying etiology. Transudate fluid accumulation results from obstruction of fluid drainage, which occurs through lymphatic channels. Exudate fluids occur secondary to inflammatory, infectious, malignant, or autoimmune processes affecting the pericardium.
Clinical manifestations of pericardial effusion are mostly dependent on the rate of accumulation of fluid in the pericardial sac. Rapid accumulation may cause elevated intrapericardial pressures with as little as 80 mL, while slowly progressing effusions can contain up to 2 L with minimal or no symptoms. CT can detect small amounts of fluid in the pericardium and reported as little as 50 mL. Pericarditis can lead to fibrosis and calcifications (Fig. 11.7c, d) in the pericardium that can lead to constrictive pericarditis (Fig. 11.7e), which impedes normal diastolic filling.
11.7.5 Pearls and Pitfalls
It is not uncommon to normally visualize a small amount of fluid in the inferior pericardial recess in asymptomatic patients. With a pericardial effusion , fluid extends superiorly surrounding the heart anterior and posteriorly.
11.8 Case 11.7 Contributed by J. Lee and C. Smuclovisky
11.8.1 History
An 81-year-old asymptomatic male presented with an abnormal nuclear stress test and silent MI.
11.8.2 Findings
There is a 3.9-cm water density mass inseparable from the free wall of the right atrium located in the cardiophrenic angle (Fig. 11.8a, b).
(a and b) Axial and coronal. Pericardial cyst in the right cardiophrenic angle (arrows). (c) Axial. Different patient with a large chronic myocardial infarct in the territory of the LAD (triple arrows), with a trapped fluid collection (single arrow) in the left cardiophrenic angle. There is a small amount of fluid (arrow head) in the pericardium. (d) Axial. Bronchogenic cyst, on a different patient (arrows)
11.8.3 Diagnosis
The diagnosis is pericardial cyst .
11.8.4 Discussion
Most pericardial cysts are congenital and are discovered, as in this case, as an incidental finding. Less common are inflammatory pericardial cysts. These include pseudocysts as well as encapsulated and loculated pericardial effusions. Pericardial scarring may trap portions of an intrapericardial exudate or hemorrhage producing a pocket or cyst-like structure (Fig. 11.8c).
Cysts occur anywhere in the pericardium and are mostly commonly located in the right cardiophrenic angle. Pericardial cysts are usually less than 3 cm in diameter and most are unilocular, have smooth borders, and contain clear fluid. The cyst arises from the parietal pericardium and consists of a single layer of mesothelial cells. Rarely, cysts can be associated with chest pain, dyspnea, cough, and significant arrhythmias, likely secondary to compression and erosion of the adjacent tissues.
The diagnosis on CT is established by the location, ovoid/triangular shape, thin walls, and homogeneous water density. These cysts have similar appearance and histology as bronchogenic cysts (Fig. 11.8d). Pericardial cysts may be hyperdense on CT, likely from containing mucoid or proteinaceous material or both that may mimic a solid mass.
11.8.5 Pearls and Pitfalls
Differential diagnosis of a pericardial cyst would include a bronchogenic cyst that is trapped in or on the pericardium, lymphangiomas, and necrotic tumors. Pericardial diverticula are less common and resemble cysts except that a comparable developmental abnormality has left a communication with the pericardial cavity.
11.9 Case 11.8 Contributed by J. Lee and C. Smuclovisky
11.9.1 History
A 79-year-old male presented with chronic shortness of breath and atrial fibrillation.
11.9.2 Findings
There is a filling defect in the left atrial appendage (Fig. 11.9a).
(a) Axial. Discrete low density in the left atrial appendage (LAA) confirmed by transesophageal echocardiography (TEE) to represent a thrombus (arrow). (b) Axial. Normal typical triangular appearance of the LAA (arrow) in a different patient. (c) Axial: Anatomic variant of the LAA with the apex toward the left sinus of Valsalva (arrow) in a different patient. (d) Axial. False-positive CTA result. Filling defect (arrow) in the LAA in a different patient with a chronic dilated cardiomyopathy and no thrombus and sluggish LAA on a TEE performed the following day
11.9.3 Diagnosis
The diagnosis is chronic nonvalvular atrial fibrillation with a thrombus in the left atrial appendage (LAA) .
11.9.4 Discussion
The LAA is well identified on cardiac CT and is contiguous anterior and superiorly with the left atrium and located to the left of the main pulmonary artery. The LAA typically has a triangular shape and enhances homogeneously with IV contrast (Fig. 11.9b). Internal striations in the apex of the appendage are also commonly visualized. Anatomic variants of the LAA are not infrequent and may appear redundant or with the apex adjacent to the left sinus of Valsalva (Fig. 11.9c).
The most common cause of thrombus in the LAA is atrial fibrillation. Other causes include mitral valvular disease, cardiomyopathy, and platelet dysfunction. Atrial fibrillation is a common arrhythmia that is found in 1% of persons older than 60 years to more than 5% of patients older than 69 years. Nonvalvular atrial fibrillation is the most common cardiac disease associated with cerebral embolism. Close to half of the cardiogenic emboli in the USA occur in patients with nonvalvular atrial fibrillation. Overall, 20–25% of ischemic strokes are due to cardiogenic emboli.
LAA thrombus is commonly difficult to identify on transthoracic echocardiography. The most widely used diagnostic test to establish the presence of thrombus is transesophageal echocardiography (TEE) . However, TEE is semi-invasive, and cardiac CTA has shown the potential to diagnose noninvasively thrombus in the LAA. Currently, there are no definitive studies establishing that CTA replaces TEE.
11.9.5 Pearls and Pitfalls
The LAA opacifies with contrast maximally in end-systole. This is usually the 30–40% phase on the cardiac CTA. LAA thrombus may be subtle and should be suspected in patients with left atrial (LA) enlargement (LA size 4.0 cm and greater). A sluggish LAA may under fill initially with contrast on CTA, giving the false appearance of a thrombus (Fig. 11.9d). Preliminary studies suggest that delayed imaging of the heart may avoid this pitfall.
11.10 Case 11.9 Contributed by J. Lee and C. Smuclovisky
11.10.1 History
A 51-year-old male presented for workup of coronary artery disease.
11.10.2 Findings
There is an incidental 3.5-cm lobulated noncalcified mass in the left atrium attached to the posterior wall (Fig. 11.10a, b).
11.10.3 Diagnosis
The diagnosis is left atrial myxoma .
11.10.4 Discussion
The tumor was surgically resected and the pathology confirmed. Myxomas are benign and represent the most common type of primary cardiac tumor. Approximately 90% are solitary and pedunculated. About 75–85% occur in the left atrial cavity. The mean age of patients with sporadic myxoma is 56 years. In the left atrium, the usual site of attachment is in the area of the fossa ovalis. Less often, myxomas also may arise from the right atrium and either ventricle. Occasionally myxomas, as in this case, arise from the posterior left atrial wall or the appendage. The mobility of the tumor depends on the extent of the attachment and length of the stalk. Clinical signs include embolization and mechanical interference with the cardiac function. Myxomas may also prolapse through the valve and cause destruction of the annulus or valve leaflets.
Familial cardiac myxomas represent approximately 10% of all myxomas. These may be associated with a syndrome called syndrome myxoma or Carney’s syndrome that consists of myxomas in other locations (breast or skin), spotty pigmentation, and endocrine dysfunction.
11.10.5 Pearls and Pitfalls
Not infrequently, mixing of IV contrast from the superior vena cava with nonopacified blood from the inferior vena cava causes a swirling artifact in the right atrium that may mimic a thrombus or tumor.
11.11 Case 11.10
11.11.1 History
A 71-year-old male presented with aortic stenosis (AS) and for prevalve replacement workup.
11.11.2 Findings
There is advanced aortic valve calcific deposits (Fig. 11.11a, b).
(a and b) Axial and coronal. There is extensive calcification in the aortic leaflets with severe aortic stenoisis (AS) (arrows). (c) Axial. Normal leaflets of the aortic valve (arrow) in another patient. (d) Axial: The aortic leaflets are deformed, thickened, and with mild calcific deposits (arrows) in a patient with bicuspid aortic valve and mild AS. (e and f) Axial and coronal (thick maximum intensity projection). Bioprosthetic aortic valve replacement (arrows). The arrow head in Fig. 6.5e indicates a pledget used to suture the valve in place. (g) Oblique sagittal: Valvular replacement with mechanical valves in the aortic (short arrow) and mitral (long arrow) position. (h) Axial: Dilatation of the ascending aorta in a patient with severe AS
11.11.3 Diagnosis
The diagnosis is aortic valvular stenosis .
11.11.4 Discussion
That aortic valve is well identified on CTA. In the normal aortic valve, the leaflets are thin and without thickening or calcific deposits (Fig. 11.11c). The normal aortic orifice is estimated at 3.0–4.0 cm2. A valve orifice of 1.0–1.5 cm2 is considered moderate stenosis, and 1.5–2.0 cm2 is considered mild stenosis. Less than 1.0 cm2 is considered critical stenosis. In the presence of a normal cardiac output, critical obstruction to the left ventricular outflow is usually characterized by a peak systolic pressure gradient exceeding 50 mmHg.
Clinical symptoms of AS include shortness of breath, syncope, chest pain, and ultimately signs of heart failure. AS refers to the obstruction of blood flow across the aortic valve. Isolated AS is usually either congenital or degenerative in origin. Congenital malformations of the aortic valve may be unicuspid, bicuspid (Fig. 11.11d), or tricuspid. The abnormal valvular architecture causes turbulent flow that damages the leaflets and leads to fibrosis, rigidity, calcification of the leaflets, and narrowing of the aortic orifice with subsequent AS.
Age-related degenerative calcific AS is currently the most common cause of AS in adults and the most frequent reason for aortic valve replacement (Fig. 11.11e–g). Other causes of acquired calcific AS, or aortic valvular sclerosis, include postinfectious, rheumatoid, and ochronosis.
AS can lead to left ventricular hypertrophy and subsequent LV dilatation. Post-stenotic dilatation of the ascending aorta may also be associated with AS (Fig. 11.11h). The noninvasive test of choice for evaluation of AS is transthoracic echocardiography. Additionally, invasive testing such as TEE and angiography is also commonly used.
11.11.5 Pearls and Pitfalls
Preliminary studies suggest that cardiac CTA appears to be accurate in the estimation of the severity of aortic valvular stenosis.
11.12 Case 11.11 Contributed by J. Lee and C. Smuclovisky
11.12.1 History
A 44-year-old male presented with a history of Marfan syndrome.
11.12.2 Findings
There is severe dilatation of the aortic root measuring 7.0 cm and without dissection. There is LV dilatation related to aortic regurgitation (Fig. 11.12a, b). There is dilatation of the suprahepatic veins and IVC from tricuspid regurgitation.
11.12.3 Diagnosis
The diagnosis is aortic root aneurysm secondary to Marfan syndrome.
11.12.4 Discussion
Marfan syndrome is an autosomal dominant disorder causing a genetic defect of connective tissue. The genetic defect is isolated to the FBN1 chain on chromosome 15, which codes for the connective tissue protein fibrillin. Abnormalities in this protein cause a constellation of clinical disorders, which commonly include the musculoskeletal, cardiac, and ocular system.
The cardiovascular involvement is the most serious problem associated with Marfan syndrome. The incidence of aortic dilatation occurs in 70–80% of cases and involves the sinuses of Valsalva. Aortic dissection is a common and often lethal complication. Mitral valve prolapse occurs in 55–69% cases. Additional findings include tricuspid valve prolapse, dilatation of the main pulmonary and dilatation, or dissection of the descending thoracic and/or abdominal aorta. Dilatation of the aortic root can cause stretching of the aortic valve leaflets resulting in lack of regurgitation.
11.12.5 Pearls and Pitfalls
The aortic root in adults normally measures <3.7 cm above the sinotubular junction.
11.13 Case 11.12
11.13.1 History
A 59-year-old male underwent coronary imaging for preoperative assessment for kidney donation. His history is significant for hypertension and hyperlipidemia.
11.13.2 Findings
There is mediastinal, hilar, and peribronchovascular lymphadenopathy (Fig. 11.13).
11.13.3 Diagnosis
Lymphadenopathy due to sarcoidosis.
11.13.4 Discussion
Lymphadenopathy is a term referring to abnormal lymph nodes, which includes lymph node enlargement, increased number of lymph nodes, and/or abnormal lymph node architecture. Lymphadenopathy is nonspecific finding that can be associated with localized or systemic pathology. Common causes include infection such as tuberculosis, autoimmune diseases, and malignancy such as lymphoma or metastatic disease. Reactive lymphadenopathy is a benign entity that represents a healthy immune response to an antigen stimulus. In some cases, reactive lymphadenopathy can mimic malignancy and a biopsy is required for diagnosis.
Sarcoidosis is a granulomatous disease characterized by noncaseating granulomas involving multiple organs including lungs, skin, joint, eyes, liver, and heart. In the USA, the disease is most common among young adult African Americans, who have an estimated lifetime risk of 2.4%. Half of cases are found incidentally on chest radiography. Definitive diagnosis is obtained by transbronchial biopsy of pulmonary lesions or percutaneous biopsy of other involved organs.
The overwhelming majority of patients with sarcoidosis have lung involvement. Patients who are symptomatic often present with cough, dyspnea, and chest pain. Imaging classically reveals bilateral hilar lymphadenopathy. Later stages of the disease involve the lung parenchyma and can be characterized on imaging by peribronchovascular nodules, ground glass opacities, cysts, and fibrosis with traction bronchiectasis.
11.13.5 Pearls and Pitfalls
Other causes of lymphadenopathy should be ruled out if biopsy is not performed. Sarcoidosis and granulomatous disease due to tuberculosis often causes calcified lymph nodes. In patients with untreated lymphoma and metastatic disease, the enlarged lymph nodes rarely calcify.
11.14 Case 11.13 Contributed by J. Lee and C. Smuclovisky
11.14.1 History
A 54-year-old male presented with a history of arrhythmias. The study was acquired for coronary venous mapping prior to defibrillator (ICD) insertion.
11.14.2 Findings
There is extensive mediastinal and bilateral hilar adenopathy containing scattered calcifications (Fig. 11.14a). There are perihilar infiltrates (Fig. 11.14b). There is marked dilatation of the left ventricle with diffuse thinning of the left ventricular walls. Abnormal density is seen in the lateral and inferolateral walls, with calcification (Fig. 11.14c). There is also focal posterolateral pericardial thickening with calcification (Fig. 11.14d). There is metal artifact in the right atrium from electrode wire leads.
(a) Axial. Hilar and mediastinal adenopathy from sarcoidosis (arrows). Metal artifact from electrode wire leads in the SVC (arrowhead). (b) Axial. Sarcoid perihilar infiltrates (arrows). (c) Axial. Diffuse thinning of the left ventricular walls, LV dilatation, and abnormal density in the lateral wall, which has epicardial calcification from myocardial sarcoidosis (arrows). (d) Axial. Pericardial thickening with calcification (arrow). Sarcoid infiltration of the myocardium (arrowheads)
11.14.3 Diagnosis
The diagnosis is granulomatous cardiomyopathy : sarcoidosis .
11.14.4 Discussion
Cardiomyopathies are commonly divided into a dilated or nondilated category. Within both of these groups, the myocardium may be hypertrophic or nonhypertrophic, and it may be accompanied by a restrictive (diastolic ventricular dysfunction) and/or congestive (systolic ventricular dysfunction) physiology. This form of classification may assist in specifying a cause for a cardiomyopathy based on the predominant clinical picture.
Sarcoidosis involving the heart is subclassified as a granulomatous cardiomyopathy. Clinically significant sarcoidosis involving the heart is uncommon and present in approximately 2–7% of patients with sarcoidosis. Clinically silent involvement of the heart has been described as greater than 20%.
Cardiac involvement may occur at any point during the course of the disease and may be present in the absence of pulmonary or systemic involvement. Sarcoidosis can involve any part of the heart, including the myocardium, endocardium, and pericardium. Cardiac sarcoidosis is a leading cause of the death among patients with sarcoidosis and with a mortality of up to 50–85% in autopsy series.
Arrhythmias or conduction defects are the most common cause of death; however, progressive heart failure due to massive granulomatous infiltration of the myocardium accounts for at least 25% of the deaths. Rapidly progressive and fatal congestive heart failure may be the presenting feature of sarcoidosis. Recurrent massive pericardial effusions or constrictive pericarditis accounts for less than 3% of cardiac deaths.
Conduction disturbances and arrhythmias are the most common cardiac manifestation secondary to granulomatous infiltration in the conduction system or ventricular walls. Variable degrees of AV block, bundle branch block, nonspecific intraventricular conduction delay, premature ventricular contractions, ventricular tachycardia, and other arrhythmias may be observed.
Extensive myocardial disease can result in a dilated cardiomyopathy and heart failure. The diagnosis of myocardial sarcoidosis can be difficult to make and may require a biopsy. Diagnostic studies commonly used are echocardiography, Holter monitoring, radionuclide scans with thallium, technetium pyrophosphate, and gallium. MRI and PET are also performed. Coronary angiography may be indicated to rule out obstructive coronary disease.
11.14.5 Pearls and Pitfalls
The accuracy of cardiac CTA in the evaluation of myocardial sarcoidosis has not been established. However, in the absence of significant or obstructive coronary artery disease, a granulomatous cardiomyopathy should be suspected in the presence of arrhythmias with abnormal density and calcifications in the myocardial walls and/or pericardium on the CTA.
11.15 Case 11.14
11.15.1 History
A 44-year-old male with history of hypertension presented to the emergency department with chest pain.
11.15.2 Findings
There was anterior mediastinal soft tissue lesion. Initial interpretation was thymoma versus thymic hyperplasia (Fig. 11.15).
11.15.3 Diagnosis
Thymic hyperplasia .
11.15.4 Discussion
The anterior mediastinum includes all structures behind the sternum, anterior to the pericardium, and below the level of the clavicles. Anterior mediastinal masses have a differential diagnosis often remembered with the mneumonic “4T’s,” which refers to masses arising from the thyroid, thymus, teratoma, and “terrible” lymphoma. Sometimes, the differential diagnosis is referred to as the “5T’s,” with the fifth “T” representing thoracic aorta aneurysm.
Thymoma comprises about 20% of mediastinal neoplasms and is the second most common mediastinal neoplasm in adults after lymphoma. Most patients are between 40 and 60 years of age with a slight male predominance. Most thymic tumors are either found incidentally or on workup of symptoms from a paraneoplastic syndrome (e.g., mysasthenia gravis) or mass effect (e.g., superior vena cava syndrome).
Up to half of patients with thymoma have myasthenia gravis, which is uncommon in thymic carcinoma. Other paraneoplastic syndromes can occur which affect the nervous system or muscle. Thymemectomy is usually curative for patients with a paraneoplastic syndrome associated with a thymoma and is often helpful in patients with thymic hyperplasia.
11.15.5 Pearls and Pitfalls
Anterior mediastinal lesions found in patients older than 40 years are likely to be lymphomatous or of thymic origin.
11.16 Case 11.15
11.16.1 History
A 75-year-old female presented to the emergency department with chest pain.
11.16.2 Findings
There is a soft tissue mass posterior to the heart containing multiple air foci (Fig. 11.16).
11.16.3 Diagnosis
Hiatal hernia .
11.16.4 Discussion
A hiatal hernia occurs when a portion of the stomach protrudes upward into the thoracic cavity.
There are two major types of hiatal hernias : sliding and paraesophageal. Sliding hiatal hernias occur when the gastric-esophageal junction slides upward more than 1 cm past the esophageal hiatus. Sliding hernias are a well-known cause of gastric reflux disease although many patients are asymptomatic. Paraesophageal hernias are much less common (approximately 1% of hiatal hernias) and occur when the fundus of the stomach herniates above the diaphragm, while the gastric-esophageal junction remains in place at the level of the diaphragm. Paraesophageal hernias can cause serious complications such as obstruction or volvulus.
11.16.5 Pearls and Pitfalls
Hiatal hernias are quite common and manifest as an air-filled soft tissue density behind the heart, which can be connected to the stomach.
11.17 Case 11.16
11.17.1 History
A 74-year-old male presented for evaluation of coronary arteries. History is significant for prior four-vessel coronary artery bypass graft.
11.17.2 Findings
There is an intimal flap in the aorta that was visible from just distal to the subclavian artery to above the diaphragmatic hiatus. The false lumen is partially thrombosed (Figs. 11.17 and 11.18).
(a) cMPR. Type A aortic dissection (long arrow) extending proximally to the aortic root and adjacent to the ostium of the left main coronary artery (LM). Metal artifact from bioprosthetic aortic valve (arrowhead). TL true lumen, FL false lumen. (b) Volume rendering. The false lumen (FL) has lower intensity on volume rendered 3D reconstruction. A felt strip (short arrow) has been placed in the proximal aorta to reinforce the suture lines related to the previous aortic valve replacement. (c–e) Axials and coronal: Type A aortic dissection—Contributed by J. Lee and C. Smuclovisky
11.17.3 Diagnosis
Thoracic aorta dissection , Stanford type B.
11.17.4 Discussion
Aortic dissection is a potentially life-threatening condition that requires prompt recognition to initiate appropriate management and reduce risk of death. Patients with an acute aortic dissection usually present with sudden onset of chest or back pain. Clinicians must have a high suspicion for aortic dissection because it is relatively rare, and most chest pain among patients who present to emergency departments is non-cardiovascular in origin.
Risk factors for aortic dissection include hypertension, collagen vascular disease, bicuspid aortic valve, a history of cardiac surgery, and trauma. Aortic dissection is most common in the older male population.
The most common classification system used today is the Stanford classification. Stanford type A involves the ascending aorta, and all other dissections are classified as type B. Dissections involving the ascending aorta (type A) carry a substantially worse prognosis because retrograde dissection can cause coronary artery occlusion, severe aortic regurgitation, and cardiac tamponade. Other complications of aortic dissection include hemothorax, limb ischemia, neurologic deficits caused by ischemic stroke or spinal cord ischemia, and abdominal viscera ischemia.
11.17.5 Pearls and Pitfalls
If an intimal flap is observed in the descending thoracic aorta on CCTA, assess the visible ascending aorta. A flap in the ascending aorta would be diagnostic of a more serious type A dissection.
The aortic root in adults is normally <3.7 cm, measured above the sinotubular junction. ECG-gated acquisition CTA is recommended in the evaluation of the thoracic aorta to avoid a pulsation artifact that may mimic a dissection in the proximal segment.
11.18 Case 11.17 Contributed by J. Lee and C. Smuclovisky
11.18.1 History
An 82-year-old male presented with a history of chronic myocardial infarct (MI), CABG, and aortic aneurysm repair.
11.18.2 Findings
There is a large chronic transmural MI involving the anteroseptal and apical segments of the left ventricle. The status was post CABG and ascending aortic aneurysm repair (Fig. 11.19a–c).
(a) Volume rendering. Large anteroseptal and apical MI (arrows). Status post CABG and ascending aortic aneurysm repair. (b and c) Axial, sagittal. Transmural MI . Thinning and low density throughout the scar (arrows). Focal calcification in the infarcted wall (arrowhead). (d and e) Oblique sagittal and axial. LV aneurysm containing thrombus in another patient (arrow)
11.18.3 Diagnosis
The diagnosis is chronic transmural left ventricular MI .
11.18.4 Discussion
Chronic myocardial infarcts of the left ventricle are well identified with CTA. Both transmural and subendocardial scarrings are visualized. The typical appearance of a transmural MI is thinning of the wall with low density from the scar. The scar may also contain calcification. Functional CTA demonstrates hypokinesis or akinesis in area of the MI. Subendocardial scars are identified as areas of low density in the subendocardial wall.
Transmural MI may develop aneurysmal dilatation, which may lead to a thrombus formation in the left ventricle (Fig. 11.19d, e). Rupture of the LV wall is most commonly fatal, and if the patient survives, can occasionally lead to formation of a pseudoaneurysm.
11.18.5 Pearls and Pitfalls
Normal left ventricular apical thinning may mimic an infarct. Normal LV systolic function with thickening in the apical segment and lack of significant disease in the LAD is helpful in substantiating the conclusion of a normal variant.
11.19 Case 11.18 Contributed by J. Lee and C. Smuclovisky
11.19.1 History
A 51-year-old female presented with a history of a dilated cardiomyopathy and previous surgery for mitral and tricuspid insufficiency.
11.19.2 Findings
There are hyperdense C-shaped rings in the mitral and tricuspid annuli (Fig. 11.20a–c).
(a) Coronal. Cosgrove-Edwards (CE) annuloplasty ring in the mitral annulus (arrow). (b) Sagittal. CE annuloplasty ring in the tricuspid annulus (arrow). (c) Axial. Partial visualization of the CE rings in the mitral and tricuspid annuli (arrows). (d–j) Surgical diagram and six different surgical devices used for valve repair (d–j, courtesy of Edwards Life sciences, Irvine, CA)
11.19.3 Diagnosis
The diagnosis is surgical mitral and tricuspid repair with Cosgrove-Edwards (CE) annuloplasty rings .
11.19.4 Discussion
The patient had viral myocarditis in the previous 2 years with subsequent development of a dilated cardiomyopathy that was complicated by severe mitral and tricuspid regurgitation. Since she was not a candidate for heart transplant, surgical repair of the valves was performed. Diseased cardiac valves may be replaced or repaired. The CE annuloplasty rings are commonly used to repair the mitral and also tricuspid valves.
11.19.5 Pearls and Pitfalls
On CTA, the CE appears as a thin hyperdense C-shaped band in the annulus.
11.20 Case 11.19
11.20.1 History
A 62-year-old female presented to the emergency department with substernal chest pain and shortness of breath.
11.20.2 Findings
There is a well-circumscribed hypodense hepatic lesion that measures 7 cm. The lesion demonstrates peripheral nodular enhancement (Fig. 11.21).
11.20.3 Diagnosis
Hepatic hemangioma .
11.20.4 Discussion
Hepatic masses in adults have a broad differential diagnosis of both benign and malignant diseases. Common benign etiologies include hepatic hemangioma (also called cavernous hemangiomas), focal nodular hyperplasia (FNH), hepatic adenoma, and idiopathic noncirrhotic portal hypertension. Malignant etiologies include hepatocellular carcinoma, cholangiocarcinoma, and metastatic disease. Parasitic infections and abscesses are less common etiologies. These lesions can often be diagnosed noninvasively by the presence of characteristic imaging features in conjunction with the patient’s history and risk factors.
Hepatic hemangiomas are the most common benign hepatic tumor and have been estimated to occur in up to 20% of the population. They are more common in females by a 3:1 ratio. These lesions can be solitary or present in multiple lobes of the liver. Most patients are asymptomatic, but lesions larger than 4 cm may cause abdominal pain, nausea, or early satiety due to mass effect. Rarely, hemorrhage or thrombosis within the tumor can cause acute right upper quadrant pain.
On contrast-enhanced CT imaging, hepatic hemangiomas have early peripheral nodular enhancement and delayed filling in a centripetal pattern. Imaging is usually sufficient for diagnosis. Biopsy of this lesion carries risk of hemorrhage and is not usually necessary for confirmation of the diagnosis.
11.20.5 Pearls and Pitfalls
MRI and ultrasound can be used to assist in distinguishing hepatic hemangiomas from more serious conditions such as metastatic disease.
11.21 Case 11.20
11.21.1 History
An 84-year-old male underwent imaging to assess his coronary arteries. His history is significant prior coronary artery bypass graft for left anterior artery (LAD) disease.
11.21.2 Findings
There is a well-circumscribed 2 cm lesion in the right adrenal gland. The density is somewhat lower than that of soft tissue (Fig. 11.22).
11.21.3 Diagnosis
Adrenal adenoma .
11.21.4 Discussion
Adrenal adenomas are common findings with use of advanced imaging such as multi-detector CT. Multiple studies have estimated that they are present in 5% or more of the general population. Adrenal adenomas are most often unilateral and nonfunctional. In one study, only 1% of adrenal lesions found incidentally proved to be adrenal carcinoma. Other important differential diagnoses include metastasis, pheochromocytoma, cyst, and hemorrhage.
Certain imaging characteristics can be used to distinguish benign from malignant adrenal lesions. Lesions that are smaller than 3 cm are most likely benign, while lesions greater than 5 cm are more likely malignant. Lesions with density less than 10 HU on a non-contrast CT are lipid-rich and most likely benign. On contrasted CT imaging, benign lesions typically have rapid contrast washout, while malignant lesions have delayed contrast washout. Moreover, lesions that show no growth on follow-up imaging are usually benign.
11.21.5 Pearls and Pitfalls
A density slightly lower than that of soft tissue is often typical of adrenal adenomas. However, dedicated abdominal CT or MRI is often necessary to further characterize incidentally found adrenal lesions.
11.22 Case 11.21
11.22.1 History
An 81-year-old female underwent coronary artery imaging after a positive stress test.
11.22.2 Findings
The abdominal aorta is abnormally enlarged (4.3 cm) and contains mural thrombus (Fig. 11.23).
11.22.3 Diagnosis
Abdominal aortic aneurysm (AAA) .
11.22.4 Discussion
Early recognition and treatment of this disease is important because a ruptured AAA is a life-threatening emergency. It is estimated that about 15,000 deaths are attributed to AAA in the USA each year.
Abdominal aortic aneurysms are defined as a focal dilation of the aorta to more than 50% of its normal size. Most men and women have an aortic diameter less than 2 cm; therefore, the upper limit of normal is considered to be 3 cm.
Risk factors for AAA include smoking, increasing age, male gender, atherosclerosis, and family history of AAA. Up to 8% of men over 65 are found to have AAA. One study found that prevalence in men peaked at age 80, while prevalence in women kept increasing with age. Patients under age 50 are extremely unlikely to have a clinically significant AAA.
Management of asymptomatic, unruptured AAA is based on size. Elective treatment is recommended for aneurysms greater than 5.5 cm or those with growth rate greater than 1 cm per year. In patients who do not meet these criteria, the risk of surgery is greater than the risk of rupture, and it is recommended that they undergo serial surveillance.
11.22.5 Pearls and Pitfalls
The U.S. Preventative Services Task force recommends a one-time screening with ultrasound to detect AAA in men between ages 65 and 75 with history of smoking.
11.23 Case 11.22
11.23.1 History
A 35-year-old male presented to the emergency department with shortness of breath and chest pain.
11.23.2 Findings
The liver is enlarged and demonstrated low density due to fatty infiltration (Fig. 11.24).
11.23.3 Diagnosis
Hepatic steatosis (fatty infiltration).
11.23.4 Discussion
Fatty infiltration of the liver is a nonspecific finding that can occur in response to insult from injury, toxins, or other diseases. When hepatic steatosis is present without any known cause, the condition is termed nonalcoholic fatty liver disease (NAFLD) . The risk of NAFLD is that it may progress to cirrhosis and ultimately liver failure.
NAFLD is subdivided into two entities: nonalcoholic fatty liver (NAFL) and nonalcoholic steatohepatitis (NASH). Histologically, NASH shows evidence of hepatocellular injury and fibrosis, which is absent in NAFL.
NAFLD is estimated to have a 20% worldwide prevalence. Risk factors include obesity, diabetes mellitus, dyslipidemia, and metabolic syndrome. Most patients are asymptomatic from NAFLD, and a variable number present with hepatomegaly. Biopsy is not always necessary for diagnosis, but is the only way to distinguish NAFL from NASH.
11.23.5 Pearls and Pitfalls
Fatty infiltration of the liver reduces its attenuation to lower than that of the spleen. A normal liver has attenuation higher than that of the spleen.
11.24 Case 11.23
11.24.1 History
A 51-year-old male presented to the emergency department with chest pain.
11.24.2 Findings
There are compression fractures of T6, T7, and T10. There is no retropulsion of bony fragments into the spinal canal (Figs. 11.25 and 11.26).
(a) Sagittal. Widespread metastatic bone disease from breast carcinoma (arrowheads). Status post vertebroplasty with injection of methylmethacrylate into a vertebral body with a small amount of leakage of the cement into the disc space (long arrows). (b) Sagittal. B-cell lymphoma involving the thoracic spine (arrows). (c) Sagittal. Widespread bony blastic metastases from prostate carcinoma (arrowheads). Status post CABG. (d) Sagittal. Expansile lytic lesion in the lower sternum (arrows) incidentally found in a 91-year-old female with intractable chest pain. Diagnosis: myeloma—Contributed J. Lee and C. Smuclovisky
11.24.3 Diagnosis
Multi-level thoracic compression fractures .
11.24.4 Discussion
Vertebral body compression fractures most commonly occur in the setting of osteoporosis, malignancy, infection, and trauma. Compression fractures are frequently located in the mid-thoracic spine or at the thoracolumbar junction.
Acute compression fractures can be caused by minor trauma such as bending, lifting, or coughing, and most of patients present with severe back pain. Chronic compression fractures may progress slowly over time, and patients may present with asymptomatic loss of height and kyphosis. Neurologic impairment can occur if there is associated compression of the spinal cord or nerve roots. In cases of severe kyphosis of the thoracic spine, patients can develop impaired respiratory function.
Pain caused by compression fractures can be managed conservatively with a back brace to provide support for the spine. Vertebroplasty and kyphoplasty are also effective techniques to reduce pain. To perform a vertebroplasty, cement is injected percutaneously through the pedicles into the vertebral body to stabilize and prevent further collapse of the vertebral body. The technique for kyphoplasty is similar, except that it also uses balloon inflation within the vertebral body to help restore vertebral body height. Surgery may be appropriate if there is spinal cord compression with neurologic deficit or frank instability of the spine.
11.24.5 Pearls and Pitfalls
Pathologic fractures should be followed up with MRI to assess for malignancy or infection. MRI will also evaluate for spinal cord compression.
11.25 Case 11.24 Contributed by J. Lee and C. Smuclovisky
11.25.1 Extracoronary Disease
During the interpretation of cardiac CT, extracoronary findings are frequently identified. It is important to evaluate the entire anatomy in the field of view in order not to miss a clinically relevant finding (Fig. 11.27a–h).
(a) Axial. Left renal upper pole carcinoma (arrows). (b) Axial. Gastric carcinoma with ulceration of the tumor (long arrow) and adjacent adenopathy (arrowheads). (c and d) Axial and coronal maximum intensity projection. PFO closure device (arrow). (e and f) Coronal and axial. Foreign body in the right pulmonary artery from a wire lost during placement of an ICD device (arrows). ICD wires in the SVC (f, long arrow). Status post CABG. (g) Sluggish filling in the LA appendage; questionable for clot (arrow). (h) Immediate delay acquisition demonstrates complete filling with no evidence of thrombus (arrow)
References
Hunold P, Schmermund A, Seibel RM, Gronemeyer DH, Erbel R. Prevalence and clinical significance of accidental findings in electron beam tomographic scans for coronary artery calcification. Eur Heart J. 2001;22:1748–58.
Macmahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner society. Radiology. 2005;237:395–400.
Suggested Reading
Abbara S, Kalan MM, Lewicki AM. Intrathoracic stomach revisited. AJR Am J Roentgenol. 2003;181:403–14.
Baughman RP, Teirstein AS, Judson MA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. 2001;164:1885–9.
Bonder A, Afdhal N. Evaluation of liver lesions. Clin Liver Dis. 2012;16:271–83.
Bosanko CM, Korobkin M, Fantone JC, et al. Lobar primary pulmonary lymphoma: CT findings. J Comput Assist Tomogr. 1991;15(4):679–82.
Chakko S. Pleural effusion in congestive heart failure. Chest. 1990;98:521–2.
Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A, Cahall DL. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005;20:557–63.
Descombes E, Gardiol D, Leuenberger P. Transbronchial lung biopsy: an analysis of 530 cases with reference to the number of samples. Monaldi Arch Chest Dis. 1997;52:324–9.
Franquet T. Imaging of pneumonia: trends and algorithms. Eur Respir J. 2001;18:196–208.
Gharib AM, Stern EJ. Radiology of pneumonia. Med Clin North Am. 2001;85:1461–91. x
Haniuda M, Kondo R, Numanami H, et al. Recurrence of thymoma: clinicopathological features, re-operation, and outcome. J Surg Oncol. 2001;78:183–8.
Jang HJ, Kim TK, Lim HK, et al. Hepatic hemangioma: atypical appearances on CT, MR imaging, and sonography. AJR Am J Roentgenol. 2003;180:135–41.
Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008;22:601–16.
Konstantinides SV, Torbicki A, Agnelli G, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3033–69.
Lee SS, Park SH. Radiologic evaluation of nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:7392–402.
Light RW, MacGregor MI, Luchsinger PC, Ball WC. Pleural effusions: the diagnostic separation of transudates and exudates. Ann Intern Med. 1972;77:507–13.
Lillington GA, Caskey CI. Evaluation and management of solitary and multiple pulmonary nodules. Clin Chest Med. 1993;14:111–9.
Lombardi G, Zustovich F, Nicoletto MO, et al. Diagnosis and treatment of malignant pleural effusion: a systematic literature review and new approaches. Am J Clin Oncol. 2010;33:420–3.
Midthun DE, Swensen SJ, Jett JR. Approach to the solitary pulmonary nodule. Mayo Clin Proc. 1993;68:378–85.
Mueller J, Jeudy J, White CS. Cardiac CT angiography after coronary artery bypass surgery: prevalence of incidental findings. AJR Am J Roentgenol. 2007;189:414–9.
Onuma Y, Tanube K, Hatori M, et al. Non-cardiac findings in coronary imaging with multi-detector computed tomography. J Am Coll Cardiol. 2006;48:402–6.
Patel U, Skingle S, Campbell GA, Crisp AJ, Boyle IT. Clinical profile of acute vertebral compression fractures in osteoporosis. Br J Rheumatol. 1991;30:418–21.
Pickhardt PJ, Park SH, Hahn L, et al. Specificity of unenhanced CT for non-invasive diagnosis of hepatic steatosis: implications for the investigation of the natural history of incidental steatosis. Eur Radiol. 2012;22:1075–82.
Rybicki BA, Major M, Popovich J Jr, et al. Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol. 1997;145:234–41.
Savage JW, Schroeder GD, Anderson PA. Vertebroplasty and kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Am Acad Orthop Surg. 2014;22:653–64.
Smith SB, Geske JB, Maguire JM, et al. Early anticoagulation is associated with reduced mortality for acute pulmonary embolism. Chest. 2010;137:1382–90.
Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee. Am J Respir Crit Care Med. 1999;160:736–55.
Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120:871–9.
Ströbel P, Bauer A, Puppe B, et al. Tumor recurrence and survival in patients treated for thymomas and thymic squamous cell carcinomas: a retrospective analysis. J Clin Oncol. 2004;22:1501–9.
Thomas KW, Hunninghake GW. Sarcoidosis. JAMA. 2003;289:3300–3.
Van Belle A, Büller HR, Huisman MV, et al. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. JAMA. 2006;295:172–9.
Yun EJ, Choi BI, Han JK, et al. Hepatic hemangioma: contrast-enhancement pattern during the arterial and portal venous phases of spiral CT. Abdom Imaging. 1999;24:262–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Brown, C., White, C.S. (2018). Extracardiac Findings on Cardiac CTA. In: Smuclovisky, C. (eds) Coronary Artery CTA. Springer, Cham. https://doi.org/10.1007/978-3-319-66988-5_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-66988-5_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-66986-1
Online ISBN: 978-3-319-66988-5
eBook Packages: MedicineMedicine (R0)