Abstract
Through human history viruses have shown enormous epidemiological and pandemic potential as the occurrence and spread of viruses in pandemic dimensions poses a threat to the health and lives of seven billion people worldwide. Scientific evidence has associated harmful health effects to indoor air hazards recognizing the existence of a vital concern in public health sector. Thus the assessment of human exposure to biological aerosols and droplets indoor became an imperative requirement of investigation. Environmental bioburden assessment of viruses relies in both culture-dependent approaches that comprise classical methodologies, still prominent and vital in the field of modern biotechnology, and culture-independent approaches based on nucleic acid amplification techniques, which are considered the gold standard in clinical virology. The main factor influencing indoor microbiology is the human being and their activities. Indoor environments to be considered are those regularly occupied by humans: residences, offices, schools, industrial buildings, health care facilities, farming activities and other settings occupied all the time, or in which occupant density is high. It’s well known that approximately 60% of total human respiratory and gastrointestinal infections are acquired indoor, since viruses have a rapid spread in the community and can be transmitted easily, especially in crowded and poorly ventilated environments, causing high morbidity and decline in quality of life and productivity. Studies have shown that respiratory syncytial virus, rhinovirus, metapneumovirus, influenza and parainfluenza virus, and human enterovirus infections may be associated with virus-induced asthma, leading to diseases such as pneumonia. Gastroenteritis infectious (about 30±40% of cases) is attributable to viruses. Rotavirus, Astrovirus, Norwalk-like viruses and other caliciviruses are responsible for 48% of all reported outbreaks of infectious intestinal disease. Safe working conditions are essential for healthy living, that’s why the programmes conceived as a result of strategic and preventive policy maintenance, in refrigeration and ventilation systems, are the determining factor for the control of biological pollutants. Moreover, the development of highly sensitive and specific detection and identification methodologies with capacity to be used in diverse applications, such as diagnosis, public health risk assessment, research and for the implementation of preventive measures and protocols are imperative.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Viruses indoor
- air transmission
- culture-dependent virus analysis
- culture-independent virus analysis
- environmental assessment
1 Environmental Exposure
Indoor air pollution is a major global public health threat requiring increased hard work, linking research to policy-making. The evidence of the effects of physical and chemical pollutants on human health, present in the external and internal environment has no superior aggression than the existing bioaerosols. Health effects from indoor air pollutants may be experienced soon after exposure or, possibly, years later, according to the nature of air contaminants, being classified, in an abbreviated approach, as physical, chemical or biological (Nazaroff, 2016).
Several studies have related hostile health effects to Indoor air hazards and adequate assessment of human exposure to biological aerosols has been recognized as an imperative requirement and a very important concern in the area of public health (Douwes et al., 2003). Scientific evidence has showed that the air within buildings can be more seriously polluted than the outdoor air, even in developed and industrialized countries, and it is well known that indoor environments occupied by humans, contain abundant material of microbial origin, consequently, the risks to human health may be greater due to exposure to air pollution indoors (Fisk et al., 2007).
On the other hand, investigation indicates that people spend approximately 90% of their time indoors, with mechanical heating, cooling and ventilation systems, influencing irrefutably the quality of life (Klepeis et al., 2001; Nazaroff, 2016). Complex syndromes arise associated with indoor air quality, such as sick building syndrome, building-related disease leading to loss of productivity and absence at work. These syndromes are associated with increased incidence and prevalence of asthma and other chronic diseases worldwide. Exposure to bioaerosol material can cause or can contribute to several relevant diseases.
Human occupancy and activities are major factors influencing indoor microbiology. Humans are important primary sources of certain bacteria and viruses. The recent development of quantitative polymerase chain reaction (PCR) and other RNA/DNA-based measurement technologies has permitted studies that measure pathogenic material in indoor air (Lax et al., 2014; Nazaroff, 2016).
1.1 Droplets vs Airborne
Droplet transmission is not to be confused with airborne transmission. Aerosols are suspensions in air (or in a gas) of solid or liquid particles, small enough to remain airborne for a prolonged period of time because of their low settling velocity. Droplets do not remain suspended in the air. Airborne transmission depends on viruses from evaporated droplets or dust particles that can remain suspended in the air for long periods. Droplet transmission occurs when viruses travel on relatively large respiratory droplets (>10 μm) that people sneeze, cough, or exhale during conversation or breathing (primary aerosolization) (La Rosa et al., 2013). Respiratory droplets initially all move forward with the exhaled air jet; very large droplets leave the jet quickly and fall on the ground and small droplets completely desiccate within the jet (Tellier, 2009).
The transport and the settling of a bioaerosol are affected by its physical properties and the environmental parameters that it encounters. Size, density and shape of droplets or particles, air currents, relative humidity and temperature, determine the capacity of generation of airborne bioaerosols from liquid suspensions, undergo desiccation, whereas those generated as dusts or powders partially rehydrate. The presence of moulds indicates a problem with water penetration or high humidity. Bioaerosols can be transmitted at long distances. Small particle aerosols, as shown during endotracheal intubation, are transmitted to persons in the immediate area near the patient. Viruses’ inductors of Severe Acute Respiratory Syndrome (SARS), influenza and norovirus are transmitted from patients primarily by contact and/or droplet routes, while airborne transmission occurs over a limited distance (Srikanth et al., 2008). Indoor–outdoor air exchange (mechanical ventilation), penetration (air filter), deposition, sources and aerosol resuspension, are extremely relevant for spread contamination.
Once aerosolized, aerosols viruses’ particles may travel significant distances through buildings before being captured and retained by HVAC filters, or they pass through as well, because most HVAC filters are not 100% efficient in capturing particles. The rapidity with which airborne viruses are inactivated during transport or after filter capture is uncertain and merits additional study. Analysis of ventilation filters certainly could play a role in the epidemiology of infectious diseases caused by pathogens released into the environment, suiting all the different situations of confinement (Goyal et al., 2011).
2 Viruses Indoor
The main source of indoor viruses is the human being. Viruses are spread by air currents after resuspension of material scattered by aerosols droplets or saliva. We can say that viral infections are probably the most common acquired diseases indoor that affect man, knowing approximately a thousand types of different viruses involved. It is estimated about 60% of total human respiratory and gastrointestinal infections, with a rapid spread in the community, being a cause of high morbidity and decline in quality of life and productivity, since viruses can be easily transmitted, especially in crowded and poorly ventilated environments. It is well-known that viruses are shed in large numbers, with transmission routes extraordinary diverse, including direct contact with infected persons, faecal-oral transmission (through contaminated food and water), droplet and airborne transmission, and can survive for long periods on surfaces or fomites, emphasizing the possible role of surfaces in the transmission of viruses (Barker et al., 2001; La Rosa et al., 2013).
For instance, faeces can contain up to 1012 viruses particles per gram and vomit up to 107 per millilitre, so the potential transfer contamination from hands to surfaces is frighteningly considerable. The most important source of potentially pathogenic viral aerosol is other humans and other means, as the flushing of a toilet that can aerosolize significant concentrations of airborne viruses. Viruses’ survival on fomites is influenced by temperature, humidity, pH and exposure to ultraviolet light.
Particle size, depth of penetration and the minimum dosage of the agent capable of causing disease are implicated in the infectivity. In addition, it is also important to be conscious of the risk groups, the most susceptible to contracting infection when exposed to microorganisms, conditioned by factors such as a weakened immune system, the children, the elderly, the pregnant women, the chronically ill, especially those suffering from respiratory or cardiovascular disease. Chronic obstructive pulmonary disease (COPD) and acute exacerbations are frequent complications, thought to be caused by interactions between host factors, bacteria, viruses and changes in air quality producing increased inflammation in the lower airway with a long-lasting adverse influence on health status (Celli and Macnee, 2004; Celli and Barnes, 2007). Approximately of 50% of acute exacerbations of COPD are associated with symptoms of viral infections of the respiratory tract by rhinovirus, respiratory syncytial virus and influenza. Studies have shown that respiratory syncytial virus (RSV), human rhinovirus (HRV), human metapneumovirus (HMPV), influenza and parainfluenza virus (HPIV), and human enterovirus infections may be associated with virus-induced asthma, leading to diseases such as pneumonia or death (Tsukagoshi et al., 2013).
Respiratory and enteric viruses are opportunistic pathogens transmitted mainly via other routes are able to spread via droplet nuclei or dust in certain circumstances (La Rosa et al., 2013). Numerous studies identify the factors that are involved in the transmission of infection by aerosol indoor with the correlation between the pulmonary mechanism, the different human activities and the critical concentration of particles expelled. A virus (H3N2) had a higher transmissibility and uncontrollable potential than the A (H1N1) and B viruses (Chen et al., 2009; Chen and Liao, 2010).
2.1 Respiratory Viruses
In developing countries, acute respiratory infections, due to various viruses, is not only the most common cause of upper respiratory infection in humans but is also a major cause of morbidity and mortality, leading to diseases such as bronchiolitis, asthma and pneumonia (Tsukagoshi et al., 2013; Paba et al., 2014).
Despite all the progress of the last decades in the prevention and care of health, respiratory infections represent one of the major causes of disease in humans. This group remains the leading cause of outpatient consultation as well as antibiotic prescription and work absence. The chronic infections, causing disability, have the most important impact on quality of life. The main effect of the inadequate quality of indoor air is in respiratory system. Most studies focus on the influenza virus, but in general, we can say that a total concentration of viruses, in a variety of environments such as classrooms, health institutions, restaurants, offices and others corresponds to an average 4.7 ± 2.5 × 105 particles per cubic meter, without significant differences between the different indoor environments. Also, is estimated that the viral particles inhaled daily indoor correspond approximately to 5 × 106. Respiratory viruses can be transported over considerable distances by air currents and be inhaled, penetrating deep into the respiratory system (Prussin II et al., 2015).
Droplet transmission occurs when viruses travel on relatively large respiratory droplets (>10 μm) that people sneeze, cough, or exhale during conversation or breathing, primary aerosolization. A single cough can release hundreds of droplets, up to 40,000, at speeds of up to 50–200 miles per hour, each droplet containing millions of viral particles. Aerosol droplets travel only short distances (1–2 m) before settlings on surfaces, where viruses can remain infectious for hours or days. Secondary aerosolization can occur when air displacements disperse the viruses back into the air from contaminated surfaces (La Rosa et al., 2013). Transmission occurs through air droplets, aerosol and fomites that may come into contact with nasal and conjunctival epithelium. The etiological viral agents involved include: influenza virus types A and B, parainfluenza viruses types 1, 2, 3, and 4, respiratory syncytial virus, adenovirus, and rhinoviruses/enteroviruses (Paba et al., 2014). The acute respiratory infections are the result of active multiplication of microbiological agents in the respiratory system when favourable conditions of the host exist. Viral or bacterial ethology, predisposing factors related to anatomical factors, immune changes, colonization of the naso and oropharynx, and the spread of these infections is favoured by the continuity of the epithelia of the respiratory system and a continuum between upper and lower airways. The upper and lower respiratory infections are in most cases (60%) of viral origin.
Adenovirus (type 4), the first virus to be isolated from indoor aerosol, was identified in 1966 in aerosol samples from the quarters of military recruits infected with Acute Respiratory Disease (Artenstein and Miller, 1966). Since then, human infections due to viral aerosol (or contact with contaminated surfaces) have been studied in various environments, including office building, hospitals, restaurants, transport systems and schools. In the last few years, other respiratory viruses have been discovered and linked to the upper and lower respiratory tract infections: human metapneumovirus, SARS coronavirus, HKU1 coronavirus, NL63 coronavirus, MERS coronavirus and bocavirus.
In 2007, two novel human polyomaviruses named KIPyV and WUPyV were discovered in the respiratory secretions of patients with acute respiratory symptoms. The outbreak of the influenza A virus (H1N1) infection in 2009 has reminded us again of the importance of monitoring and controlling airborne microorganisms in public facilities (Lee et al., 2012). Unlike conventional viral cell cultures, with the introduction of the real-time PCR assay, the diagnosis of respiratory infections improved greatly. It is possible to search for up to 21 different respiratory pathogens including viruses and bacteria. In addition, it is possible to detect co-infections that may have implications on disease severity or therapeutic strategies (Paba et al., 2014).
For bioaerosol particles, maybe the most important exposure pathway is inhalation followed by deposition in the respiratory tract. The probability of deposition varies with particle size, with lung morphology, and with breathing characteristics. Airborne exposure indoors makes a meaningful contribution to the occurrence or spread of disease.
2.2 Respiratory Viruses Associated with Indoor Air Transmission
2.2.1 Rhinovirus
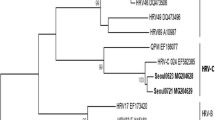
Rhinovirus (RV) is a small RNA virus belonging to the Picornaviridae family. More than 100 immunologically distinct serotypes have been identified and new serotypes are continuously emerging. This virus is responsible for more than 50% of cases of common cold, being the virus with the highest morbidity among respiratory diseases. In children causes bronchitis. Although the method of transmission of RVs is in doubt, they are thought to be mainly transmitted via large droplets, but indirect contact with contaminated fomites has also shown to transmit infection or by aerosols. It’s known that RV need only 10 s of contact (hand-to-hand) for infecting another person. The recurrence of viral infections is predominantly associated with an immune response to a serotype that does not provide immunity to reinfection with another serotype for the same virus (Ballow, 2008).
Rhinoviruses can survive on environmental surfaces for several hours. Infectious viruses have been recovered from naturally contaminated objects in the surroundings of persons with RV colds. Aerosols are generated by coughing, talking, sneezing and even simply breathing (Huynh et al., 2008). Rhinovirus outbreaks in health care facilities, capable of determining severe infections and also death have been documented (MacIntyre et al., 2012). RVs have also been detected in transport vehicles (La Rosa et al., 2013). Even in the common cold, rhinoviruses and coronaviruses predominate (Barker et al., 2001; Heikkinen et al., 2003), but the role of rhinoviruses is the most prominent, in particular are responsible for outbreaks of the common cold in the general community such as schools, day care centres and hospitals (Barker et al., 2001; Heikkinen et al., 2003; La Rosa et al., 2013). Rhinoviruses and coronaviruses also cause a greater disease burden in elderly people living at home, compared with influenza or syncytial viruses.
The infections by rhinovirus may be triggering factors of exacerbations of asthma, probably because they induce inflammation in airways that are already damaged and sensitized. Rhinoviruses were detected by RT-PCR among infants (von Mutius, 2004), in the acute exacerbation of asthma when infection was prolonged (Tsukagoshi et al., 2013). Some authors describe that bronchial epithelial patient cells with asthma are more effectively infected with RV than normal epithelia. It was shown that viral are upregulated in the epithelial cells of patients with allergies (Canonica et al., 1995; Tantilipikorn and Auewarakul, 2011).
2.2.2 Respiratory Syncytial Virus
Respiratory syncytial virus (RSV) is a single-stranded RNA virus belonging to Paramixoviridae family. RSV infections occur all over the world and outbreaks are common in the cold season in temperate climates and in the rainy season in tropical climates. Is one of the most common viruses which can cause a type of potentially lethal pneumonia in older people and is a major cause of respiratory illness in young children producing bronchitis and pneumonia worldwide, affecting about 90% of children by the age of 2 years (24), inducting a preparative stage in the development of asthma (Tsukagoshi et al., 2013).
School-aged children often carry RSV to their homes and extent infection to younger brothers as well as when admitted to hospital, tend to shed the virus abundantly and for prolonged periods permitting sufficient opportunity for spread in adults. Sometimes this virus produces a Flu-like syndrome indistinguishable from influenza (Barker et al., 2001).
RSV is highly contagious and transmission can occur when infectious material comes into contact with mucous membranes of the eyes, mouth or nose, and possibly through the inhalation of droplets generated by a sneeze or cough. Also result from contact with contaminated environmental surfaces, the commonest mode of transmission in school classrooms and day care centres. Transmission with fomites predominates over droplet contact can be transmitted by the airborne route. RSV RNA is detected in air samples from the hospital rooms of infected patients at large distances from the patient’s bedside. Particles containing RSV RNA were detected in airborne throughout a health care facility, particles small enough to remain in the air for an extended period and to be inhaled deeply into the respiratory tract (6). Evidence shows that direct and indirect contact is a key factor in transmission hands, touching surfaces contaminated with fresh secretions from RSV-infected infants (Barker et al., 2001).
2.2.3 Influenza Virus
Influenza virus (IV) is one of the most common and highly contagious infectious diseases and can occur in people of any age. Influenza or flu produces an acute infection of the respiratory system with high transmissibility and global distribution. Is a RNA virus belonging to the Orthomixoviridae family which is subdivided into three distinct antigenic serotypes: A, B and C, causing moderate to severe acute febrile illness, resulting in variable degrees of systemic symptoms, ranging from mild fatigue to respiratory failure and death. Strains A and B have greatest potential epidemic, causing more versions of the flu. The flu vaccine only protects against viruses A and B. Influenza C viruses are antigenically stable, cause subclinical disease and do not cause epidemics. The influenza A and B have multiple subtypes that still suffer mutations, emerging new strains with consequent increased risk of epidemics or pandemics.
The continuing threat of pandemics by the human influenza virus suggests an urgent and constant surveillance. Despite the vaccination continues to be considered the intervention of containment of infection, the viruses A (H1N1), A (H3N2) and influenza B persist with a global distribution and with such a power of infectivity that Influenza activity management has been undertaken by the Centres for Diseases Control. Influenza A (H3N2) has a uncontrolled and potential infectivity demonstrating a much greater transmissibility than A (H1N1) and B viruses (Chen and Liao, 2010). Influenza affects all age groups, but it is the elderly and persons with underlying health problems who are at particular risk from complications of influenza and are more likely to require hospitalization. Both influenza virus A and B revealed to survive on hard surfaces such as stainless steel and plastic for 24 ± 48 h and on absorbent surfaces such as cloth, paper and tissues for up to 12 h (Barker et al., 2001). Asymptomatic patients shed virus and can transmit the disease, thus creating a reservoir for the virus. Influenza virus is transmitted by droplets, through the coughing and sneezing of infected persons, but it can also be transmitted by airborne droplet nuclei as well as by contact, either through direct skin-to-skin contact or through indirect contact with contaminated environments (La Rosa et al., 2013).
Influenza viruses have been detected in different indoor environments, homes, schools, offices and others public buildings. Places such as hospitals, where the presence of a susceptible population is often combined with a high population density, may harbour high concentrations of pathogens and therefore pose a considerable risk for the transmission of the virus, with potentially fatal consequences for hospitalized patients. Schools are known to have an important role in influenza transmission in the community since children have a higher influenza attack rate than adults (children get the flu twice as often as adults) (Zhao et al., 2007).
On buildings ventilation systems Influenza A and B were detected (along with other groups of viruses), meaning that contamination exists in the surrounding environment. Several reviews consider three modes of transmission of influenza, not mutually exclusive, by large droplets, self-inoculation of the nasal mucosa by contaminated hands and the aerosol transmission, the mode of the greatest impact for infection, since it requires specialized personal protective equipment. Influenza virus RNA was directly detected in aerosol particles generated by normal breathing in patients with influenza and collected through an orinasal facemask; particles of 5 mm or less have a significant penetration into the respiratory tract all the way to the alveolar region. Increasing evidences point towards a role for aerosol transmission in the spread of influenza, at least over short distance where exposure to both aerosol and large droplets occurs. In most settings where there is adequate ventilation, long-range transmission does not appear to occur so frequently (Tellier, 2009).
The relative importance of the aerosol transmission route for influenza remains controversial. To determine the potential for influenza to spread via the aerosol route, the authors 6x measured the size distribution of airborne influenza A virus. Collected size-segregated aerosol samples during the 2009–2010 flu season in a health centre, a day-care facility and on board of aeroplanes. Filter extracts were analysed using quantitative reverse transcriptase polymerase chain reaction. Half of the 16 samples were positive, and their total virus concentrations ranged from 5800 to 37,000 genome copies m23. On average, 64% of the viral genome copies were associated with fine particles smaller than 2.5 mm, which can remain suspended for hours. Modelling of virus concentrations indoors suggested source strength of 1.6 + 1.2 × 105 genome copies m23 air h21 and a deposition flux onto surfaces of 13 + 7 genome copies m22 h21 by Brownian motion. Over 1 h, the inhalation dose was estimated to be 30 +18 median tissue culture infectious dose (TCID50), adequate to induce infection. These results provide quantitative support for the idea that the aerosol route can be an important mode of influenza transmission (Yang et al., 2011). Parainfluenza viruses (PIVs) are a further major group of respiratory pathogens. They cause severe colds, croup, bronchitis and pneumonia in children and adults and in infants the virus can cause life-threatening disease. Infection is probably spread by aerosols in addition to direct contact with contaminated surfaces. The persistence of PIV on hospital surfaces contaminated with patients’ secretions was noted as a potential source of transmission (Barker et al., 2001).
Goals for epidemiological surveillance of Influenza include supervise the currently circulating virus subtypes and offer quick response to spread of new subtypes; follow the tendency of the morbidity and mortality to plan strategies to reduce the burden of the disease in public health; define strategies to reduce the occurrence of deaths; monitor the severity standard of the disease by detecting any virulence changes.
2.2.4 Severe Acute Respiratory Syndrome
Severe acute respiratory syndrome (SARS) is a respiratory illness caused by a type of coronavirus from the Coronaviridae family, which can cause mild to moderate upper respiratory illness, such as the common cold or develop into potentially severe pneumonia. This virus is known as SARS-CoV. The SARS epidemic broke out in 2002–2003 in southern China, and spread to other regions of Asia and also to Europe and North America. It caused more than 8000 infections worldwide with an approximately 10% fatality rate, along with enormous economic losses. One or a few trivial mutations at the receptor-binding surface of a virus may lead to dramatic epidemic outcomes by facilitating cross-species infections and human-to-human transmission of the virus (Li, 2013). SARS is a condition associated with substantial morbidity and mortality with patterns suggesting droplet or contact transmission (Poutanen et al., 2003).
The earliest symptom is a sudden onset of high fever. Some patients may also have chills and headaches followed by pneumonia; others showed respiratory distress (severe breathing difficulty) and sometimes death (La Rosa et al., 2013).
The most common mode of transmission is contamination by warm air indoor, by water droplets generated by coughs or sneezes, but may be transmitted through the airborne route as well. Transmission in an aircraft from an infected person to passengers located seven rows of seats ahead had been described. Aerosol generated by the building’s sewage systems is also responsible. Many health care workers were infected after endotracheal intubation and bronchoscopy procedures which often involve aerosolization. These observations indicate the possible role of more remote modes of transmission, including airborne spread by small droplet nuclei, and emphasize the need for adequate respiratory protection in addition to strict contact and droplet precautions when managing SARS patients. Contaminated fomites or hospital surfaces might contribute to spread. It is known that these viruses may live on hands, tissues and other surfaces for up to 6 h and up to 3 h after droplets have dried. Airborne spread of the virus appears to explain the happened large community outbreaks of SARS (Ignatius et al., 2004; Hui and Chan, 2010; La Rosa et al., 2013).
A novel coronavirus, MERS-CoV (NCoV, HCoV-EMC/2012), originating from the Middle-East, has been discovered. Incoming data reveal that the virus is highly virulent to humans. The members of this group (C) are likely to persist in the environment for a longer period of time and possess the highest oral-fecal components but relatively low respiratory transmission components. Oral-urine and saliva transmission are also highly possible (Goh et al., 2013).
2.2.5 Adenovirus
Human adenovirus (AdV) is a non-enveloped, icosahedral virus of the genus Mastadenovirus, family Adenoviridae. There are more than 60 types classified into seven strains from A to G, defined via biological and molecular characteristics. Clinical manifestations are highly heterogeneous, ranging from upper and lower respiratory tract infections to gastroenteritis, pneumonia, urinary tract infection, conjunctivitis, hepatitis, myocarditis and encephalitis. The burden of disease manifests as pneumonia, bronchiolitis, otitis media, conjunctivitis, and tonsillitis. The adenoviral detection rates indicate the potential contamination of the environment, with adverse effects on public health. Adenoviruses can cause severe or life-threatening illness, particularly in immunocompromised patients, children and the elderly. Some types are capable of establishing persistent asymptomatic infections in tonsils, adenoids, and intestines of infected hosts, and shedding can occur for months or years (Lessa et al., 2009; Osuolale and Okoh, 2015). Adenoviruses can occur anytime throughout the year but adenoviral respiratory infections are most common in the late winter, spring, and early summer.
Modes of transmission are also diverse, primarily spread by the respiratory route, person-to-person contact, fomites, and occasionally by airborne aerosols. Since AdVs are able to infect a wide range of tissues, they can be excreted in large numbers in different body fluids during the acute illness, including oral secretions and faeces. The spread by the fecal-oral route happens through the ingestion of contaminated food or water. Small doses of AdV in aerosols resulted in infection accompanied by febrile acute respiratory disease, sometimes with pneumonia. Humidity affects the viability and dispersal of AdVs in aerosol. These viruses tend to survive best at high relative humidities. Aerosols seem to be very resistant to UV air disinfection. Adenovirus outbreaks have been documented in different indoor environments, including health care facilities, schools, military hospitals and barracks, throughout the year (La Rosa et al., 2013).
2.3 Gastrointestinal Viruses Associated with Indoor Air Transmission
In developed countries, it is estimated that 30% ± 40% of infectious gastroenteritis cases are attributable to viruses. Rotavirus, Astrovirus, Norwalk-like viruses, also known as small round structured viruses and other caliciviruses are responsible for 48% of all reported outbreaks of infectious intestinal disease.
2.3.1 Rotavirus
Rotaviruses belong to the Reoviridae family; they are segmented bicatenary RNA viruses, which explain their genetic variability. Is the most common cause of severe diarrhea among children, resulting in the death of over 500,000 children annually worldwide. Rotaviral gastroenteritis is a serious public health problem in both developed and developing countries.
The disease occurs most often in the winter, with annual epidemics occurring from December to June. The highest rates of illness occur among infants and young children. A large proportion of hospital admissions due to gastroenteritis in children less than 5 years old are caused by rotavirus. Some adults acquired rotavirus infections a few days after their children’s illnesses, suggesting that the children rather than the parents brought infection into the home, though disease tends to be mild. Immunity after infection is incomplete, but repeated infections tend to be less severe than the original infection.
Rotavirus is shed in large numbers from an infected person by animate and non-porous inanimate surfaces. Excretion of the virus can persist for up to 57 days after diarrhea has stopped in symptomatic patients, contributing to an increase of the number of environmental surfaces contaminated with rotavirus. It has been suggested that low humidity and people spending more time indoors contribute to the spread of rotavirus infections. Handwashing is a very important means of preventing the spread of rotavirus (Barker et al., 2001; Anderson et al., 2004; Bernstein, 2009).
2.3.2 Norwalk-Like Virus
Norwalk-like viruses (NLVs), RNA virus belonging to Caliciviridae family, also known as small round structured viruses or caliciviruses, are an important cause of gastroenteritis outbreaks and are spread frequently through contaminated food or water. Projectile vomiting associated with NLVs is probably a major source of cross-infection because it is estimated that 3×107 particles are distributed as an aerosol into the environment during a vomiting attack. Carpets can also serve as reservoirs of infection.
Aerosols produced by vomiting can be inhaled or can contaminate hands or work surfaces, with the potential for subsequent transfer to foods or direct hand-to-mouth transfer. The importance of airborne transmission was demonstrated in a recent outbreak in a restaurant where no food source was detected but an analysis of the attack rate showed an inverse correlation with the distance from a person who had vomited. It was found that the risk of gastroenteritis amongst workers and customers who shared toilet facilities was twice of those who had a private bathroom (Green et al., 2000; Barker et al., 2001).
2.3.3 Enterovirus
Enteroviruses (EVs) are members of the Picornaviridae family, a large and diverse group of small RNA viruses present worldwide. In humans, EVs target a variety of different organs causing gastrointestinal, respiratory and myocardial and central nervous system diseases. In temperate climates, enteroviral infection occurs primarily in the summer and early fall. Although the majority of infections are asymptomatic or result in a self-limited illness, fatalities do occur, especially in neonates or individuals with B-cell immunodeficiency. Enterovirus outbreaks in neonatal units and school nurseries, reflects the susceptibility of infants to EVs infection, leading to extensive discussion on control measures and interventions.
Faecal-oral transmission is the major mode of transmission. Other important routes of transmission are person-to-person contact and the inhalation of airborne viruses in respiratory droplets. Infectious coxsackievirus, a member of the EV genus, in large droplets and droplet nuclei generated by coughs and sneezes as well as in the air of rooms contaminated by such discharges, transmit this viral infection by the airborne route. Aerosol transmission is suspected of having contributed significantly to the EV epidemic which infected up to 300,000 children and caused 78 deaths in Taiwan in 1998 (Chang et al., 2004; La Rosa et al., 2013).
2.3.4 Norovirus
Noroviruses (NoVs), emerging as the leading cause of epidemic gastroenteritis, are RNA viruses belonging to the family Caliciviridae, currently subdivided into five genogroups. NoVs are responsible for nearly half of all gastroenteritis cases and for more than 90% of non-bacterial infection epidemics worldwide. The illness can be severe and sometimes fatal, especially among vulnerable populations – young children, the elderly and the immunocompromised – and is a common cause of hospitalization. Encephalopathy, disseminated intravascular coagulation, convulsions, necrotizing enterocolitis, post-infectious irritable bowel syndrome, and infantile seizures highly contagious with a low infectious dose, occurs repeatedly.
Faecal-oral spread is the primary transmission mode and the foodborne and waterborne transmission. Airborne transmission of NoV is also a cause of acute viral gastroenteritis. Sources of contaminated aerosol are diverse. Droplets being inhaled can be deposited in the upper respiratory tract, and subsequently be swallowed along with respiratory mucus. Aerosol droplets produced during vomiting could settle onto indoor surfaces that might then be transferred to hands of exposed individuals through physical contact, or deposited on the floor from which they can be resuspended by human movement and turbulence. Aerosol droplets can also be generated from toilet flushing. Transmission via fomites is documented. The viruses were identified in indoor environments such as hospitals, schools, kindergartens, restaurants, care facilities, hotels and concert halls as well as airplanes, buses and cruise ships (Morillo and Timenetsky Mdo, 2011; La Rosa et al., 2013).
2.3.5 Enteric Adenovirues
Human adenoviruses (AdV) are classified into 47 serotypes and six subgenera (A–F) with different tropisms are associated with outbreaks of gastroenteritis in schools, paediatric hospital and nursing homes. They may be second to rotavirus as a cause of gastroenteritis in young children, especially newborns, mainly caused by serotypes AdV 40 and AdV 41 of subgenus F. The clinical characteristics include watery diarrhea accompanied by vomiting, low grade fever and mild dehydration. Institutionalized persons, immunocompromised persons and Transplant recipients seem to be among the most severely affected, with mortality rates as high as 60%. Respiratory symptoms are infrequent but some studies have suggested that adenovirus infections may be involved with chronic airway obstruction, pulmonary dysplasia, myocarditis and dilated cardiomyopathy, mononucleosis-like syndromes, sudden infant perinatal death and, perhaps most intriguingly, the development of obesity. Although these associations may or may not be causal, understanding adenovirus transmission seems to be the key to their further study. Adenoviruses are the most UV-resistant viruses, and their detection is now a key indicator of water quality (Uhnoo et al., 1990; Zlateva et al., 2005; Gray, 2006).
3 Healthcare Facilities Infections
Indoor air quality proves to be of great importance in hospitals due to the spread of air microorganisms maximizing nosocomial infections. Reports about infections correlated with the presence of viral aerosols in indoor air remain scarce. During and after illness, viruses are shed in large numbers in body secretions, including blood, faeces, urine, saliva, and nasal fluid (La Rosa et al., 2013). The microbial load in hospital indoor air is highline nuanced by the number of occupants, their activity and the ventilation. Occupants are a potential source of microorganisms as they shed the microorganisms from the skin squamous and the respiratory tract. Ventilation causes dilution thus reducing the microbial load. Sinks, wash-basins and drains, nebulisers, humidiphiers, and cooling towers are the potential sources which colonize on the moist surfaces. Sweeping of floors, changing of bed linens and entry into the hospital buildings through ventilation ducts also can be the sources of airborne microorganisms. Since exposure levels are high, this may be an issue for immunocompromised patients (Srikanth et al., 2008).
During the 2009–2010 flu seasons, size-resolved particle samples were collected on filters in a day care center and a health center. Influenza A virus was identified in 50% of the samples with concentrations ranging from 5800 to 37,000 genomes per cubic meter and a substantial proportion of the detected viruses was associated with fine particles (<2.5 μm) that can remain airborne for extended periods and that can also penetrate and deposit deeply in the respiratory tract when inhaled (Barker et al., 2001; Nazaroff, 2016).
Establishing how viruses are transmitted under different circumstances, and whether transmission requires close contact, is of great importance as such information will affect the choice of infection control measures in health-care settings (La Rosa et al., 2013).
In a hospital paediatric unit when there was an increase in the number of children suffering from rotavirus gastroenteritis, on the surfaces in direct contact with children (thermometers, play mats and toys) rotavirus was detected in 63% of samples compared with 36% for surfaces without direct contact (telephones, door handles and washbasins). Rotavirus was also found in hand washings of 19% of attendants of patients with non-rotavirus diarrhoea, indicating that they may have come into contact with other attendants and patients in adjacent beds. This highlights the potential for contaminated hands to spread the infection (Soule et al., 1999).
Norwalk-like virus gastroenteritis in an elderly care unit spread rapidly within and between wards, affecting both patients and staff. Although infectious aerosols were probably the main route of dissemination of infection within a particular cohort of guests, contact with contaminated fomites was the most likely factor responsible for maintaining the outbreak by forming the link between successive cohorts (Barker et al., 2001).
4 Farming Activities
Farming, one of the oldest professions of mankind, is by far the one that employs the largest number of individuals worldwide. Although outdoor country work is supposedly healthy, farmers are at risk of respiratory diseases because of their work environment. It is very well established that chronic and acute respiratory diseases have been associated with work in confinement operations, like under-floor manure pits. Respirable dust and asphyxiating gases such as hydrogen sulphide, carbon dioxide, methane, and ammonia in high concentrations were measured on these area stations (Reeve et al., 2013; Manbeck et al., 2016). But bioaerosols are recognized as a serious threat on these environments. Mice are prevalent on farms. Faeces of deer mice can be contaminated with the Hantavirus, which can cause a devastating infection in humans, an influenza-like syndrome that often leads to respiratory failure. Farmers should wear protective respiratory equipment when cleaning building areas where mouse droppings are present. Farms are also the usual sources of influenza outbreaks. Influenza viruses infect pigs or poultry that can be transferred from animals to humans even without a mutation. This has so far been the case of the Influenza A virus subtype H5N1 that, to date, only infected farmers in close contact with birds (Cormier, 2007).
In animal slaughterhouses handling out cattle and sheep is hypothesized that these environments would contain significant amounts of bioaerosol due to the mechanical processes used to kill and process animals, a high degree of splashing and fluid handling, and also a high relative humidity of the environment. Workers on these conditions and meatworkers having exposure to a number of significant zoonotic diseases including leptospirosis, parapoxvirus, human papillomavirus subtypes HPV2, HPV4 and HPV7 are known to be at occupational health risk. These workers are also affected by a higher-rate of malignancies of the lung compared to the general population (Hall et al., 2013). Farmers and consumers of fresh farm products from farms irrigated with river water may be at risk of infection from adenoviruses. The findings highlight the lurking dangers of using contaminated surface water and the need for routine monitoring of such waters for protection of public health (Sibanda and Okoh, 2012). Workers in concentrated animal feeding operations are at risk of adverse respiratory outcomes from exposures to indoor contaminants. Is indispensable an optimal management of indoor air quality, preventing the transmission of infectious respiratory disease to workers and animals (Kim et al., 2005).
5 Analyses Approaches for Virus
5.1 Virus Analysis Methods
5.1.1 Culture-Dependent Analysis
Considering that viruses are obligate intracellular parasites, the use of culture-dependent methods is achieved with the use of suitable hosts, such as whole animals or cultured cells. Currently the most commonly used methods for virus cultures are inoculation of viruses into embryonated eggs and tissue cultures.
5.1.1.1 Inoculation of Embryonated Eggs
Virus started to be propagated in whole animals or embryonated chicken eggs before the use of cell culture methods. Virus cultivation in embryonated eggs is intrinsically dependent on the utilized egg, which must be sterile and the shell should be intact and healthy. The inoculation of the samples is made by injection into the fluid of the egg through a hole drilled in the shell. Viral growth and multiplication is revealed by embryo death, cell damage or through the formation of typical pocks or lesions on the membranes. The selection of the sites of viral inoculation in embryonated eggs is dependent of the studied virus, as each virus has different preferential location for growth and replication.
-
Chorioallantoic Membrane (CAM): Virus growth and replication is indicated by visible lesions (pocks) derived, under optimal conditions, from a single virion and a grey white area in transparent CAM.
-
Allantoic Cavity: Usually utilized for growth and replication of virus for vaccine production, provide a rich yield of influenza, some paramyxoviruses and avian viruses isolation.
-
Amniotic Cavity: Virus growth and replication of virus can be analyzed by haemagglutination assay.
-
Yolk Sac: Frequently utilized for growth, multiplication and isolation of mammalian viruses.
Currently, embryonated egg inoculation is conventionally considered the “gold standard” method for isolation and propagation of virus such as the influenza virus (Jianqiang Zhang, 2014).
5.1.1.2 Cell Culture
Mammalian cell culture technology has become a prominent and fundamental field in modern biotechnology, especially in the area of human health and has replaced embryonated eggs as the preferred methodology for virus growth and replication. Cellular cultures rely on techniques such as media changes, passaging, and transfection under aseptic conditions to avoid contaminations (e.g. bacteria, yeast, among others). Presently, numerous valuable cell monolayers are commercially available, and are regularly utilized in clinical laboratories for the diagnosis of virus infections. Some of the most utilized cell are HeLa derivative (Hep2), rhesus monkey kidney cells (RhMK), human lung fibroblasts (MRC-5), human lung carcinoma cells (A549), among others. These cell lines are selected for their ability to support the replication of a wide variety of clinically relevant viruses due to their ability to express cell type-specific factors that contribute to pathology during viral infection. For instance A549 cell line is considered representative of the Alveolar Type II pneumocytes of the human lung as it exhibits features of an ATII epithelial cell phenotype. Applying such methodology enables the isolation of diverse viruses, such as adenovirus, CMV, RSV, influenza A & B, parainfluenza viruses types 1 to 3, VZV, as well as the Ebola virus, severe acute respiratory coronavirus (SARS-CoV), and human metapneumovirus (hMPV).
The recent adaptation of cellular cultures to shell vials with subsequent direct or indirect immunofluorescence technique has dramatically decreased the time of diagnostics for clinical samples from weeks to less than 48 h by staining for early antigens of viral infections. Currently, this methodology is the most sensitive, non-molecular viral detection method, utilized for the identification of viruses such as respiratory viruses, enterovirus and adenovirus among others. Although embryonated chicken egg inoculation is still considered the “gold standard” method for influenza virus isolation and propagation, several primary cells as well as continuous cell lines have also been developed for influenza virus isolation and replication (Jianqiang Zhang, 2014).
5.1.2 Culture-Independent Virus Analysis
5.1.2.1 Nucleic Acid Amplification
The development of nucleic acid amplification techniques has endorsed the advance of molecular tools for virus identification using low specimen quantity with higher sensitivity and specificity, at the same time dramatically decreasing the time for identification. Currently these methodologies are accepted as the gold standard for clinical virology and have been utilized for the identification of different viruses in environmental samples from diverse contexts.
5.1.2.2 Single Target Nucleic Acid Amplification
The fundamental principles of nucleic acid amplification techniques are based on the thermostable polymerase-based target nucleic acid amplification which results in the production of millions of copies of the targeted sequence. These amplification products are then analyzed through diverse techniques. The advances in molecular analysis techniques lead to the development of the real-time PCR where the target amplification and detection steps, using fluorescent dyes, occur concomitantly. This methodology uses copulated software that monitors the thermal cycler data at every cycle and produces a quantitative amplification plot for each reaction. Thus, RT-PCR allows the performance of viral load assays to quantitatively assess the amount of virus in a sample. Furthermore, a modification of polymerase chain reaction, nested polymerase chain reaction (nested PCR), has been developed in order to decrease non-specific binding in products. This methodology encompasses two sets of primers, used in two successive PCR runs, whereas the second set intended to amplify a secondary target within the first run product. Currently, nucleic acid amplification techniques are considered the gold standard for rapid and accurate detection of viruses, compared to methodologies such as shell vial cell cultures.
5.1.2.3 Multiplex Nucleic Acid Amplification
Multiplex PCR assays were developed based on single target nucleic acid amplification methodologies with the aim to quantify multiple nucleic acid targets using specific probes to diverse viral targets in a single PCR reaction, allowing the assessment of viral co-infections. Currently, for respiratory viruses three FDA-approved platforms for multiplex PCR assays are available.
-
Multiplex PCR combined with liquid-phase bead-based array technology.
-
Multiplex RT-PCR followed by electrochemical detection of hybridized capture probes on gold-plated electrodes.
-
Multiplex-PCR preceded by nested RT-PCR with detection trough melt curve analysis.
5.1.2.4 Sequencing and Genotyping
Currently, DNA sequencing is considered one of the most valuable, accurate and consistent methodologies for microorganisms identification and is applied in contexts were quick and precise identifications are required. This method is used to determine the exact sequence of a certain stretch of DNA. Several new sequencing technologies have been developed (next generation sequencing) with the aim to provide fast/efficient techniques for analysis of microorganisms bioburden. Genotyping assays utilize a combination of PCR and nucleic acid sequencing to identify viral genotypes. Genotyping methodology allows for the identification of genetic variants and can be performed via genotyping chips or arrays, depending on the variants of interest and resources available. Viral genotyping is mostly utilized to provide relevant clinical data to predict therapeutic responses to antiviral drugs and/or epidemiologic comparison.
5.2 Viral Contamination Assessments in Environmental Samples
Currently, it is a consensus among researchers that methodologies based on nucleic acid amplification techniques offer advantages compared with traditional methods such as inoculation on embryonated eggs and cell culture, due to higher sensitivity, specificity and fast results, which will be further discussed. A comparison between the different viral identification methods is presented in Table 7.1. The efficacy of sampling methodologies for viruses in environmental samples is still a matter of intense debate. A meta-analysis study performed with the aim to assess the efficacy of virus concentration methods associated to the molecular detection of adenovirus demonstrated that for detection in environmental samples qPCR or Nested-PCR should be prioritized over PCR; in water samples (e.g. rivers or lakes) ultracentrifugation should be associated with nested-PCR and that microfiltration membrane, ultrafiltration, and qPCR must be associated for assessment of treated and untreated sewage samples (Silva and Melo, 2010).
5.2.1 Viral Contamination in Water
It is currently acknowledged that viral contamination of recreational water presents a high risk of infection and is considered a significant public health hazard. Published studies, summarized in Table 7.2, have addressed the assessment of virus bioburden in water environmental samples. The most commonly found viruses in aquatics environments are enteric viruses, such as Enterovirus, Rotavirus and Norovirus, Adenovirus and Hepatitis Virus A and C. Begier and coworkers have correlated swimming in polluted seawater with enterovirus infection (Begier et al., 2008). For enteroviruses, the most common mode of transmission is the fecal-oral route, although aerosol transmission has also been reported. In a similar manner, drinking water contaminated with virus, such as Norovirus, also presents a risk for human health, highlighting the importance of good hygiene practices with respect to water storage, Shin and Sobsey suggested that water chlorination could inactivate enteric viruses (Shin & Sobsey, 2008). Sample concentration is a critical step in viral diagnosis, since the number of viral particles in water is generally very low, which often results in false results if samples are tested directly using PCR (Katayama et al., 2002). Therefore, some authors choose an adsorption–elution method, followed by ultrafiltration, to concentrate the viruses, before nested-PCR or quantitative Real Time PCR. In severally contaminated environments such as hospital wastewater treatment plants, Prado and coworkers utilized PCR/RT-PCR, quantitative real-time PCR (qPCR) and genome sequencing, after sample concentrations techniques, to assess the presence of viruses associated with human pathologies such as acute gastroenteritis and hepatitis (Prado et al., 2011). In intermediate contaminated environments, such as urban and bathing waters the assessment of microbial hazards with potential public health risk associated with viral contamination also preferentially utilizes nucleic acid amplification methodologies, after sample concentration.
Some authors chose to utilize the combination of culture dependent and independent methodologies for virus identification from environmental samples. In a study performed by Roberto A. Rodríguez and coworkers that aimed to assess the effects of sewer overflows to the viral contamination of receiving waters, concentrated samples were assayed for total culturable viruses using the PLC/PRF/5 cell line with associated confirmation by PCR/RT-PCR (Rodríguez et al., 2012).
5.2.2 Viral Contamination on Surfaces
Viruses can be transmitted directly from individual to individual via sneezing, coughing and touching, or indirectly via the environment. The prevalence of pathogenic viruses in healthcare settings potentially transmitted by airborne, droplet and contact represents a significant threat for both workers’ and patients’ health. Thus, most of the presently performed studies regarding virus contamination of surfaces have focused on clinical settings, as demonstrated in Table 7.3. The data resultant from these studies is of foremost importance since it can allow the identification of critical locations and direct the selection of infection control measures for health-care settings to decrease viral associated nosocomial infections. Protocols regarding transmission based precautions in both hospital personnel and patients are continuously updated at the international level (La Rosa et al., 2013).
5.2.3 Viral Aerosol Contamination
Airborne diseases are caused by pathogens transmitted through the air, that may be spread through coughing, sneezing, resuspension of dust, spraying of liquids, or similar activities likely to generate aerosol particles or droplets. The World Health Organization (WHO) has suggested that aerosol exposure may be the major route for spreading viral diseases (World Health Organization, 2010). Environmental monitoring of airborne viruses could provide an early indicator of dangerous viruses in the air. Filtration methods that may utilize gelatin membrane filters, impaction collectors and impingers are usually used to collect viral aerosols. Sampling using air filters for several hours with posterior extraction and nucleic acid amplification can increase the sensitivity of virus detection. Currently, well-established filter/real-time qPCR assays are performed to successfully measure viral aerosols. The prevalence of respiratory tract infections is intrinsically associated with respiratory viruses which account for high percentage of pediatric as well as adult infections. A study performed in a pediatrics department of a medical center, detected influenza A virus, human adenovirus, and enterovirus in aerosol samples trough filtration method combined with real-time quantitative polymerase chain reaction (qPCR) technique (Tseng et al., 2010). In hospital settings, torque teno virus has been detected in samples collected with an impactor sampler with posterior culture in Tryptone Soy Agar (TSA) and identification trough nested RT-PCR (Carducci et al., 2011) or trough Burkard C90M cyclone sampler and qRT-PCR (D’Arcy et al., 2014).
Nevertheless, culture-dependent methods and nucleic acid amplification techniques can also be used simultaneously. As an example, a study performed by Goyal and coworkers utilized embryonated eggs and tissue cultures of Vero, MDCK, and RK-13 cell lines combined with nucleic acid extraction, PCR, RT-PCR and Nucleic acid sequencing to assess contamination of respiratory viruses (VSR, Influenza A and B, Parainfluenza 1, 2 and 3, Rinovirus, Enterovirus, Coronavirus, Filoviruses, Adenovirus and Orthopoxvirus) and viruses with bioterrorism potential in ventilation filters from two large public buildings (Goyal et al., 2011).
5.3 State of the Art and Future Directions
The assessment of viral contamination and/or infections play a key role in reducing global viral disease associated burden. It is currently acknowledged that the advances and development of molecular assays such as PCR, qRT-PCR, genotyping and multiplex assays endorsed important improvements in viral assessments regarding sensitivity, specificity, speed, simplicity and cost-effectiveness. Nevertheless, the developments of new approaches that can provide alternatives to evade the limitations of nucleic acid amplification techniques are of foremost importance. In this context, currently nanobiosensors represent a new promising tool for virus detection. This methodology, still at research stage, encompasses the technology of viral disease biosensors with nanoparticles and nanomaterials, focused on the development of miniaturized biosensors with high sensitivity, specificity, and stability. This state of the art technology aims to deliver an alternative tool for effective and rapid viral disease diagnosis with no requirement of highly trained personnel or heightened laboratory facilities (Kizek et al., 2015).
6 Concluding Notes
During the last two decades, there has been increasing concern within the scientific community over the effects of indoor air quality on human health. Everything looked definitive when vaccines were produced, diseases had the end announced, but the truth is that infections insist on persisting in our common environment although the better knowledge.
Changes in building design formulated to improve energy efficiency have meant that modern homes and offices are frequently more airtight than older structures. Indoor pollutants can emanate from a range of sources and we know much less about the health risks from indoor air pollution than we do about those attributable to the contamination of outdoor air (Jones, 1999).
The indoor environments to be considered are those ordinarily and commonly occupied by humans: residences, offices, schools, industrial buildings, hospitals and other settings occupied a high proportion of the time, or in which occupant density is high (Hanski et al., 2012). Biological hazards to man arise from exposure to high concentrations forms of bio-aerosols and three major groups of diseases associated with bio-aerosol exposure are infectious diseases, respiratory diseases and cancer. Current knowledge is unclear regarding risk to cancer whether these excess risks occur from exposures to biological agents or are due to various chemicals used in industries (Srikanth et al., 2008).
Acclimated environments have an artificially multitude of chemical compounds (toxic, carcinogenic, radioactive) and biological (pathogenic) issued by a variety of sources, depending on the physical conditions (air humidity, air temperature, inadequate ventilation) of the environment. The air recirculation phenomenon is responsible for the increase of pathogenic microorganisms in the order of 1000 to 100,000 times in relation to the external air (Lee et al., 2006). Incorrect cleaning filters and ducts of air conditioning provide the development of microbial particles including viruses that may lead the occupants of air-conditioned environments contracting respiratory infections or allergic diseases. Viruses can persist in sufficient number to act as sources of infection for several hours, weeks or even months.
The level of information and awareness of agricultural health and safety risks, disease, and injury prevention among the dairy farmers is low. Training on health and safety in agriculture field is urgently needed.
Safe working conditions are essential for healthy living. The lack of a preventive policy maintenance programmes in refrigeration and ventilation systems is the determining factor for the occurrence of biological pollutants. Take corrective actions preventing the spread of pathogens by the airborne route requires the use of special air handling and ventilation systems, such as airborne infection isolation rooms to contain and then safely remove the infectious agents. In addition, respiratory protection with validated and certified equipment is recommended (Fisk et al., 2007).
Environments have been studied more extensively than other issues due to their greater clinical significance. However, more work is still needed to provide a clearer picture regarding the rates of viral diseases transmission, airborne transmission in particular, in closed environments, and potential ways for reducing the levels of indoor viral pollution and transmission must be investigated. Studies including homes, non-industrial workplaces and public buildings, are scarce (Prussin II et al., 2015).
Ventilation filters of two large public buildings were sampled to determine the presence of human respiratory viruses by polymerase chain reaction and reverse-transcription polymerase chain reaction. Nine of the 64 filters tested were positive for influenza A virus, two filters were positive for influenza B virus, and one filter was positive for parainfluenza virus 1. Filters are installed in HVAC systems of buildings to protect ventilation equipment and maintain healthy indoor air quality. These filters process enormous volumes of air. Building HVAC filters may be used as a method of detection for airborne viruses. They may yield valuable information on the epidemiology and aerobiology of viruses in air that can report to the development of methods to prevent airborne transmission of viruses (Goyal et al., 2011). Regrettably, several investigations have revealed that many HVAC installations have a lot of operational and maintenance problems. Numerous practical recommendations for design and operation of HVAC systems are needed. Following the recommendations will result in less pollution and increased indoor environmental quality (Hanssen, 2004). Basic strategies of source control should not to make indoor air sterile but keep indoor environments dry, maintain good hygienic conditions in ventilation systems, apply effective filtration on mechanical supply ventilation, and use masks in the event of respiratory illness. The importance of hands in the transmission of viruses is well recognized and many of the studies relate specifically to handwashing.
The number of asthma patients in most industrial countries has greatly increased, resulting in a morbidity rate of around 10−15% of the population. May be aerosol transmission is responsible for the most severe cases of disease involving viral infection of the lower respiratory tract (Tellier, 2009; Tsukagoshi et al., 2013).
References
Anderson EJ, Weber SG (2004 Feb) Rotavirus infection in adults. Lancet Infect Dis 4(2):91–9
Artenstein MS, Miller WS (1966) Air sampling for respiratory disease agents in army recruits. Bacteriol Rev 30(3):571–572
Ballow M (2008) Approach to the patient with recurrent infections. Clin Rev Allergy Immunol 34(2):129–140
Barker J, Stevens D, Bloomfield SF (2001) Spread and prevention of some common viral infections in community facilities and domestic homes. J Appl Microbiol 91:7–21
Begier EM, Oberste MS, Landry ML et al (2008) An outbreak of concurrent echovirus 30 and coxsackievirus A1 infections associated with sea swimming among a group of travelers to Mexico. Clin Infect Dis 47(5):616–623. doi:10.1086/590562
Bernstein DI (2009) Rotavirus overview. Pediatr Infect Dis J 28(3):50–53
Canonica GW, Ciprandi G, Pesce GP et al (1995) ICAM-1 on epithelial cells in allergic subjects: a hallmark of allergic inflammation. Int Arch Allergy Immunol 107(1–3):99–102
Carducci A, Verani M, Lombardi R et al (2011) Environmental survey to assess viral contamination of air and surfaces in hospital settings. Journal of Hospital Infection 77(3):242–247. doi:10.1016/j.jhin.2010.10.010
Celli BR, Macnee W (2004) Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 23:932–946
Celli BR, Barnes PJ (2007) Exacerbations of chronic obstructive pulmonary disease. Eur Respir J. 29(6):1224–1238
Chang LY, Tsao KC, Hsia SH et al (2004) Transmission and clinical features of enterovirus 71 infections in household contacts in Taiwan. JAMA 291(2):222–227
Chen SC, Chio CP, Jou LJ et al (2009) Viral kinetics and exhaled droplet size affect indoor transmission dynamics of influenza infection. Indoor Air 19:401–413
Chen SC, Liao CM (2010) Probabilistic indoor transmission modeling for influenza (sub) type viruses. J Infect 60(1):26–35
Cormier Y (2007) Respiratory health and farming: an essay. Can Respir J 14(7):419–422
D’Arcy N, Cloutman-Green E, Klein N et al (2014) Environmental viral contamination in a pediatric hospital outpatient waiting area: implications for infection control. Am J Infect Control 42(8):856–860. doi:10.1016/j.ajic.2014.04.014
Douwes J, Thorene P, Pearce N et al (2003) Bioaerosol health effects and exposure assessment: progress and prospects. Ann Occup Hyg 47:187–200
Fisk WJ, Lei-Gomez Q, Mendell MJ (2007) Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air 17(4):284–296
Fongaro G, Nascimento MA, Viancelli A et al (2012) Surveillance of human viral contamination and physicochemical profiles in a surface water lagoon. Water Sci Technol. 66(12):2683–2687. doi:10.2166/wst.2012.504
Gallimore CI, Taylor C, Gennery AR et al (2006) Environmental monitoring for gastroenteric viruses in a pediatric primary immunodeficiency unit. J Clin Microbiol 44(2):395–399. doi:10.1128/JCM.44.2.395
Gallimore CI, Taylor C, Gennery AR et al (2008) Contamination of the hospital environment with gastroenteric viruses: comparison of two pediatric wards over a winter season. J Clin Microbiol 46(9):3112–3115. doi:10.1128/JCM.00400-08
Ganime AC, Carvalho-Costa FA, Mendonça MCL et al (2012) Group A rotavirus detection on environmental surfaces in a hospital intensive care unit. Am J Infect Control 40(6):544–547. doi:10.1016/j.ajic.2011.07.017
Goh GK, Dunker AK, Uversky V (2013) Prediction of intrinsic disorder in MERS-CoV/HCoV-EMC supports a high oral-fecal transmission. PLoS Curr 13(1):1–63
Goyal SM, Anantharaman S, Ramakrishnan MA et al (2011) Detection of viruses in used ventilation filters from two large public buildings. Am J Infect Control 39(7):e30–e38. doi:10.1016/j.ajic.2010.10.036
Gray GC (2006) Adenovirus transmission – worthy of our attention. J Infect Dis 194(7):871–873
Green KY, Ando T, Balayan MS et al (2000) Taxonomy of the caliciviruses. J Infect Dis 181(2):322–330
Hall RJ, Mily LM, Wang J et al (2013) Metagenomic detection of viruses in aerosol samples from workers in animal slaughterhouses. PLoS One 8(8):1–8
Hanski I, von Hertzen L, Fyhrquist N et al (2012) Environmental biodiversity, human microbiota, and allergy are interrelated. Proc Natl Acad Sci U S A 109(21):8334–8339
Hanssen SO (2004) HVAC – the importance of clean intake section and dry air filter in cold climate. Indoor Air 14(7):195–201
Heikkinen T, Jarvinen A (2003) The common cold. Lancet 361:51–59
Hui DS, Chan PK (2010) Severe acute respiratory syndrome and coronavirus. Infect Dis Clin North Am 24(3):619–638
Huynh KN, Oliver BG, Stelzer S et al (2008) A new method for sampling and detection of exhaled respiratory virus aerosols. Clin Infect Dis 46(1):93–95
Ibfelt T, Engelund EH, Schultz AC et al (2015) Effect of cleaning and disinfection of toys on infectious diseases and micro-organisms in daycare nurseries. J Hosp Infect 89(2):109–115. doi:10.1016/j.jhin.2014.10.007
Ignatius TS, Yu, Li Y et al (2004) Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Engl J Med 350:1731–1739
Jianqiang Zhang PCG (2014) Isolation of swine influenza virus in cell cultures and embryonated chicken eggs. Methods Mol Biol. 1161:265–276. doi:10.1007/978-1-4939-0758-8_22
Jones AP (1999) Indoor air quality and health. Atmos Environ 33(28):4535–4564
Katayama H, Shimasaki A, Katayama H et al (2002) Development of a virus concentration method and its application to detection of enterovirus and Norwalk Virus from Coastal Seawater. Appl Environ Microbiol 68(3):1033–1039. doi:10.1128/AEM.68.3.1033
Kim KY, Ko HJ, Lee KJ et al (2005) Temporal and spatial distributions of aerial contaminants in an enclosed pig building in winter. Environ Res 99(2):150–157
Kizek R, Krejcova L, Michalek P et al (2015) Nanoscale virus biosensors: state of the art. Nanobiosensors Dis Diagn 4:47. doi:10.2147/NDD.S56771
Klepeis NE, Nelson WC, Ott WR et al (2001) The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol 11:231–252
La Rosa G, Fratini M, Della Libera S et al (2013) Viral infections acquired indoors through airborne, droplet or contact transmission. Ann Ist Super Sanità 49(2):124–132
Lax S, Smith DP, Hampton-Marcell J et al (2014) Longitudinal analysis of microbial interaction between humans and the indoor environment. Science 345:1048–1052
Lee ByungUk, Hong InGi, Lee DaeHee et al (2012) Bacterial bioaerosol concentrations in public restroom environments. Aerosol Air Qual Res 12:251–255
Lee T, Grinshpun SA, Martuzevicius D et al (2006) Relationship between indoor and outdoor bioaerosols collected with a button inhalable aerosol sampler in urban homes. Indoor Air 16(1):37–47
Lessa FC, Gould PL, Pascoe N et al (2009) Health care transmission of a newly emergent adenovirus serotype in health care person nel at a military hospital in Texas. J Infect Dis 200(11):1759–1765
Li Fang (2013) Receptor recognition and cross-species infections of SARS coronavirus. Antiviral Res 100(1):246–254
Ling WX, Juan S, Qin SQ et al (2016) Viral contamination source in clinical microbiology laboratory. Biomed Environ Sci 29(8):609–611. doi:10.3967/bes2016.082
MacIntyre CR, Ridda I, Seale H et al (2012) Respiratory viruses transmission from children to adults within a household. Vaccine 30(19):3009–3014
Manbeck HB, Hofstetter DW, Murphy DJ et al (2016) Online design aid for evaluating manure pit ventilation systems to reduce entry risk. Fronti Public Health 4(108):1–16
Morillo SG, Timenetsky Mdo C (2011) Norovirus: an overview. Rev Assoc Med Bras 57(4):453–458
Nazaroff WW (2016) Indoor bioaerosol dynamics. Indoor Air 26(1):61–78
Osuolale O, Okoh A (2015) Incidence of human adenoviruses and hepatitis A virus in the final effluent of selected wastewater treatment plants in Eastern Cape Province, South Africa. Virol J 12(98):1–8
Paba P, Farchi F, Mortati E et al (2014) Screening of respiratory pathogens by Respiratory Multi Well System (MWS) r-gene™ assay in hospitalized patients. New Microbiologica 37:231–236
Poutanen SM, Low DE, Henry B et al (2003) Identification of severe acute respiratory syndrome in Canada. N Engl J Med 348:1995–2005
Prado T, Silva DM, Guilayn WC et al (2011) Quantification and molecular characterization of enteric viruses detected in effluents from two hospital wastewater treatment plants. Water Res 45(3):1287–1297. doi:10.1016/j.watres.2010.10.012
Prussin II AJ, Garcia EB, Marr LC (2015) Total virus and bacteria concentrations in indoor and outdoor. Environ Sci Technol 2(4):84–88
Reeve KA, Peters TM, Anthony TR (2013) Wintertime factors affecting contaminant distribution in a swine farrowing room. J Occup Environ Hyg 10(6):287–296
Rodríguez RA, Gundy PM, Rijal GK et al (2012) The impact of combined sewage overflows on the viral contamination of receiving waters. Food Environ Virol 4(1):34–40. doi:10.1007/s12560-011-9076-3
Shin GA, Sobsey MD (2008) Inactivation of norovirus by chlorine disinfection of water. Water Res 42(17):4562–4568. doi:10.1016/j.watres.2008.08.001
Sibanda T, Okoh AI (2012) Assessment of the incidence of enteric adenovirus species and serotypes in surface waters in the Eastern Cape Province of South Africa: Tyume River as a case study. ScientificWorldJournal 949216:1–9
Silva HD, Melo MR (2010) Artículo original Avaliação de métodos de concentração e detecção molecular de adenovírus em águas não tratadas – uma metanálise, 65–71.
Soule H, Genoulaz O, Gratacap-Cavallier B et al (1999) Monitoring rotavirus environmental contamination in a paediatric unit using polymerase chain reaction. Infect Control Hosp Epidemiol 20:432–434
Srikanth P, Sudharsanam S, Steinberg R (2008) Bio-aerosols In indoor environment: composition, health effects and analysis. Indian J Med Microbiol 26(4):302–312
Tantilipikorn P, Auewarakul P (2011) Airway allergy and viral infection. Asian Pac J Allergy Immunol 29:113–119
Tellier R (2009) Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface 6:783–790
Tseng CC, Chang LY, Li C (2010) Detection of airborne viruses in a pediatrics department measured using real-time qPCR coupled to an air-sampling filter method. J Environ Health 73(4):22–28
Tsukagoshi H, Ishioka T, Noda M et al (2013) Molecular epidemiology of respiratory viruses in virus-induced asthma. Front Microbiol 4(278):1–10
Uhnoo I, Svensson L, Wadell G (1990) Enteric adenoviruses. Baillieres Clin Gastroenterol 4(3):627–642
von Mutius E (2004) Influences in allergy: epidemiology and the environment. J Allergy Clin Immunol 113(3):373–379
World Health Organization. (2010). Limiting spread. Retrieved from http://www.who.int/influenza/resources/research/research_agenda_influenza_stream_2_limiting_spread.pdf
Yang W, Elankumaran S, Marr LC (2011) Concentrations and size distributions of airborn e influenza A viruses measured indoors at a health centre, a day-care centre and on aeroplanes. J R Soc Interface 8:1176–1184
Zhang CM, Wang XC, Liu YJ et al (2008) Characteristics of bacterial and viral contamination of urban waters: a case study in Xi’an, China. Water Sci Technol. 58(3):653–660. 10.2166/wst.2008.438
Zhao H, Joseph C, Phin N (2007) Outbreaks of influenza and influenza-like illness in schools in England and Wales, 2005/06. Euro Surveill 12(5):3–4
Zhou LF, Zhu HH, Lin J et al (2006) Surveillance of viral contamination of invasive medical instruments in dentistry. J Zhejiang Univ Sci B 7(9):745–748. doi:10.1631/jzus.2006.B0745
Zlateva KT, Maes P, Rahman M et al (2005) Chromatography paper strip sampling of enteric adenoviruses type 40 and 41 positive stool specimens. Virol J 2(6):1–5
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Ribeiro, E., Leitão, C., Cristovam, E., Dias, A. (2017). Viruses Present Indoors and Analyses Approaches. In: Viegas, C., Viegas, S., Gomes, A., Täubel, M., Sabino, R. (eds) Exposure to Microbiological Agents in Indoor and Occupational Environments. Springer, Cham. https://doi.org/10.1007/978-3-319-61688-9_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-61688-9_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-61686-5
Online ISBN: 978-3-319-61688-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)