Abstract
The goal of this work is to evaluate if changes in brain connectivity can predict behavioral changes among subjects who have suffered stroke and have completed brain-computer interface (BCI) interventional therapy. A total of 23 stroke subjects, with persistent upper-extremity motor deficits, received the stroke rehabilitation therapy using a closed-loop neurofeedback BCI device. Over the course of the entire interventional therapy, resting-state fMRI were collected at two time points: prior to start and immediately upon completion of therapy. Behavioral assessments were administered at each time point via neuropsychological testing to collect measures on Action Research Arm Test, Nine-Hole Peg Test, Barthel Index and Stroke Impact Scale. Resting-state functional connectivity changes in the motor network were computed from pre- to post-interventional therapy and were combined with clinical data corresponding to each subject to estimate the change in behavioral performance between the two time-points using a machine learning based predictive model. Inter-hemispheric correlations emerged as stronger predictors of changes across multiple behavioral measures in comparison to intra-hemispheric links. Additionally, age predicted behavioral changes better than other clinical variables such as gender, pre-stroke handedness, etc. Machine learning model serves as a valuable tool in predicting BCI therapy-induced behavioral changes on the basis of functional connectivity and clinical data.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
- Brain-computer interface
- Stroke rehabilitation
- BCI therapy
- Upper extremity motor recovery
- Resting-state fMRI
- Machine learning
- Predictive model
1 Introduction
Approximately 800,000 individuals in the U.S. experience a new or recurrent stroke (ischemic or hemorrhagic) each year [7]. In recent years, there has been a significant decrease in stroke mortality, indicating that most stroke subjects survive their initial stroke event; however, survivors are often left with life-long impairments involving one or more of their motor, speech, visual etc., abilities. Specifically, upper extremity motor deficits are frequently observed in 30–66% of stroke survivors after six months of the stroke [6]. The majority of subjects have some spontaneous functional recovery after a stroke event. However, rehabilitative therapies can further improve motor recovery several months after stroke to enhance quality of life for survivors [13].
An emerging technology for stroke rehabilitation that has been shown to stimulate additional recovery is brain-computer interface (BCI). Electroencephalogram (EEG)-based BCI detects neural signals and uses them as inputs to provide real-time feedback, enabling users to modulate their own brain activity. This is a promising therapy for those with motor disabilities by allowing self-modulation of neural signals to control assistive devices such as computers during rehabilitative tasks without relying on residual muscle control [3]. Previous studies have shown potential functional benefits associated with the use of BCI technology in stroke rehabilitation including neural reorganization and improved behavioral and motor function [8, 10, 11, 13]. Real-time feedback in the form of reward for the production of certain brain activity patterns relative to others while performing a task raises the possibility that there are changes in brain activation patterns produced during tasks similar to those involved in BCI therapy; an important implication could be that BCI therapy can induce detectable changes in brain activation patterns in stroke subjects.
Studies have suggested that an association exists between resting-state networks and the reorganization of neural processes in post-stroke motor recovery [2, 11]. Resting-state functional magnetic resonance imaging (rs-fMRI) is a powerful tool to measure the temporal correlation of the spontaneous, low-frequency (<0.1 Hz) blood oxygenation level dependent (BOLD) signals across regions in the resting brain. Oscillations in the BOLD fMRI signals are indicative of self-organizing dynamic behavior of the brain, and these fluctuations are suggested to be associated with the flexibility and variability in motor function and cognition [1, 5]. Recent neuroimaging studies have demonstrated that there are overlapping networks involved during resting-state fMRI as well as motor imagery and motor execution fMRI tasks [4, 8]. The motor network commonly includes cortical areas such as the primary motor area (M1), premotor cortex (PMC) and supplementary motor area (SMA) as it is widely accepted that activity in these cortical regions maintains a dynamic equilibrium at resting-state and is modulated during task performance. Prior work indicates that resting-state brain connectivity can be potentially used to track brain changes following brain-computer interface (BCI) therapy [8], which serves as the motivation for this present study.
EEG-based BCI intervention is a promising rehabilitation therapy for improving motor function after stroke; however, the changes in functional connectivity in the brain following this therapy are not fully understood. Changes in resting-state functional connectivity (rs-FC) were examined in eight seed regions of interest within the motor network that play a dominant role in motor development, specification and execution. Specifically intra-hemispheric and inter-hemispheric connectivity measures were compared within this network. The aim of this present study was to investigate the effect of BCI interventional therapy using a closed-loop neurofeedback device intended to improve motor function in stroke subjects on behavioral performance metrics using changes in rs-FC in the motor network by analyzing data of 23 stroke subjects. To study the change in FC and behavior over time, we chose to utilize rs-fMRI data from two different time points, namely before starting and immediately upon completion of the interventional therapy. Additionally, clinical variables associated with the subjects were factored in. A number of behavioral measures were collected during neuropsychological assessments that served as the behavioral outcome variables. With the help a non-linear machine learning regression model, we analyzed the correlation between change in FC and clinical variables to change in behavioral outcomes.
2 Materials and Methods
2.1 Study Design
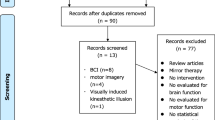
A permuted-block design that included subject characteristics such as gender, stroke chronicity and severity of motor impairment was employed to randomly assign subjects to either the Crossover Control group or BCI therapy group (Experimental Only). Subjects in the BCI therapy group received interventional rehabilitation therapy with functional assessment and MRI scans at four time points: (1) pre-therapy, (2) mid-therapy, (3) post-therapy and (4) 1 month after completing the last BCI therapy. Subjects in the Crossover Control group first received three functional assessments and MRI scans during the control phase in which no BCI therapy was administered, and their assessments were spaced at intervals similar to those given during the BCI therapy phase. After completing the control phase of the study, the Crossover Control group moved to the BCI therapy phase of the study. This study paradigm, as illustrated in Fig. 1, was chosen to determine if any outcome effects were attributable to BCI training vs. practice effects. All subjects completed at least 9 and up to 15 two-hour sessions of interventional BCI therapy. For the purposes of this study, we chose to analyze the change in rs-FC and change in behavior between time points (1) and (3) i.e. pre-therapy to post-therapy. Furthermore, we combined the subjects from the Crossover Control group and the BCI therapy into a single sample group to provide more power to the analysis.
Study paradigm of BCI-EEG interventional therapy [13]
2.2 Sample Characteristics
Subjects were recruited as part of an ongoing stroke rehabilitation study to evaluate interventional therapy using a BCI device targeting upper extremity motor function. Inclusion criteria were as follows: (1) at least 18 years or older; (2) persistent upper extremity motor impairment resulting from ischemic or hemorrhagic stroke; (3) ability to provide written informed consent. Exclusion criteria included: (1) concurrent neurodegenerative or other neurological disorders; (2) psychiatric disorders or cognitive deficits that would preclude a subject’s ability to provide informed consent; (3) pregnant or likely to become pregnant during the study; (4) allergies to electrode gel, metal and/or surgical tape, contraindications to MRI; (5) concurrent treatment for infectious disease. All participants provided written informed consent. The Health Sciences Institutional Review Board of the University of Wisconsin-Madison approved the study, including all of the measures assessed and therapies administered to subjects. The mean age of the sample was 63 years. The sample included 10 female and 13 male subjects; 20 right-handed subjects, 2 left-handed subjects and 1 ambidextrous subject; 13 subjects with a right-hemispheric lesion and 10 subjects with a left-hemispheric lesion. Individual study subject characteristics are summarized in Table 1 below.
2.3 BCI Intervention Procedure
The BCI-EEG setup is presented in Fig. 2. The closed-loop neurofeedback device used in therapy incorporates feedback from EEG from visual display, tongue stimulation and functional electrical stimulation. Subjects received no more than three sessions of interventional therapy per week, and the total BCI therapy lasted up to six weeks. The BCI therapy ran on the BCI2000 software 9 version 2 with modifications for administering tongue stimulation (TDU 01.30, Wicab Inc.), along with functional electrical stimulation (FES) (LG-7500, LGMedSupply; Arduino 1.0.4). EEG signals were detected and recorded from a 16-channel EEG cap and amplifier (Guger Technologies) during the BCI therapy.
BCI-EEG interventional therapy setup [8]
Each session started with an open-loop screening task to optimize the control signals. During this screening task, each subject was asked to move either their left or right hand with resting periods in between; this was conducted using words on a screen as cues, “right”, “left” or “rest”, in blocks of 4 s. The specific movements, that subjects chose, ranged from opening or closing one’s hand, squeezing hand and wrist flexion; these movements served as baseline abilities for each individual. During the screening session, the subjects were not given any feedback. Attempted movement was used for the initial screening and closed-loop feedback conditions to structure the neurofeedback training conditions similar to the mental processes used when performing real-world movement. For this reason, control signals were based on neural activity patterns of subjects performing movement to aid in strengthening the persistence of movement-related brain activity patterns. Following the initial screening, subjects performed a closed-loop task, where they received real-time visual feedback in the context of a game to gain training on how to modulate brain activity while moving each hand. In the game, subjects were prompted to move a cursor (ball) onto a target area, and target areas were positioned on the left or right side of the computer screen. Subjects were told to move his/her left or right hand to control the movement of the ball towards the direction of the target presented on the screen. Real-time EEG signals were used to calculate lateral cursor movement. During each BCI therapy session, all subjects completed 10 runs of the game, each run including 8–12 trials, with visual feedback.
Once subjects successfully completed 10 runs of the game with visual feedback and achieved consistent accuracy (≥70%), both tongue stimulation and functional electrical stimulation (FES) were incorporated into the session. Tongue stimulation, continuous electro-tactile stimulation of the tongue on an electrode grid, was administered in each following trial. FES was administered to muscles of the impaired arm when neural activity signals corresponding to impaired arm movement were detected on EEG during a trial in which subjects had to move the cursor to a target on the screen that matched the side of the impaired arm. In order to keep subjects engaged in the tasks, the size of the target on the screen could be changed to increase the difficulty of the task if they showed normal cursor control and accuracy. Additionally, if subjects were unable to perform the task with proper cursor control, the task difficulty could be reduced.
2.4 Data Acquisition
Neuroimaging scans were acquired at all the four time points mentioned previously. However, we chose to use the imaging data from two of those four time points, namely: time point (1) i.e. prior to starting the intervention and time point (3) i.e. immediately upon completion of intervention. Rs-fMRI scans were acquired on GE 750 3T MRI scanners (GE Healthcare, Waukesha, WI) using an 8-channel head coil. 10-minute resting state scans were acquired while subjects’ eyes were closed using single-shot echo-planar T2*-weighted imaging: TR = 2.6 s, 231 time-points, TE = 22 ms, FOV = 22.4 cm, flip angle = 60°, voxel dimensions of 3.5 × 3.5 × 3.5 mm3, 40 slices. T1-weighted axial images were obtained at the start of each scan using FSPGR BRAVO sequence (TR = 8.132 ms, TE = 3.18 ms, TI = 450 ms) over a 256 × 256 matrix with 156 slices (flip angle = 12°, FOV = 25.6 cm and slice thickness = 1 mm).
2.5 Neuropsychological Assessment
In order to assess the behavioral impact of the BCI therapy, neuropsychological assessments were administered at the four previously specified time points. Corresponding to the imaging data, we were interested in behavioral changes between pre-therapy to post-therapy. The following standard behavioral measures were evaluated each time: Action Research Arm Test (ARAT) [9, 14], the 9-Hole Peg Test (9-HPT) [15], Barthel Index [18], and Stroke Impact Scale (SIS) [16, 17]. Scores for the 9-HPT were calculated using the mean of two attempts with the impaired hand. ARAT scores reflect a total score assigned for the subject’s impaired hand. The SIS scores encompass multiple aspects of which we take into account the following standard domains: Activities of Daily Living, Hand Function, Mobility and Strength. In accordance with standard SIS scoring practice, SIS domain scores were transformed to yield a percentage of possible points obtained that have been used for the analysis here.
2.6 Data Preprocessing
Rs-fMRI data were preprocessed using Analysis of Functional NeuroImages [20] and FMRIB Software Library [21]. The preprocessing steps included: removing the first three volumes of each scan, images despiking, slice time correction, alignment with anatomical scan, spatial smoothing with a 4-mm FWHM (full width at half maximum) Gaussian kernel, transformation into TLRC space (3.5 mm isotropic), motion censoring (per TR motion > 1 mm or 1°), nuisance regression, bandpass filtering (0.009–0.08 Hz). We did not perform global signal regression. Additionally, motion within each volume was computed, and volumes with motion > 1 mm were censored.
2.7 Functional Connectivity in the Regions of Interest
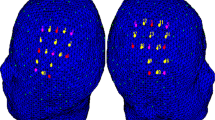
Seed regions within the motor network were based on prior findings that have looked at resting-state connectivity in stroke population [4, 8]. The areas identified were based on a network of cortical and subcortical areas activated during visually paced hand movements. The regions of interest (ROIs) of this network include the primary motor cortex (M1), supplementary motor area (SMA), thalamus and lateral premotor cortex (PMC) in the right and left hemispheres visualized in Fig. 3, [12] and are abbreviated as per Table 2. The MNI coordinates for the 8 ROIs were used to create 8-mm spherical seed ROIs for this study. For each subject, time series from the 8 ROIs were extracted from the spatially standardized residuals for the resting EPI data. The motor mask constituting the 8 ROIS was then used to extract the time series for each region, and an 8 × 8 ROI correlation matrix was computed for each subject. The computed correlation coefficients were standardized to their z-scores. The change in FC from time-point before BCI therapy to time-point after BCI therapy were used as input features for the machine learning regression model.
Motor network with seed regions used in analysis [8]
2.8 Clinical Data
Often times, factors such as age and gender can impact the changes in behavior over time and need to be taken into account. Thus, in the regression model for this work, we consider the following clinical variables: age, gender, side of affected arm, NIH Stroke Scale (NIHSS), time since last stroke (TSS) and pre-stroke handedness score (pre-hand). These clinical factors were evaluated separately, as well as combined with FC features, in order to predict change in behavioral measures.
2.9 Data Analysis
We model this data by fitting a machine learning based regression model to FC and clinical data in order to predict behavioral measures. In particular, supervised learning support vector machines (SVM) [19] are employed. Typically used as a classifier, SVM can also be used for regression analysis [22] and is known as Support Vector Regression (SVR). SVR forms a non-parametric method by implementing the kernel trick. The principle behind the using SVR analysis is described below:
Consider pair of multiple data points, \( \left\{ {\left( {x_{1} ,y_{1} } \right), \ldots \left( {x_{l} ,y_{l} } \right)} \right\} \subset {\rm X}\, \times \,{\mathbb{R}} \), \( {\rm X} \) being the input space. While the \( x_{i} s \) represent the input features, the \( y_{i} s \) represent the outcome variable. Here, the \( x_{i} s \) are the FC values or the clinical data corresponding to each subject and \( y_{i} s \) stand for the behavioral outcomes such as 9-HPT, ARAT, BI, SIS measures. The goal, then, is to find a non-linear function that fits the \( x_{i} s \) such that the estimated value of \( y_{i} s \) within a specified small margin of error from the true \( y_{i} s \). If \( f \) is the estimated function, we have:
where, \( w \in X \), and \( b \in {\mathbb{R}} \), \( { \lessdot } ,{ \gtrdot } \) denotes the dot product in \( X \).
Ensuring that \( w \) turns out to be small ensures that the estimated \( y_{i} s \) will deviate from true \( y_{i} s \) within a small margin. This problem can be rewritten in the form of a convex optimization as follows:
where, \( \varepsilon \) is the small allowable margin of error between true \( y_{i} \) and estimated \( y_{i} \).
The above can be reformulated again to cope with possible infeasible constraints that may arise in the optimization problem by incorporating slack variables. This is analogous to the concept of “soft margin” in SVM classifiers that allow for marginally higher error to get a more superior performance overall. The reformulation, then, becomes:
where, \( C > 0 \) is a constant that determines the extent to which error more than \( \varepsilon \) are allowed. The given method for regression can be applied to the linear case where a linear estimate between input and output values is predicted. With the use of SVM, a kernel method [23] can be applied which can predict non-linear relationships between the input and the output variables, thus, giving a better fit to the data. We implemented the SVR using a Gaussian radial basis function for a kernel given by:
where, \( ||x_{i} - x_{j} ||^{2} \) is the squared Euclidean distance between two input feature points and \( \sigma \) is a free parameter. The kernel transforms the input feature dataset into a higher dimensional feature space where a linear separation may exist.
A leave-one-out-cross-validation (LOOCV) was used to predict the outcome variable since it is a method that gives the most unbiased estimate of test error [25]. In a LOOCV approach, the same dataset can be used for both the training and testing phases. During each fold of LOOCV, a data point is left out and training is performed on the remaining data points. The left out data point is used as a testing point to predict the outcome corresponding to it and evaluate the error measure of prediction. Each data point is left out only once, and so, the number of folds is equal to the number of data points in the sample. We assessed the performance of the SVR using the root mean squared error given by the following equation:
where, \( y_{{est_{i} }} \; - \;y_{i} \) term is the measure of error between the estimated outcome and the true outcome. A good SVR should have low values of RMSE.
Three cases of SVR were implemented, namely: (a) change in FC from pre-intervention to post-intervention as the input features to predict behavioral outcomes, (b) clinical variables as input variables to predict behavioral outcomes, (c) change in FC and clinical variables together as input variables to predict behavioral outcomes. The SVR generates a weighting system to rank the various input features in the order of their importance in predicting the outcome variables. We implemented SVR on MATLAB (R2015b; MathWorks, Natick, MA, USA) with the help of The Spider Machine Learning Toolbox library for SVR [24].
3 Results
We present the results of using a non-linear SVR with a Gaussian kernel by the following cases: The prediction of changes in behavioral outcomes from pre-intervention to post-intervention was performed using (a) changes in FC only (b) clinical variables only and (c) changes in FC and clinical variables combined. Among the top 10 ranked predictors, a greater number of inter-hemispheric FC changes were observed compared to intra-hemispheric FC changes for almost all the behavioral measures in cases (a) and (c). Also in both these instances, while intra-hemispheric FC change between left M1 and left PMC was ranked within top 10 predictors, inter-hemispheric FC change between left M1 and right M1 was ranked within top 5 predictors corresponding to changes across all behavioral measures. Age emerged as the top ranked clinical variable associated with changes in all the behavioral outcomes in (b) as expected. In (c), however, age predicted changes particularly in ARAT for affected side, BI, SIS for strength of affected side and SIS for mobility. Although the difference is small, reduced RMSE values were observed in case (c), thus, suggesting that combining FC changes with clinical variables might form a better predictive model as compared to cases (a) and (b) with a larger sample size. Detailed list of top 10 ranked predictors by the SVR weights can be found in Tables 3, 4 and 5 below. The behavioral outcomes are listed by the following shorthand: 9HPT (A) for 9-HPT of affected side, 9HPT (U) for 9-HPT of unaffected side, ARAT (A) for ARAT of affected side, ARAT(U) for ARAT of unaffected side, SIS (Str) for Strength, SIS (ADL) for Activities of Daily Living, SIS (Mob) for Mobility and SIS (Hand) for Hand Function.
Each SVR is evaluated using RMSE for assessment of quality of prediction. Lower RMSE values represent better performance. The RMSE for the three SVRs are presented by case in Table 6 below. RMSE_FC, RMSE_Clinical, RMSE_FC+Clinical are used as shorthand to denote the three cases of SVR respectively.
4 Conclusion
4.1 Summary
Changes in functional connectivity and clinical measures, together, can predict behavioral changes in subjects undergoing BCI-aided rehabilitation for stroke recovery and machine learning can help rank the predictors of change in behavior. Notably, it was demonstrated that inter-hemispheric changes in FC in the motor network are more significant than intra-hemispheric changes in driving the prediction for most of the behavioral scales included in the neuropsychological battery. Among the clinical variables, age appeared to be a significant factor in assessing changes in behavioral outcomes.
4.2 Discussion and Future Scope
This study highlights that machine learning based statistical tools such as the SVR can provide information correlating neuroimaging changes to behavioral changes, although it can be limited by the sample size used in the analysis. Additionally, the heterogeneity of the cohort in terms of their lesion location, lesion volume and affected side due to stroke may influence the result of the predictive model. A left hemispheric dominance was observed among the top weighted features predicting behavioral measures. This could potentially arise due to most subjects being right-handed prior to occurrence of the stroke and would require inclusion of comparable number of left-handed subjects in the sample in order to further analyze the effect of handedness. Furthermore, we have not taken into consideration, the relationship between the multiple behavioral outcomes in this work. Also, the direction of change in behavioral measurements has not been considered. In particular, future work could assess the relationship between behavioral gains and functional connectivity changes. The complete BCI-aided intervention involved collection of imaging as well as behavioral data at four different time points, of which the pre- and post-intervention data have been used in the current analysis. The analysis, here, uses only two of the four time-points and could be expanded further by considering the changes in FC over all the four time points and correlating it to behavioral changes. This current approach, however, provides a basic framework for future work to build a larger predictive model that incorporates data from additional predictors in the form of other imaging modalities such as diffusion tensor imaging (DTI), task-based fMRI, lesion maps, implements a multiple-output SVR to control for possible correlations between outcome variables and utilizes a larger sample size.
References
Bajaj, S., Butler, A.J., Drake, D., Dhamala, M.: Functional organization and restoration of the brain motor-execution network after stroke and rehabilitation. Front. Hum. Neurosci. 9(173), 1–14 (2015)
Carter, A.R., Astafiev, S.V., Lang, C.E., Connor, L.T., Rengachary, J., Strube, M.J., Pope, D.L.W., Shulman, G.L., Corbetta, M.: Resting inter-hemispheric fMRI connectivity predicts performance after stroke. Ann. Neurol. 67(3), 365–375 (2010)
Felton, E.A., Radwin, R.G., Wilson, J.A., Williams, J.C.: Evaluation of a modified Fitts law brain-computer interface. J. Neural Eng. 6, 1–7 (2009)
Grefkes, C., Eickhoff, S.B., Nowak, D.A., Dafotakis, M., Fink, G.R.: Dynamic intra- and interhemispheric interactions during unilateral and bilateral hand movements assessed with fMRI and DCM. NeuroImage 41(4), 1382–1394 (2008)
Lee, M.H., Smyser, C.D., Shimony, J.S.: Resting state fMRI: a review of methods and clinical applications. AJNR Am. J. Neuroradiol. 34(10), 1866–1872 (2013)
Kwakkel, G., Kollen, B.J., van der Grond, J., Prevo, A.J.H.: Probability of regaining dexterity in the flaccid upper limb: impact of severity of paresis and time since onset in acute stroke. Stroke 34(9), 2181–2186 (2003)
Mozaffarian, D., Benjamin, E.J., Go, A.S., Arnett, D.K., Blaha, M.J., Cushman, M., et al.: Execute summary: heart disease and stroke statistics – 2016 update: a report from the American heart association. Circulation 133(4), 447–454 (2016)
Nair, V.A., Young, B.M., Nigogosyan, Z., Remsick, A., Weber, S., Diffee, K., Walton, L., Tyler, M., Sattin, J., Edwards, D.F., Williams, J., Prabhakaran, V.: Abstract 6: resting-state functional connectivity changes after stroke rehabilitation using closed loop neurofeedback. Stroke 4, A6 (2015)
Carroll, D.: A quantitative test of upper extremity function. J. Chronic Dis. 18, 479–491 (1965). doi:10.1016/0021-9681(65)90030-5
Soekadar, S.R., Birbaumer, N., Slutzky, M.W., Cohen, L.G.: Brain-machine interfaces in neurorehabilitation of stroke. Neurobiol. Dis. 83, 172–179 (2015)
Varkuti, B., Guan, C., Pan, Y., Phua, K.S., Ang, K.K., Kuah, C.W.K., Chua, K., Ang, B.T., Birbaumer, N., Sitaram, R.: Resting state changes in functional connectivity correlate with movement recovery for BCI and robot-assisted upper-extremity training after stroke. Neurorehabil. Neural Repair 27(1), 53–62 (2013)
Xia, M., Wang, J., He, Y.: BrainNet Viewer: a network visualization tool for human brain connectomics. PLoS ONE 8(7), e68910 (2013)
Young, B.M., Nigogosyan, Z., Walton, L.M., Song, J., Nair, V.A., Grogan, S.W., Tyler, M.E., Edwards, D.F., Caldera, K., Sattin, J.A., Williams, J.C., Prabhakaran, V.: Changes in functional brain organization and behavioral correlations after rehabilitative therapy using a brain-computer interface. Front. Neuroeng. 7(26), 1–15 (2014)
Lang, C.E., Wagner, J.M., Dromerick, A.W., Edwards, D.F.: Measurement of upper-extremity function early after stroke: properties of the action research arm test. Arch. Phys. Med. Rehabil. 87, 1605–1610 (2006). doi:10.1016/j.apmr.2006.09.003
Beebe, J.A., Lang, C.E.: Relationships and responsiveness of six upper extremity function tests during the first six months of recovery after stroke. J. Neurol. Phys. Ther. 33, 96–103 (2009). doi:10.1097/NPT.0b013e3181a33638
Duncan, P.W., Wallace, D., Lai, S.M., Johnson, D., Embretson, S., Laster, L.J.: The stroke impact scale version 2.0. Evaluation of reliability, validity and sensitivity to change. Stroke 30, 2131–2140 (1999). doi:10.1161/01.str.30.10.2131
Carod-Artal, F.J., Coral, L.F., Trizotto, D.S., Moreira, C.M.: The stroke impact scale 3.0: evaluation of acceptability, reliability and validity of the Brazilian version. Stroke 39, 2477–2484 (2008). doi:10.1161/STROKEAHA.107.513671
Mahoney, F.I., Barthel, D.: Functional evaluation: the Barthel Index. Maryland State Med J. 14, 56–61 (1965)
Scholkopf, B., Smola, A.J.: Learning with Kernels: Support Vector Machines, Regularization, Optimization, and Beyond. MIT Press, Cambridge, (2001)
Vapnik, V.: The Nature of Statistical Learning Theory. Springer, New York (1995)
Schölkopf, B., Smola, A.J.: Learning with Kernels: Support Vector Machines, Regularization, Optimization and Beyond, p. 633. MIT Press, Cambridge (2002)
Weston J., Elisseeff A., Bakir G., Sinz F.: The Spider Machine Learning Toolbox. Resource object oriented environment. http://people.kyb.tuebingen.mpg.de/spider/main.html
Hastie, T., Tibshirani, R., Friedman, J.H.: The Elements of Statistical Learning: Data Mining, Inference, and Prediction. Springer Publishing Company Inc., New York (2001). pp. 193–224
Acknowledgments
The authors would like to thank all the subjects and their families for their participation in the stroke rehabilitation program. Thanks to the study coordinator Theresa Jungae Kang and the MRI technicians Sara John and Jenelle Fuller at the Wisconsin Institutes for Medical Research. This study was supported by NIH grants RC1MH090912-01, K23NS086852, T32GM008692, UL1TR000427, T32EB011434 and TL1TR000429. Additional funding was also provided through a Coulter Translational Research Award, an American Heart Association Postdoctoral Fellow Research Award, AHA Midwest Grant-in-Aid Award, AHA National Innovation Award, UW Milwaukee-Madison Intercampus Grants, UW Graduate School, Grants from Shapiro Foundation and Foundation of ASNR award.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this paper
Cite this paper
Mohanty, R. et al. (2017). Machine Learning-Based Prediction of Changes in Behavioral Outcomes Using Functional Connectivity and Clinical Measures in Brain-Computer Interface Stroke Rehabilitation. In: Schmorrow, D., Fidopiastis, C. (eds) Augmented Cognition. Neurocognition and Machine Learning. AC 2017. Lecture Notes in Computer Science(), vol 10284. Springer, Cham. https://doi.org/10.1007/978-3-319-58628-1_41
Download citation
DOI: https://doi.org/10.1007/978-3-319-58628-1_41
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-58627-4
Online ISBN: 978-3-319-58628-1
eBook Packages: Computer ScienceComputer Science (R0)