Abstract
Arteriovenous hemodialysis catheters have lower rates of primary and secondary patency than autologous arteriovenous fistulas in most patients. While emphasis has been placed on de novo construction of arteriovenous fistulae, grafts are still placed for primary access in a large population of end-stage renal disease placements. Unfortunately, once these grafts fail, patients are often left with no peripheral hemodialysis access and require central venous catheter placement. Construction of secondary arteriovenous fistulae prior to graft failure obviates the need for this period of hemodialysis catheter placement.
Similar content being viewed by others
Keywords
Case Presentation
A 65-year-old male has been dialyzed for 4 years via a left forearm looped brachiobasilic arteriovenous (AV ) polytetrafluoroethylene graft. At the time of access creation, his basilic, median antebrachial, and cephalic veins in his forearm and upper arm were not suitable for construction of a primary AV fistula. Over the past few months, he has had difficulty achieving adequate dialysis flow rates during his Monday/Wednesday/Friday sessions. On exam, he is noted to have a pulse in his graft. He was referred to an interventional nephrologist who performed an angiogram demonstrating a venous anastomotic stenosis of greater than 50% of the luminal diameter (see Fig. 1.1). There was no upper arm or central venous stenosis present. An angioplasty was performed, and the patient was dialyzed for another 2 months until the graft thrombosed. Despite attempts to reestablish flow, the thrombosis could not be corrected. A right-sided internal jugular hemodialysis catheter was placed. The patient was subsequently referred to a local vascular surgeon for reconstruction of peripheral access. Approximately 4 months later, a contralateral brachiocephalic AV fistula was constructed. The catheter was removed 2 months later, once the fistula matured. In the interim, he was hospitalized once with a methicillin-resistant Staphylococcus aureus bloodstream infection. The line was removed and replaced on the contralateral side. He was treated with vancomycin immediately after his hemodialysis sessions for 4 weeks.
Discussion
Unfortunately, as in the case above, AV graft failure is all too frequent, requiring subsequent catheter placementa. The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (K/DOQI) clinical practice guidelines prioritize the construction of autogenous AV fistulae in a distal-to-proximal fashion, always considering the preservation of more proximal surgical sites for future access construction. This emphasis is based on fistula’s inherent higher primary and secondary patency rates and, with that, a lower need for interventions and, in select groups, longer patient survival. The K/DOQI guidelines, along with the “Fistula First Catheter Last” (FFCL) Coalition , seem to have changed practice patterns in the United States [1]. From 1996 to 2007, autogenous fistula access use in the United States increased from 24% to 47%, while prosthetic graft use decreased from 58% to 28%. Still, however, 53% of patients are dialyzed via a central venous catheter or AV graft. To contextualize, in Japan, according to the collaborative international Dialysis Outcomes and Practice Patterns Study, this number is only 9% [2].
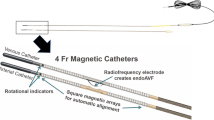
In most cases, as in the case above, AV graft failure is followed by a period of catheter placement prior to construction of new access. This cycle often repeats itself leading to unnecessary catheter days and high risks of central line-associated bloodstream infections. To avoid this, the FFCL has advocated for proactive construction of new AV fistulas prior to graft failures, so-called secondary AV fistulas (sAVF ). The FFCL recommends nephrologists evaluate every AV graft patient for possible sAVF conversion [3, 4] and has put forth a convenient “Sleeves Up Protocol ” to assist with this. The evaluation, which occurs briefly at bedside immediately prior to or after a dialysis session, helps identify suitable outflow vein for immediate conversion to an AVF. Every month, a practitioner should roll the patient’s “sleeves up” exposing the entire arm up to the shoulder. Then, the upper arm should be lightly compressed to assess the caliber and prominence of the graft’s venous outflow. If the primary outflow vein appears suitable for access, it should be cannulated with the venous dialysis access needle for two consecutive hemodialysis sessions. If there are no issues, a fistulogram or duplex ultrasound of the arm should be performed to confirm the vein’s suitability and ensure patent venous drainage back to the right atrium. Assuming both of these tests go well, a prompt sAVF conversion plan should be made (see Fig. 1.1).
While AV grafts may spontaneously stop working, graft dysfunction is often predictable. Indicators of venous outflow stenosis include strong pulsatility and shortening or even absence of the diastolic phase of the thrill on exam. In severely obstructed grafts, there may be only a high-pitched thrill during systolic phase. Indicators of outflow problems on dialysis may include low flow rates, high venous pressures, or increased recirculation. There may be persistent post-dialysis bleeding. Other predictors of graft failure include requiring multiple interventions to maintain patency. Cumulative patency at 12 months of angioplastied grafts is around 30–50%, whereas it is only around 10–20% in thrombectomized grafts. Unfortunately, recent studies have shown no benefit to prophylactic treatment of graft stenosis detected on routine angiography. Thus, a preemptive sAVF conversion plan should be considered in patients with graft dysfunction requiring endovascular therapy. Similarly, as AV grafts have a greater rate of infection than autologous fistulae, sAVF is an attractive option to preserve access in patients requiring graft excision from recurrent infections. All of this forms the basis for the FFCL ’s recommendation that evaluation for sAVF conversion takes place no later than the first signs of AV graft failure. Meanwhile, the impetus is on the surgeon to perform the operation prior to a second intervention for graft stenosis or thrombosis. As such, the prudent surgeon should plan for sAVF conversion while placing an AV graft in a patient with initially unsuitable venous targets (see Fig. 1.2). In fact, in these cases, if a patient is being dialyzed via a catheter, an AV graft can be placed as a bridge to sAVF. Here, an immediate-access graft conduit (e.g., Flixene) is used to allow prompt removal of the catheter. Months later, once the outflow becomes suitable, the graft can be excised and a sAVF constructed.
The classic sAVF, constructed using the main outflow vein from a graft, is termed a Type 1 sAVF. These fistulae can be constructed using below- or above-the-elbow veins following placement of a forearm AV graft. Duplex sonography and contrast venography are essential to both identify outflow veins of sufficient caliber and rule out central venous stenosis. Approximately 75% of patients with forearm AV grafts have vascular anatomy suitable for construction of a Type 1 sAVF (see Fig. 1.3). In the simplest scenarios, the sAVF can be made using arterialized basilic, cephalic, or brachial vein just distal to the previous venous anastomosis. Arterial inflow is typically provided by the brachial or proximal radial artery. Intraoperatively, the AVG is ligated and the outflow vein is mobilized and used for an anastomosis. To gain additional length, venous tributaries flowing into the suitable vein can be mobilized and used for an anastomosis. Frequently, after construction, Type 1 sAVFs are immediately available for dialysis access. A basilic or brachial vein can be transposed to a superficial position at the same time or as a staged approach. Even despite complete graft thrombosis, primary draining veins are often kept patent by tributaries, and a fistula can be constructed (see Fig. 1.4). In these settings, timely Type 1 sAVF construction can avert the need for catheter placement where it would otherwise be necessary.
Angiogram of upper arm veins draining a forearm loop graft : (a) basilic vein and (b) cephalic vein (c) venous anastomosis with lower arm AV graft (Reprinted with permission from Beathard [5])
Appearance of the left arm cephalic vein receiving drainage from a clotted forearm AV graft. The cephalic vein is indicated by the arrow. (a) Appearance when the graft is clotted with no flow or pressure. (b) Same vein with flow and pressure after graft was opened (Reprinted with permission from Beathard [5])
In cases where the AV graft outflow is not amenable to Type 1 sAVF creation, vein mapping of the ipsilateral arm should be performed with the goal of finding other veins suitable for fistula creation. More frequently, these are patients with upper arm AV grafts, where only a small segment of primary outflow vein exists distally to the axilla. It remains important to still ensure that there is no central venous stenosis. As for termed Type 2 sAVFs, these are not dissimilar from standard primary AV fistulae and must be promptly constructed. The ipsilateral proximal radial artery will often have adequate inflow in an untouched surgical field. Venous targets may be more difficult to find however. Other than the median antebrachial or cephalic veins, in the setting of more proximal obstruction, forearm veins may be used in a retrograde fashion once valves are obliterated. Perforating veins may also be used. Overall, proximal radial artery fistulas have low rates of steal with excellent 2-year secondary patency rates. If however there are no inflow or outflow options on the ipsilateral arm, the contralateral arm must be interrogated for de novo fistula creation. Unfortunately, whereas a failing AV graft will hopefully last long enough to allow for maturation, a failed AV graft will require interim dialysis catheter placement. Therefore, early recognition of graft dysfunction and construction of autologous access are a priority.
Pearls
-
New autogenous access sites should be considered prior to AV graft failure to avert the need for hemodialysis catheter placement.
-
Primary dialysis providers can evaluate patients for suitability for referral for secondary AV fistula formation quickly, during hemodialysis sessions.
-
Secondary AV fistulas can frequently be constructed using the primary outflow of an AV graft, allowing immediate use for hemodialysis.
Abbreviations
- AV:
-
Arteriovenous
- FFCL:
-
“Fistula First Catheter Last” Coalition
- K/DOQI:
-
Kidney Disease Outcomes Quality Initiative
- sAVF:
-
Secondary arteriovenous fistula
References
Park HS, et al. Comparison of outcomes with Arteriovenous fistula and arteriovenous graft for vascular access in hemodialysis: a prospective cohort Study. Am J Nephrol. 2016;43(2):120–8.
Becker B, Mitch W, Blake P, Obrador G, Collins A, Parekh R et al. NKF KDOQI Guidelines. http://www2.kidney.org/professionals/KDOQI/guideline_upHD_PD_VA/. Accessed 13 Apr 2016.
Ethier J, Mendelssohn DC, Elder SJ, Hasegawa T, Akizawa T, Akiba T, et al. Vascular access use and outcomes: an international perspective from the dialysis outcomes and practice patterns Study. Nephrol Dial Transplant. 2008;23(10):3219–26.
ESRD NCC. Secondary AVF placement in patients with AV grafts. http://esrdncc.org/ffcl/change-concepts/change-concept-6/. Accessed 13 Apr 2016.
Beathard GA. Interventionalist’s role in identifying candidates for secondary fistulas. Semin Dial. 2004;17(3):233–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Grodstein, E.I., Redfield, R.R. (2017). Arteriovenous Graft-Arteriovenous Fistula Conversion (Secondary Arteriovenous Fistula Creation). In: Yevzlin, A., Asif , A., Redfield III, R., Beathard, G. (eds) Dialysis Access Cases. Springer, Cham. https://doi.org/10.1007/978-3-319-57500-1_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-57500-1_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-57498-1
Online ISBN: 978-3-319-57500-1
eBook Packages: MedicineMedicine (R0)