Abstract
Food safety is a concern worldwide and according to the World Health Organization, developing countries are probably more at risk of foodborne illness because many of these, including those in the Middle East, have limited disease surveillance and prevention and control strategies. Specifically, the Middle East and North Africa (MENA) region has the third highest estimated burden of foodborne diseases per population, after the African and South-East Asia regions. However, it is difficult to determine what the burden is since little is published in peer-reviewed journals or government reports for public access. This chapter reviews 16 autonomous nations, namely, Afghanistan, Bahrain, Egypt, Iran, Iraq, Israel, Palestine, Kuwait, Lebanon, Oman, Pakistan, Qatar, Saudi Arabia (KSA), Syrian Arab Republic (Syria), United Arab Emirates (UAE) and Yemen. Countries range in size from Bahrain with 1.8 million inhabitants to Pakistan with a population of 184 million. Agriculture and local food production is much influenced by water availability for irrigation. Water shortages are most severe in the Gulf countries which rely on aquifers, desalination, and recycled waste water for most of their water supplies. This means that most food is imported which is expensive if not subsidized through petrodollars. This impacts food security which is a particular concern in countries under conflict, particularly, Syria, Yemen and Iraq. Gastrointestinal infections are frequent in this region from Salmonella Typhi and other Salmonella spp., Shigella spp., Campylobacter jejuni and C. coli, rotavirus, hepatitis A virus, parasites, and more rarely from Aeromonas, Yersinia enterocolitica, Brucella spp., and Middle East Respiratory Syndrome coronavirus (MERS-CoV). Reports indicate that children are the most susceptible and that many isolates are multidrug resistant. Chemical contamination of water supplies and crops are probably more of a concern than published reports indicate, because of widespread indiscriminate use of fertilizers, antibiotics, and pesticides, coupled with increased industrial pollution affecting the water supplies. Like many other parts of the developing world, foodborne disease surveillance is limited and outbreaks are most often reported through the Press but with insufficient detail to determine the etiological agents and the factors contributing to the outbreaks, leading to speculation to the cause by those interested or responsible for food prevention and control. However, there are some well investigated outbreaks in the region that have those details, and reveal where the shortcomings of both the establishments and the inspection systems have been. Where the causative agents are known, the kinds of pathogens are generally similar to those found in the West, e.g., Salmonella, but many outbreaks seem to have short incubation periods that point to a toxin of some kind of chemical or biological origin, but these are almost never identified. Because of sectarian warfare, residents and refugees have been given food that has made them sick and solders? have been deliberately poisoned. Research has been focused on microbial contamination of locally-sold foodstuffs and manager and employee knowledge of food safety and hygienic conditions in food preparation establishments. An innovative pilot project in Qatar is to use seawater and sunlight for raising crops through the Sahara Forest Project. All countries have some kind of food establishment inspection system, but they tend to be punitive if faults are found in management or employees on the premises rather than being used for their education for improving food safety. Restaurants may be closed down and owners and employees fined for often unspecified infringements. However, some food control agents are moving towards employee training through seminars and courses before problems occur, which is a good disease prevention strategy. Unfortunately, many of the food handlers are from Asian countries with languages other than Arabic and English, which makes effective food safety communication and training difficult. Tourists visiting popular resorts in Turkey and Egypt have suffered from foodborne illnesses, usually of unknown origin but poor hygienic conditions are blamed with law suits following, and the adverse publicity affects the long-term viability of some of these resorts. Food exports, important for local economies, have occasionally been contaminated resulting in recalls and sometimes illnesses and deaths, notably fenugreek seeds from Egypt (E. coli O104:H4), pomegranate arils from Turkey (hepatitis A virus), and tahini from Lebanon (Salmonella). Overall, in recent decades, the Middle East has made strides towards improving food safety for both residents and foreign visitors or ex-pat workers. However, within the countries there are large discrepancies in the extent of effective public health oversight including food safety and food security. Currently, almost all of the countries are involved to a greater or lesser extent in the civil wars in Syria and Yemen, or are affected through political tensions and strife in Egypt, Iraq, Iran, Israel, Palestine, Lebanon and Turkey. In addition, the current overproduction of oil on a world-wide scale has led to a rapid decrease in revenues to most Gulf states. All this points to a severe setback, and an uncertain foreseeable future for improvements in obtaining both sufficient and safe food for residents in this region.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
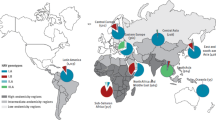
The World Health Organization (WHO) Eastern Mediterranean region, comprising countries in the Middle East and North Africa (MENA), has the third highest estimated burden of foodborne diseases per population, after the African and South-East Asia regions. According to the WHO ( 2015a), more than 100 million people living in this region are estimated to become ill with a foodborne disease every year and 32 million of those affected are children under 5 years. Diarrheal diseases caused by E. coli, norovirus, Campylobacter and nontyphoidal Salmonella account for 70% of the burden of foodborne disease. An estimated 3000 people die each year from unsafe food, caused primarily by diarrheal diseases, typhoid fever, hepatitis A, and brucellosis. Both typhoid fever and hepatitis A are contracted from food contaminated by the feces of an infected person and the source of brucellosis is typically unpasteurized milk or cheese from infected goats or sheep. Half of the global cases of brucellosis are in people living in this region, with more than 195,000 people infected every year, causing fever, muscle pain or more severe arthritis, chronic fatigue, neurologic symptoms and depression. Cholera, which after a short incubation period of 2–5 days causing severe diarrhea and dehydration, is returning to those countries with limited public health infrastructure caused by conflict, such as Iraq (Agence France-Presse 2015).
The list of countries covered by this chapter is similar to that of WHO but leaving out North African countries except Egypt (which has territory in eastern Asia) and adding Turkey which is not always considered in the region because it is not Arabic, but has interesting food safety data. Therefore, the countries under review are Afghanistan, Bahrain, Egypt, Iran, Iraq, Israel and Palestine, Kuwait, Lebanon, Oman, Pakistan, Qatar, Saudi Arabia (KSA), Syrian Arab Republic (Syria), United Arab Emirates (UAE) and Yemen. Gulf countries Bahrain, Kuwait, Oman, Qatar, KSA and the UAE have similar social, political, economic, culture, religion, language and ancestry with several similarities in their food control systems and food safety programs (Al-Kandari and Jukes 2009).
A Food and Agriculture Organization (FAO) report covering international investments in agriculture in the Near East (not identical to the countries chosen for this chapter, but many of the findings apply) states that this region is characterized by a mix of very different countries’ resources and incomes (Tanyeri-Abur and Elamin 2011). The wealth in the richer countries of the region is primarily dependent on oil revenues and the past economic growth has been closely linked to the oil market; about 43% of regional Gross Domestic Product (GDP) is concentrated in the high income countries (Qatar, Kuwait, UAE, Saudi Arabia, and Bahrain) which are home to only11.8% of the population in the region, and many of these are expatriates working in these countries. The report indicates that food insecurity varies sharply in the region but overall the percent of the undernourished population does not exceed 57% in most countries of the region, except for Sudan, Mauritania, Djibouti and Yemen where the proportion of undernourished exceeds 25%; however, in 2016 these percentages will be totally out of date for countries like Syria and Iraq and in neighboring countries where refugees have reached because civil war and jihadi terrorist groups have put considerable stress on public health facilities and food availability. The countries in the region however, are largely similar when it comes to the challenges in achieving sustainable agriculture and food security. For most of these countries, the overwhelming concern is to secure adequate and stable supplies of food at the national level, making food security a concern for both rich and poor countries of the region (Tanyeri-Abur and Elamin 2011). The three major problems affecting most of the countries are (i) limited water availability; (ii) population growth; and (iii) heavy dependence on food imports. Water scarcity in particular, is the most critical development problem in the region and the single most important factor in limiting agricultural growth, and water availability has been declining steadily since the late 1950s. The region as a whole has 70% less availability of renewable water per person in 2003–2007 than in 1958–1962. Lack of water for irrigating crops but also for potable water supplies affects many of the countries, particularly in the Gulf region. It is important to note that the wealthiest countries are also those with the highest water depletion record, namely, the UAE and Qatar. The unprecedented growth in investment in agriculture is in large part a result of the food crisis of 2007, which brought about a rethinking of agricultural support policies, mostly in countries of the Gulf and particularly Saudi Arabia, which has invested heavily in the last 30 years in large-scale agricultural production using up valuable water resources. Saudi Arabia announced in January 2008 that it would phase out wheat and agricultural production in the course of the next 8 years. In July 2008, Qatar and UAE took similar policy decisions (Tanyeri-Abur and Elamin 2011).
Crops grown in the region may serve as fresh food sources for the population, but much of the food is imported with limited locally processed products, and if the policies of KSA, Qatar and UAE expand to other countries, more will be imported in the future (Tanyeri-Abur and Elamin 2011). Thus, the main foodborne disease issues are with homemade, restaurant and street food, where isolated claims of illness are followed up by inspections and possible punitive action by public health agencies responsible for food safety. Those countries that rely on tourism for their main source of GDP have sometimes been damaged by adverse publicity, e.g., Egypt, and to a lesser extent, Turkey and Lebanon. According to the Food and Agriculture Organization, less than 4% of the world agricultural trade is conducted in the region. Even though by tradition many of these countries relied on growing their own food, today some of these countries import almost 90% of their food; 2.3% of the food in the world alone was imported to Saudi Arabia and United Arab Emirates in 2007, and the food trade balance in food in Middle East is negative, estimated at over 50 US $ billion dollars (Tajkarimi et al. 2013). There are specific restrictions prevalent in the Arab-speaking countries related to Islam and Judaism with the prohibition of eating pork and blood, the drinking of alcohol, and mixing dairy foods and meat under Halal and Kosher food laws. Therefore, parasites related to pigs, e.g., Trichinella and Taenia spp., are unlikely to be prevalent in these populations. However, there are many Muslim and Jewish feast occasions with large gatherings such as Eid linked to Ramadan and particularly the Muslim Hajj, which put a strain on food preparation, distribution and storage. Good health conditions for travelers to Saudi Arabia for the pilgrimage to Mecca (Hajj) are critical and any incident that occurs has to be quickly contained to prevent extensive infectious disease outbreaks (Memish and Al Rabeeah 2011).
Traditional Middle Eastern foods are mainly related to legumes, leafy greens, fruit, dairy products and meat on special occasions; details can be found in Brittin (2010). In urban areas today, grocery stores and supermarkets can supply most of the food requirements of a family but imported foods tend to be expensive. Also, some fruit and vegetable items are seasonal and are only available once or twice a year such as local plums, almonds and bananas, which tend to be cheaper than imported varieties. Quality of raw produce in stores varies but they often have short shelf lives and can spoil quickly because of harvesting ripe products, bruising, and high storage temperatures. Traditional rural foods include aromatic stews, stuffed vegetables, wild leaves, pulses and cracked wheat, and occasional goat or lamb meat. A typical Middle Eastern meal starts with a variety of cold and hot mezze (appetizers), salads and pastries, especially in Greece, Turkey and Lebanon. Many contain herbs, cheese, pickles, nuts, seeds, and parsley and lettuce are widely eaten in salads or traditional mezzes. Most mezzes are vegetarian and fresh fruits and vegetables are an integral and important part of the cuisine when they are in season. Tabbouleh, a salad where parsley is a major ingredient with small pieces of tomato, and some bulgur (ground wheat) in it, is often served in leaves of romaine lettuce or raw cabbage. Almost as popular is fattoush, a mixed bowl of lettuce, tomatoes, cucumbers, and fried or toasted pita chips, typically seasoned with a dusting of sumac and pomegranate molasses. Since leafy greens do not have a final decontamination step, they are at risk from environmental fecal contamination as reported in Lebanon by Faour-Klingbeil et al. (2016). Hummus, a smooth chickpea paste made with tahini/tehineh, lemon juice or citric acid, garlic and salt, and often served with olive oil, is the most ubiquitous mezze. Since tahini and hummus are major exported products from the region, particularly Lebanon, they are prone to Salmonella contamination, and are sometimes recalled from other countries, which is damaging to the local economies. Dairy products are also served regularly at meals and these are locally made or imported. Labneh, strained yogurt, very similar to Greek yogurts, is widely used as a base for mezze which might have olive oil, pine nuts or za’atar (a mixture of thyme, sumac, and sesame seeds) added. Cheeses including the popular haloumi are frequently served in restaurants. Shawarma/shwarma is frozen or refrigerated raw or marinated meat (lamb, beef or chicken) cooked on a vertical rotisserie popular throughout MENA countries and now frequently seen in western nations. Higher fish consumption tends to be close to where these are locally caught, either sea or river netted. One example from Iraq is masquf (split large fish cooked on stakes over a fire, and eaten outdoors by a river, served with slices of tomato and onion and Arab bread. Crustaceans are less frequently eaten but can be obtained from imports. Cosmopolitan foods are widely available in the larger cities, as are multinational fast-food chains.
Foodborne illnesses have been sporadically reported throughout the region over the past decades and global assessments of the kinds of problems encountered reviewed, e.g., Todd (2001) and Al-Mazrou (2004) and more recently by Tajkarimi et al. (2013). These last authors indicate that reporting foodborne disease is functioning well in Jordan, Kuwait, Oman, Saudi Arabia and UAE, compared to other countries in the region. However, the foodborne outbreak surveillance systems in Middle Eastern developing countries are still limited with reporting of less than 1% of the actual outbreaks; one reason is that many foodborne illnesses occur in homes and those ill may not visit medical care facilities. In addition, available laboratory analytical support for public health agencies is often minimal or lacking, even though some research institutions may have up-to-date equipment and technical expertize. Change is gradually coming and a food and drug authority has been established in both Saudi Arabia and Jordan (Al-Kandari and Jukes 2009). Also, new food legislation has been initiated by Egypt, Lebanon and Syria (Tajkarimi et al. 2013), but is currently stalled in last two countries. Improvements in inspection service, hand held computers, customized software and improved surveillance systems are some examples of developments in food safety systems in the region. Jordan, Saudi Arabia and Bahrain have been developing unified food safety activities from farm to fork (Al-Kandari and Jukes 2009). However, there is a need for substantive food safety education for all foodservice staff. Increasing quality and quantity of the food safety training and human resources in governmental agencies in the region will improve the public health infrastructure. For example, the Municipality of Dubai has established an international annual food safety conference to improve the food safety education system of those in the region, now in its 10th year (2016).
The following sections of the chapter focus on five aspects: gastrointestinal infections; foodborne disease outbreaks in specific countries; food safety related research and surveys; issues relating to tourism and exported food; and government oversight of the food industry, with specific examples from countries in the region.
Gastrointestinal Infections
Gastrointestinal diseases are frequently encountered in the Middle East and many etiological agents have been identified where specific studies have been carried out to look for bacterial, viral and parasitic pathogens. The average annual incidence of culture-proven shigellosis in Israel was 97/100,000 from 1998 to 2012, but each reported case was considered to represent 25 cases indicating the high burden of the disease in the country (Cohen et al. 2014). Orthodox Jewish communities, living in highly crowded conditions and with a high number of children aged <5 years were the epicenter of country-wide biennial propagated epidemics of S. sonnei shigellosis. S. flexneri was the leading Shigella serogroup in Israeli Arabs. Isolates showed high rates of resistance to ampicillin and trimethoprim/sulfamethoxazole, but very low rates to quinolones and third-generation cephalosporins. There is no indication if foods or water were vehicles of these shigellosis cases. Also, in Israel a study of pregnancy-related listeriosis cases from 1998 to 2007, identified 166 cases, resulting in a yearly incidence of 5–25 cases per 100,000 births (Elinav et al. 2014). There were 29 fetal deaths, two neonate deaths and one maternal mortality. The incidence of Israeli pregnancy-associated listeriosis has a high yearly variability and is one of the highest worldwide. The geographical distribution varied greatly between years and had a different epidemiological pattern compared with non-pregnancy-related listeriosis. The sources of the infections were not studied but all listeriosis cases have a foodborne link. This has to be further researched as to diet, and the unawareness of the Israeli public of the risk for certain food products contributing to the extremely high incidence in Israel, in both general and pregnancy-associated listeriosis, as occurs in other countries. A total of 132 stool samples were collected from Palestinian patients with acute diarrhea from which 12 (9.1%) yielded enteropathogenic bacteria. Salmonella, Campylobacter coli/jejuni, and Aeromonas hydrophilia were isolated in equal numbers from samples 3/12 (25% each), Shigella boydii 2/12 (16.7%), Yersinia enterocolytica 1/12 (8.3%) (Abdelateef 2011). Many strains were antibiotic-resistant. Children younger than 5 years old were more susceptible to infectious diarrhea; in addition, diarrhea was more frequent in those living in crowded houses, and in houses rearing poultry, including pigeons. Salmonella enterica serovar Typhi continues to be an important public health problem in Kuwait. Analysis of the isolates from 163 patients, collected between 1995 and 2003, showed that the majority were from patients from the Indian sub-continent, and many strains were drug resistant (Dashti et al. 2008). Typhoid fever in Kuwait is predominantly associated with those who have traveled from endemic areas to work in Kuwait.
The circulation of enteric viruses among the population of Cairo, Egypt, between March 2006 and February 2007 was studied by Kamel et al. (2009). At least one type of virus was detected in 50% of fecal samples, 57.4% of which were positive for rotavirus, 26% for norovirus, 10.4% for adenovirus, and 1.7% for astrovirus. Over 10% of infections were mixed infections. Among the noroviruses, half belonged to the predominant GGII.4 cluster which were similar to those circulating elsewhere, but there were also new GGII.4 variants that were not associated with any previously known GGII.4 isolate. Although norovirus is rarely implicated in foodborne outbreaks compared with the US and other western countries, it is clearly present in Egypt. Further studies are required to assess the disease burden of enteric viruses in Egypt and the impact of atypical strains. The disease burden of hepatitis A and E in Egypt is one of the heaviest worldwide, based on serological analysis, with HAV infections occurring very early in life, with almost 100% seropositivity after the first years of life (Kamel et al. 2011). To determine the actual contamination levels in the environment, these authors conducted a survey of HAV and hepatitis E virus (HEV) in sewage in Cairo. HAV was detected by RT-PCR in 11 of 76 (15%) sewage samples. In addition, all the HAV-positive samples were also positive for enteroviruses. That only one stool sample was HEV-positive might be explained by the lower level of excretion of the virus in stools, the fragility of the virion in the environment, and technical difficulties in concentrating and amplifying the virus with standard methods. Bacterial etiology was found in 15.2% of cases of childhood diarrhea in Dhahira, Oman, mostly Shigella sonnei and to a lesser extent Salmonella (Patel et al. 2008). Antibiotics were prescribed in 36.2% of cases and the resistance to the common antibiotics tested was low. One reason for the low pathogen isolation rate could be that many cases had viral etiology. Rotavirus was detected in stool specimens from 1712 (49%) of 3470 children, who were admitted to 11 regional public hospitals in Oman for a median of 3 days with severe diarrhea (Al Awaidy et al. 2009). A diverse rotavirus strain pattern in Oman was identified with G2 (37%), G1 (38%), and G9 (11%) accounting for most of typeable strains. The authors estimated the burden for the Omani government at US$791,817 and US$1.8 million annually to treat rotavirus-associated diarrhea in the outpatient and hospital settings, respectively. They recommended a rotavirus vaccination program that would substantially reduce the burden of severe diarrhea among children in the country.
Unlike the above countries where the health care system functions for most residents, though not always to Western standards, the same cannot be said for Pakistan, particularly in rural areas. Poor nutrition combined with diarrheal and other foodborne diseases puts the population at risk for serious illness and death, especially among infant and children in Pakistan (Akhtar 2015). Cholera, campylobacteriosis, E. coli gastroenteritis, salmonellosis, shigellosis, typhoid, and brucellosis have been demonstrated to be the major foodborne illnesses in the country as well as infectious diseases caused by viral and parasitic agents. Many fatalities have been associated with food poisoning but the actual agent has rarely been determined. Many health experts believe that rapid spread of gastrointestinal diseases cannot be controlled if the public has no awareness of prevention and control measures against cholera and other forms of gastroenteritis, and that in most parts of the country, sewage is continuously contaminating streams, lakes, springs, wells, and other drinking water sources (Qasim 2009). In May 2011, an epidemic of diarrhea and gastroenteritis occurred in Kamalia, Toba Tek Singh, with over 30 children and others being admitted to hospitals which had few medical supplies. Apart from lack of potable drinking water, the main reason given for the rise in cases was the heat of summer when there were frequent power cuts so that food “rots” or becomes “stale” (Islam 2011). In remote areas of Pakistan, cholera has been responsible for many outbreaks. Two examples in July and August of 2013, both in areas of conflict near Afghanistan, give an idea of local but severe outbreaks. In one case authorities seemed not to want to be involved and in the other vaccinations are carried out. Although water is the primary vehicle of the Vibrio cholerae pathogen, it can easily contaminate prepared foods through poor hygienic practices. In July 2013, five deaths from cholera occurred in Pashtoon Kot area, Balochistan region of Pakistan (Federally Administered Tribal Areas) along the Afghan border (Staff 2013), some 70 km from Quetta, in the absence of any emergency medical aid. The condition of an additional 20 people suffering from the disease was said to be critical. A local tribal elder expressed the fear that outbreak of cholera might cause loss of life at large scale. He complained that the doctor and paramedics deployed at the basic health center in Panjpai live in Quetta and are rarely seen at the center. Officials of the provincial health department appeared to be unaware about the cholera outbreak and loss of lives (or ignored these), as they sent no medical teams to the affected area. In fact, Pakistani government rebuffed international media’s claims, and did not respond to requests to dispatch healthcare professionals to the Balochistan area. It was assumed the outbreak would continue without medical aid. In 2012, cholera outbreaks killed hundreds of people, mostly children, in flood-hit districts of Nasirabad, Jaffarabad and Jhal Magsi where waterborne diseases were reported at a large scale because of consumption of contaminated water by local people. In August 2013, two people died and 320 others had fallen ill, following a cholera outbreak in Kurram Tribal Agency near Afghanistan (Hussain 2013). Dhand and Kudiad Khel were the worst-hit areas but vaccinations were carried out amid tight security, and tribesmen were instructed not to drink water directly from the well and boil it first instead since the wells had been contaminated from the rain water. Around 100 people were shifted to Parachinar Headquarters Hospital, while others were discharged after medical aid.
Sometimes diseases kept at bay by functioning public health systems come back when these break down as is occurring in a few of the countries embroiled in internal strife and outside attacks. For instance, in Iraq in October, 2015, >1800 cases and 6 deaths of cholera occurred which started along the Euphrates valley in September with the governorates of Baghdad and Babil, south of the capital, being the worst affected with more than 500 cases each. The epidemic then spread to the northern autonomous Kurdish region, which hosts hundreds of thousands of people displaced by conflict from other parts of Iraq (Agence France-Presse 2015). A previous outbreak killed four people in the Kurdistan region in 2012. The United Nations says the number of people displaced by conflict in Iraq since the start of 2014 has topped 3.2 million which would exacerbate the spread of the disease. Authorities blamed the cholera outbreak mostly on the poor quality of water caused by the low level of the Euphrates. Limited vaccination programs are in place in areas of conflict. In October, 2015, two persons arriving in Kuwait from Iraq tested positive for cholera and both were provided proper treatment and recovered. The Ministry of Health recognized that further cases could be discovered among people arriving from Iraq, but because Kuwait has a well-structured health infrastructure with water and sewers grids, and a supply of healthy and safe food, the disease should not spread into the Kuwaiti population (Anonymous 2015a).
Probably there are some cases in Yemen and Syria, countries also with limited public health infrastructures, but have yet to be identified. In Saudi Arabia, a country with a well-maintained health system, the main infectious disease concern today are the infections and deaths arising from exposure to the Middle East respiratory syndrome corona virus (MERS-CoV), which has reservoirs in camels and bats (Todd and Greig 2015). A potential food source for this virus and other pathogens is from unpasteurized camel milk, as camel farmers drink the milk as well as being exposed through other aspects of camel contact. This brief review indicates that diarrheal diseases, caused by cholera, dysentery, hepatitis A, salmonellosis, shigellosis, typhoid fever, and other enteric diseases through water and food are major contributors to ill health in the region in agreement with the WHO (2015b) report on global estimates of foodborne diseases.
Foodborne Disease in Specific Countries
In the region, not very many outbreaks of foodborne disease tend to be investigated, or at least reported publically, and those that are tend to have fatalities or are very large. For instance, in June, 2009, two children and one adult were brought to a hospital in Dubai, UAE, with suspected food poisoning (vomiting) after they ate take-away food (the father was out of town). Although the mother eventually recovered, the two young children (5 and 7 years old) died, one on arrival and the other the next day. The cause was not determined (Saberi and Scott 2009). It is not known if the family or restaurant was primarily responsible for the deadly gastrointestinal attack as bacteria can multiply quickly in the hot summer months, and the public had been recently warned to minimize eating out at this time of year, especially at smaller eateries where hygiene levels are often of lower standard. A toxin was likely involved to cause fatalities so rapidly, but it could have been an accidental contamination of the food with a chemical such as a pesticide, as much as it could have been with an enterotoxin produced by Staphylococcus aureus or Bacillus cereus through careless ambient temperature storage. Unfortunately, this was one episode in a string of incidents, most of them with fatalities, in the county. In April, 2007, a 3-year-old died of suspected food poisoning in Sharjah, and in August, a 10-year-old girl died of food poisoning in Abu Dhabi. In March, 2008, six people fell ill after eating buffet food at a restaurant in the large Ibn Battuta Mall, Dubai; in November of the same year, 14 employees at a cement factory were hospitalized after consuming what was considered rotten food prepared at the factory kitchen in another Emirate, Ras Al Khaimah. In May, 2009, a 4-year-old girl died of suspected food poisoning in Sharjah. The Indian family of four rushed to the hospital after series of vomiting but were too late to save the girl. Dubai has been reporting foodborne outbreaks and cases through its foodborne disease investigation and surveillance system since 2011; in that year there were 1663 cases reported in the first nine months (Saseendran 2014). In 2013, 1123 suspected cases of foodborne illnesses were reported but only 518 cases were confirmed. No deaths were reported since the surveillance system was in place.
Egypt has had a particular problem with foodborne illnesses in universities and schools, mostly without a confirmed etiology, which seem to be related to poor food quality. Food poisoning is not uncommon in Egyptian university dormitories, where basic hygiene standards are often not observed, but the following outbreak was one of the largest. On April 2, 2013 hundreds of Egyptian students angered by a mass outbreak of food poisoning at a Cairo university stormed the offices of the country’s top Muslim cleric and university president, Ahmed el-Tayeb, because of the 479 students who were hospitalized after a meal served at the university dormitories in the Nasr City district of Cairo (Associated Press 2013). The university is affiliated with Al-Azhar mosque, the world’s foremost seat of Sunni Muslim learning, and awards degrees in sciences and humanities, as well as in religious studies. In the protest, thousands of Al-Azhar students blocked roads, broke into el-Tayeb’s offices by the main campus, and chanted slogans against the university’s management. The causative agent was unknown, and only with the incubation period, types of symptoms and their duration would it be possible to consider the potential etiologies of this illness. Because of their poor quality, campus meals were not very popular before they were being blamed for the current food poisoning outbreak. Although investigators were not able to find a specific cause, the university suspended its food services director and some other staff members. Within a few weeks food poisoning affected 161 students on April 29, 2013 at the same university, Al-Azhar (Masriya 2013). Investigations were initiated within the University and by the Ministry of Health, and apparently “bad tuna” had been served at the campus cafeteria; no further details were given. If tuna was the vehicle of the outbreak, scombroid poisoning was the likely cause of the illnesses. The allergic-like symptoms generally begin 15–60 minutes after ingestion and usually resolve in a few hours. Scombroid fish poisoning occurs after fish, most frequently tuna, with high levels of accumulated histamine or other biogenic amines, is eaten. But “bad tuna’ could equally be contaminated with bacterial or viral enteric pathogens with a longer incubation period. A month later there was another outbreak. Because at least three outbreaks of food poisoning occurred at Al-Azhar University between April and May 2013 with over 700 cases of food poisoning detected in the university’s male dorms, the dorm’s director, the university’s kitchen manager and eight chefs were sentenced in November, 2013, to 5 years in prison with a financial bail. In a similar situation, Egypt’s top prosecutor ordered a swift investigation into the 178 cases of food poisoning reported in two primary schools in October, 2014, in Suez (Masriya 2014). An official of the Ministry of Education indicated that the poisoning was caused by the consumption of milk provided by the schools. The distribution of milk to all schools in the governorate was halted until the milk’s validity was ensured. If milk was responsible, the etiological agent could be Bacillus cereus enterotoxin if the onset time was short, or less likely an infectious disease pathogen such as Salmonella or E. coli O157:H7. On January 1, 2015, 150 female students were diagnosed with food poisoning at Al-Azhar University in Upper Egypt’s Assiut/Asyut Governorate, by the banks of the Nile, and were briefly hospitalized in an Assiut city (Anonymous 2015b). This follows a similar incident which occurred in April 2014 when 29 students, also in the girls’ dormitories, contracted food poisoning on the university campus in Luxor. This report also flags two major poisoning incidents involving at least 500 students ill consecutively at its campuses in Cairo in 2013 (probably the ones already discussed). The reason given for these repeated mass foodborne illnesses among university students is the quality of the food served them. Apparently cheap, subsidized food is poorly stored, cooked and distributed to the poorer university students. In most cases the attorney general would open a criminal investigation that would be closed without knowing the microbiological cause of these outbreaks. The ProMED-MENA Editor speculated that enterotoxins of Staphylococcus aureus were the most probable cause of such communal food poisoning, as a toxic dose of less than 1.0 microgram in contaminated food is sufficient to produce symptoms of staphylococcal intoxication. This toxin level is reached when S. aureus populations exceed 100,000/g, a condition likely to be present in these university kitchens because of intense pressure on them to feed a huge number of students in a short time, taking into consideration that most of these kitchens lack basic hygienic measures with regard to safe food handling. The Editor also considered Shigella, with its low infective dose (10–200 depending on the species) as another possible agent. However, the incubation period and symptoms of S. aureus intoxication and shigellosis or dysentery are quite different.
Pakistan is similar to Egypt in that much of the country is rural but with very large cities with high populations (total population is 89 million in Egypt and 184 million in Pakistan, the most populous of all Middle Eastern countries). In September, 2010, more than 250 of the 1400 flood victims at a relief camp in Bengali Boys Sindhi Section School in Ibrahim Hyderi vomited after eating cooked food and then fell unconscious; 59 of them had to be taken to a nearby hospital (Aligi 2010). A local philanthropist had been providing cooked food to the flood victims but by the time the food arrived at the relief camp, the cooked rice had turned “stale”. Since the rice did not show any sign of spoilage, it was served to the flood victims. A similar incident had taken place 3 days earlier at another town where more than 80 flood affectees had fallen unconscious after consuming “stale” food and 10 were hospitalized. None was seriously affected. During the investigation, it was noticed that the sanitary situation in and around the relief camps was very poor. Even though the reason for the illness was not determined, the police took action against the donor and two caterers. In fact, based on the information of the vehicle and the symptoms, Bacillus cereus enterotoxin which is known to be produced in boiled rice, was the most likely agent.
In the following two outbreaks yoghurt is blamed for the serious illness and deaths though details of the symptoms are not given. Rapid onset of symptoms indicates the presence of a toxin of some kind, although yoghurt is not a food known to be frequently contaminated with pathogens because of its high acidity. Either the yoghurt was made under very unhygienic condition with the source of the milk perhaps being spoiled (possibly containing Bacillus cereus enterotoxin), or a chemical had been added accidently such as a pesticide, or deliberately and illegally to enhance the flavor. However, it is possible other foods were involved and yoghurt was not the contaminated vehicle. In January 2011, in Lahore, a hospital employee died and two other employees became critically ill after eating contaminated yoghurt. The three employees ate rice with yoghurt at a local restaurant (Ians 2011). Action was taken against the restaurant owner and manager. No further details are known. In early April, 2014, a Rawalpindi family of ten became seriously ill after eating a home-prepared evening meal where yoghurt was suspected to have been the contaminated food, and they were taken to a hospital, where a teenage boy and 7-year-old girl died (Asghar 2014). The surviving family members remained in critical condition for some time but eventually recovered; the cause of the illnesses was not discovered, although it was postulated by a relative who had eaten the yogurt with the meal that it was possibly poisonous or, strangely he thought a lizard might have fallen into it.
In February 2012, at least four people died and another seven were hospitalized in a critical state after eating home-cooked biryani (a dish made with spices, rice and meat or vegetables) in a suburb of Karachi (Mahmood 2012). The owner of a grocery shop, who provided the ingredients, was arrested, and a sample taken for analysis. It is not known if any toxin was found. A month later in March, in Faisalabad, more than 60 children and women were ill after eating contaminated aalo-chanay (potatoes, chick peas, onions, tomatoes and spices) purchased from an unidentified vender (Anonymous 2012c). As soon as the children ate the aalo-chaney, they felt ill and started vomiting. Although they were immediately rushed to a rural health center, one boy died. A medical opinion was given that the eaters suffered from “diarrhea and cholera”. However, the onset was too rapid for anything but a toxin of some kind, most likely heat-resistant since the aalo-chanay was cooked. Also, in March 2012, as many as 47 student nurses and eight staff nurses were hospitalized with acute food poisoning at a hospital in Rawalpindi after eating food at the nursing hostel, but none was critically ill (Anonymous 2012d). The nurses residing in the hostel started reporting complaints of vomiting and diarrhea along with high-grade fever at an undisclosed time after a meal. The hospital administration was criticized for failing to provide safe food and drinking water to its employees and demanded immediate inquiry into the case, but none was reported on. The illnesses are consistent with an enteric infection such as Salmonella or norovirus.
In April 2015, at least 20 constables suffered from diarrhea and were admitted to hospitals when they ate food during the Sehat Ka Insaf program, which is a blanket method of administering the polio vaccine along with eight other vaccines, hygiene kits and vitamin A drops in order to circumvent polio-specific terrorist attacks in Pakistan. Local administration purchased packed food, including piece of chicken and juices from a local supporter (Mayar 2015). No further details are given but the chicken could have been undercooked or cross-contaminated with enteric pathogens such as Salmonella and Campylobacter; if the packs had been left at ambient temperatures for some time, these pathogens could have multiplied on the chicken to large numbers. Over thirty children in Faisalabad were hospitalized over 4 days because of diarrhea and gastroenteritis, three seriously, and other children were expected to be ill. Undetermined contaminated food was postulated as the cause, more than usual because of the extreme seasonal heat combined with frequent power outages to allow rapid bacterial growth in contaminated food. The unavailability of clean drinking water was mentioned as a contributing factor to the increasing number of gastrointestinal disease cases. Hospital administrators complained that vaccines and medications were required but were not forthcoming from the Health Department. Probably many family meals were contaminated because of the lack of potable water and any unspecified enteric bacterial pathogens present could grow rapidly in the heat. Children are more vulnerable than healthy adults to infections which might explain the high proportion of sick children seeking medical help.
Botulism outbreaks occur periodically in Iran. In a study of stool and serum specimens of 115 patients with clinical symptoms of botulism, who were at inpatient and outpatient medical centers in Tehran and other areas of Iran, between April 1984 to August 1994, specimens of 73 patients showed the toxin and spores of C. botulinum (Modarres 1997). Type E was the most common causative agent found in this study, being responsible for 71.2% in all specimens; other etiologic types, in order of frequency were types A (16.4%) and B (12.3%). Type E strains are typically associated with fish and freshwater and marine sediments. The results of this study indicate that the cases had consumed salted fish, smoked fish and canned fish, along with cans of green beans and cucumbers. A similar result over a decade later confirms that C. botulinum type E is a major pathogen in Iran. In Gilan Province, of 146 fish samples collected in 2008, 11% of processed fish and 7.5% of non-processed fish contained Clostridium botulinum, mainly type E (Tavakoli and Imani Fooladi 2011). The processing is insufficient to kill the spores or reduce much of toxin produced because the fish tend to be partly cooked with the intestines kept intact. A total of 131 traditional food product samples (57 cheese, 11 kashk [a type of dried yoghurt or thick cream], and 63 salted fish) were examined using a bioassay method for detection of Clostridium botulinum toxin (Hosseini et al. 2010). Standard monovalent antitoxins were used to determine the toxin types. C. botulinum toxins were detected in 4.6% of examined samples (3.5% of cheese samples and 6.4% of salted fish samples). None was found in kashk samples. C. botulinum types A and E were dominant in cheese and salted fish samples, respectively. Consumption of these traditional foods either raw or processed may contribute to foodborne toxicity in Iranian populations. In May 2014, a quick-thinking mother immediately brought her 7-month old boy to an Israeli hospital when she saw he was suffering from vomiting, difficulty in breathing, listlessness, glassy-eyed, apathetic, and an inability to nurse or eat (Bender 2014). A doctor at the hospital diagnosed the child as suffering from infant botulism. He decided to treat the baby with the antitoxin stored in the emergency stocks, even before they got back the lab test results. The hospital like all Israeli medical facilities keep ample supplies of biological and chemical warfare antidotes on hand in case of war or terrorist attacks, and staffers are regularly drilled in dealing with the symptoms of various chemical, neural and blister agents. The infant started recovering soon after the administration of the antidote. In the rare disease of infant botulism, spores of Clostridium botulinum are ingested and the infant’s flora is not mature enough to prevent germination and slow growth of the toxigenic pathogen. It is entirely possible that infant botulism occurs more frequently in the region but is not diagnosed.
Foodborne disease surveillance depends on an infrastructure of reporting and diagnosis in hospitals, epidemiologists, and food testing laboratories. Lebanon is an example of a country where modernization in public health seems to occur at a glacial pace. However, diseases including those of foodborne and waterborne origin, are documented and published. The Law of December 31, 1957 regarding communicable diseases in Lebanon mandates all physicians, from private or public sectors, in hospitals or ambulatory services, to declare to the epidemiologic surveillance unit of the MOPH all diseases considered a risk to public health. The data available at the Ministry of Public Health (MOPH) are compiled from different sources, and the declaration of cases remains irregular and insufficient (MOPH 2012). In 2011, foodborne and waterborne diseases were the most frequently reported in Lebanon at a rate of 0.4 ‰ (total of 1468 cases), with the highest rate in the Bekaa (0.7 ‰) and the lowest in the South (0.1 ‰). The most common infection was viral hepatitis A, which represented 30.5% of the total food and waterborne diseases with 448 cases. There were also 362 cases of typhoid (24.7%), 311 cases of food poisoning (unspecified, 21.2%), 186 cases of dysentery (12.7%), 34 cases of brucellosis (9.1%, 15 cases of parasitic worms (1.0%) and 12 cases of hydiatic cyst (0.8%). No cases of cholera and trichinosis were declared. Hydiatic cyst (cystic echinococcosisis) caused by Echinococcosis (typically E. granulosis) is acquired by contact with animal feces contaminated with tapeworm eggs. Sources include contaminated food (meat), water, and animal fur. Cysts containing tapeworm larvae may grow in the body for years before symptoms appear. When cysts become large, they may cause nausea, weakness, coughing, and belly or chest pain.
Occasionally, well-investigated outbreaks are published; the following two examples are from Lebanon and neighboring Jordan. In May 2004, 32 employees suffered from diarrhea, fever, and abdominal pains 5.5–22.5 h (mean, 10.3 h) after eating chicken noodles au gratin at a catered lunch served at a bank cafeteria (Hanna et al. 2009). A few cases had systemic infections. Salmonella Enteritidis (SE) was confirmed in stool and blood cultures within 48–72 h after hospital admission of the first cases, and also in leftovers of the suspect food. The same dish had been served at the bank in the past with no apparent health problems. Preparation normally started in the evening prior to the day the dish is served. However, in this instance, some of the constituents had been prepared 3 days ahead, because the dish was to be served on a Monday, immediately after the week-end closure. No Salmonella was found in rectal and nasal mucosal swabs taken from all 18 kitchen workers, or in the tanker water supply (although it had high fecal coliform counts), but SE was found in a frozen batch of the same raw chicken breast consignment that had been used for the chicken noodles. The batch of chicken came from a large producer of poultry and eggs in Lebanon, who was advised of its potential involvement in a major foodborne outbreak. However, the investigators were refused access to the poultry-producing facility. It is highly likely that contaminated chicken carcasses had been, and would continue to be, shipped to many parts of Lebanon. That the same SE strain occurred in the patients, the raw chicken, and the leftover food was confirmed through random amplified polymorphic DNA polymerase chain reaction (RAPD-PCR). It would appear the 3-day delay in the chicken noodle preparation was significant in allowing the Salmonella present in the ingredients not only to survive but probably to grow; undercooking, cross-contamination, inadequate storage and reheating all may have played a role in the outbreak, but no more information was available to determine which of these were the key factors in the outbreak. The bank management decided to sue the caterer and because they were aware of apparently inefficient way that public authorities were conducting the procedure, they took the initiative to call upon an independent investigative team to obtain solid evidence to win any court action. The caterers, concerned that they would be the only party blamed for the Salmonella outbreak, had succeeded in concealing some raw and cooked items from destruction by the public health authorities, which was their normal practice after a complaint. These items were central to establishing contamination upstream from the caterer’s kitchen. No action seems to have been taken against the poultry producer who was the source of the SE, a pathogen that is invasive of flocks and difficult to eradicate. The authors complained about the obsolete Lebanese laws dating back to the 1930s that still governed what should be done following a report of “food poisoning”. Public health officers are mandated to stop the spread by destroying allegedly contaminated food items and closing down incriminated facilities. Hanna et al. (2009) stated that this kind of action is generally lauded by the public but does not help determine the cause to develop appropriate prevention and control strategies. They also complained that because no investigation is typically done, many non-implicated foods and ingredients are wastefully discarded.
The Jordanian example is over two decades old, but is worth noting in detail. In September 1989, a 183-case outbreak of salmonellosis occurred in a university hospital in Amman after employees, patients and visitors ate in the cafeteria. The incubation period ranged from 16 to 72 h. Symptoms included diarrhea (88%), fever (71%), abdominal pain (74%), dehydration (34%), and bloody stool (5%); 84 were hospitalized (Khuri-Bulos et al. 1994). Cultures of eight food items were negative, but stool culture on 90 of 180 patients and 11 of 61 kitchen employees yielded Salmonella Enteritidis (SE) group D1. A cohort study revealed a food-specific attack rate of 72% for the steak and potato meal and 18% for the rice and meat meal. Stratified analysis of the steak and potato meal revealed that the potatoes were implicated most strongly. Cultures were obtained from all kitchen employees, who showed no symptoms of illness, but 11 of 61 grew SE group D1. One asymptomatic, culture-positive employee had prepared the mashed potatoes on September 23, 16 h before the first case presented at the hospital emergency with severe gastroenteritis symptoms. All of the food workers had negative stool cultures 3 months earlier. The potatoes were mashed by machine, but peeled after boiling and mixed with milk by hand, using a ladle but no gloves. Two different batches, the first of which was served exclusively to hospitalized patients and the second to a few remaining patients and employees, were prepared and served within 30 to 60 minutes of preparation. From the epidemiological data it can be assumed that the infected handler fecally contaminated only the second batch of potatoes, thus sparing most of the highly susceptible inpatients from exposure. Furthermore, while potatoes clearly were implicated, individuals who ate steak only had an elevated risk of being attacked. This probably was due to surface contamination of foods being served on the same plate. Kitchen employees harboring Salmonella were excluded from work until they had three negative stool cultures taken 1 week apart; it took 6 weeks for them to return to work. Stool surveillance that was routinely carried out in the hospital was ineffective in detecting infected employees to prevent this outbreak and the investigators recommended that employees adhere to proper hygienic practices including thorough washing of hands, especially when preparing food.
Today, Salmonella is only one of many of the pathogens that can be encountered in foodborne illness. One of the newer pathogens, well established in the West is norovirus (NoV), which causes more cases of foodborne disease in the U.S. than any other agent (Scallan et al. 2011). In May 2009, a significant increase in acute gastroenteritis (AGE) cases was noted in the American health clinic at Incirlik Air Base (IAB) in Adana, Turkey. This increased rate of AGE led to discussions with local Turkish military public health authorities, which confirmed that the Turkish military community and the residents of Adana were also experiencing an anecdotal increase in AGE illnesses (Ahmed et al. 2012). An epidemiologic investigation was launched to attempt to identify the cause and possible source of this AGE outbreak at IAB from May to June with the peak incidence of cases during the week of May 31–June 6, with a total of 71 patients seeking medical care at the clinic. Of the total 187 infected persons, 82 patients completed the case survey, 79% reported diarrhea, 46% reported vomiting, and 29% reported fever. The median number of days between symptom onset and clinic visit was 2 days. During the 7 days prior to symptoms, 73% of respondents reported travelling off base, 56% reported eating off base, and 24% reported using an outdoor pool. This outbreak had a significant negative operational impact, degrading mission readiness with nearly 20% of the American population in a 1-month period affected. Initiation of a clinic case-based investigation yielded 37 stool specimens in which NoV was detected in 43%, with 81% of the positive NoV specimens identified without a copathogen. DNA sequencing data demonstrated that several relatively rare genotypes of NoV contributed to this outbreak; four different genotypes were isolated from 16 positive specimens. Two of the NoV strains were previously reported in Iraq and only from deployed troops, while the other two genotypes were reported in South Africa and in the US. In Turkey, little systematic data on circulating NoV genotypes exist. However, GIIb/GII.4 strains have been frequently identified in Turkish children with gastroenteritis; strains belonging to this genotype have been found in Europe and mainly in children. Previous reports from British troops deployed to Iraq indicated that two NoV strains isolated were responsible for cases of gastroenteritis there. Similar mixed NoV outbreaks have been previously observed and are often attributed to systematic failure of cooking/cleaning/drinking water supplies (Ahmed et al. 2012). One limitation of this investigation was that the survey was not used to capture data from a control group, those without recent AGE, preventing carrying out a risk factor analysis. Another limitation was the lack of environmental samples that could be tested for NoV in order to track the source of outbreak. From anecdotal information, it is likely many in the local population and the Turkish military base were ill, but a formal outbreak investigation in the Turkish population was never performed. From the multiple genetic types involved, one specific contaminated food or water source seems unlikely. The largest Turkish NoV outbreak was in Keçiborlu province of Isparta county between April 5 and 17, 2010, with 1428 patients seeking medical help from the healthcare centers, after suffering from nausea, vomiting and abdominal pain (more frequent than diarrhea) (Sözen et al. 2014). Because of underreporting, the number of affected people was estimated to be higher. Municipal water was the suspected source but no samples tested positive. As a cautionary note, the authors suggest that NoV may not be the only causative agent of gastroenteritis outbreaks, especially from an undetermined fecal source, and bacterial, viral and parasitic agents should be examined together with the NoV.
In Saudi Arabia, a national policy for reporting, notifying, and recording incidents of bacterial food poisoning was established in 1984 (Al-Joudy et al. 2010). Since then Salmonella food poisoning outbreaks have been reported from different regions of KSA, exhibiting seasonal and regional variations, with chicken, meat, and rice being commonly incriminated food items, and frequently reported in the Saudi Epidemiological Bulletin. Al-Mazrou (2004) reviewed the history of foodborne outbreaks in KSA and saw an increase over the last few decades, especially those caused by Salmonella, with the main food vehicles being chicken, meat and eggs, and S. Enteritidis being the most frequent Salmonella serovar responsible. According to ProMED editorials, restaurants and communal feasts and institutional feeding (such as in school cafeterias, hospitals, nursing homes, prisons, etc.) where large quantities of food are prepared several hours before serving are the most common settings in which foodborne illness incidents occur (http://www.promedmail.org). For instance, in 2005, a hospital in the Jizan Region received 19 suspected food poisoning cases that were ill after taking meals from a restaurant, including a woman who suffered from severe diarrhea, abdominal pain, vomiting and dizziness (Fagbo 2005). The restaurant was closed down and three of its workers were detained pending the results of laboratory tests. The report of an investigative committee could not find a specific cause, but noted that the restaurant had earlier been responsible for some hygienic violations. In 2015, 80 cases suspected of foodborne illness after eating a meal at a restaurant were admitted to various hospitals in the Najran region (AlHayat 2015). Most of the cases were not seriously ill. No report was given on the samples that were taken from the suspected restaurant, which was closed temporarily. There is an interesting observation related to variant Creutzfeldt-Jakob Disease (vCJD); four cases have occurred in the US since the disease was first diagnosed in the United Kingdom in 1996 linked to consumption of cow meat suffering from bovine spongiform encephalopathy (BSE); two of these were associated with the United Kingdom (where BSE was first reported), but one came from Saudi Arabia and the most recent case in 2014 had extensive travel to the Middle East and Europe (CDC 2014). This may indicate some source of vCJD in the Middle East including Saudi Arabia.
One of the big concerns for KSA is the annual Hajj with millions of Muslims from around the world converging on Mecca, in Saudi Arabia, each year. No other mass gathering can compare with the Hajj, either in scale or in regularity, and various communicable disease outbreaks of various infectious diseases have been reported repeatedly, during and following the Hajj (Memish 2010). In 2006, an outbreak during the Hajj occurred where all the cases came from one tent occupied by 50 soldiers located in a government camp in Mina, Makkah province, near Mecca (Al-Joudi 2007). The camp was served by a catering company that prepared and distributed three meals daily (breakfast, lunch, and dinner). A case was defined as any individual who developed diarrhea with or without abdominal pain after eating at the camp in Mina in January, 2006. Of the soldiers who were interviewed, 16 (39%) had developed gastroenteritis, most commonly manifested by diarrhea (100%), and abdominal pains (87.5%). The mean incubation period was 12.6 ± 4.9 h and the epidemic curve suggested a common point source outbreak. Out of three served meals, lunch with a rice dish was found to have a statistically significant association with illness. Unfortunately, no food remnants were found for sampling, and the results of stool cultures of all diarrhea patients, and rectal swabs from all food handlers were inconclusive. Temperature abuse was cited as a contributory factor in this outbreak. Based on the incubation period and symptomatology, Bacillus cereus would be the most likely etiological agent. Another example of a foodborne illnesses associated with the Hajj occurred in 2011 when 81 Bangladeshi pilgrims were taken to hospitals in Madina (Medina) after eating a meal prepared by an unlicensed caterer (ProMED-MENA 2011). They suffered from abdominal pains associated with diarrhea and vomiting. The pilgrims were all treated and discharged, except for one who remained hospitalized. Samples of the food they had eaten were sent for analysis but the results are not known. Considering the mass of people converging on this small part of the Middle East, it is surprising there are not more foodborne disease outbreaks. This may mean excellent food control by the authorities or some illnesses are simply not recognized and reported.
At least 750 Bahrainis suffered from food poisoning after eating catered sandwiches served during a wedding celebration, the biggest mass poisoning outbreak in the country’s history (ProMED-MENA 2002). The wedding took place in the Safala village, near the eastern island of Sitra. All eventually recovered after treatment but one man who had sickle cell disease, died. Teams were formed to investigate the outbreak, and blood specimens from all workers at the bakery who prepared the egg, cheese, and mayonnaise sandwiches along with leftover sandwiches and their ingredients on the caterer’s premises were sent for bacteriological analysis. The bakery which supplied the sandwiches was closed by the Public Health Directorate at the ministry pending the investigation’s results. Unfortunately, no final report was released to the public. The ProMED editor considered the etiological agent could be Salmonella or Staphylococcus aureus enterotoxin, depending on the length of the unstated incubation period.
The region experiences some unusual type of illnesses relating to on-going hostilities. For instance, the United Nations has been sending aid to reach besieged towns in Syria, close to the Lebanese border, but in October, 2015, it sent hundreds of boxes of “moldy” high-energy biscuits past their ‘sell-by’ date in September (320 of the 650 boxes transported) to Zabadani and Madaya, apparently causing food poisoning (Afanasieva et al. 2015; Muhkalalati and Kieke 2015). Officials stated these could be the only cause of an outbreak of food poisoning among almost 200 residents who came to makeshift hospitals, mainly children who had vomiting, diarrhea and abdominal swelling almost immediately after eating the biscuits. The biscuits were described as “moldy and rotten and had been poorly stored”. Apparently, when the last aid order that was sent was filled, there was a shortage of food. The Red Crescent, who was filling the order, took some of the expired goods to complete it. However, these biscuits had only just expired and normally would not have posed any health risks to those eating them. Nevertheless, the words poorly stored suggest that moisture may have encouraged microbial growth (visible mold more likely than bacteria because fungi can grow aerobically in the presence of the presumably elevated sugar content in the high energy biscuits). Also, contributing to the symptoms, the residents of Zabadani and Madaya had been blockaded for 120 consecutive days, and their immune systems were extremely weak.
Refugees are also at risk of gastrointestinal diseases from contaminated water or food. Up to two million Syrian migrants fleeing Syria due to the civil war were living in Turkey, and supplying them with safe and secure food supplies is a challenge for any host country. One incident, no doubt, one among many indicates the risk of contaminated food. In April, 2015, five security forces were injured after Syrian migrants in a tent city in Turkey’s southeastern province of Mardin reportedly attacked guards over allegedly being poisoned from the lunch at the camp (Anadolu Agency 2015). Some 17 Syrian migrants were detained after the incident; 66 Syrian migrants out of the 5230 currently residing in the Temporary Sheltering Center in Mardin’s Derik district applied to the center’s hospital with symptoms of food poisoning, dizziness, and vomiting. After treatment they were discharged, none of them in a critical condition. Although an investigation was conducted and samples from the lunch sent to the lab for analysis, no further information was available on the outbreak. ProMED speculated that if the lunch food was the vehicle, it would be a short incubation illness likely caused by Staphylococcus aureus, Bacillus cereus, Clostridium perfringens, or possibly a non-biological toxin. These illnesses may cause vomiting, diarrhea, or both, and are usually short in duration (less than 24 h), and are not associated with prominent fever.
In Iraq, no recent foodborne disease outbreaks have been published, but no doubt many have occurred in the last decades with so much public health infrastructure dismantled. Only the most newsworthy of outbreaks are being covered by the press today. Iraq and other Middle Eastern countries are in sectarian turmoil and on two occasions Islamic State (ISIS/IS/ISIL) fighters (jihadis) were likely poisoned by cooks who infiltrated their camps. In November, 2014, a group of defected Syrian soldiers (Free Syrian Army men) who posed as cooks reportedly poisoned ISIS militants after they ate a contaminated lunch at the Fath El-Sahel camp, where 1200 of them were based (Gee 2014). Apparently about a dozen of the jihadis were killed and 15 taken to nearby field hospitals. The ‘cooks’ immediately fled, along with their families, with the help of fellow revolutionaries. Seven months later, in July 2015, 45 jihadis died after ingesting an Iftar meal eaten by 145 ISIS militants (Akbar 2015; Variyar 2015). It remains unclear whether the jihadis, who were breaking their Ramadan fast in Mosul, Iraq, died of accidental food poisoning or intentional poisoning, but it is likely a repeat attack of the earlier incident described above. The nature of the poison or details of the illnesses in either episode are not known. However, in both episodes, onset and severity of the attack were rapid, probably caused by a relatively tasteless chemical in lethal doses added to one or more foods. Targeting the military by any means including poisoning food has always been a strategy of opposing forces. In February 2012, a deliberate attack was foiled when Afghan border police detected a significant amount of bleach in fruit and coffee stored at their main border checkpoint between Afghanistan and Pakistan, a likely attempt to poison the Afghan security forces (Tucker 2012). The police decided that although none of this food had been consumed, the level of contamination was high enough to cause serious injury, and it must have been done intentionally. There had been previous incidents of intentional food poisoning aimed at Afghanistan’s civil defense forces, including an episode in Kabul in 2011 when several people were sickened. In 2012, in southern Helmand province militants killed four Afghan policemen and two civilians inside a police checkpoint by poisoning their yoghurt coordinated with an attack (Anonymous 2012a). There had been several recent poisoning incidents involving members of the Afghan National Police, as part of attempts by the Taliban to infiltrate the security forces; three police officers were reported missing, along with their weapons and a police vehicle, following that attack in Helmand province. Taliban militants had first poisoned the police officers’ yoghurt before launching a full scale attack on the checkpoint. Similar tactics had been used by insurgents in Helmand before. The same thing happened again in January 2016 when a rogue policeman collaborating with insurgents in southern province of Uruzgan shot dead 10 colleagues after first poisoning their food, but no further details are given (Reuters 2016).
Food Safety Research and Surveys
Turkey does have food laws that are supposed to limit food contamination and resultant foodborne illnesses. The 2000 Turkish Food Code stipulates that all Turkish food businesses have to provide food hygiene training commensurate with the work activities of their staff. To see what progress had been made in this area Baş et al. (2006) evaluated knowledge, attitudes, and practices concerning food safety issues among food handlers in Ankara, conducting face to face interviews and administrating questionnaires. The majority of the 764 food handlers who responded (47.8%) had not taken a basic food safety training (and probably most of non-respondents had not either). The mean food safety knowledge score was 43.4 ± 16.3 of 100 possible points. The self-reported hygienic practices showed that only 9.6% of those who were involved in touching or distributing unwrapped foods always used protective gloves during their working activity. Of those food handlers who used gloves, only 8.1% and 3.8% always washed their hands before putting them on and after removing them, respectively. In addition, there was a difference handlers’ scores depending on where they worked. Scores were higher for food handlers in catering establishments (50.4 ± 9.4), school food services (52.5 ± 9.2) and hospital food services (50.9 ± 9.2) than restaurants (47.3 ± 8.6), hotels (47.4 ± 8.3), takeaways (44.1 ± 2.5) and kebab houses (37.9 ± 6.7). These scores may also be biased upwards since they were self-reported and not observed practices. The study demonstrated that food handlers in Turkish food businesses often have lack of knowledge regarding the basic food hygiene, e.g., critical temperatures of hot or cold ready-to-eat foods, acceptable refrigerator temperature ranges, and cross-contamination. Those who were trained scored better, and the authors stated there was an immediate need for education and increasing awareness among food handlers regarding safe food handling practices.
In Istanbul from 2005/2006, thermophilic Campylobacter was isolated from 11.1%, 21.6%, and 50.4% of beef, mutton, and chicken samples tested, respectively (Bostan et al. 2009). There was no significant seasonal variation in the prevalence of the pathogen. C. jejuni was the species most commonly isolated from chicken meat, while C. coli was the most common in beef (63.3%) and mutton (63.9%) carcasses. Campylobacter isolates were most often resistant to tetracycline (69.1%), followed by trimethoprim-sulfamethoxazole (64.2%), nalidixic acid (58.1%), erythromycin (56.9%), enrofloxacin (48.8%), ciprofloxacin (42.7%), chloramphenicol (36.2%), and gentamicin (26.0%). The results of this study suggest that a high proportion of meat samples, particularly chicken carcasses, are contaminated by campylobacters, most of which are antimicrobial-resistant strains. In Yemen, the prevalence of Salmonella in food was determined in Sana’a city from April 2009 to April 2010 by Ahmed (2013). Of the 362 different food samples collected from local markets, Salmonella spp. were isolated from 26 (7.2%). The highest prevalences were in red meat (14.7%), chicken (12.1%), eggs (11.8%), cooked foods (9.5%), raw milk and milk products (5%), juices (4.8%), vegetables (4.4%), sandwiches (3%), and pastries (2.6%). Serogroups identified were B, C1, C2-C3, D1, E1, and E4, and some foods contained more than one isolate with different serogroups, especially red meat.
Because handlers in foodservice facilities play a major role in transmission of foodborne diseases (Greig et al. 2007), studies have been carried out to demonstrate their knowledge of practices related to food safety. In Jordan, Osaili et al. (2013) measured food safety knowledge of food handlers working in fast food restaurants in the cities of Amman and Irbid. A total of 1084 food handlers in 297 fast food restaurants participated in this question survey study. The overall knowledge of food handlers on food safety concepts was considered to be fair (69.4%). The food safety aspect with the highest percentage of correct answers was “knowledge of symptoms of foodborne illnesses” (81.7%) and “personal hygiene” (79.9%), while the lowest percentage of correct answers was for “safe storage, thawing, cooking and reheating of the foods” (52.4%), critical practices to prevent the survival and growth of pathogens. The mean knowledge score of “personal hygiene” reported in the study was much higher than 51.5% and 31.8% reported by Martins et al. (2012) and Baş et al. (2006), for the food handlers in Portugal and Turkey, respectively. Also, only 31.9% of respondents considered the duration of hand washing to be ≥20 s. When they were asked how they check that the poultry is sufficiently cooked, only 31% knew “when the meat has the correct thermometer reading”, although 85% of the respondents had thermometers in their restaurants. About 25% of them answered that poultry is cooked “when it has been cooked for the stated time” (24%) and “when it looks cooked” (27%). About 50% of them would store leftovers on the steam table (40%) and in the refrigerator (53%) while about 27% of the correspondents would store leftovers at room temperature in kitchen or in the oven. A low percentage of the respondents (20%) reheated leftovers to the appropriate temperature (73 °C). About 40% and 20% of the respondents had heard about Salmonella and hepatitis A virus, respectively, but ≤10% of the respondents knew about Listeria monocytogenes, Staphylococcus aureus, Bacillus cereus, Escherichia coli O157:H7, Clostridium perfringens, Campylobacter jejuni, or Shigella. Food workers who had enrolled in a food safety training course had significantly higher total food safety knowledge score than those who did not take any training. There was no association between the experience or any other characteristic of food workers and total food safety knowledge score. This study suggests adopting proper food safety education training courses to food handlers, periodic evaluation of food handlers’ knowledge and food safety training course materials. Also, the authors considered that better pay for food handlers would improve the food safety status in foodservice institutions. Similar concerns over practices that could lead to food contamination and foodborne illnesses were demonstrated in Lebanon. A survey was conducted in Beirut to evaluate the knowledge, attitudes and practices related to food safety issues of food handlers (n = 80) in foodservice establishments (n = 50), and to assess the influence of management type on enactment of safe practices on food premises (Faour-Klingbeil et al. 2015). The data suggest that while respondents do have some knowledge of food safety aspects, substantial gaps in their knowledge and self-reported practices associated with critical temperature of foods and cross contamination remain, therefore posing health risks to consumer health. Food handlers in corporate managed food outlets showed a significantly higher awareness on food safety practices. It is concluded that the management type is an integral element of the Theory of Planned Behavior that influence food handlers’ practices and substantiate the need for more research work on safe food handling in the context of food safety culture framework in food businesses. As in many other MENA countries, there is a critical need for food safety education interventions and technical guidance fostered by synergistic participation of the private and public sector to support food handlers in SMEs (small and medium sized enterprises).
Parasites are not often looked for in Middle Eastern countries but they are frequent, and one of the ones of most concern for pregnant women is Toxoplasma gondii which is transmitted through undercooked meat and cat feces. Since stray cats are common in some localities, of 240 fecal samples of stray cats examined in Kuwait, 22 (9.2%) were found to be infected with oocysts of coccidian protozoa (Abdou et al. 2013). Toxoplasma gondii was found in 2.1%, and cats <6 months old had higher infection rate with oocyst of enteric protozoa than older cats. A sero-survey of the 240 stray cats revealed that 19.6% were positive to T. gondii IgG. Toxoplasma sero-positivity was observed in a higher number of adult cats compared to younger ones suggesting that with age the risk of exposure to T. gondii increases. Thus, pregnant women handling cats and particularly kittens or cleaning out sand boxes have a chance of infecting their fetuses and eating raw meat.
In Pakistan, enteric pathogens are present not only in water but also foods contaminated from the environment or through human actions. Mishandling of foods allows these pathogens to contaminate and multiply in them. For example, street-vended fruit salads, locally called fruit chats, offered for sale at high ambient temperatures without coverings, and khoya and burfi, two indigenous sweet dairy products, and locally produced ice cream are often heavily contaminated with Enterobacter, E. coli, Klebsiella, Salmonella and S. aureus (Akhtar 2015). These contamination scenarios have led to outbreaks with cases severe enough to be hospitalized. Bus and train stations where pulses (edible seeds of various crops as peas, beans, or lentils), ground meat dishes, and chickpeas are sold to passengers, and are also heavily contaminated with bacteria including Clostridium perfringens. Sweet dishes and home-prepared foods in small communities are commonly contaminated with S. aureus, C. perfringens, and Bacillus cereus leading to rapid intoxications. One study confirmed campylobacters to be present in 48% of 1636 tested samples of milk and meats and 40.9% of vegetables in three major cities of Pakistan (Akhtar 2015). A wide array of vegetables is routinely consumed in this country and serve as a rich source of vitamins, minerals, bioactive compounds, and fiber but these can be sources of enteric infections if they are consumed contaminated. Shigella spp. has been shown to develop resistance and is generally thought to be a major cause of foodborne illnesses, especially among the poor where health care facilities are minimal; shigellosis is associated with poor sanitary conditions and unsafe water for drinking and preparing foods. Possible etiologies can be postulated in the following outbreaks.
Unfortunately, it is not only pathogens that give rise to food-associated disease. Soomro et al. (2008) highlighted the indiscreet use of pesticides in agriculture and its impact on environmental pollution. Despite the increased production cost associated with extensive use of pesticides, their use is common in developing countries. Numerous studies have demonstrated substantial levels of pesticide residues in various foodstuffs in Pakistan, and the groundwater has been observed to be considerably polluted in many parts of Punjab and Sindh provinces of Pakistan (Akhtar 2015). Commonly used open rural wells in the Punjab were polluted with six pesticides: bifenthrin, λ-cyhalothrin, carbofuran, endosulfan, methyl parathion, and monocrotophos. In the Hyderabad region 61% of the tested samples of eight vegetables (cauliflower, green chili, eggplant, tomato, peas, bitter gourd, spinach, and apple gourd) were found to be contaminated with pesticide residues exceeding maximum recommended limits (MRLs) (Tariq et al. 2003; Anwar et al. 2011). Heavy metals such as cadmium (Cd), copper (Cu), lead (Pb), and zinc (Zn) arising from increased industrialization can contaminate agricultural soils and these can be found in fruits (including widely-consumed mangoes), fruit juices, vegetables directly from soil uptake or from the processing and packaging (Akhtar 2015). For instance, spinach, coriander, and peppermint, grown in Sindh province contained 0.90–1.20 mg/kg of arsenic resulting in a total ingestion of arsenic 9.7–12.2 μg/kg body weight/day in diet (Arain et al. 2009; Khan et al. 2010). Aluminum concentration in branded and nonbranded biscuit samples from Hyderabad were found to range 7.4–84.3 and 34.5–70.2 mg/kg, respectively (Jalbani et al. 2007). Similarly, Javed et al. (2009) detected higher concentrations of Cd, Cr, Ni, and Pb residues (mg/L) in bovine and goat milk. Pakistani foods are more prone to aflatoxin contamination because of the warm and humid climate, and the situation is exacerbated by malpractices during handling and storage of edible commodities (Mobeen et al. 2011). Samples of broken rice, wheat, maize, barley, and sorghum ranged 15–45% with the highest aflatoxin concentration (15.5 μg/kg), in wheat samples (Akhtar 2015). Chilies are widely eaten and exported, but aflatoxin levels can be eightfold higher than the EU permissible limits to pose a potential health risk to Pakistani consumers; concentrations can be reduced by more appropriate care and handling of the chilies at pre- and postharvest stages. Nuts and dried fruits in Pakistan are cultivated and processed in the northern areas and have been shown to have aflatoxin levels above the EU limit of 4 μg/kg in up to 70% of samples (Ahmad et al. 1989; Luttfullah and Hussain 2011). Aflatoxin M1 in milk and milk products requires regular monitoring in Pakistan since 3% of the total tested samples of milk were found to exceed the US tolerance limit of 0.5 μg/L (Hussain and Anwar 2008; Hussain et al. 2010), and buffalo milk had higher levels of aflatoxin compared with cow’s milk. Intentional deception of consumers by blending low cost and inferior quality ingredients to make more profit of food intended for sale is prevalent in Pakistan, where families are exposed toxic dyes, sawdust, soapstone, and harmful chemicals in beverages, oil or ghee, bakery products, spices, tea, sweets, bottled water, and especially milk and milk products where more than 50% of samples tested have had adulterants added (Akhtar 2015).
One of the more innovative research projects to provide more home-grown food is in Qatar. The Sahara Forest Pilot (SFP) pilot study demonstrated that there are significant comparative advantages using saltwater for the integration of food production, revegetation and renewable processes: (1) seawater cooling system for greenhouses supports production of high-quality vegetables throughout the Qatari summer, and reduces freshwater usage to less than half that of comparable greenhouses in the region; (2) solar and desalination technologies were successfully integrated as designed into the SFP system, such as the greenhouse and evaporative hedges providing wet-cooling efficiencies without cooling towers; (3) the external evaporative hedges provide cooling of up to 10°C for agricultural crops and desert revegetation with vegetable and grain crops growing outdoors throughout the year; (4) commercially interesting algae showed good tolerance to heat and high evaporation rates in the leftover salty water (miss22 2013; Clery 2013). The concentrated solar power plant uses mirrors in the shape of a parabolic trough to heat a fluid flowing through a pipe at its focus. The heated fluid then boils water, and the steam drives a turbine to generate power. Hence, the plant has electricity to run its control systems and pumps, and can use any excess to desalinate water for irrigating the plants. In summary, SFP allows food production in all 12 months of the year (3 crops) with half the fresh water usage than in comparable greenhouses. On the basis of the pilot success, SFP is now engaged in studies aimed at building a 20-hectare test facility near Aqaba in Jordan, large enough from the 1-hectare operation in Qatar to demonstrate a commercial enterprise.
Issues Involving Tourism and Food Exports
Tourism is popular in several Middle Eastern countries, particularly beach and coastal resorts in Egypt and Turkey. Tourism has been the major economy in Egypt for many years but can be threatened not only by civil unrest and terrorism but also by foodborne illness (Costa 2008). Tourists might not stop coming to Egypt due to a few reports of diarrhea; however, widespread reporting of severe cases, and lawsuits, will make tour operators much more selective, and bring pressure on the Egyptian hospitality industry to improve its hygienic standards. The greater challenge is for Egypt to ensure that it has the capacity to sustain a safe food supply for its own people. In doing so, it provides safe food for those who want to explore its rich history and seaside resort areas. Multiple reports of illness have been reported from Nile River cruises and a resort town on the coast. From September to November, 2008, 34 cases of hepatitis A imported from Egypt were reported to the German public health authorities (Bernard and Frank 2009). Investigations pointed to a continuing common source of infection, most likely linked to Nile river cruises. In addition, eight cases from France had been travelling on a Nile cruise and one on a Red Sea diving safari (Couturier et al. 2009). One specific cruise ship was mentioned by six of ten Belgian cases (Robesyn et al. 2009). Those who took a Nile cruise had typically done this in combination with a hotel stay. At least three different ships and three different hotel accommodations were mentioned in the travel histories of the French cases. The patients affected had not been vaccinated, which emphasized the need for more effective travel advice before trips to hepatitis A endemic countries (Sane et al. 2015). Possible sources of infection might have been contaminated food obtained from a common food catering company consumed onboard, contaminated tap water supplies for the ships’ bunkers, or a common exposure on shore (e.g., a restaurant where tourist groups from various ships were taken during day trips). As all of these ships continuously traveled up and down a short stretch of the river (Aswan to Luxor and back) with standard must-see stops along the way, the cases possibly shared an exposure on land. Both the long incubation period of hepatitis A (15–50 days) and long delays in collecting information on the individual cases precluded any rapid intervention on location. No specific food source was identified but it could have been juices as recognized in an earlier major outbreak. In 2004, tourists returning from Egypt included 351 hepatitis A case-patients from 9 European countries who were infected with a single HAV strain (genotype 1b) (Frank et al. 2007). The case-control study identified orange juice most likely contaminated during the manufacturing process, e.g., by an infected worker with inadequate hand hygiene or by contact of fruit or machinery with sewage-contaminated water. Citrus fruit and citrus juices have occasionally been implicated as vehicles of HAV and Salmonella infections, with contamination typically occurring during production, or preparation just before consumption. As HAV is resistant to acid, it likely can survive for prolonged periods in orange juice. It is also possible that leafy greens could contribute to foodborne illness in Egypt. An international study of contamination of 562 leafy green lettuce and spinach samples taken between 2011 and 2013 from 23 open-field farms in Belgium, Brazil, Egypt, Norway, and Spain showed that the Egyptian samples were the most contaminated at 55.6% (Liu et al. 2016). These authors claimed that temperature had a stronger influence than did management practices on E. coli presence and concentration. Region was a variable that masked many management variables, including rainwater, surface water, manure, inorganic fertilizer, and spray irrigation. Temperature, irrigation water type, fertilizer type, and irrigation method should be systematically considered in future studies of fresh produce safety.
Also in the spring of 2008, a young couple was ill with vomiting and abdominal cramps after their first meal at a Sharm El Sheikh 4-star hotel in the Egyptian coastal resort area, and they remained there in their bedrooms for the rest of their week (This is Staffordshire 2008). Both continued to have ongoing issues 6 months later, with one of them suffering from reactive arthritis. Other guests also complained about diarrhea. They stated that the food was disgusting; the meat was undercooked, the buffet was left out for long periods of time, with new food being piled on top of the old food, and there were flies landing on food items. In August 2014, a family stayed at a resort hotel, also in Sharm El Sheikh, and all suffered severe symptoms including diarrhea, stomach cramps, and vomiting. They were put into the hotel clinic given antibiotics and intravenous drips but had not completely recovered after they returned home (Galley 2014). At the time other guests were also ill. They noticed that the food including chicken and beef, appeared to be undercooked a couple of times, and that one of the chefs touched raw meat and then touched cooked meat without changing gloves. The booking company confirmed that “a very small number” of guests staying at the resort in 2014 reported that they had been unwell, “with symptoms similar to a virus”. The company said that guests were offered the appropriate support and advice by their overseas holiday advisors. It claimed that all of its hotels were subject to stringent monitoring and audits and this hotel achieved an extremely high score in its audit carried out in the summer of 2014. However, high audit scores do not necessarily correlate with day-to-day safe hygienic practices (Powell et al. 2013).
The popular beach resort of Sarigerme, Turkey, on the Aegean Sea also has had a reputation for gastroenteritis, with repeat problems of foodborne illness with British tourists on vacations organized by tour companies, although the actual hotels were different. In 2009, an outbreak of gastric illness at this resort led to £1.7 m paid out in compensation, with 595 people suffering from infections including Salmonella, Cryptosporidium, Campylobacter and E. coli (Hutchison 2015). In September, 2012, hundreds of British holidaymakers suffered from salmonellosis after returning from a hotel complex in Sarigerme (Disley 2012). Final figures may have been close to 1000, and several were hospitalized. In October 2014, the Swannell family had booked a week’s stay at the First Choice Holiday Village resort in Sarigerme, when Mark Swannell, 46, fell seriously ill a few days into the break with diarrhea, abdominal pain, nausea and lethargy (Hutchison 2015). He said that some of the food he was served at the hotel had been undercooked, with some chicken bloody in the middle, food was not served at the correct temperature, food was left uncovered for prolonged periods of time, and the same food had been served more than once. The family stated that cutlery, crockery and table linen used in the restaurant was not up to standard, and they saw cats in the public areas of the hotel and in the restaurant. Legal action was taken.
In addition to ill tourists in Middle Eastern countries, contaminated exported food can affect those abroad, as illustrated in the following U.S. outbreak. From March to August 2013, of 165 patients identified with hepatitis A in ten states, 69 (42%) were admitted to hospital, two developed fulminant hepatitis, and one needed a liver transplant, but none died (Collier et al. 2014). Almost all cases reported consuming pomegranate arils (seeds) from one retail chain. Hepatitis A virus genotype IB, uncommon in the Americas, was recovered from specimens from 117 people with hepatitis A virus illness. Pomegranate frozen arils imported from Turkey were identified as the vehicle early in the investigation by combining epidemiology, genetic analysis of patient samples, and product tracing. The product was then removed from store shelves, the public warned not to eat the seeds, recalls took place, and post-exposure prophylaxis with both hepatitis A virus vaccine and immunoglobulin was provided. This investigation showed that modern public health actions can help rapidly detect and control hepatitis A virus illness caused by imported food. Egyptian trade has also been adversely affected by exports. In 2013, there were three outbreaks of hepatitis A sickening 400 persons in 16 European countries. In the first report in April, 106 persons in four Scandinavian countries were infected with hepatitis A (Andrews 2014). Epidemiological investigations traced those cases to frozen strawberries grown in Egypt and Morocco, though no strawberries were found to be positive for HAV. The second outbreak in April was larger in extent with 107 ill in 14 countries, all having recently visited Egypt, and the outbreak strain of the virus had the same subgenotype as the first outbreak associated with strawberries. An epidemiological investigation into the second outbreak suggested the likely source was strawberries or another fruit distributed to hotels in Egypt. The third outbreak was reported in Germany in May, after nine Germans were infected with hepatitis A after traveling to Italy. This third outbreak infected about 200 Italian residents, as well as nine Germans, one Dutch traveler and five Polish travelers; 21 Irish residents with no travel history to Italy were infected by the same strain of the virus. Separate investigations in Italy and Ireland both implicated imported frozen mixed berries as the source, with most of those berries coming from Eastern Europe. It is not known if these berries came from other regions, such as Egypt, or were local to Eastern Europe. Contributing factors to the larger number ill was lack of vaccination. Because HAV infections were declining in Europe over the last few decades, fewer people had developed antibodies to repel the virus. Couple that with the fact that hepatitis A was not on the vaccination schedule for citizens of many of the countries affected, and the result was a highly susceptible population. Also, most of the European travelers to Egypt were not advised to get hepatitis A vaccinations when staying in all-inclusive resorts, which were attracting an increasing number of Europeans traveling to Egypt. Further, the investigators believe contamination of the berries occurred early in the food production chain. Investigators suspect that irrigation water contaminated with sewage water likely contaminated the strawberries in the two outbreaks connected to Egypt. But the contamination might have also been caused by infected workers in the field or the processing facility, or by contaminated water sprayed on the berries sometime before distribution. The outbreaks indicate that fresh and frozen berries are efficient vehicles of HAV infection, as previously demonstrated in the US and elsewhere (Palumbo et al. 2013). European authorities agreed that “the 2013 experience demonstrated the absolute necessity for extensive collaboration between countries and between the public health and food sectors to identify as quickly as possible the vehicle of infection and, ideally, to control the outbreak in a timely fashion.”
A more serious outbreak damaged Egypt’s food export trade. In July 2011, the European Union (EU) banned the import of certain Egyptian seeds and beans till at least October following an official report that a single batch of Egyptian fenugreek seeds probably caused two European outbreaks of E. coli infections responsible for 4211 ill persons and at least 50 deaths. A task force of health officials set up by the European Food Safety Authority (EFSA) reported that one lot of fenugreek seeds imported from Egypt was the most likely common link between the two outbreaks in northern Germany and in Bordeaux, France (Anderson 2011). Both were traced back a year and a half to a shipment of 33,000 pounds (15,000 kg) of fenugreek seeds, that was loaded onto a ship at the Egyptian port of Damietta on November 24, 2009. On the ship’s arrival at Antwerp, Belgium, the seeds were barged to Rotterdam to clear customs. The sealed container was trucked into Germany to an unidentified importer, who resold most of the lot. An unidentified German company then resold about 150 pounds of the seeds to the German sprouter, which is believed to be the source of the sprouts that caused the extensive German outbreak. The German importer also sold about 800 pounds of sprout seed to the English company Thompson & Morgan, which repackaged the seeds into 1.75-ounce (50 grams) packages. Those packages were shipped to a French distributor, who resold the seeds to about 200 garden centers around France. Investigators believe that one of those packets was the source of the second European outbreak with 16 cases in the Bordeaux area. Because the seeds were likely contaminated with E. coli O104:H4 at some point before leaving the importer, and more contaminated seeds could be in circulation, it was deemed appropriate to consider all lots of fenugreek from the Egyptian exporter as suspect. Soil contact or animal or human fecal contamination of the seeds likely occurred during their production or distribution in Egypt. Even a negative laboratory test of those seeds could not be interpreted as proof that a batch was not contaminated. Trace-forward findings indicate the German importer sold seeds from the suspected lot to 70 companies, and the shelf life of the seed can be up to 5 years.
By mid-October, 2011, the European Commission (EC) lifted import restrictions on fresh and chilled podded peas and green beans and other fresh produce from Egypt, but the ban on Egyptian seeds and sprouts, scheduled to expire on October 31, was to be extended until the end of March, 2012, following an “unsatisfactory audit” of seed producers in Egypt (News Desk 2011). The extended ban involved arugula sprouts, leguminous vegetable sprouts (fresh or chilled), soy bean sprouts, dried (shelled) leguminous vegetables, fenugreek seeds, soy beans and mustard seeds. The EC audit showed that measures taken by the Egyptian authorities to address shortcomings in the production of seeds that may be sprouted for human consumption were not sufficient “to tackle the identified risks.” Those shortcomings were not seen in the growing and processing sites for fresh peas and beans, and therefore those vegetables were no longer considered a food safety risk.
There is no need for actual illnesses to occur to affect trade. Recalls, seizures, and bans can be employed by importing countries if standards are not met, and force exporting countries like Egypt to take action. For instance, in 1999 the EC suspended the import of peanuts from Egypt due to the presence of aflatoxin in concentrations in excess of maximum levels specified in EU regulations (Technical Cooperation Department 2003). Egypt is a major peanut exporting country and the European markets then accounted for 68% of its peanut exports. This decision was repealed on 1 December 1999 and was replaced by another Decision, which imposed a requirement for certification to accompany every consignment and required systematic analysis of consignments and documentation by the importing member state. Under this system only 18 Egyptian exporters were allowed to ship to the EU. In August 2003, the 1999 Decision was replaced by another Decision that required the competent authorities in EU Member States to undertake random sampling and analysis of 20% only of peanut consignments from Egypt for aflatoxin B1 and total aflatoxins. This improvement came as a result of the efforts that the Egyptian Government put in complying with the requirements of the EU. To this end, the Egyptian Ministries of Agriculture and Land Reclamation (MALR) and Ministry of Foreign Trade (MOFT) issued Ministerial Decree No. 2/2000, which covered all stages of production, processing, sampling and exporting of peanuts. The main provisions of the decree were:
-
exported peanuts must be produced, inspected and prepared according to set scientific procedures; and exporters who violate the rules would be suspended for 1 year;
The decree also established the legal limit for aflatoxin in peanuts in both the domestic and EU export markets. In the Egyptian domestic market, the legal limit was 5 mg/kg aflatoxin B1 and 10 mg/kg total aflatoxin content. For the EU market, the legal limits were 2 mg/kg aflatoxin B1 and 4 mg/kg total aflatoxin content. In addition, the decree specified the sampling procedures that must be followed for export certification. In September of 2001 the Food and Veterinary Office sent a mission to Egypt to assess Egypt’s compliance with its certification system requirements. A number of recommendations on steps Egypt should take to improve the control system of foodstuffs intended for export to the EU were made. In response, the Egyptian authorities declared that they were taking actions to address the Mission’s recommendation. But to achieve that there was a need to coordinate among a number of Egyptian agencies involved in the production and export of peanuts and aflatoxin control: MALR, The Central Administration for Plant Quarantine (CAPQ), The Agricultural Research Center (ARC), The Ministry of Foreign Trade (MOFT), and The Customs Service. Also a laboratory capable of testing for mycotoxins was necessary. Alongside this; Egypt had technical assistance from international organizations in order to build human and physical capacities necessary for achieving compliance. The action by the EU forces Egypt to improve the safety of its peanut production which would be beneficial both to Europeans and to all who eat products made from Egyptian peanuts, including the domestic consumers.
Lebanon used to be a tourist haven but is less today because of a seemingly dysfunctional government following a civil war. The country produces food for both the domestic and overseas markets. Unfortunately, some exported food has caused illnesses and recalls. Twenty-three cases of Salmonella Bovismorbificans in eight states and in the District of Columbia (Washington, D. C.) from August to November, were linked epidemiologically to hummus eaten at three Mediterranean-style restaurants in the D. C. area, all owned by the same individual (Goetz 2012). Although samples collected from all ingredients used to make the hummus tested negative for any Salmonella, the hummus was recalled and the outbreak ceased. During its investigation of the restaurants, the D.C. Department of Health discovered multiple food safety violations at the establishments, including inadequate food temperature control, insufficient hand washing, and the presence of pests and insects, which had to be corrected. It is not clear if any abusive temperature conditions could have allowed growth of the Salmonella in the hummus. The public was not notified because by the time the hummus had been withdrawn from the market, there were no further cases. However, the contaminated ingredient in the hummus was not discovered until May, 2012, when a traceback by the U.S. Food and Drug Administration (FDA) revealed that the tahini used to make the hummus in one of the restaurants had recently been associated with recalls in Canada for contamination with S. Cubana (September 2011) and S. Senftenberg (February 2012). All tahini linked to these outbreaks had been imported from the same company in Lebanon. The FDA then mandated that all tahini products coming from this Lebanese company be tested for Salmonella before entering the U.S. and has recommended that U.S. and Canadian officials partner to inspect the tahini manufacturing plant. This was the first time S. Bovismorbificans had been implicated in a tahini outbreak in the U.S. As a result of this outbreak, the author stated it is important for public health officials and consumers to be informed that products made with imported sesame paste have been shown to be associated with Salmonella outbreaks and that they should be considered as possible sources for foodborne illness in the future. In fact, contaminated sesame seed paste was in the news a few days before a CDC report on the outbreak was made public, after a supply of contaminated tahini was stolen from a California importer’s warehouse, where it was being stored because a sample had tested positive for Salmonella. The tahini, which had also been imported from Lebanon but from a different manufacturer, was awaiting destruction, and the FDA warned the public that the stolen, potentially contaminated tahini may be on the market. Lebanese tahini has been implicated in several outbreaks in the past and subject to recalls (Harris et al. 2015).
Government Oversight of the Food Industry
Government oversight of the food industry is variable across the region with many regulations stemming back to colonial days, but modernization changes are gradually being considered or implemented. Unfortunately, where some Middle Eastern countries are slowly moving forward to improve food safety, others are slipping back in their oversight because of conflict and lower public health priorities. There are relatively few large food processing operations except those managed by multi-national companies, and most of the government oversight is on SMEs particularly small foodservice outlets. The states in the Gulf Cooperation Council (GCC), each have an aggressive food safety policy but do not always follow identical approaches, some of which are well-established and some of which are innovative. The KSA has had a food inspection system in place for many years with reports of outbreaks published regularly, though no doubt it could be improved with more cooperation between the Ministry of Health, the municipalities and the Saudi Food and Drug Authority (SFDA). The SFDA was established under the Council of Ministers resolution no (1) dated January 1, 2003, as an independent body that directly reports to the Prime Minister (El Sheikha 2015). The SFDA is responsible to regulate, oversee, and control food, drug, medical devices, as well as set mandatory standard specifications thereof, whether they are imported or locally manufactured. The control and/or testing activities can be conducted at the SFDA or any other agency’s laboratories. Moreover, the SFDA is in charge of consumers’ awareness on all matters related to food, drug and medical devices and associated other products and supplies. The SFDA has to negotiate with the MOH their mutual responsibilities following specific foodborne disease instances or consumer complaints.
Bahrain claims to have one of the more advanced food control systems in the region. In July 2008, as ambient temperatures heated up, the Ministry of Heath urged people to make sure the food they consume is properly stored during the summer months to avoid microbial growth and risk of food poisoning, e.g., keeping meat and fish at ≤4°C and to cook food thoroughly (Haider 2008). The Ministry was aware that both visitors and locals want to eat safe food, especially as Bahrain is moving towards more tourism with people are eating out more often. The Ministry ordered shops to provide appropriate storage facilities, e.g., coolers and refrigerators, for food as part of its efforts to protect the public’s health. Inspectors were checking food stalls, ice-cream parlors and vegetable shops to ensure that customers were not being sold contaminated or rotten products. The Ministry claimed to thoroughly investigate any complaints it receives, and to facilitate this a new hotline number was launched by the Ministry for general public to report food contamination complaints against supermarkets, restaurants, coffee shops and hotels. Specific advice for consumers included: being careful when buying salads; fruits and vegetables should be washed thoroughly before they are consumed; and dairy products such as milk, cheese and eggs, should always be refrigerated, since microorganisms grow faster in these products. The Ministry claimed that Bahrain has one of the best food control methods and food safety records in the region, and could even act in the future as a consultant in this field for other countries, including other GCC states. By 2015, government oversight had stepped up. In April, the Ministry of Health warned people against buying food advertised on social media or sold on the street by unlicensed retailers in Bahrain, either made in people’s homes or by street hawkers (Anonymous 2015c). The Ministry stated that control of these home operations is difficult if someone suffers from food poisoning since inspectors are not allowed to go into homes. Many homes sell food without a license and some would-be entrepreneurs even have barns where they slaughter livestock and market the meat illegally. There were 54,968 inspection visits conducted in 2014 by 25 inspectors from the Food Safety and Licenses group, which closed 41 of around 7000 registered outlets. Inspections cover imported food from ports right up to where it reaches restaurants and food outlets; 71,886 visits revealed around 883,584 tonnes of imported food were permitted for consumption, but 1873 tonnes were considered as non-consumable (rejected), during the same period. One of the more recent important programs is the Smart Inspection Project launched in April 2012. Inspectors, many with Masters and PhD degrees, visit restaurants and coffee shops to take food samples, as well as explain to staff how to store food and ensure its safety (Anonymous 2015c). It includes awarding food outlets that achieve a 100% food safety standard a blue sticker, while those meeting 80% of standards get a green sticker. Outlets that fail to achieve basic standards are warned with a red sticker. The total number of outlets assessed between August 2013 and February 2015 was 241; 17 were presented with blue stickers, 174 with green stickers and 50 with red stickers. This project features daily inspections and is focused on small food outlets, some of which have caused food poisoning in the past. Inspection visits depend on the hygiene of each outlet and the complaints received about them; some require two or more visits annually. High-level restaurants already have certified inspectors for evaluation and most of them require only one visit per year. The Ministry’s ultimate goal through this project is to decrease cases of foodborne disease, particularly important as Bahrain is increasing its tourism efforts and, thus, ensuring food safety is essential. To support the Ministry’s initiatives, live demonstrations on food safety practices were promoted in kitchens in hypermarkets. However, if red sticker facilities fail to take advantage of educational material, they may be punished for neglecting food safety standards and guidelines though public prosecution.
In a bid to improve standards of hygiene in restaurants, Qatar’s Supreme Council of Health (SCH) increased the number of spot checks on food outlets and has launched a hotline for residents to report food poisoning (Walker 2014). The council is responsible for monitoring food establishments and implementing Qatar’s food laws along with the Ministry of Municipality and Urban Planning (MMUP/Baladiya). The SCH embarked on an intensive inspection campaign, collecting food samples from all restaurants and food outlets in the country including suppliers. The inspection teams, which include specialized doctors from the SCH’s communicable diseases department and the environmental health inspection department, also medically check workers responsible for preparing food to ensure they are not carrying infections. Those found to be handling food in an unhygienic way would be immediately dismissed. Following a hotline complaint call, a report is filed, a team from the SCH visits the affected people, then inspects the related food outlet and collects samples for laboratory examination. The latest crackdown was in response to the illness of a family of four which suffered food poisoning after eating chicken, rice and salad at a popular Turkish restaurant which was closed down because a medical report prepared by the SCH’s environmental health section confirmed that the outlet served contaminated food and violated health regulations. Tests conducted in the Central Food Laboratory at SCH found three types of bacteria causing diseases in food served by the restaurant. Medical tests on the victims also showed that they were infected by the same bacteria, as well as one of the restaurant workers. Another popular Turkish restaurant was closed for 2 months after it was found that several customers were treated in the hospital for food poisoning symptoms including intense nausea, vomiting and diarrhea. As part of the SCH’s new campaign, experts would undertake community awareness drives, and organize seminars and training sessions about food contamination to improve understanding among owners and workers in food establishments. Other closures occurred because of serving food with moldy ingredients, rotten vegetables in the kitchen, insects in pasta, and generally violating the provisions of the food law. The MMUP increased the number of spot-checks and naming and shaming erring establishments on its website in Arabic. The 2014 amendments to the food law gave greater powers to authorities to fine and close down venues that break the law including temporarily closing down establishments if it has violated food safety and hygiene regulations, and also has the power to recommend severe penalties. A follow up to one of these closed Doha Turkish restaurants was after a trial when five staff were each been handed fines, jail sentences and deportation orders after they were found guilty of causing food poisoning to approximately 20 customers ill with vomiting, nausea and diarrhea (Santacruz 2015). The restaurant was accused of serving spoiled and unsafe food on October, 2014. An affected pregnant woman gave birth to her baby 2 months prematurely. The manager of the restaurant was fined approximately $2500 and sentenced to spend 3 months in jail while three other staff members were each fined approximately $2000 and sentenced to 1 month in jail. During an inspection it was found that another staff member did not hold the necessary health certificate and was subsequently fined approximately $1800 and also sentenced to 1 month in jail. As well as the staff members being sentenced to jail and fined, the Court of Environmental Misdemeanours also found that the restaurant itself was guilty of causing the food poisoning outbreak, and issued the restaurant with approximately $8100 in fines and ordered it closed for a further 3 months. In other parts of the world these penalties would seem unduly harsh, as it would be difficult for this restaurant ever to recover financially.
Coupled with education, there has been recent enforcement blitzes on food establishments such as hotels, restaurants and bakeries by Oman municipalities, and a leading bakery in Muscat was closed down because of rats in the premises in late December, 2015 (Staff 2015). This led food safety experts and the public to call for stricter rules and heftier fines to be imposed after surprise checks conducted by the Muscat Municipality, especially when it was disclosed that nearly half the restaurants in the Bausher area were not following food safety standards. Surprise inspections by the Muscat Municipality at 125 restaurants in Bausher found that around 53 restaurants did not meet food safety standards and were violating rules formulated by the municipality. Also, in the same time frame, Ibri Municipality officials were forced to shut down 42 commercial shops and they destroyed more than 3000 km of outdated food in 2015. According to the Municipality’s officials, 698 health violation letters were issued throughout the year, as well as 541 warnings were issued to different institutions operating in the wilayat of Ibri.
There are no easily-accessible reports on government oversight in Pakistan and inspection actions are more likely to be released to the public through the Press. In 2015, the Islamabad Capital Territory (ICT), Administration conducted a drive against adulterated food items with unannounced inspections of food outlets in different markets and imposed fines amounting to Rs110,000 (about US$1000) on owners for unhygienic conditions at their premises including restaurants, cafes, bakers, candy (sweet) stores, and a hotel was sealed (APP 2015). Cleanliness conditions at the outlets’ kitchens were found unsatisfactory and unhygienic while workers had not been vaccinated against viral diseases. Some business owners were also paying less to their workers in contravention of the minimum wages act. Business owners were directed to improve cleanliness conditions and ensure food safety standards failing which strict action would be taken against them. A cattle market was also ordered to “beef up” its security. Punjab, Pakistan’s most populous province, has a population that is more than double that of California, and Lahore, the provincial capital, has a vast array of food outlets. From the available Press reports, the Punjab Food Authority (PFA) has a mixed record of oversight of food operations. A PFA team visited the Polo Ground restaurant at the Race Ground Park and found expired food, blocked sinks and unhygienic conditions in the kitchen and food storage area in contrast to the claimed high quality standards by the management of the supposedly high-class restaurant (Raza 2015). The team faced resistance from the management but it managed to enter the kitchen for inspection. PFA officials said the kitchen condition was similar to that of an ordinary road-side eatery, dispelling general perception that restaurants serving the elite follow higher standards of hygiene and food safety. However, the PFA in Lahore had received a complaint that an assistant food safety officer had received Rs50,000 (about US$475) bribe from the restaurant owner so he could keep his restaurant open (Anonymous 2015d). Another restaurant on Peco Road sealed by the PFA for poor hygiene and unsanitary conditions of its workers in the second week of March, was opened for business the very next day. Typically, according to the PFA’s standard operating procedure (SOP), a restaurant sealed for the first time may resume business after a week. At the end of the week, the proprietor has to submit an affidavit assuring the authority that all problems pointed out by the food safety officer had been taken care of prior to reopening it for business. The PFA Director General (DG) had constituted a three-member committee to probe the complaint of bribery but it was later shelved. Similar situations occurred when restaurants that had reopened before the stipulated period for closure had expired. In the first week of 2015, a restaurant was fined Rs25,000 (about US$240) for unhygienic conditions and lack of soaps in the workers’ washrooms, instead of following the PFA SOPs of sealing the premises. The SOPs regarding duration of closure and required permission from the PFA DG were stated to be flouted openly. However, a PFA spokesperson denied any wrongdoing, and the SOP was being observed to the letter. She said a written permission from the DG used to be mandatory in order to de-seal restaurants, but now an operations deputy director can also issue permission for it. She also stated that the restaurant on Peco Road had not reopened on orders of the PFA; its owner had de-sealed it illegally. These reports indicate that there may be some illegal activities including bribery by inspectors but miscommunication on how much leeway inspection staff have on prevention and control practices may be more of the issue.
In mid-2015 Ayesha Mumtaz became the new operations director of the PFA, tasked with ensuring food in Punjab is unadulterated and safe (Reeves 2015). Her self-declared war on unhygienic food generated so much publicity in the last 6 months that she became a household name in Pakistan. Mumtaz says many food producers know nothing about hygiene but are willing to learn. There’s also a hardened mafia who are only interested in profit, she says. Everyone in the street seems to know about Mumtaz. Storekeepers begin shooing away customers, hauling down the shutters, and heading into the shadows in the hope that Mumtaz’s scrutinizing eye will not fall on them. These traders would sooner lose business than risk a visit from a woman whose campaign to clean up the kitchens and food factories of Pakistan has made her a national celebrity. She declared that the PFA cannot allow them to get away with their “perverse” activities and to “play havoc” with the lives of the people. Consumers are unaware that the cakes and sweets that they buy over the counter are produced amid unhygienic conditions. She has found spoons encrusted with filth, fly-blown cans of gooey liquid lying around haphazardly, dirty containers, grimy rags and rusty tin cans, moldy scraps of cake, all involved in making cakes and sweets to be sold to the public. Civil servants in Pakistan are often accused of being lazy and corrupt. Mumtaz is being feted as a rare example of a government official who actually champions the public’s rights. She and her inspectors have so far raided more than 13,000 businesses, and Pakistanis seem to approve. Her fans call Mumtaz the Fearless One. Hundreds of thousands have clicked like on the PFA’s Facebook page in appreciation of her work. There was a very famous hotel in the heart of Lahore that she inspected and found the chiller where they keep all the foods together (vegetables with chicken, meat), but also a big rat; this became big news for the public. However, there are complaints that she does her raids with police and cameras to be broadcast nationally even before the owners are convicted, according to the Lahore Restaurant Association.
In 2011, the Abu Dhabi Food Control Authority (ADFCA) planned to check all food handlers by 2012. The Authority’s emirate food safety training (EFST) program, started in 2008, provides basic training in food hygiene and safety to those who work in food outlets (Olarte 2011). According to the ADFCA, small catering businesses in most countries have the lowest standards of food safety, and most workers in Abu Dhabi’s 2500 small restaurants are illiterate and do not speak fluent Arabic or English, making it a challenge for them to understand and follow safety guidelines and regulations; 69% of managers and 73% food handlers in the capital speak South Asian languages such as Urdu, Hindi and Malayalam (Pennington 2014). The training is now offered in four languages — English, Arabic, Urdu and Malayalam — which the majority of food service personnel speak, and covers basic food hygiene issues including staff hygiene, food temperature, cross-contamination, cleaning and sterilization. To help them understand and follow food-safety rules, the ADFCA is using photographs to teach employees how to handle food safely according to international standards. The scheme is an extension of a pilot involving 600 small restaurants carried out in 2012–2014. As part of the efforts to ensure retention of their learning, the ADFCA conducted spot checks at 94 food outlets in Marina and Khalidiya Malls, and gave guidance and advice to staff for those with violations, rather than just penalizing them, the normal practice in most Middle Eastern countries. The field operations manager at the ADFCA noted that the differing cultures, education and languages are the barriers that sometimes hinder food handlers from carrying out what they are trained to do. He recommends that supervisors should quiz them on hygienic and safety issues so that they know how to properly prepare and serve food. Those who have learning difficulty or are illiterate are given assistance through illustrations, in order to make it through the lessons and pass the examination. One of the critical elements of food safety that the ADFCA has to monitor and ensure, is that food handlers are aware of cold ready-to-eat food being kept at 4°C, while hot food should be kept and served very hot > 60°C. The ADFCA categorizes the food premises and carries out inspections based on their risk factors — high, medium and low. Restaurants and hypermarkets belong to the high-risk group; warehouses to the medium risk; while groceries, honey shops and vegetable and fruit outlets are considered low risk.
Recently, the establishment of the Egyptian Food Safety Authority was initiated by the Minister of Trade and Industry, with the support of the Ministry of Health and the Ministry of Agriculture. It would be responsible for food safety and consumer protection through the provision of sound data and guidance to deal with processed or genetically modified food in accordance with food safety standards (Anonymous 2012b). The strategic plan for the new draft law includes a revision of all Egyptian laws and legislation that deal with food safety since 1893, including around 2446 other legislations. The authority would need to apply food safety standards on imported food the same way it does for locally produced foodstuffs. Adopting the draft law would in effect cancel all existing laws and create one food safety law for the country. The Food Safety Authority plans to monitor the foods consumed by Egyptians of different age groups as a basis for where to put resources. Another issue to be faced is that studies in Egypt based on US statistics have revealed that the cost of food spoilage costs the country 144 million Egyptian pounds annually. The Chamber of Food Industries indicated that a unified body for food safety to apply international quality specifications and unite regulators was lacking. This reduced the competitiveness of local products, especially since most foreign countries do not recognize Egyptian regulations. It was hoped that investors in food industries would bring in new investments to the sector in the upcoming period if a Food Safety Authority were to be established, as per a ministerial decision issued in 2011. The Food Safety Authority has received several approvals from governments that ruled during the 4-year period following the revolution, but apparently nothing has been yet finalized until recently (Mefreh and Saeed 2015).
In a similar way to Egypt, the Lebanese government has been debating a new law on food safety for many years but unlike Egypt, it has yet to make much progress. Lack of agreement at the parliamentary level has resulted in different ministries (Health, Agriculture, Industry, Environment, Tourism) taking action as they see fit. The latest was in November 2014, when the Minister of Health conducted an extensive campaign of inspections in Lebanese establishments and naming of facilities that did not meet the Ministry’s expectations (Naylor 2014). The minister personally revealed that numerous supermarkets, bakeries, butchers and restaurants had been violating food safety and sanitation standards. They shut down slaughterhouses, restaurants, supermarkets and other retailers selling contaminated food. For instance, changes needed to be made for the slaughterhouse to conform to health standards; the report said livestock must be hanged during slaughter and not laid on the ground and that the abattoir should also be equipped with refrigerators and storage units for separate types of meat and their cuts. However, discord among ministries is apparent with the tourism minister trying play down the publicity of the health minister’s food safety blitzes by saying “We are in favor of full transparency, but we feel like we were ‘deceived’ because the food safety situation in Lebanon is good and better than other countries. We apologize to tourists, but more importantly, any of the Ministry of Health staff is ready to apologize to the Lebanese citizens for the public sector’s failures throughout the years?” (Yaliban 2014). Foodborne disease surveillance is limited in Lebanon and cannot be used to indicate the actual level of foodborne illnesses in the country. Lebanese food exports are also being required to conform to international standards. Tahini made from sesame seed paste is a major food export to the West, but recalls of tahini manufactured in Lebanon because of Salmonella contamination are more frequent than they should be; one recent example was a Health Hazard Alert for Certain Clic, Al Nakhil and Al Koura brand Tahina products that may have contained Salmonella, Recall/advisory dated August 16, 2013 posted from Canadian Food Inspection Agency [also see tahini/hummus linked illnesses under Foodborne disease in specific countries]. Under the new US Food and Drug Administration Food Safety Modernization Act, foreign companies importing foods to the US must demonstrate that they have the operational plans and facilities sufficient to produce safe food before they can ship any product to the US (FDA 2015), which is causing some concern among Lebanese tahini manufacturers and government agencies. Thus, although there is knowledge about foodborne disease and other food safety issues within government, industry and academia, the political inertia means that many foodborne illnesses will continue to occur but not be properly reported or know what factors were present to cause the outbreaks. Industry currently is taking the lead; apart from companies promoting food safety like Boecker and GWR Food Safety, MENA Food Safety Associates (MEFOSA) (http://www.mefosa.com/), based in Beirut, assists MENA companies hone their competitive edge by establishing and verifying procedures and practices that ensure quality, wholesome and safe products through consulting, auditing and training services in HACCP, GMPs, and hygienic practices.
However, Lebanon’s lack of a coordinated system of government oversight of the food industry pales into insignificance compared to that in Syria. Prior to the war, Syria’s healthcare system had hospital and doctor levels equivalent to other middle-income countries such as Brazil, Turkey and China, with life expectancy of 76 years, and most of the disease burden being similar to that in the West with non-communicable diseases, but four years of violence have changed all of that. Child vaccination levels dropped from 90% pre-conflict to 50% in March 2014 (Templeton 2015). As a result, outbreaks of diseases that had long been under control have spread across the land and into neighboring countries: hepatitis, measles, leishmaniasis, multi-drug-resistant tuberculosis, typhoid and even polio, which had not been seen in the Middle East for 20 years. Life expectancy has dropped by two decades. Medical personnel are clearly targeted because they are seen as potential enemies helping the opposite side. The majority of Syria’s doctors have been killed or fled the country (>700 medical workers have been killed since 2011). The situation has been called the worst humanitarian catastrophe this century, and the worst concerted attack on healthcare in living memory. At least 300,000 Syrians have been killed and more than 11 million others have been forced from their homes since the conflict began on March 15, 2011, with over four million people in areas that are hard to reach for humanitarian aid, and 4·5 million have fled mostly to neighboring Turkey, Lebanon, Jordan, and northern Iraq, while others have sought safety in Europe, provoking a political crisis in the 28-member bloc (Devi 2016).
Another Middle Eastern country under stress but with less publicity is Yemen. Currently there is little government oversight into food as there is little to be had. The situation in Yemen is characterized by large-scale displacement, civil conflict, food insecurity, high food prices, endemic poverty, diminishing resources, and movement of refugees and migrants (WFP 2016). The UN World Food Programme (WFP) has been in Yemen since 1967. In 2014, WFP conducted a Comprehensive Food Security Survey which found that 41% of the people (10.6 million) were food insecure, of which some five million were severely food insecure, meaning they were unable to buy or produce the food they need to survive. The organization’s protracted relief and recovery operation (PRRO), aims to reach six million people between mid-2014 and mid-2016 with 366,734 metric tons of food and US$74.5 million in cash and vouchers at an overall cost of US$491 million. If the conflict continues, this goal is unlikely to be met in time since both the airport and shipping port are areas being fought over. The WFP has been attempting to bring in relief supplies but cannot do so under fire, which means that only small amounts are occasionally delivered to the country (Mukhashaf and Miles 2015). One example of this occurred in Aden on July 20, 2015 when a ship docked after waiting a month to unload enough U.N. food aid to feed 180,000 people for a month. Previous repeated attempts to send ships to Aden were been blocked due to severe fighting in the port area. The PRRO is aligning WFP’s activities with moves to increase the Government’s capacity to respond to the crisis and will promote recovery and resilience to enable food insecure households and communities to better withstand and recover from the effects of conflict and shocks.
Discussion and Conclusions
There are many similarities as well as substantial differences in the descriptions of issues concerning food safety and foodborne disease of each country in the region. Gastrointestinal diseases are frequent throughout the Middle East with some countries identifying their etiologies, such as Egypt, Kuwait, Israel, Pakistan, Turkey, Yemen. These include bacteria and parasites, e.g., Salmonella, Shigella, Campylobacter, enterotoxigenic E. coli (ETEC), Giardia, Entamoeba, and occasionally enteric viruses such as HAV and norovirus. However, none of the countries has a well-functioning foodborne disease surveillance system, but a few report on a regular basis like KSA, and starting recently, Lebanon with PulseNet. Mostly it seems that only large outbreaks or ones with fatalities that are reported on, and mainly through the Press. These outbreaks are often related to point sources which are in most cases communal foods prepared for a large number of individuals as in feasts, student hostels, schools, campuses, or military camps. However, the actual etiological agents and the factors contributing to outbreaks are only rarely determined. One example is a very large outbreak in Bahrain in 2002 with at least 750 people suffering from foodborne illness after eating contaminated egg-and-mayonnaise sandwiches served at a wedding party, but the etiology was not determined, even though clinical specimens and food samples were analyzed, at least in a publically-released report (ProMED-MENA 2002). Based on the type of preparation including the length of time taken for preparation of the implicated food and the time from consumption to the appearance of symptoms of foodborne illness, the types of symptoms, and what has already occurred historically in foodborne disease outbreaks, possible agents can be surmised, such as Bacillus cereus and staphylococcal enterotoxins, and Salmonella, Shigella, or norovirus infections, but ProMED is continually asking for more information once an outbreak is announced, and hardly ever receiving it (ProMED-MENA 2014). All this indicates that even if clinical specimens or food samples are taken and analyzed, laboratories are only rarely able to determine an etiologic agent, or at least report on their results. Most agents described with the little information available seem similar in all the MENA countries and to those encountered in the West. However, a few pathogens are more likely to be restricted to a few nations, such polio in Pakistan, cholera in Iraq, MERS-CoV in KSA, and botulism in Egypt and Iran where river fish are often eaten (one case of infant botulism was diagnosed in Israel but it is a rare disease anywhere); the first two are more likely transmitted though water or poor hygienic conditions, the third by camels, and only botulism exclusively through food. Brucellosis is widespread in the Middle East but only a few country studies indicate its link to meat or dairy products. Much of the Middle East is in the throes of conflict which results in unique situations in specific countries to exacerbate foodborne disease or food poisonings; these include relief agencies supplying “stale” food to those trapped and starving by the Syrian civil war, almost lack of food at all in Yemen, deliberate poisonings of enemies in Afghanistan, Syria and Iraq, accidental pesticide poisonings in Iran, preventing unsafe food being sold to those on the Hajj in KSA, improperly prepared catered food for foreign troops in bases in Afghanistan, Iraq, Kuwait, KSA, and Turkey. Countries where tourism is a major source of income can be adversely affected by bad publicity over complaints over food served in resorts, such as in Egypt and Turkey. Also, Gulf countries tend to employ workers from India and other surrounding territories, and these are typically housed in camps or separate communities from citizens and visitors, and are transported to work sites and back; conditions are not always conducive to safe food, and outbreaks are occasionally reported either from their work sites or their overnight residences where meals are prepared or catered. Most food to many of these countries is imported, especially those with limited agricultural land and adequate water supplies; fruits and fresh vegetables, tend to be grown in rural or peri-urban settings for local consumption and these can be contaminated at source through polluted river or well water, such as in the Bekaa Valley of Lebanon and mountain communities in Pakistan, and the Nile, Tigris and Euphrates fluvial plains. On one occasion, Iranian watermelons were recalled and future sales banned in KSA, Qatar, and UAE because they were suspected of being poisoned or were injected with pesticides (nobody claimed to be ill after eating the melons), because holes were found in a few of them. However, the rationale of Iranian farmers deliberately losing money seems to counter this argument, and it is more likely a sectarian economic barrier (Abdullah 2015). In fact, with the temporary ban the price of watermelons went up in the countries that had banned them. Random tests carried out on the fruit confirmed they were free from any chemical substances, insecticides or other pollutants. The holes were most likely caused by emerging insect pupae. Countries outside the Gulf region reported no problems with the imported Iranian melons.
Where some processed foods are exported, there is a risk of the importing countries recalling these if they cause foodborne illnesses or contaminants are found in them. This has happened in Egypt with hepatitis A virus in strawberries and E. coli O104:H4 in fenugreek seeds causing serious illnesses in Europe and restricting further trade for an extended period. The same issue affected Turkish pomegranate arils and Lebanese tahini (made from imported ground sesame seeds), both containing Salmonella, exported to the US. Large to medium operations for broiler chickens and egg layers in KSA, Kuwait, Lebanon and other countries try and meet national standards or international guidelines for Salmonella but are not always achieved, resulting in recalls and fines. Governments are also aware of increasing concern over Campylobacter in chickens, as widely-eaten poultry is a major source of this pathogen, but campylobacteriosis is not often cited as causing foodborne disease. Raw milk (cow, sheep and camel) and raw milk cheese are still widely consumed in the Middle East at the local level, though not usually obtained through supermarkets, and the risk of infections is high, as it is in other parts of the world, but with the added concern of Brucella spp. and MERS CoV (the latter in the Gulf countries where camels are bred and milked), both serious pathogens. Yoghurt, surprisingly since it is acidic and is a source of gut beneficial lactobacilli, apparently was the foodborne vehicle to cause illnesses and deaths in Afghanistan, Israel, and Pakistan. No agent was found in any of the samples. In the Afghani example, the yoghurt was claimed to be deliberately poisoned; in the Israeli one, it was apparently “stale” given to Palestinian prisoners; there were two episodes in Pakistan, one was from a home-prepared meal and the other from a restaurant which served rice and yoghurt.
For prevention and controls strategies, most countries seem to rely on local authorities (municipalities) to do inspection of food facilities, more typically restaurants than processing plants as there are far more of them. Illegal sales for unapproved products by local entrepreneurs are sometimes an issue, e.g., home-slaughtered meat in Bahrain, and Palestinians shipping food to Israel. These illegal operations probably occur more often in porous borders within the region, and are only recognized when authorities decide to become vigilant in this area. Some countries have conducted research and surveys much more than others based on the publication record, e.g., Egypt, Israel, Palestine, KSA, Turkey, and to a lesser extent, Iran, Lebanon, Pakistan, UAE, and Yemen, but some research may occur without formal publication in recognized journals, making it difficult to have a true picture of how food safety problems are recognized and controlled. A few surveys have shown that home makers and food employees have limited knowledge of food safety, as in other regions. Thus, some agencies or industry associations, sometimes in collaboration with outside organizations like FAO or WHO, have attempted to train food employees in basic HACCP principles, including best hand hygiene practices, and speakers give the latest food safety issues at the annual Dubai International Food Safety Conference, now in its 10th year.
A few governments have established food safety agencies that have broad powers to inspect and control without overlapping responsibilities; these include Jordan and KSA with food and drug administrations, UAE with Abu Dhabi and Dubai food control authorities, Oman with its National Food Quality and Safety Centre, and Pakistan with a Punjab Food Authority. Egypt and Lebanon are initiating food safety authorities. Israel, Palestine and Jordan have a cross-border agreement to collaborate on food safety issues. Typical of many food control agencies in developing countries, periodic campaigns are launched to “crack down” on foodservice operations and sometimes processing plants. These are usually stimulated by complaints of the public, or the need for the responsible ministry to be seen doing something to justify its existence in compliance with regulations (if they exist). This has occurred recently in Lebanon, Qatar and Pakistan. One issue is that poorly constructed or out-of-date regulations may be interpreted in different ways by the owners and the agencies (Kullab 2014). If a violation is found, the facility may be fined and/or temporarily closed down until it has satisfied the inspectors at the next visit. In one extreme instance in Qatar, the owners and employees, were fined, imprisoned and deported. Unfortunately, although the names of those at fault are often publicized by the media, their specific violations and how they relate to the regulations are not usually documented or at least publically released. Another issue is that whether illnesses are suspected or not following a complaint, inspectors often insist that all food be discarded as soon as a sufficient violation, which may be unrelated to the complaint, has been determined; this prevents any samples being taken for outbreak investigations (Hanna et al. 2009), as well as using the outbreak for a teaching tool for the owner and other similar operations.
In conclusion, some progress has been made in the surveillance of foodborne disease in the Middle East, but the disease’s health and economic burden is barely being considered in many countries for future decision-making policies, an issue that is being tackled at the global level (WHO 2015b). Food control agencies seem to be trying to stop apparent abuses but have limited resources to do much more. This region, in particular, is severely strained because of sectarian distrust, on-going civil wars, and terrorist attacks, with refugees from Iraq seeking shelter toward Europe but stalled in Turkey and Lebanon for long periods of time. The crisis in Syria is considered the greatest humanitarian disaster of the twenty first century, or even since World War II, and it looks like the on-going fighting including outside armed forces will make food insecurity in the affected countries even worse in the foreseeable future. Less public attention has been directed to Yemen where food insecurity is a major concern. This coupled with Gulf countries losing their wealth over low oil prices and a resultant stagnant global economy means a focus on food safety will likely become lower in priority for many of these countries. Since secure food has to be safe, as illustrated by “stale” food being issued to besieged Syrian residents and prisoners, it is important that relief agencies and countries themselves be aware of the risk of foodborne diseases associated with immunocompromised persons, particularly children. However, even in countries where the food supply is acceptable, inadequate hygienic practices put the local and tourist population at risk of illness and exported foods jeopardize industry profits and a poor reputation for future trade. As demonstrated by KSA, Jordan and UAE, single agencies or multiple agencies with clear-cut roles responsible for food safety, should be pursued by governments in consultation with industry and academia. Duplication creates ambiguities for enforcement and education strategies as well as being unnecessarily costly. Water supplies are also critical and some governments are weaning away farmers from depleted groundwater aquifers, and making irrigation more efficient where there are sustainable supplies. Water for irrigation and processing has to be both free of pathogens and unacceptable levels of chemicals, and effectively treated waste water can substitute for groundwater. The Sahara Forest Project in Qatar is one example of a very dry country using seawater resources effectively; an even larger project is being considered from the 1-hectare in Qatar to a 20-hectare test facility in Jordan (Clery 2013). All these issues are being compounded by climate change and expected higher temperatures in already arid lands, which will make the region all the more dependent on more expensive imported foods. Gulf counties have enough petro-dollars to afford these, but other countries are struggling to be self-sufficient for the near future even if the fighting ceases. The repair to destroyed infrastructure will be immense, coupled with the lack of trained personnel to create a restored food system at all levels from primary production through food processing, foodservice, and retail to the home.
References
Abdelateef, N. (2011). Antimicrobial resistance for enteric pathogens isolated from acute gastroenteritis patients in Gaza strip, Palestine. Thesis. The Islamic University – Gaza. Available at: http://library.iugaza.edu.ps/thesis/95584.pdf. Accessed 14 Dec 2015.
Abdou, N. E., Al-Batel, M. K., El-Azazy, O. M., Sami, A. M., & Majeed, Q. A. (2013). Enteric protozoan parasites in stray cats in Kuwait with special references to toxoplasmosis and risk factors affecting its occurrence. Journal of the Egyptian Society of Parasitology, 43(2), 303–314.
Abdullah, A. (2015, May 4). Sale of watermelons with holes stopped in UAE. Khaleej Times. Available at: http://www.khaleejtimes.com/nation/general/sale-of-watermelons-with-holes-stopped-in-uae. Accessed 12 Mar 2016.
Afanasieva, D., Miles, T., & Karouny, M. (2015, October 30). U.N. causes food-poisoning with deliveries of old, ‘moldy’ biscuits to Syria, says rights body. Reuters. Available at: http://www.reuters.com/article/us-mideast-crisis-syria-aid-idUSKCN0SO24L20151030. Accessed 20 Jan 2016.
Agence France-Presse. (2015, October 20). Iraq cholera cases grow, spread to Kurdish region. Relief Web. Available at: http://reliefweb.int/report/iraq/iraq-cholera-cases-grow-spread-kurdish-region. Accessed 30 Dec 2015.
Ahmad, M. A., Khan, B. A., Shamsuddin, Z. A., & Anwarullah, M. (1989). Presence of Aflatoxin B1 in the shelled peanuts in Karachi. Pakistan Journal of Scientific and Industrial Research, 32, 526–527.
Ahmed, M. (2013.) Incidence and distribution of Salmonella serogroups in some local food in Sana’a – Yemen. Al-Nasser University, Yemen. Available at: http://journals.sfu.ca/alnasseru/index.php/alnasseru/article/view/2. Accessed 5 Jan 2016.
Ahmed, S. F., Klena, J. D., Mostafa, M., Dogantemur, J., Middleton, T., Hanson, J., & Sebeny, P. J. (2012, May 11). Viral gastroenteritis associated with Genogroup II norovirus among U.S. military personnel in Turkey, 2009. PLoS One.DOI: 10.1371/journal.pone.0035791. Accessed 21 Dec 2015.
Akbar, J. (2015, July 09). 45 ISIS fighters killed by poisoned Ramadan meal. Daily Mail Online. Available at: http://www.dailymail.co.uk/news/article-3153194/45-ISIS-fighters-die-eating-poisoned-Ramadan-meal-Iraq.html. Accessed 30 Dec 2015.
Akhtar, S. (2015). Food safety challenges—a Pakistan’s perspective. Critical Reviews in Food Science and Nutrition, 55(2), 219–226.
Al Awaidy, S. A., Bawikar, S., Al Busaidy, S., Baqiani, S., Al Abedani, I.,Varghese, R., Abdoan, H. S., Al Abdoon, H., Bhatnagar, S., Al Hasini, K. S., Mohan, P., Shah, S., Elamir, E., Klena, J., Ahmed, S. F., Teleb, N., Parashar, U., & Patel, M. M. 2009. Considerations for introduction of a rotavirus vaccine in Oman: Rotavirus disease and economic burden. Journal of Infectious Diseases, 200(Suppl. 1), S248–S253.
AlHayat. (2015, March 25). Foodborne illness – Saudi Arabia: (Najran) restaurant. Archive Number: 20150330.3265029. ProMED-MENA . Available at: http://www.promedmail.org/post/20150330.3265029. Accessed 25 Jan 2016.
Aligi, I. (2010, September 07). 250 flood victims suffer food poisoning. The Daily Times. Available at: http://archives.dailytimes.com.pk/karachi/07-Sep-2010/250-flood-victims-suffer-food-poisoning. Accessed on 24 Nov 2015.
Al-Joudi, A. S. 2007. An outbreak of foodborne diarrheal illness among soldiers in mina during Hajj: The role of consumer food handling behaviors. Journal of Family and Community Medicine.14(1): 29–33.
Aljoudi, A. S., Al-Mazam, A., & Choudhry, A. J. (2010). Outbreak of food borne Salmonella among guests of a wedding ceremony: The role of cultural factors. Journal of Family and Community Medicine, 17(1), 29–34.
Al-Kandari, D., & Jukes, D. J. (2009). A situation analysis of the food control systems in Arab Gulf Cooperation Council (GCC) countries. Food Control, 20, 1112–1118.
Al-Mazrou, Y. Y. (2004). Food poisoning in Saudi Arabia. Potential for prevention? Saudi Medical Journal, 25(1), 11–14.
Anadolu Agency. (2015, May 01). Syrian migrants attack gendarmerie in southeastern Turkish tent city, five injured. Hurriyet Daily News. Available at: http://www.hurriyetdailynews.com/Default.aspx?pageID=238&nid=81827&NewsCatID=341. Accessed 29 Dec 2015.
Anderson, R. (2011, July 6). One Egyptian seed shipment: Two outbreaks. Food Safety News. Available at: http://www.foodsafetynews.com/2011/07/one-egyptian-seed-shipment-two-outbreaks/#.VldO3narSM8. Accessed 27 Nov 2015.
Andrews, J. (2014, November 05). What can we learn? Food Safety News. Available at: http://www.foodsafetynews.com/2014/11/europes-3-hep-a-outbreaks-from-2013-what-can-we-learn/#.VldPLXarSM8. Accessed 28 Nov 2015.
Anonymous. (2012a, April 03). Afghanistan: Militants ‘kill police by poisoning food’. BBC News . Available at: http://www.bbc.com/news/world-asia-17597797. Accessed 4 Feb 2016.
Anonymous. (2012b). New food safety law to come up in Egypt. Clean. Available at: http://www.cleanmiddleeast.ae/articles/18/new-food-safety-law-to-come-up-in-egypt.html. Accessed 13 Jan 2016.
Anonymous. (2012c, March 09). Pakistan-Minor dies of food poisoning. The News International. Available at: http://www.thenews.com.pk/article-38916-Minor-dies-of-food-poisoning. Accessed 24 Nov 2015.
Anonymous. (2012d). Pakistan – Over 50 nurses hospitalized after food poisoning. The News. Available at: http://www.thenews.com.pk/Todays-News-Over-50-nurses-hospitalised-after-food-poisoning-6-95733. Accessed 15 Mar 2016.
Anonymous. (2015a, October 04). MoH on cholera alert; two patients detected. IndiansinKuwait.com. Available at: http://www.indiansinkuwait.com/ShowArticle.aspx?ID=36788&SECTION=0. Accessed 2 Feb 2016.
Anonymous, (2015b, January 01). 150 ‘food poisoning’ cases at Al-Azhar dorms in Egypt’s Assiut. Ahramonline. Available at: http://english.ahram.org.eg/NewsContent/1/64/119286/Egypt/Politics-/-food-poisoning-cases-at-AlAzhar-dorms-in-Egypts-A.aspx. Accessed 27 Nov 2015.
Anonymous. (2015c, April 07). New alarm over ‘unhealthy’ food in Bahrain. Trade Arabia. Available at: http://www.tradearabia.com/news/HEAL_279164.html. Accessed 11 Mar 2016.
Anonymous, (2015d, April 25). New guidelines: Punjab Food Authority giving ‘unsanitary’ restaurants an easy time of it. Tribune Express. Available at: http://tribune.com.pk/story/875525/new-guidelines-punjab-food-authority-giving-unsanitary-restaurants-an-easy-time-of-it/. Accessed 25 Nov 2015.
Anwar, T., Ahmad, I., & Tahir, S. (2011). Determination of pesticide residues in fruits of Nawabshah district, Sindh, Pakistan. Pakistan Journal of Botany, 43, 1133–1139.
APP. (2015, January 13). Surprise inspections: Pakistan officials fine food outlets, seal hotel. Express Tribune. Available at: http://tribune.com.pk/story/820907/surprise-inspections-ict-officials-fine-food-outlets-seal-hotel/. Accessed 25 Nov 2015.
Arain, M. B., Kazi, T. G., Baig, J. A., Jamali, M. K., Afridi, H. I., Shah, A. Q., Jalbani, N. & Sarfraz, R. A. (2009). Determination of arsenic levels in lake water, sediment, and foodstuff from selected area of Sindh, Pakistan: Estimation of daily dietary intake. Food and Chemical Toxicology, 47, 242–248.
Asghar, M. (2014, April 03). Teenage boy, sister die of food poisoning. Dawn. Available at: https://www.dawn.com/news/1097361/teenage-boy-sister-die-of-food-poisoning. Accessed 25 Nov 2015.
Associated Press. (2013, April 03). Egypt students storm office of top al-Azhar cleric. The Record. Available at: http://www.therecord.com/news/world/article/911866--egyptian-students-angered-by-food-poisoning-outbreak-storm-cleric-s-office. Accessed 27 Nov 2015.
Baş, M., Ersun, A. Ş., & Kıvanç, G. (2006). The evaluation of food hygiene knowledge, attitudes, and practices of food handlers in food businesses in Turkey. Food Control, 17, 317–322.
Bender, D. (2014, May 28). Israeli Doctor’s bio-warfare serum saves infant from botulism death. Thealgemeiner. Available at: http://www.algemeiner.com/2014/05/28/israeli-doctors-bio-warfare-serum-saves-infant-from-botulism-death/#. Accessed 12 Dec 2015.
Bernard, H. & Frank, C. (2009). Cluster of hepatitis A cases among travellers returning from Egypt, Germany, September through November 2008. Euro Surveillance. 14(3).
Bostan, K., Aydın, A., & Ang, M. K. (2009). Prevalence and antibiotic susceptibility of thermophilic Campylobacter species on beef, mutton, and chicken carcasses in Istanbul, Turkey. Microbial Drug Resistance, 15(2), 143–149.
Brittin, H. C. (2010). The food and agriculture around the world handbook. New Jersey: Pearson Education.
CDC (US Centers for Disease Control and Prevention). (2014). Confirmed variant Creutzfeldt-Jakob Disease (variant CJD) case in Texas. Available at: http://www.cdc.gov/ncidod/dvrd/vcjd/other/confirmed-case-in-texas.htm. Accessed 20 Nov 2015.
Clery, D. (2013, November 7). Desert farming experiment yields first results. Science Magazine. Available at: http://news.sciencemag.org/asiapacific/2013/11/desert-farming-experiment-yields-first-results. Accessed 9 Feb 2016.
Cohen, D., Bassal, R., Goren, S., Rouach, T., Taran, D., Schemberg, B., Peled, N., Keness, Y., Ken-Dror, S., Vasilev, V., Nissan, I., Agmon, V., & Shohat, T. (2014). Recent trends in the epidemiology of shigellosis in Israel. Epidemiology and Infection, 142(12), 2583–2594.
Cohen, D., Gargouri, N., Ramlawi, A., Abdeen, Z., Belbesi, A., Al Hijawi, B., Haddadin, A., Sheikh Ali S., Al Shuaibi, N., Bassal, R., Yishai, R., Green, M. S. & Leventhal, A. (2010). A middle east subregional laboratory-based surveillance network on foodborne diseases established by Jordan, Israel, and the Palestinian Authority. Epidemiology and Infection, 138(10), 1443–1448.
Collier, M.G., Khudyakov, Y. E., Selvage, D., Adams-Cameron, M., Epson, E., Cronquist, A., Jervis, R. H., Lamba, K., Kimura, A. C., Sowadsky, R., Hassan, R., Park, S. Y., Garza, E., Elliott, A. J., Rotstein, D. S., Beal, J., Kuntz, T., Lance, S. E., Dreisch, R., Wise, M. E., Nelson, N. P., Suryaprasad, A., Drobeniuc, J., Holmberg, S. D., & Xu, F., for the Hepatitis A Outbreak Investigation Team. (2014). Outbreak of hepatitis A in the USA associated with frozen pomegranate arils imported from Turkey: An epidemiological case study. Lancet Infectious Diseases, 14(10), 976–981.
Costa, R. (2008). Food-borne Illness and its Effect on Tourism in Egypt. Food Safety and Environmental Health Blog. Available at: http://www.safefoodsblog.com/2008/11/articles/international-food-safety/foodborne-illness-and-its-effect-on-tourism-in-egypt/. Accessed 27 Nov 2015.
Couturier, E., Roque-Afonso, A. M., Letort, M. J., Dussaix, E., Vaillant, V., & de Valk. H. (2009). Cluster of cases of hepatitis A with a travel history to Egypt, September–November 2008, France. Euro Surveillance, 14(3): pii=19094. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19094. Accessed 15 Mar 2016.
Dashti, A. A., Jadaon, M. M., Habeeb, F., West, P. W., Panigrahi, D., & Amyes, S. G. (2008). Salmonella enterica Serotype typhi in Kuwait and its reduced susceptibility to ciprofloxacin. Journal of Chemotherapy, 20(3), 297–302.
Devi, S. (2016, March 12). Syria’s health crisis: 5 years on. Lancet, 387, 1042–1043. www.thelancet.com http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(16)00690-5.pdf. Accessed 11 Mar 2016.
Disley, J. (2012, September 09). British holidaymakers in Turkey hit by salmonella. Mirror. Available at: http://www.mirror.co.uk/news/uk-news/british-holidaymakers-in-turkey-hit-by-salmonella-335726. Accessed 27 Dec 2015.
El Sheikha, A. F. (2015). Food safety issues in Saudi Arabia. Nutrit ion and Food Technology , 1(1): doi http://dx.doi.org/10.16966/nftoa.103. Accessed 15 Mar 2016.
Elinav, H., Hershko-Klement, A., Valinsky, L., Jaffe, J., Wiseman, A., Shimon, H., Braun, E., Paitan, Y., Block, C., Sorek, R., & Nir-Paz, R. for the Israeli Listeria Study Group. 2014. Pregnancy-associated listeriosis: clinical characteristics and geospatial analysis of a 10-Year period in Israel. Clinical Infectious Diseases 59 (7): 953–961.
Fagbo, S. (2005, February 04). Food poisoning – Saudi Arabia (Jizan): Request for information. Archive Number: 20050204.0380. ProMED-MENA. Available at: http://promedmail.org/post/20050204.0380. Accessed 25 Jan 2016.
Faour-Klingbeil, D., Kuri, V., & Todd, E. C. D. (2015). Investigating a link of two different types of food business management to the food safety knowledge, attitudes and practices of food handlers in Beirut, Lebanon. Food Control, 55, 166–175.
Faour-Klingbeil, D., Murtada, M., Kuri, V., & Todd, E. C. D. (2016). Understanding the routes of contamination of ready-to-eat vegetables in the Middle East. Food Control, 62, 125–133. doi: http://dx.doi.org/10.1016/j.foodcont.2015.10.024. Accessed 15 Mar 2016.
FDA (US Food and Drug Administration). (2015). Making certain imported foods meet U.S. standards under FDA Food Safety Modernization Act. U.S. Food and Drug Administration, Washington, D. C. Available at: http://www.fda.gov/Food/GuidanceRegulation/FSMA/ucm257980.htm. Accessed 28 Jan 2016.
Frank, C., Walter, J., Muehlen, M., Jansen, A., van Treeck, U., Hauri A. M., Zoellner, I., Rakha, M., Hoehne, M., Hamouda, O., Schreier, E., & Stark, K. 2007. Major outbreak of hepatitis A associated with orange juice among tourists, Egypt, 2004. Emerging Infectious Diseases 13(1), 156–158. Available from http://wwwnc.cdc.gov/eid/article/13/1/06-0487. Accessed 15 Mar 2016.
Galley, J. (2014, November 10). Dream five-star holiday ‘ruined’ after family struck down by vomiting bug. Mirror. Available at: http://www.mirror.co.uk/news/world-news/dream-five-star-holiday-ruined-after-4604283. Accessed 27 Nov 2015.
Gee, C. (2014). A dozen ISIS fighters killed after chefs infiltrate camp and POISON terrorists’ lunch. Daily Mirror, 08 November. Available at: http://www.mirror.co.uk/news/world-news/dozen-isis-fighters-killed-after-4590573. Accessed 20 Jan 2016.
Goetz, G. (2012, November 29). CDC: Salmonella from tahini sickened 23 last year. Food Safety News. Available at: http://www.foodsafetynews.com/2012/11/government-reports-2011-salmonella-outbreak-linked-to-tahini/#.VqqcjvkrKM8. Accessed 28 Jan 2016.
Greig, J. D., Todd, E. C. D., Bartleson, C. A., & Michaels, B. (2007). Outbreaks where food workers have been implicated in the spread of foodborne disease. Part 1. Description of the problem, methods and agents involved. Journal of Food Protection, 70, 1752–1761.
Haider, A. (2008, July 19). Poisoning alert over improper food storage. Gulf Digital News (GDN Online). Available at: http://archives.gdnonline.com/NewsDetails.aspx?date=04/07/2015&storyid=223513. Accessed 6 Jan 2016.
Hanna, N. M., Adib, S. M., & Daoud, Z. (2009). Food-borne salmonella outbreak at a bank cafeteria: an investigation in an Arab country in transition. La Revue de Santé de la Méditerranée orientale, 15(2), 470–474.
Harris, L. J., Palumbo, M., Beuchat, L. R., & Danyluk, M. D. (2015). Outbreaks of foodborne illness associated with the consumption of tree nuts, peanuts, and sesame seeds. In Outbreaks from tree nuts, peanuts, and sesame seeds. Available at: http://ucfoodsafety.ucdavis.edu/Nuts_and_Nut_Pastes. Accessed 15 Mar 2016.
Hosseini, H., Reza, H., Tavakoli, H. R., Meshgi, M. A., Khaksar, R., Hosseini, M., & Khakpour, M. (2010). Survey of Clostridium botulinum toxins in Iranian traditional food products. Comparative Clinical Pathology, 19(3), 247–250.
Hussain, M. (2013, August 16). Deadly disease: two dead, over 300 affected in Kurram’s cholera outbreak. Express Tribune. Available at: http://tribune.com.pk/story/590683/deadly-disease-two-dead-over-300-affected-in-kurrams-cholera-outbreak/ Accessed 25 Nov 2015.
Hussain, I., & Anwar, J. (2008). A study on contamination of aflatoxin M1 in raw milk in the Punjab province of Pakistan. Food Control, 19, 393–395.
Hussain, I., Anwar, J., Asi, M. R., Munawar, M. A., & Kashif, M. (2010). Aflatoxin M1 contamination in milk from five dairy species in Pakistan. Journal of Food Protection, 21, 122–124.
Hutchison, J. (2015, January 14). ‘Blood in the chicken and cats around food’: Father-of-three hospitalised with severe gastric illness at SAME Turkish holiday resort where 595 fell ill in 2009. Online DailyMail. Available at: http://www.dailymail.co.uk/travel/travel_news/article-2909698/Blood-chicken-cats-food-Father-hospitalised-severe-gastric-illness-family-holiday-Turkish-resort-595-fell-ill-2009.html. Accessed on 30 Dec 2015.
Ians. (2011, January 28). Man dies after eating contaminated yoghurt. Gaea Times. Available at: http://health.gaeatimes.com/2011/01/28/man-dies-after-eating-contaminated-yoghurt-30264/. Accessed 24 Nov 2015.
Islam, S. (2011, May 23). Gastro epidemic: Rising temperatures turn stomachs. Express Tribune. Available at: http://tribune.com.pk/story/173943/gastro-epidemic-rising-temperatures-turn-stomachs/ Accessed 10 Feb 2016.
Jalbani, N., Kazi, T. G., Jamali, M. K., Arain, B. M., Afridi, H., & Baloch, A. (2007). Evaluation of aluminum contents in different bakery foods by electrothermal atomic absorption spectrometer. Journal of Food Composition and Analysis, 20(3–4), 226–231.
Javed, I., Jan, I. U., Muhammad, F., Rahman, Z. U., Khan, M. Z., Aslam, B., & Sultan, J. I. (2009). Heavy metal residues in the milk of cattle and goats during winter season. Bulletin of Environmental Contamination and Toxicology, 82, 616–620.
Kamel, A. H., Ali, M. A., El-Nady, H. G., de Rougemont, A., Pothier, P., & Belliot, G. (2009). Predominance and circulation of enteric viruses in the region of Greater Cairo, Egypt. Journal of Clinical Microbiology, 47, 1037–1045.
Kamel, A. H., Ali, M. A., El-Nady, H. G., Deraz, A., Aho, S., Pothier, P., & Belliot, G. (2011). Presence of enteric hepatitis viruses in the sewage and population of Greater Cairo. Clinical Microbiology and Infection, 17, 1182–1185.
Khan, S., Rehman, S., Khan, A. Z., Khan, M. A., & Shah, M. T. (2010). Soil and vegetables enrichment with heavy metals from geological sources in Gilgit, northern Pakistan. Ecotoxicology and Environmental Safety, 73, 1820–1827.
Khuri-Bulos, N. A., Khalaf, M. A., Shehabi, A., & Shami, K. (1994). Foodhandler-associated Salmonella outbreak in a university hospital despite routine surveillance cultures of kitchen employees. Infection Control and Hospital Epidemiology, 15, 311–314.
Kullab, S. (2014, April 19). Experts emphasize need for food safety measures after scandals. Daily Star. Available at: http://www.dailystar.com.lb/Article.aspx?id=253840&link=News/Lebanon-News/2014/Apr-19/253840-experts-emphasize-need-for-food-safety-measures-after-scandals.ashx. Accessed 27 Jan 2016.
Liu, C., Hofstra, N., & Franz, E. (2016). Impacts of climate and management variables on the contamination of preharvest leafy greens with Escherichia coli. Journal of Food Protection, 79(1), 17–29.
Luttfullah, G., & Hussain, A. (2011). Studies on contamination level of aflatoxins in some dried fruits and nuts of Pakistan. Food Control, 22, 426–429.
Mahmood, N. (2012, February 07). Pakistan- Food poisoning claims four lives. Pakistan Observer . Available at: http://pakobserver.net/detailnews.asp?id=139008, Accessed Nov 2015.
Martins, R. B., Hogg, T., & Otero, J. G. (2012). Food handlers’ knowledge on food hygiene: the case of a catering company in Portugal. Food Control, 23, 184–190.
Masriya, A. (2013, April 30). Egypt: Azhar’s food poisoning cases rise to 161 – MOH. AllAfrica. Available at: http://allafrica.com/stories/201305010321.html. Accessed 27 Nov 2015.
Masriya, A. (2014, October 22). Egypt: 178 cases of food poisoning in two Suez primary schools. AllAfrica. Available at: http://allafrica.com/stories/201410230249.html Accessed 27 Nov 2015.
Mayar, M. R. (2015, April 8). 20 cops suffered from diarrhea during Sehat Ka Insaaf drive. The Nation. Available at: http://nation.com.pk/national/08-Apr-2014/20-cops-suffered-from-diarrhea-during-sehat-ka-insaaf-drive. Accessed 25 Nov 2015.
Mefreh, M, & Saeed, S. (2015, October 08). Establishment of Food Safety Authority will allow investments in food industries. Daily News Egypt. Available at: http://www.dailynewsegypt.com/2015/10/08/establishment-of-food-safety-authority-will-allow-investments-in-food-industries/. Accessed 13 Jan 2016.
Memish, Z. A. (2010). The Hajj: communicable and non-communicable health hazards and current guidance for pilgrims. Eurosurveillance 15 (39). Available at: http://www.eurosurveillance.org/images/dynamic/EE/V15N39/art19671.pdf. Accessed 25 Jan 2016.
Memish, Z. A., & Al Rabeeah, A. A. (2011). Global perspectives for prevention of infectious diseases associated with mass gatherings. Lancet Infectious Diseases, 12, 66–74.
miss22. (2013, June 22). Qatar pursues water and food security. Global Risk Insights. Available at: http://globalriskinsights.com/2013/06/qatar-pursues-water-and-food-security/. Accessed 12 Jan 2016.
Mobeen, A. K., Aftab, A., Asif, A., & Zuzzer, A. S. (2011). Aflatoxins B1 and B2 contamination of peanut and peanut products and subsequent microwave detoxification. Journal of Pharmacy and Nutrition Science, 1, 1–31.
Modarres, S. (1997). A survey of Clostridium botulinum in food poisoning in Iran. Tehran University Medical Journal. 55(6):30–34. Available at: http://tumj.tums.ac.ir/browse.php?a_code=A-10-25-1610&slc_lang=en&sid=1. Accessed 10 Feb 2016.
MOPH (Ministry of Public Health). (2012). National Health Statistics Report in Lebanon. Beirut: Ministry of Public Health, Government of Lebanon. Available at: file:///C:/Users/Ewen/AppData/Local/Microsoft/Windows/INetCache/Content.Outlook/SRQ0M881/20120000_MoPH_National_Health_Statistics_Report_in_Lebanon.pdf. Accessed 15 Feb 2015.
Mughal, R. (2010, December 6) Hepatitis A spreading because of lack of awareness. Tribune. Available at: http://tribune.com.pk/story/86427/hepatitis-a-spreading-because-of-lack-of-awareness/ Accessed 25 Nov 2015.
Muhkalalati, G., & Kieke, S. (2015, October 26). Aid delivers food poisoning as residents’ immunity ‘extremely weak’. Syria:Direct. Available at: http://syriadirect.org/news/aid-delivers-food-poisoning-as-residents%E2%80%99-immunity-%E2%80%98extremely-weak%E2%80%99/. Accessed 20 Jan 2016.
Mukhashaf, M., & Miles, T. (2015, July 21). U.N. ship brings food aid to Yemen’s Aden as fighting rages. BBC News. Available at: http://www.bbc.com/news/world-middle-east-29319423. Accessed 14 Feb 2016.
Naylor, H. (2014, November 19). In food-crazed Lebanon, a war over tainted chicken and messed-up meze. The Washington Post. Available at: https://www.washingtonpost.com/world/middle_east/in-food-crazed-lebanon-a-war-over-tainted-chicken-and-messed-up-meze/2014/11/18/76a14136-6e7b-11e4-a2c2-478179fd0489_story.html. Accessed 15 Mar 2016.
News Desk. (2011, October 21). EU ban on Egyptian fenugreek seeds extended. Food Safety News, . Available at: http://www.foodsafetynews.com/2011/10/ban-on-egyptian-fenugreek-seeds-extended/#.Vli8T3arSM8. Accessed 27 Nov 2015.
Olarte, O. (2011, March 22). 86% of food handlers complete hygiene and safety training. Khaleej Times. Available at: http://www.khaleejtimes.com/article/20110322/ARTICLE/303229813/1002, Accessed 4 Dec 2015.
Osaili, T. M., Jamous, D. O., Jamous, A., Obeidat, B. A., Bawadi, H. A., Tayyem, R. F., & Subih, H. S. (2013). Food safety knowledge among food workers in restaurants in Jordan. Food Control, 31(1), 145–150.
Palumbo, M., Harris, L. J., & Danyluk, M. D. (2013). Survival of foodborne pathogens on berries. FSHN13–12, Food Science and Human Nutrition Department, UF/IFAS Extension, Gainesville, Florida. Available at: https://edis.ifas.ufl.edu/fs236. Accessed 15 Mar 2016.
Patel, P. K., Mercy, J., Shenoy, J., & Ashwini, B. (2008). Factors associated with acute diarrhoea in children in Dhahira, Oman: a hospital-based study. Eastern Mediterranean Health Journal, 14(3), 571–578.
Pennington, R. (2014). Abu Dhabi food authority provides clearer picture of safety rules in restaurants. The National UAE. Available at: http://www.thenational.ae/uae/abu-dhabi-food-authority-provides-clearer-picture-of-safetyrules-in-restaurants. Accessed 24 Dec 2016.
Powell, D. A., Erdozain, S., Dodd, S., Costa, R., Morley, K., & Chapman, B. J. (2013). Audits and inspections are never enough: A critique to enhance food safety. Food Control, 30(2), 686–691.
ProMED-MENA. (2002, July 2). Mass poisoning in Bahrain. Available at: http://promedmail.org/post/20020703.4663. Accessed 15 Mar 2016.
ProMED-MENA. (2011, November 02). Foodborne illness – Saudi Arabia: (Al Madinah), Hajj pilgrims. Archive Number: 20111102.3259. Available at: http://promedmail.org/post/20111102.3259. Accessed 25 Jan 2016.
ProMED-MENA. (2014). Foodborne illness – Egypt: (Suez) school children, milk susp, RFI. Editorial comments. Archive Number: 20141023.2891144. Available at: http://promedmail.org/post/20141023.2891144. Accessed 11 Feb 2016.
Qasim, M. (2009, July 20). NIH confirms cholera case in capital. News International. Available at: http://www.thenews.com.pk/TodaysPrintDetail.aspx?ID=188937&Cat=6&dt=7/20/2009. Accessed 25 Nov 2015.
Raza, A. (2015, April 3). Polo Ground eatery fined for expired food, lack of hygiene. The News International. Available at: http://www.thenews.com.pk/Todays-News-5-310414-Polo-Ground-eatery-fined-for-expired-food-lack-of-hygiene. Accessed 25 Nov 2015.
Reeves, P. (2015). Pakistan’s food safety czar declares ‘war’ on unhygienic food. NPR Salt Blog. Posted on December 29. Available at: http://www.npr.org/templates/transcript/transcript.php?storyId=459835645. Accessed 29 Dec 2015.
Reuters. (2016, January 26). After poisoning, rogue cop shoots dead 10 policemen in Afghanistan. Hindustani Times. Available at: http://www.hindustantimes.com/world/after-poisoning-rogue-cop-shoots-dead-10-policemen-in-afghanistan/story-rdRLBpczKFhRjJJerNoBxJ.html. Accessed 5 Feb 2016.
Robesyn, E., Micalessi, M. I., Quoilin, S., Naranjo, M., & Thomas, I. (2009). Cluster of hepatitis A cases among travellers returning from Egypt, Belgium, September through November 2008. Euro Surveillance, 14(3): pii=19095. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19095. Accessed 15 Mar 2016.
Saberi, M. & Scott, K. (2009, June 14). Dubai siblings die of suspected food poisoning. Gulf News. Available at: http://gulfnews.com/news/uae/general/dubai-siblings-die-of-suspected-food-poisoning-1.28846. Accessed 11 Mar 2016.
Sane, J., MacDonald, E., Vold. L., Gossner, C., Severi, E., on behalf of the International Outbreak Investigation Team. (2015). Multistate foodborne hepatitis A outbreak among European tourists returning from Egypt– need for reinforced vaccination recommendations, November 2012 to April 2013. Euro Surveillance, 20(4): pii=21018. Article DOI: http://dx.doi.org/10.2807/1560-7917.ES2015.20.4.21018. Accessed 15 Mar 2016.
Santacruz, S. (2015, May 14). Jail sentences and deportation for Qatar food poisoning. Australian Food Safety News. Available at: https://www.foodsafety.com.au/2015/05/jail-sentences-and-deportation-for-qatar-food-poisoning/. Accessed 12 Jan 2016.
Saseendran, S. (2014, January 31). 518 cases of food borne diseases recorded in Dubai. Khaleej Times. Available at: http://www.khaleejtimes.com/lifestyle/health-fitness/518-cases-of-food-borne-diseases-recorded-in-dubai. Accessed 11 Mar 2016.
Scallan, E., Hoekstra, R. M., Angulo, F. J., Tauxe, R. V., Widdowson, M.-A., Roy, S. L., Jones, J. L., & Griffin, P. M. 2011. Foodborne illness acquired in the United States—Major pathogens. Emerging Infectious Diseases, 17(1), 7–15.
Soomro, A. M., Seehar, G. M., Bhangar, M. I., & Channa, N. A. (2008). Insecticides in the blood samples of spray-workers at agriculture environment: The toxicological evaluation. Pakistan Journal of Analytical & Environmental Chemistry, 9, 32–37.
Sözen, H., Gönen, I., & Beydilli, H. (2014). An outbreak of norovirus gastroenteritis in a county in Turkey. Journal of Microbiology and Infectious Diseases, 4(1), 26–29.
Staff. (2013, July 16). Cholera claims five lives. Dawn. Available at: http://www.dawn.com/news/1029567/cholera-claims-five-lives. Accessed 25 Nov 2015.
Staff. (2015, December 30) Muscat municipality shuts down leading bakery in Ruwi. Times of Oman. Available at: http://foodsafety.einnews.com/article/304062229/7UuJiJ5FyCzvXi4j. Accessed 11 Jan 2016.
Tajkarimi, M., Ibrahim, S. A., & Fraser, A. M. (2013). Food safety challenges associated with traditional foods in Arabic speaking countries in the Middle East. Trends in Food Science and Technology, 29, 116–123.
Tanyeri-Abur, T., & Elamin, N. (2011). An Overview of International Investments in Agriculture in the Near East. Available at: http://www.fao.org/fileadmin/templates/est/INTERNATIONAL-TRADE/FDIs/Egy_Mor_Sud.pdf. Accessed 7 Feb 2016.
Tariq, M., Shahzad, A., & Ishtiaq, H. (2003). Pesticides in shallow groundwater of Bahawalnagar, Muzafargarh, D.G. Khan and Rajan Pur Districts of Punjab, Pakistan. Environment International, 30, 471–479.
Tavakoli, H. R., & Imani Fooladi, A. A. (2011). Determination of contamination with Clostridium botulinum in two species of processed and non-processed fish. [Article in Persian]. Journal of Gorgan University of Medical Sciences, 13(1), 79–87.
Technical Cooperation Department. (2003). “Regional Programmes for Food Security in the Near East: Towards Sustainable Food Security and Poverty Alleviation”, High-Level Technical Workshop, Executive Summary, Jeddah, 8–9 October 2003. Food and Agriculture Organization, Rome. Available at: http://www.fao.org/docrep/MEETING/007/AD388E/ad388e00.htm#TopOfPage. Accessed 4 Dec 2015.
Templeton, T. (2015, March 17). Syria’s shameful healthcare quagmire. New Internationalist Blog. Available at: http://newint.org/blog/2015/03/17/syria-healthcare/. Accessed 20 Jan 2016.
This is Staffordshire. (2008, November 8). Couple may take action on holiday nightmare sickness. The Sentinel. Available at: http://www.stokesentinel.co.uk/Couple-action-holiday-nightmare-sickness/story-12530636-detail/story.html. Accessed 27 Nov 2015.
Todd, E. C. D. (2001). Foodborne and waterborne disease in developing countries – Africa and the middle east. Dairy Food and Environmental Sanitation, 21(2), 110–122.
Todd, E. C. D., & Greig, J. D. (2015). Viruses of foodborne origin: a review. Virus Adaptation and Treatment, 7, 27–45.
Tucker, R, (2012, February 27). Afghan cops; food poisoning at border post. CBS News. Available at: http://www.cbsnews.com/news/afghan-cops-food-poisoning-at-border-post/. Accessed 4 Feb 2016.
Variyar, M. (2015, July 8). 45 Isis fighters die in ‘Iftar Poisoning’; 100 more ill after eating Ramadan meals in Mosul. International Business Times, India Edition. Available at: http://www.ibtimes.co.in/45-isis-fighters-die-iftar-poisoning-100-more-ill-after-eating-ramadan-meals-mosul-638488. Accessed on 20 Nov 2015.
Walker, L. (2014, December 1). Amid growing complaints, SCH launches food poisoning hotline in Qatar. Doha News. Available at: http://dohanews.co/amid-growing-complaints-sch-launches-food-poisoning-hotline-qatar/. Accessed 12 Jan 2016.
WFP (World Food Programme). (2016). Yemen: current issues and what the World Food Programme is doing. World Food Programme, Rome, Italy. Available at: https://www.wfp.org/countries/yemen. Accessed 14 Feb 2016.
WHO (World Health Organization). (2015a). WHO’s first ever global estimates of foodborne diseases find children under 5 account for almost one third of deaths. World Health Organization, Geneva. Available at: http://www.who.int/mediacentre/news/releases/2015/foodborne-disease-estimates/en/. Accessed 7 Feb 2016.
WHO (World Health Organization). (2015b).WHO estimates of the global burden of foodborne diseases. Foodborne diseases burden epidemiology reference group 2007–2015. World Health Organization, Geneva. Available at: http://apps.who.int/iris/bitstream/10665/199350/1/9789241565165_eng.pdf?ua=1. Accessed 9 Feb 2016.
Yaliban. (2014, November 18). Food scandal: Food poisoning rate in Lebanon lowest, says tourism minister. Yaliban Blog. Available at: http://yalibnan.com/2014/11/18/food-scandal-food-poisoning-rate-in-lebanon-lowest-says-tourism-minister/. Accessed 15 Mar 2016.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Todd, E.C.D. (2017). Foodborne Disease in the Middle East. In: Murad, S., Baydoun, E., Daghir, N. (eds) Water, Energy & Food Sustainability in the Middle East. Springer, Cham. https://doi.org/10.1007/978-3-319-48920-9_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-48920-9_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-48919-3
Online ISBN: 978-3-319-48920-9
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)