Abstract
An Ideal Care System should incorporate fundamental elements of control engineering, such as effective and data-driven sensing, computation, actuation, and feedback.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Take Home Messages-
An Ideal Care System should incorporate fundamental elements of control engineering, such as effective and data-driven sensing, computation, actuation, and feedback.
-
These systems must be carefully and intentionally designed to support clinical decision-making, rather than being allowed to evolve based on market pressures and user convenience.
This chapter presents ideas on how data could be systematically more effectively employed in a purposefully engineered healthcare system. We have previously written on potential components of such a system—e.g. dynamic clinical data mining, closing the loop on ICU data, optimizing the data system itself, crowdsourcing, etc., and will attempt to ‘pull it all together’ in this chapter, which we hope will inspire and encourage others to think about and move to create such a system [1–10]. Such a system, in theory, would support clinical workflow by [1] leveraging data to provide both accurate personalized, or ‘precision,’ care for individuals while ensuring optimal care at a population level; [2] providing coordination and communication among the users of the system; and [3] defining, tracking, and enhancing safety and quality. While health care is intrinsically heterogeneous at the level of individual patients, encounters, specialties, and clinical settings, we also propose some general systems-based solutions derived from contextually defined use cases. This chapter describes the fundamental infrastructure of an Ideal Care System (ICS) achieved through identifying, organizing, capturing, analyzing, utilizing and appropriately sharing the data.
1 Use Case Examples Based on Unavoidable Medical Heterogeneity
The intrinsic heterogeneities inherent in health care at the level of individual patients, encounters, specialties, and clinical settings has rendered the possibility of a single simple systems solution impossible. We anticipate requirements in an ICS of identifying common core elements that apply to the medical care of all patients (e.g. safety principles, preventive care, effective end of life care, accurate and up-to-date problem list and medication list management), and subsequently formulating pathways based on specific context. One should note that an individual patient can cross over multiple categories. Any complex outpatient will also have the baseline requirements of meeting objectives of an outpatient in good health and may at some point have an inpatient encounter. Table 4.1 identifies a variety of use cases including abbreviated forms of the pertinent clinical and data issues associated with them.
2 Clinical Workflow, Documentation, and Decisions
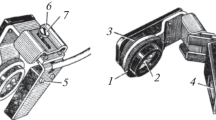
The digitalization of medicine has been proceeding with the wide adoption of electronic health records, thanks in part to meaningful use as part of the Health Information Technology for Economic and Clinical Health (HITECH) Act [11], but has received varying responses by clinicians. An extensive degree of digitalization is a fundamental element for creating an ICS. Defined at the highest level, a system is a collection of parts and functions (a.k.a. components and protocols) that accepts inputs and produces outputs [3]. In healthcare, the inputs are the patients in various states of health and disease, and the outputs are the outcomes of these patients. Figure 4.1 provides a simple control loop describing the configuration of a data driven health system.
Control loop depicting a data-driven care system. A clinical issue such as an infection or vascular occlusion affects the state of the patient. Subsequently, the system sensor detects this change and submits the relevant data to the computer for storage and analysis. This may or may not result in actuation of a clinical practice intervention that further affects the state of the patient, which feeds back into the system for further analysis. Feed-forward control involves the transmission of disturbances directly to the sensor without first affecting the state of the patient. The detection of a risk factor for venous thromboembolism that triggers prophylaxis in a protocol-based manner represents a clinical example of feed-forward control [3]
The practice of medicine has a long history of being data driven, with diagnostic medicine dating back to ancient times [12]. Doctors collect and assemble data from histories, physical exams, and a large variety of tests to formulate diagnoses, prognoses, and subsequent treatments. However, this process has not been optimal in the sense that these decisions, and the subsequent actuations based on these decisions, have been made in relative isolation. The decisions depend on the prior experience and current knowledge state of the involved clinician(s), which may or may not be based appropriately on supporting evidence. In addition, these decisions have, for the most part, not been tracked and measured to determine their impact on safety and quality. We have thereby lost much of what has been done that was good and failed to detect much of what was bad [1]. The digitization of medicine provides an opportunity to remedy these issues. In spite of the suboptimal usability of traditional paper documentation, the entries in physicians’ notes in natural language constitute the core data required to fuel an ideal care system. While data items such as lab values and raw physiological vital signs may be reasonably reliable and quantitative, they generally do not represent the decision-making and the diagnoses that are established or being considered, which are derived from the analysis and synthesis of the available data (the assessment with differential diagnosis) as well as the data to be acquired in the diagnostic workup (the plan).
The digitalization of medicine has encountered two key issues: [1] How does one develop a digitally based workflow that supports rapid, accurate documentation so that the clinician feels enlightened rather than burdened by the process? [2] How can the documentation process of data entry support and enhance the medical decision-making process? The first iteration of electronic health records (EHRs) has simply attempted to replicate the traditional paper documentation in a digital format. In order to address the first issue, smarter support of the documentation process will require innovative redesigns to improve the EHR as it evolves. Rather than requiring the clinician to sit at a keyboard facing away from a patient, the process needs to capture real-time input from the patient encounter in such potential modes as voice and visual recognition. This must be done so that the important details are captured without unduly interfering with personal interactions or without erroneous entries due to delayed recall. The receiving system must ‘consider’ the patient’s prior information in interpreting new inputs in order to accurately recognize and assimilate the essential information from the current encounter. Furthermore, the data that is collected should not be functionally lost as the patient advances through time and moves between geographic locales. A critical issue is one that has been perpetuated in the current practice of medicine from one encounter to another—the physician and patient should not need to ‘reinvent the informational wheel’ with every encounter. While each physician should provide a fresh approach to the patient, this should not require refreshing the patient’s entire medical story with each single encounter, wasting time and effort. Furthermore, what is documented should be transparent to the patient in contrast to the physician beneficence model that has been practiced for most of the history of medicine where it was considered beneficial to restrict patients’ access to their own records. Steps are being taken toward this goal of transparency with the patient with the OpenNotes movement that began in 2010. The effects of this movement are being recognized nationally with significant potential benefits in many areas relating to patient safety and quality of care [13].
Regarding the second issue, we have written of how quality data entry can support medical decision-making [14]. Future iterations of an innovatively redesigned EHR in an ideal care system should assist in the smart assembly and presentation of the data as well as presentation of decision support in the form of evidence and education. The decision-maker is then able to approach each encounter with the advantage of prior knowledge and supporting evidence longitudinally for the individual patient as well as comparisons of their states of health with patients with similar data and diagnoses (Fig. 4.2). Patterns and trends in the data can be recognized, particularly in the context of that patient’s prior medical history and evolving current state (Fig. 4.3).
Clinician documentation with fully integrated data systems support. Prior notes and data are input for future notes and decisions. The digital system analyzes input and displays suggested diagnoses and problem list, and then diagnostic test and treatment recommendations hierarchically based on various levels of evidence: CPG—clinical practice guidelines, UTD—Up to Date®, DCDM—Dynamic clinical data mining [14]
Mock screenshot for the Assessment screen with examples of background data analytics. Based on these analytics that are constantly being performed by the system and are updated as the user begins to enter a note, a series of problems are identified and suggested to the user by EMR display. After consideration of these suggestions in addition to their own analysis, the user can select or edit the problems that are suggested or input entirely new problems. The final selection of problems is considered with ongoing analytics for future assessments [14]
Population data should be leveraged to optimize decisions for individuals, with information from individual encounters captured, stored and utilized to support the care of others as we have described as ‘dynamic clinical data mining [2].’ This also is similar to what has been described as a ‘learning healthcare system’ or by a ‘green button’ for consulting such population data for decision support [15, 16].
In summary, an ICS must have tools (e.g. enhanced versions of current EHRs) to capture and utilize the data in ways that make documentation and decision-making effective and efficient rather than isolated and burdensome. While we realize that individual clinicians function brilliantly in spite of the technical and systems-level obstacles and inefficiencies with which they are faced, we have reached a point of necessity, one recognized by the Institute of Medicine threatening the quality and safety of healthcare, requiring the development of digital tools that facilitate necessary data input and decisions as well as tools that can interact with and incorporate other features of an integrated digitally-based ICS [17]. This will require close interactions and collaborations among health care workers, engineers including software and hardware experts, as well as patients, regulators, policymakers, vendors and hospital business and technical administrators [5].
3 Levels of Precision and Personalization
Many of the tools available to clinicians have become fantastically sophisticated, including technical devices and molecular biological and biochemical knowledge. However, other elements, including those used intensively on a daily basis, are more primitive and would be familiar to clinicians of the distant past. These elements include clinical data such as the heart rates and blood pressures recorded in a nursing flowsheet. Patient monitoring is not generally employed on a data driven basis, particularly decisions regarding who gets monitored with what particular signals, the duration of monitoring, and whether the data are stored, analyzed, and utilized beyond the current time. Furthermore, it is questionable whether the precedent of setting common numeric thresholds for abnormally high or low values extracts maximal clinical information from those signals. This recognition of abnormal values has become a significant problem of excessive false alarms and alarm fatigue [18]. Data analysis should provide clinicians with personalized and contextualized characterizations of individual vital signs (e.g. heart and respiratory rate variability patterns, subtle ECG waveform shapes, etc.) so that truly important changes can be recognized quickly and effectively while not overwhelming the cognitive load of the clinician. This would constitute ‘personalized data driven monitoring’ in which the raw data on the monitor screen is analyzed in real time to provide more information regarding the state of the patient. This will become more important and pressing as monitoring becomes more ubiquitous both in the hospital and in outpatient settings, which is not far from a reality with the exponential development of mobile health monitors and applications. A potential approach to this issue would be to treat monitors as specialized component of the EHR rather than standalone devices that display the heart rate and beep frequently, at times even when there is no good reason. In fact, this has occurred to some functional extent as monitors have become networked and in many cases can import data into the EHR. The loop will be closed when information flows bi-directionally so that the EHR (and other elements such as infusion pumps) can assist in providing clinical contexts and personalized information to enhance the performance potential of the monitors [14]. Whereas the user interface of the monitor is currently solely one of adjusting the monitored channels and the alarm settings, the user interface will also be increasingly rich so that the user could, for instance with the proper credentials, access, edit and annotate the EHR from a bedside or central monitor, or add information directly to the monitor to calibrate the monitoring process.
The data from monitors is beginning to be used for prospective analytic purposes in terms of predicting neonatal sepsis and post cardiac surgery problems [19, 20]. The HeRO neonatal alert focuses on diminution in heart rate variability and increase in decelerations to identify potential sepsis, whereas the Etiometry alert employs a sophisticated statistical analysis of those monitored elements reflecting cardiac function to detect and define problems earlier than humans could ordinarily do. The HeRO team is now working to develop predictive analytics for respiratory deterioration, significant hemorrhage, and sepsis in adults [21]. The essential point is that monitors employing such predictive analytics, as well as streaming and retrospective analytics, can leverage large amounts of personal data to improve the monitoring process as well as the healthcare encounter experience, particularly in areas of quality and safety. However, it is essential that such individual applications, exponentially growing in complexity and sophistication, not be introduced as unrelated bits into an already data-overburdened and under-engineered health care system. In the current state of the healthcare system, there is already plenty of data. However, it is not being systematically handled, utilized and leveraged. It is essential that such new applications be embedded thoughtfully into workflows. They must also be systematically interfaced and interoperable with the core care system, represented by the next generation of EHRs, so that the information can be used in a coordinated fashion, audited in terms of its impact on workflows, and tracked in terms of its impact on patient outcomes, quality, and safety. The addition of further system elements should be planned, monitored, and evaluated in a data-driven fashion. New elements should contribute to the system that uses data in a targeted, well-managed fashion rather than simply collecting it. The introduction of elements outside the core EHR requires communication and coordination among all system elements, just as effectively using the EHR alone requires communication and coordination among caregivers and patients.
4 Coordination, Communication, and Guidance Through the Clinical Labyrinth
Coordination and communication would be fundamental properties of an ICS contrasted with the enormous individual efforts required to achieve these goals in the current state. Patients and caregivers should be able to assume that the system captures, stores, and shares their information where and when it is needed. When the patient leaves her nursing home to be seen in a local emergency room or by her neurologist, the clinicians should have all previously available information necessary to treat her. This should also be the case when she returns to the nursing home with the system updating her record with events from her previous encounter as well as implementing new orders reflecting that encounter. This seamless communication and coordination is especially important for the kinds of patients who cannot provide this support themselves: people who are elderly, cognitively impaired, acutely ill, etc. Unfortunately, the current system was developed as a tool to aid in billing and reimbursement of interventions and the challenge that we face with transforming and continuing to develop it into an ICS is to transition its focus to patient care. Currently, patients and their advocates must battle with unrelenting challenges of opacity and obstruction facing immense frustration and threats to patient safety and quality of care where such risks would not be tolerated in any other industry.
Data and the efficient transmission of information where and when it is needed are at the core of an ICS. Information networks that permeate all the relevant locales must be created employing all the interoperability, privacy, and security features necessary. The system must maintain its focus on the patient and must instantly (or sufficiently quickly to meet clinical needs) update, synchronize, and transmit the information to all those who need to know, including qualified and permitted family members and the patients themselves relevant to the care of the patient. Many clinicians may be misinterpreted as being unresponsive, or even uncaring, in response to their continuing frustration with the difficulty of obtaining timely and accurate information. The current state of siloed healthcare systems makes obtaining information from other locales prohibitively challenging with no particular reward for continuing to struggle to obtain pertinent information for the continued care of patients, evoking reactions from caregivers including rudeness, neglect, hostility, or burnout. This challenge to obtain information from outside sources also leads to repeat diagnostic testing exposing patients to unnecessary risks and exposures such as is seen when a patient is transferred from one institution to another but the imaging obtained at the first institution is not able to be transferred appropriately [22]. Unfortunately, the Health Insurance Portability and Accountability Act of 1996 (HIPAA), the very legislation designed to enable the portability of information relevant to patient care, has further hindered this transmission of information. An efficient system of communication and coordination would benefit the caregiver experience in addition to the patients by providing them with the tools and information that they need to carry out their jobs.
The scope of those affected by the challenges inherent in the current healthcare system is broad. Not only does it affect those that are cognitively impaired, but also those with limited education or resources. It affects those that have complicated medical histories as well as those without previous histories. Even when patients are capable of contributing to the management of their own clinical data, there is potential to be overwhelmed and incapacitated through the complexities of the system when affected by illness, no matter the acuity, severity, or complexity. Interoperable EHRs focused on patients rather than locations or brands would provide the necessary and updated information as a patient moves from office A to hospital system B to home and back to emergency room C. When people are sick, they and their caregivers should be supported by the system rather than forced to battle it.
The sharing of data among patients and caregivers in a safe and efficient manner is not primarily a technical problem at this time, although there are many technical challenges to achieving such seamless interoperability. It is also a business as well as a political problem. This complex interaction can be seen in efforts toward healthcare architecture and standards supporting interoperability described in the JASON report, “A Robust Health Data Infrastructure” with responses from industry and EHR vendors in the development and adoption of HL7 Fast Healthcare Interoperability Resources (FHIR) standards [23, 24]. In an ICS, all parties must cooperate to interconnect EHRs among caregivers and locals so that the accurate and reliable data essential for healthcare can be coordinated, synchronized, and communicated across practice domains but within each patient’s domain. As we have seen on individual patient levels, an overabundance of data is not useful if it is not processed, analyzed, placed into the appropriate context, and available to the right people at the right places and times.
5 Safety and Quality in an ICS
There are many examples in healthcare, such as with bloodletting with leeches, where what was thought to be best practice, based on knowledge or evidence at the time, was later found to be harmful to patients. Our knowledge and its application must be in a continual state of assessment and re-assessment so that unreliable elements can be identified and action taken before, or at least minimal, harm is done [4]. There is currently no agreement on standard metrics for safety and quality in healthcare and we are not going to attempt to establish standard definitions in this chapter [25]. However, in order to discuss these issues, it is important to establish a common understanding of the terminologies and their meaning.
At a conceptual level, we conceive clinical safety as a strategic optimization problem in which the maximum level of permissible actuation must be considered and implemented in the simultaneous context of allowing the minimal degree of care-related harm. The objective is to design and implement a care system that minimizes safety risks to approach a goal of zero. The digitization of medicine affords a realistic chance of attaining this goal in an efficient and effective manner. The application of systems engineering principles also provides tools to design these kinds of systems.
The overall quality of healthcare is a summation of the experience of individuals, and for these individuals, there may be varying degrees of quality for different periods of their experience. Similar to safety, we also think of quality as a strategic optimization problem in which outcomes and benefits are maximized or optimized, while the costs and risks involved in the processes required to achieve them, are minimized. The provision of quality via optimized outcomes in clinical care is, to a large extent, a problem in engineering information reliability and flow, providing the best evidence at the right times to assist in making the best decisions [3]. The concepts of the ‘best evidence’ and ‘best decisions’ themselves depend on input sources that range from randomized control trials to informed expert opinion to local best practices. To provide actual actuation, information flows must be supplemented by chemical (medications), mechanical (surgery, physical therapy, injections, human touch) and electromagnetic (imaging, ultrasound, radiation therapy, human speech) modalities, which can institute the processes indicated by those information flows.
Furthermore, quality may also be defined with respect to the degree of success in treatment of the disease state. Diseases addressed in modern medicine are, to a surprisingly large and increasingly recognized extent, those of control problems in bioengineering [10]. These diseases may stem from control problems affecting inflammation, metabolism, physiological homeostasis, or the genome. However, these all represent failure in an element or elements of a normally well-controlled biological system. The quality of the clinical response to these failures is best improved by understanding them sufficiently and thoroughly enough so that targeted and tolerable treatments can be developed that control and/or eliminate the systems dysfunction represented by clinical disease. This should be accomplished in a way that minimizes undue costs in physical, mental, or even spiritual suffering. Ultimately, medical quality is based primarily on outcomes, but the nature of the processes leading to those outcomes must be considered. Optimal outcomes are desirable, but not at any cost, in the broad definition of the term. For example, prolonging life indefinitely is not an optimal outcome in some circumstances that are contextually defined by individual, family, and cultural preferences.
Having defined safety and quality in our context, the next step is to develop systems that capture, track and manage these concepts in retrospective, real-time, and predictive manners. It is only when we know precisely what static and dynamic elements of safety and quality we wish to ensure that we can design the systems to support these endeavors. These systems will involve the integration of hardware and software systems such as physiologic monitors with the EHR (including Computerized Provider Order Entry, Picture Archiving and Communication System, etc.), and will require a variety of specialized, domain-specific data analytics as well as technical innovations such as wireless body sensor networks to capture patient status in real time. The system will connect and communicate pertinent information among caregivers by populating standardized, essential access and alert nodes with timely and accurate information. It is also necessary that information flows bi-directionality (from the records of individuals to the population record, and from the population record to individuals) so that both can benefit from the data [2, 14]. Clearly, this will require an overall monitoring and information system that is interoperable, interactive both with its own components and its users, and actively but selectively informative. Future generations of clinicians will receive their education in an environment in which these systems are ubiquitous, selectively modifiable based on inputs such as crowdsourcing, and intrinsic to the tasks at hand, in contrast to the siloed and apparently arbitrarily imposed applications current clinicians may resist and resent [5, 8].
We noted the importance of control problems in disease, and control will also represent a fundamental component in the design of future safety and quality systems. The detection and prevention of adverse events is a significant challenge when depending on self-reporting methods or chart review and this issue is of high importance in the US [26, 27]. Predictive analytics can be developed as elements of the system to prospectively inform users of threats to safety and quality [19–21]. Carefully designed feed-forward components will inform participants in real time that an high risk activity is occurring so that it can be rectified without requiring retroactive analysis (Fig. 4.4—safety control loop below). Retrospective data analytics will track the factors affecting quality and safety so that practice, workflow, and technological systems can be accordingly modified. Such an ICS will be capable of monitoring medical errors, adverse events, regulatory and safety agency concerns and metrics, and compliance with best practice as well as meaningful use in parallel with costs and outcomes.
Control loop depicting a data-driven safety system. A clinical safety issue affects the state of the patient. Subsequently, the system sensor detects this change and submits the relevant data to the computer for storage and analysis. This may or may not result in actuation of a counteractive intervention that further affects the state of the patient, which feeds back into the system for further analysis. Feed-forward control involves the transmission of disturbances directly to the sensor without first affecting the state of the patient. An example of such a feed-forward control includes a faulty device or a biohazard
6 Conclusion
The basic systems solutions to the health care data problem rest on fully and inclusively addressing the axes of patient, care giver and care system considerations, which at times are apparently independent, but are ultimately interactive and interdependent. The required systems design will also greatly benefit from basic incorporation of the fundamental elements of control engineering such as effective and data-driven sensing, computation, actuation, and feedback. An Ideal Care System must be carefully and intentionally designed rather than allowed to evolve based on market pressures and user convenience.
The patient’s data should be accurate, complete, and up-to-date. As patients progress in time, their records must be properly and timely updated with new data while concurrently, old data are modified and/or deleted as the latter become irrelevant or no longer accurate. New entry pipelines such as patient-generated and remotely generated data, as well as genomic data, must be taken into consideration and planned for. These data should be securely, reliably, and easily accessible to the designated appropriate users including the patient. The caregiver should have access to these data via a well-designed application that positively supports the clinical documentation process and includes reasonable and necessary decision support modalities reflecting best evidence, historical data of similar cases in the population, as well as the patient’s own longitudinal data. All should have access to the data so far as it is utilized to construct the current and historical patterns of safety and quality. In addition to the data of individuals, access to the data of populations is required for the above purposes as well as to provide effective interventions in emergency situations such as epidemics. The creation of this kind of multimodal systems solution (Fig. 4.5—Ideal Care System Architecture below) will require the input of a great variety of experts including those from the EHR, monitoring devices, data storage, and data analytic industries along with leaders in healthcare legislation, policy makers, regulation, and administration.
Information Architecture of an Ideal Care System. This diagram integrates the concepts described in this chapter depicting data driven care systems, safety systems, along with connection and coordination of patient data across multiple modalities to achieve an Ideal Care System. Patients move through time and interact with the ICS in different contexts. Parallel databases are integrated with the patient data states in time including an individual patient’s longitudinal database, hospital quality and safety database, and a population database. Data from the patient, mobile technologies and from the home care entities keep caregivers informed of the most current patient data state
Many important engineering, economic, and political questions remain that are not addressed in this chapter. What and who will provide the infrastructure and who will pay for it? Will this kind of system continue to work with current hardware and software or require fundamental upgrades to function at the required level of reliability and security? How and where will the controls be embedded in the system? For example, will they be at the individual smart monitoring level or at a statewide public health level? How will the metadata obtained be handled for the good of individuals and populations? It is critical that the addition of new modalities and devices be fully integrated into the system rather than adding standalone components that may contribute more complexity and confusion than benefit. These goals will require cooperation previously unseen among real and potential competitors and those who have previously been able to work in relative isolation.
References
Celi LA, Mark RG, Stone DJ, Montgomery R (2013) “Big data” in the ICU: closing the data loop. Am J Respir Crit Care Med 187(11):1157–1160
Celi LA, Zimolzak AJ, Stone DJ (2014) Dynamic clinical data mining: search engine-based clinical decision support. J Med Internet Res Med Inform 2(1):e13. doi:10.2196/medinform.3110
Celi LA, Csete M, Stone D (2014) Optimal data systems: the future of clinical predictions and decision support. Curr Opin Crit Care 20:573–580
Moseley ET, Hsu D, Stone DJ, Celi LA (2014) Beyond data liberation: addressing the problem of unreliable research. J Med Internet Res 16(11):e259
Celi LA, Ippolito A, Montgomery R, Moses C, Stone DJ (2014) Crowdsourcing knowledge discovery and innovations in medicine. J Med Internet Res 16(9):e216. doi:10.2196/jmir.3761
Celi LA, Moseley E, Moses C, Ryan P, Somai M, Stone DJ, Tang K (2014) From pharmacovigilance to clinical care optimization. Big Data 2(3):134–141. doi:10.1089/big.2014.0008
Badawi O, Brennan T, Celi LA, Feng M, Ghassemi M, Ippolito A, Johnson A, Mark RG, Mayaud L, Moody G, Moses C, Naumann T, Pimentel M, Pollard TJ, Santos M, Stone DJ, Zimolzak AJ (2014) Making big data useful for health care: a summary of the inaugural MIT critical data conference. J Med Internet Res Med Inform 2(2):e22. doi:10.2196/medinform.3447
Moskowitz A, McSparron J, Stone DJ, Celi LA (2015) Preparing a new generation of clinicians for the era of big data. Harvard Med Student Rev 2(1):24–27
Ghassemi M, Celi LA, Stone DJ (2015) The data revolution in critical care. Ann Update Intensive Care Emerg Med 2015(2015):573–586
Stone DJ, Csete ME, Celi LA (2015) Engineering control into medicine. J Crit Care. Published Online: January 29, 2015. doi:10.1016/j.jcrc.2015.01.019
Health Information Technology for Economic and Clinical Health (HITECH) Act, Title XIII of Division A and Title IV of Division B of the American Recovery and Reinvestment Act of 2009 (ARRA), Pub. L. No. 111-5, 123 Stat. 226 (Feb. 17, 2009), codified at 42 U.S.C. §§300jj et seq.; §§17901 et seq
Horstmanshoff HFJ, Stol M, Tilburg C (2004) Magic and rationality in ancient near Eastern and Graeco-Roman medicine, pp 97–99. Brill Publishers. ISBN 978-90-04-13666-3
Bell SK, Folcarelli PH, Anselmo MK, Crotty BH, Flier LA, Walker J (2014) Connecting Patients and Clinicians: The Anticipated Effects of Open Notes on Patient Safety and Quality of Care. Jt Comm J Qual Patient Saf 41(8):378–384(7)
Celi LA, Marshall JD, Lai Y, Stone DJ, Physician documentation and decision making in the digital era. J Med Internet Res Med Inform (Forthcoming)
Longhurst CA, Harrington RA, Shah NH (2014) A ‘green button’ for using aggregate patient data at the point of care. Health Aff 33(7):1229–1235
Friedman C, Rubin J, Brown J et al (2014) J Am Med Inform Assoc 0:1–6. doi:10.1136/amiajnl-2014-002977
Institute of Medicine (2012) Best care at lower cost: the path to continuously learning health care in America. Retrieved from: http://iom.nationalacademies.org/Reports/2012/Best-Care-at-Lower-Cost-The-Path-to-Continuously-Learning-Health-Care-in-America.aspx
The Joint Commission (2014) National Patient safety goal on alarm management 2013
Personal communication, Randall Moorman, MD
Sodickson A, Opraseuth J, Ledbetter S (2011) Outside imaging in emergency department transfer patients: CD import reduces rates of subsequent imaging utilization. Radiology 260(2):408–413
A Robust Health Data Infrastructure. (Prepared by JASON at the MITRE Corporation under Contract No. JSR-13-700). Agency for Healthcare Research and Quality, Rockville, MD. April 2014. AHRQ Publication No. 14-0041-EF
Health Level Seven® International. HL7 Launches Joint Argonaut Project to Advance FHIR. N.p., 4 Dec. 2014. Web. 31 Aug. 2015. http://www.hl7.org/documentcenter/public_temp_32560CB2-1C23-BA17-0CBD5D492A8F70CD/pressreleases/HL7_PRESS_20141204.pdf
Austin JM et al (2015) National hospital ratings systems share few common scores and may generate confusion instead of clarity. Health Aff 34(3):423–430. doi:10.1377/hlthaff.2014.0201
Elton GEBM, Ripcsak GEH (2005) Automated detection of adverse events using natural language processing of discharge summaries. J Am Med Inform Assoc 12:448–458
Kohn LT, Corrigan JM, Donaldson MS (eds) (2000) To err is human: building a safer health system, vol 2. National Academy Press, Washington, DC
Author information
Authors and Affiliations
Rights and permissions
Open Access This chapter is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, a link is provided to the Creative Commons license and any changes made are indicated.
The images or other third party material in this chapter are included in the work’s Creative Commons license, unless indicated otherwise in the credit line; if such material is not included in the work’s Creative Commons license and the respective action is not permitted by statutory regulation, users will need to obtain permission from the license holder to duplicate, adapt or reproduce the material.
Copyright information
© 2016 The Author(s)
About this chapter
Cite this chapter
Stone, D., Rousseau, J., Lai, Y. (2016). Pulling It All Together: Envisioning a Data-Driven, Ideal Care System. In: Secondary Analysis of Electronic Health Records. Springer, Cham. https://doi.org/10.1007/978-3-319-43742-2_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-43742-2_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43740-8
Online ISBN: 978-3-319-43742-2
eBook Packages: MedicineMedicine (R0)