Abstract
Sickle cell disease (SCD) is one of the most common monogenetic diseases worldwide and is attributable to significant morbidity and mortality. Mutations causing abnormal hemoglobin formation in this disease lead to structural abnormalities and cumulative damage to the cellular membrane of sickled erythrocytes. Polymerization and aggregation of these cells within the microvasculature results in severe vaso-occlusive pain crisis, chronic hemolytic anemia, and multiorgan pathology in patients. Pulmonary manifestations of SCD, including the acute chest syndrome (ACS), are a leading cause of hospitalization and mortality. ACS is a severe type of acute lung injury, defined as the development of a new pulmonary infiltrate, involving at least one complete lung segment, that is accompanied by fever, chest pain, tachypnea, wheezing, or cough in a patient with SCD. The etiology of ACS is multifactorial, with the most common mechanisms including infection, fat and bone marrow embolism, and direct microvascular vaso-occlusion. Despite recent advances in our understanding of the pathogenesis and clinical management of ACS in SCD, patient outcomes remain unacceptably poor. This chapter reviews the epidemiology, diagnosis, management, and outcomes of ACS in SCD. Proper screening, a high index of clinical suspicion, and immediate clinical care for this condition are pivotal for improving patient outcomes.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Sickle cell disease
- Acute chest syndrome
- Pulmonary
- Lung diseases
- Hematologic disorders
- Anemia
- Vaso-occlusion
- Pain crisis
- Hemoglobin
- Epidemiology
Introduction
Sickle cell disease (SCD) is an autosomal recessive disorder affecting millions of individuals worldwide, making it one of the most common monogenetic diseases. Sickle cell anemia, the most common and severe form of SCD, occurs in patients with a single amino acid substitution of glutamic acid for valine in the β-globin gene, resulting in an abnormal hemoglobin form called hemoglobin S (HbS) within the erythrocytes. Mutant HbS has reduced solubility when deoxygenated compared to normal hemoglobin A (HbA), leading to polymerization and aggregation of sickle erythrocytes in the microvasculature. Structural abnormalities and cumulative damage to the cellular membrane of sickled erythrocytes results in hemolysis and the development of chronic hemolytic anemia, as well as vaso-occlusion and multiorgan pathology. Compound heterozygosity of HbS with other β-globin gene mutations results in additional types of SCD, such as hemoglobin SC or hemoglobin S-β-thalassemia [1]. Despite significant improvements in the life expectancy of patients with sickle cell disease, estimates of the median age at death range from 42 to 53 years for men and 48 to 58.5 years for women [2, 3].
The pathology of SCD is multifactorial and results from the structural and functional changes of sickled erythrocytes. Deoxygenated HbS polymerizes and aggregates inside erythrocytes, forming rigid, sickled cells. The abundance of polymerized HbS is strongly influenced by both the level of deoxygenation and the concentration of intracellular HbS [4], and determines the severity of SCD [5]. Pathologic sickled erythrocytes have increased adherence to the vascular endothelium, leading to microvasculature occlusion and subsequent multiorgan damage. Vaso-occlusion often manifests as episodic pain crises in SCD patients , a disease hallmark, as well as a high frequency of acute chest syndrome (ACS) [2, 6]. Due to chronically low Hb levels in SCD, patients rely on an overproduction of erythrocytes. Acute splenic sequestration and infectious and inflammatory processes, such as ACS, can interfere with erythropoiesis and trigger reticulocytopenia, or “aplastic crisis” in patients.
Sickled erythrocytes navigating the microcirculation are continually exposed to mechanical and oxidant injury, damaging the cell membrane and leading to a shortened erythrocyte lifespan, increased hemolysis and the development of chronic hemolytic anemia in patients. Importantly, intravascular hemolysis depletes the bioavailability of nitric oxide (NO) levels through the abundant release of both cell-free Hb, an NO scavenger, and arginase, which catabolizes arginine, a substrate necessary for NO synthesis [7]. Reduction in NO disrupts vascular homeostasis, leading to endothelial dysfunction, proliferation of cells within the vascular wall, thrombosis, and inflammatory stress [8–11]. Ischemia-reperfusion injury at sites of vessel occlusion can also promote inflammation and oxidative stress [12–15].
The low pressure and oxygen-tension within the pulmonary arterial bed can promote enhanced HbS polymerization and erythrocyte sickling [16]. Both acute and chronic pulmonary complications occur commonly in SCD and are a major cause of morbidity and mortality among these patients [2, 16–18]. Acute complications of SCD include asthma and ACS, while chronic complications can include pulmonary hypertension, restrictive lung disease (fibrosis), and corpulmonale [8, 19, 20]. In the Cooperative Study of Sickle Cell Disease (CSSCD) [21], a prospective, multi-institutional study of 3764 patients, over 20 % of adults with SCD likely had fatal pulmonary complications [2]. In another long-term, follow-up study of 299 SCD patients who participated in the Multicenter Study of Hydroxyurea in Sickle Cell Anemia (MSH), pulmonary complications were found to account for 24 % of deaths [22]. Though these results demonstrate the increasing recognition of pulmonary disease in SCD, there remains an imperative need for improved mechanistic understanding of these disease processes and novel therapeutic strategies.
Acute Chest Syndrome
The acute chest syndrome (ACS) is a lung injury syndrome of multiple etiologies first described in 1979 to describe a cohort of SCD patients presenting with fever, chest pain, increased white blood cell count, and pulmonary infiltrates [23]. The pathogenic mechanisms and epidemiology of ACS in SCD has been further studied since that time, and is currently defined as the development of a new pulmonary infiltrate, involving at least one complete lung segment, that is accompanied by fever, chest pain, tachypnea, wheezing, or cough [6, 24–26]. The pulmonary infiltrate appearing on chest radiography must be consistent with alveolar consolidation and not atelectasis [27]. ACS can affect both children and adults with any type of sickle hemoglobinopathy, but is more prevalent in individuals with homozygous sickle cell disease (HbSS) [28].
Three major mechanisms are known to be involved in the vaso-occlusive pathogenesis of ACS in SCD: infection, bone marrow and/or fat embolization, and direct pulmonary microvascular infarction due to red blood cell (RBC) sequestration [24, 29] (Fig. 4.1). The National Acute Chest Syndrome Study Group analyzed 671 episodes of ACS in 538 patients with SCD to determine the cause, outcome, and response to therapy [6]. Respiratory samples obtained from sputum and bronchoalveolar lavage were analyzed for viral and bacterial infections. A specific pathogen could not be identified in the majority of cases, however numerous different pathogens were identified, including Chlamydia pneumoniae (29 % of patients), Mycoplasma pneumoniae (20 %), and respiratory syncytial virus (10 %). Cases of severe ACS related to seasonal influenza have also been described [30, 31].
Pathologic mechanisms of acute chest syndrome. (From: Gladwin MT and Vichinsky E. Pulmonary complications of sickle cell disease. New England Journal of Medicine.2008;359(21):2254–65. [PMID:19020327]). The acute chest syndrome in sickle cell disease is a lung injury syndrome known to be initiated by three major mechanisms, including infection, bone marrow and/or fat embolization, and direct pulmonary microvascular infarction due to red blood cell sequestration. The mechanisms lead to vaso-occlusion by sickle cells with resulting infarction and lung injury. Ventilation–perfusion mismatch and hypoxemia due to lung injury leads to increased deoxygenation and polymerization of hemoglobin S, and erythrocyte vaso-occlusion. This pathologic mechanism promotes bone marrow infarction and pulmonary vaso-occlusion. NO nitric oxide; VCAM-1 vascular cell adhesion molecule 1
Bone marrow ischemia and necrosis are characteristic of vaso-occlusion in SCD and can lead to the release of fat and bone marrow into the circulation. ACS due to pulmonary fat and bone marrow embolizationhas a distinct and severe clinical course, associated with a high prevalence of bone and chest pain, neurologic symptoms, and decreased time to recovery [29, 32], and may be involved in up to 77 % of ACS episodes in adults [33]. Fat embolization can be diagnosed by the presence of lipid-laden macrophages in bronchoalveolar lavage fluid (BALF) from ACS patients [32–34]. However, due to the requirement of bronchoscopy, this method is not routinely performed and the true incidence of embolization is unknown. Since chest and rib pain are common manifestations of SCD, non-sickle pulmonary conditions such as fat embolism can be difficult to diagnose.
Direct pulmonary vaso-occlusion and infarction due to adhesion of sickled RBCs also contributes to ACS in SCD, though the exact incidence or primary causative nature of these events is unknown. A study in 144 cases of ACS to evaluate pulmonary artery thrombosis by CT–pulmonary angiography found a 17 % prevalence of pulmonary thrombosis without associated peripheral venous thrombosis [35]. These events occurred in patients with higher platelet counts and lower hemolytic rates during ACS, suggestive of in situ thrombosis. It is important to note that other causes of ACS, including infection and fat or bone emboli, as well as hypoxemia, may contribute to the development of pulmonary thrombosis in ACS. Prophylactic therapy for venous thromboembolism with low molecular weight or unfractionated heparin is therefore commonly used in adults with ACS, unless otherwise contraindicated.
In addition, severe acute hemolysis has been identified as a predictor of sudden death due to ACS [36]. The role of hemolysis-derived plasma-free Hb and its byproducts, including hemin (the oxidized prosthetic moiety of Hb), have been proposed as a novel inflammatory mechanism in ACS [37], and this may directly contribute to lung injury in the context of vaso-occlusive crisis. In support of the role of hemolysis in ACS, genetic variants in inducible hemeoxygenase 1 (HO-1), the rate-limiting enzyme in heme catabolism, are associated with ACS incidence in children [38].
Other pulmonary complications of SCD can be modulated by ACS, including pulmonary hypertension [39]. Pulmonary pressures can rise during episodes of ACS, leading to the development of acute right heart failure and increased mortality following the ACS event [17]. Therefore, prevention of ACS may reduce mortality in SCD patients with PH [40].
Epidemiology and Clinical Presentation
ACS is the second most common cause of hospitalization in SCD, second only to vaso-occlusive pain crisis, and is a leading cause of admission to an intensive care unit and premature death [2, 27]. Ten to twenty percent of patients admitted with acute vaso-occlusive pain crisis develop ACS in the first 3 days of hospitalization, and the mean duration of hospitalization for patients with ACS is 10.5 days [6]. While most cases are self-limited, some progress rapidly to acute respiratory failure with high rates of morbidity and mortality [41]. Overall mortality is 3 % in all ACS patients and 9 % in adults [6]. ACS therefore requires rapid management to prevent clinical decompensation and death. Recent increased awareness, the chronic use of hydroxyurea, and the aggressive use of early transfusion therapy, collectively, have led to a decrease in ACS-related mortality [42]. For example, a multicenter trial of inhaled NO for vaso-occlusive crisis found that only 10 % of patients in the placebo and treatment arm developed ACS and none required mechanical ventilation or died [42].
A natural history study by the CSSCD in both adults and children found that 29 % of all SCD patients will have at least one episode of ACS, and approximately half of those patients will have more than one ACS episode [28]. In patients with ACS, up to 78 % of episodes are associated with vaso-occlusive pain crisis, and the majority of patients also have chest pain, cough, and fever [33, 36]. The incidence of ACS in SCD is dependent on the subtype present. ACS episodes can affect patients with any type of SCD, but is most prevalent in individuals with HbSS (12.8 per 100 patient-years) compared to those with HbS-β0-thalassemia (9.4 per 100 patient-years), HbSC (5.2 per 100 patient-years), or HbS-β+-thalassemia (3.9 per 100 patient-years) [28]. The presence of α-thalassemia does not alter the ACS incidence rate in HbSS patients [28].
There are significant differences in the incidence and clinical presentation of ACS between adults and children with SCD, likely reflecting the differing etiologies in these age groups (Table 4.1). The incidence of ACS is higher in children (2–4 years of age) than adults (>20 years of age) with HbSS, with 25.3 events vs. 8.8 events per 100 patient-years, respectively [28, 36]. The course of disease tends to be milder in children, with higher rates of infectious causes. Adult cases of ACS are more severe, associated with pain, and have higher rates of mortality, with a higher incidence of pulmonary fat and bone marrow emboli [6, 29]. Adults with greater ACS incidence have a higher rate of all-cause mortality than those with low ACS incidence, and this increased rate of mortality may contribute to the decline in ACS incidence with age [28]. Despite these important differences between age groups, the clinical management is similar in both children and adults.
Numerous risk factors are associated with increased frequency of ACS. In children, asthma has been identified as an important modifiable risk factor. A CSSCD study in 291 African American children with HbSS followed beyond age 5 years found that asthma was significantly associated with more frequent ACS episodes (0.39 vs. 0.20 events per patient-year) and painful episodes (1.39 vs. 0.47 events per patient-year) [43]. Other clinical events that increase the risk of ACS include major surgical procedures, hypoxemia, a vascular necrosis of the hips, acute rib infarcts, pregnancy, use of narcotics, acute anemic events (aplastic crises), and previous pulmonary events [28, 36]. Active cigarette smoking or environmental smoke exposure are associated with more than twice the rate of ACS episodes, though no dose effect has been determined [44]. Significantly higher rates of ACS have also been reported following influenza infection [30, 31] and in winter months [36], findings most evident in children but present in all age groups.
Several laboratory parameters are associated with the development of ACS. Rates of ACS are positively correlated with non-vaso-occlusive crisis, steady-state white blood cell counts and Hb concentration and inversely correlated with fetal Hb (HbF) levels [28]. Though higher steady-state Hb levels are associated with ACS, during acute hospitalization for vaso-occlusive crisis, the development of ACS is often preceded by an abrupt drop in Hb levels (mean decrease of 0.78 g/dL from steady-state levels) and increases in markers of hemolysis, such as lactate dehydrogenase (LDH) [6, 27]. A drop in platelet count also has been shown to precede ACS, with levels <200,000 cells/mm3, and is an independent predictor of neurologic complications during hospitalization and need for mechanical ventilation [6, 45]. Understanding the epidemiology and complex etiologies of ACS in SCD, which differ among age groups, is critically important to diagnosing and treating this devastating disease manifestation.
Diagnosis
ACS is currently defined as an acute illness in SCD patients presenting with radiographic evidence of a new pulmonary infiltrate, involving at least one complete lung segment, that is accompanied by fever, chest pain, tachypnea, wheezing, or cough [6, 24–26] (Fig. 4.2a). Abdominal, limb, rib, or sternal pain is also common, along with intercostal retractions, nasal flaring, the use of accessory muscles for respiration, and decreased SpO2 (>2 % from steady-state). The clinical presentation, epidemiology, risks, and outcomes of ACS are variable, and the syndrome can often be diagnosed as pneumonia due to the number of shared features. Many of the clinical features of ACS are also age-dependent, reflecting differences in etiology among age groups, with adults having more causative fat embolization and children with a higher proportion of infectious causes and reactive airway disease.
(a–c): Radiographic and pathologic findings in acute chest syndrome. (From: Vij R and Machado RF. Pulmonary Complications of Hemoglobinopathies. Chest. 2010;138(4):973–983. [PMID:20923801]). (a) Chest CT scan of a 27-year-old woman with multifocal bilateral consolidations due to acute chest syndrome. (b) Post mortem specimen of a patient who died during an episode of vaso-occlusive crisis and acute chest syndrome depicting bone marrow emboli within a small pulmonary artery (hematoxylin and eosin stain, original magnification 40×). (c) Lipid inclusions within alveolar macrophages obtained by sputum induction in a patient with acute chest syndrome (oil-red O stain, original magnification 40×)
The diagnosis of ACS in SCD patients requires a high index of suspicion, and there are a number of recommended diagnostic approaches. Since the development of ACS often occurs 24–72 h after the onset of severe vaso-occlusive pain symptoms, it is critical that vigilance be kept during hospitalization of SCD patients , as they may be in the prodromal stages of ACS [25]. A thorough history and physical exam is required for all patients with SCD who present clinically with suspected signs of ACS, along with assessment of vital signs including oxygen saturation. Respiratory rate, pulse rate, and body temperature values have been shown to be higher in children than adults with ACS [36]. Patients with evidence of oxygen desaturation should have arterial blood gas measurements obtained to confirm the hypoxia [46], since pulse oximetry can be inaccurate in the presence of significant anemia. It is important to note that hypoventilation due to pain crisis or over-sedation can contribute to hypoxemia and exacerbation of ACS.
Chest radiography is required for all suspected ACS cases presenting with chest pain and/or fevers, though the findings may differ between adults and children. The CSSCD found that young children had more frequent infiltrates in the upper and middle lung lobes, while adults had more frequent lower and multiple lobe involvement and pleural effusion. However, another large, multicenter study found similar radiographic findings between adults and children with ACS [6, 36]. Radiologic signs are often absent early in development of ACS and may underestimate the severity of hypoxia [47], therefore treatment should not be delayed in the absence of significant findings and repeated chest X-rays should be obtained in suspected ACS cases.
Obtaining complete blood counts with white blood cell (WBC) differential, reticulocyte counts, and cultures of blood and sputum are also recommended for workup of suspected ACS cases. As mentioned above, an abrupt decrease in Hb concentration and platelet number often precede the development of ACS and are markers of disease severity [6, 45]. Reticulocyte counts can be used to assess for adequate bone marrow function and exclude red cell aplasia due to erythrovirus B19 infection [48]. ACS is associated with a systemic inflammatory state, with a mean peak temperature of 38.9 °C during hospitalization and a mean WBC count of 23,000 cell/mm3 [6]. Biochemical testing for C-reactive protein (CRP) can be useful in monitoring the inflammatory state of ACS patients, especially given the risk of multiorgan failure syndrome (discussed below), though the sensitivity and specificity of this test may be decreased if an infectious agent is present. Elevation in secretory phospholipase A2, a potent inflammatory mediator, occurs early in the course of ACS, before radiographic changes are detected, and has been shown to predict ACS onset [49].
Serological testing for infectious agents should also be considered in patients with ACS, both acutely and throughout illness, including detection of atypical respiratory organisms associated with ACS, such as Chlamyophila pneumoniae, Mycoplasma pneumoniae, and Legionella [48]. Pneumococcal and Legionella antigens may be detected in the urine. Testing for viral agents within sputum and nasopharyngeal samples via PCR and immunofluorescence staining, including influenza, respiratory syncytial virus, and erythrovirus B19, may also be indicated in ACS based on clinical and hematological findings [6, 48]. Identification of infective organisms can guide therapeutic treatment and/or the use of isolation facilities.
Bone marrow ischemia and necrosis lead to systemic fat and marrow embolization and contribute to a multiorgan failure syndrome with high clinical overlap and association with ACS (Fig. 4.2b). Patients with this syndrome can present with acute dysfunction of the lung, kidney, or liver, along with fever, alterations in mental status, seizures, decreased hemoglobin levels, thrombocytopenia, and coagulopathy. The similar presentation of multiorgan failure syndrome and ACS demonstrates a shared underlying etiology, with ACS predominantly affecting the lung [50]. Since the clinical manifestations of pulmonary fat embolization can be indistinguishable from other ACS causes, the diagnosis requires the identification of lipid-laden alveolar macrophages using Oil Red O staining (Fig. 4.2c). Bronchoscopy with BALF collection can be used for diagnosis, including identification of bacterial and viral agents, however this technique has been associated with an increased risk of requiring mechanical ventilation [6]. A significant correlation between results from the bronchoscopy method and induced sputum sampling of alveolar macrophages has been reported, and ACS patients with the presence of lipid-ladenalveolar macrophages in induced sputum have more extra-thoracic pain, neurological symptoms, thrombocytopenia, and elevated transaminase levels [51].
Other diagnostic procedures for ACS could include chest CT, ventilation-perfusion scanning, and angiographic imaging techniques to evaluate for pulmonary emboli, which have been shown to occur in the lungs due to both in situ vaso-occlusion of sickled erythrocytes and also secondary to pulmonary artery thrombosis in ACS [6]. Pulmonary artery filling defects are expected in these studies due to sickle cell vaso-occlusion [47, 52]. Though the extent of vascular occlusion identified by chest CT has been shown to correlate with clinical severity and degree of hypoxia in contrast to chest X-ray [47], it is not routinely recommended due to the high radiation exposure and the recurrence rate of ACS [48]. A recent study comparing the diagnostic performance and reproducibility of CT and bedside chest radiography during ACS found that CT more frequently identified lung consolidation patterns predominating in the lung bases and correlated with severity and disease course, however bedside chest radiography using CT as a reference had high sensitivity but low specificity [53].
Blood type should be determined for all patients at risk of ACS, given the potential requirement of emergency transfusion [48]. Erythrocyte alloimmunization is a serious complication in SCD patients and may result in delayed hemolytic transfusion reactions and difficulty finding compatible units [54]. Erythrocyte alloantibodies also may become undetectable over time in SCD patients, posing an even greater risk for adverse reactions during transfusion [54].
When SCD patients present with symptoms of ACS, several other life-threatening conditions should be considered in the differential diagnosis, as mentioned previously. These include pneumonia, pulmonary embolus, and acute coronary syndrome. Pneumonia cannot be distinguished clinically from ACS, therefore empirical antibiotic therapy is administered upon presentation. Pulmonary emboli originating from deep vein thrombosis are difficult to distinguish from in situ pulmonary thrombi or fat or bone marrow emboli occurring frequently in ACS, which do not respond to anti-coagulation therapy [24, 29]. Signs and symptoms of vaso-occlusive pain crisis and evidence of new pulmonary radiographic densities can assist in ruling out pulmonary embolus. Testing for D-dimers is unhelpful in SCD patients due to basally elevated levels [55]. ACS symptoms along with the detection of deep vein thrombosis in the lower extremities by ultrasound imaging, recent surgery, or extended periods of immobility suggest the presence of pulmonary emboli.
Acute coronary syndrome due to the rupture and dislodging of an atherosclerotic plaque within a coronary artery should also be considered with ACS symptom presentation, though coronary artery disease is uncommon in SCD [56]. Depending on clinical suspicion and patient history, electrocardiography and serum troponin levels can also be measured to evaluate for myocardial damage, since acute multiorgan failure may be present when vaso-occlusive pain crisis and myocardial damage are both present.
As described above, the diagnostic evaluation of ACS in SCD requires a high degree of clinical suspicion. Though most cases are self-limited, rapid progression to acute respiratory failure can occur with high rates of morbidity and mortality [41]. ACS therefore requires aggressive management in order to minimize poor clinical outcomes. All patients suspected of having ACS should receive chest radiography, complete blood counts with WBC differential, blood oxygen saturation testing (ABG), standard biochemistry testing, and blood group and screen [48]. Clinical indications may warrant the use of diagnostic blood cultures, sputum bacterial cultures, nasopharyngeal and sputum testing for viruses, and serology and urine testing. Other procedures and testing described should be carefully considered based on the clinical presentation and identification of potential differential diagnoses.
Management
Acute care for patients with ACS focuses on the prevention and reversal of acute respiratory failure, and will potentially mitigate irreversible lung damage. This includes immediate pain control, fluid management, supplemental oxygen, blood transfusion, antibiotic therapy, and prophylaxis for deep vein thromboembolism. These measures will typically result in the rapid resolution of symptoms in the majority of patients. However, it is imperative to recognize the course of ACS development differs among age groups, as ACS in adult cases can occur acutely or may evolve several days after admission for severe pain crisis, versus children who more often present acutely. Therefore, clinical suspicion for ACS in SCD patients should be high following any vaso-occlusive pain episode.
Vaso-occlusive pain crisis in SCD affecting the thorax can lead to severe discomfort and alveolar hypoventilation. Proper pain control with parenteral opioids is imperative during ACS episodes, and is often delivered by patient-controlled analgesia in adults. Continuous cardiorespiratory monitoring is required to avoid over-sedation and narcosis, which can lead to hypoventilation and subsequent hypoxemia, worsening ACS outcomes [6].
The severity of ACS often limits oral hydration in patients. Therefore, fluid management must be utilized to prevent hypovolemia and should be individualized based on the cardiopulmonary status of the patient. Though fluid replacement therapy is important in the management of ACS , care must be taken to prevent over-hydration, which can result in pulmonary vascular congestion and edema, exacerbating the course of ACS [48]. It is also important to recognize that a substantial proportion of patients with ACS develop right ventricular dysfunction and in these patients aggressive IV fluid therapy could lead to worsening cor pulmonale.
Supplemental oxygen therapy is delivered to adults with ACS with oxygen saturation (SaO2) <90 % or arterial oxygen partial pressure (PaO2) <60 mmHg [6]. SaO2 levels estimated by pulse oximetry should be confirmed with ABG analysis, and baseline values may be helpful in determining desaturation (decrease >3 % from baseline) when available. Co-oximetry provides the most accurate measure of SaO2 in patients with SCD, as vasoconstriction, hypotension, and hypothermia can affect pulse oximetry values. It is important to note that patients with SCD have a right-shifted oxyhemoglobin dissociation curve due to the presence of HbS. The need for supplemental oxygen should be continuously monitored in ACS.
Incentive spirometry, used to improve lung function and prevent atelectasis and pulmonary infiltrates, has been shown to decrease the rate of ACS in children admitted to the hospital for vaso-occlusive pain crisis [57]. While no studies to date have determined the benefit of this therapy in preventing the worsening of ACS in SCD patients, it is likely to be an important adjunct therapy. The use of this intervention may be limited by pain and should be tailored to the individual patient with the help of a respiratory physiotherapist [48].
Empirical antibiotic therapy is administered to patients suspected of having ACS, though infectious causes are less common in adults than children with SCD and respiratory samples from sputum and BALF do not identify a causative pathogen in the majority of ACS cases [6]. The most commonly identified organisms are atypical bacteria, including Chlamydia pneumoniae and Mycoplasma pneumoniae, along with Streptococcus pneumoniae and Haemophilus influenzae [6] (Table 4.2). Therefore, a typical antibiotic regimen may consist of a cephalosporin and a macrolide intravenously until fever subsides for at least 24 h, followed by oral administration for 7–10 days [6]. The antibiotics used should be tailored to culture results, when available, and local antibiotic resistance profiles should be considered [48]. There are currently no randomized control trials for antibiotic treatment regimens in the management of ACS.
Transfusion therapy is a mainstay treatment for patients with ACS despite the absence of any prospective cohort studies to demonstrate a change in patient outcomes. One large study found an increase in PaO2of 8 mmHg and increase in SaO2 of 3 % following transfusion in ACS patients, with an even greater improvement in SaO2 in patients who had demonstrated hypoxia prior to transfusion [6]. The oxygenation benefits of transfusion are due to a left-shift in the oxyhemoglobin dissociation curves, which is usually right-shifted at baseline in SCD due to the presence of HbS. Sickle-negative, leukocyte-depleted packed RBCs with extensive matching to Rhesus D, C, and E, as well as Kell antigens should be used for transfusion [58]. Since SCD patients often receive transfusions for many acute and chronic complications throughout the course of their disease, there is a risk for iron overload and alloimmunization. Therefore even with the use of antigen-matched and cross match-compatible blood, transfusions may pose a risk to patients with ACS.
The need for transfusion and the modality of simple versus exchange transfusion should be individualized based on ACS severity and the risk for developing acute respiratory failure [58]. Transfusion is required less often in children with ACS, who tend to have shorter, self-limited episodes due mainly to respiratory infections [6]. Simple RBC transfusion decreases the concentration of HbS by dilution, and should be considered in more stable patients with single-lobe involvement, mild hypoxemia responsive to low-flow oxygen, and worsening anemia [58]. Exchange transfusion performed by automated erythrocytapheresis can rapidly reduce the percentage of HbS without the risks of iron overload or hyperviscosity, but the risk of alloimmunization remains. This modality is often reserved for ACS patients with multilobar involvement, refractory hypoxemia, and imminent or rapidly progressing lung injury, or in less severe patients with high Hb concentrations (≥9 g/dL) to avoid hyperviscosity [58]. It has been demonstrated that conservative transfusion regimens are as effective as aggressive regimens in preventing perioperative complications in SCD, with the conservative regimen resulting in significantly fewer transfusion-associated complications [59]. Additionally, similar improvements in oxygen saturation were observed in a large cohort of ACS patients receiving either simple or exchange transfusions [6].
Bronchodilator therapy is often used in the treatment of ACS , however, there is a need for a randomized control trial to assess the risks and benefits of this therapy for ACS in SCD patients. Since wheezing occurs more often in children during ACS episodes compared to adults [6], and an association between ACS and asthma is known in children [43], the use of bronchodilators in ACS in this patient population may have increased benefit. Patients with evidence of reactive airway disease, acute bronchospasm, or the development of progressive respiratory distress during ACS should be considered for this therapy [48].
Advanced respiratory support in a critical care setting is needed for some ACS patients, indicated by worsening hypoxemia, severe dyspnea, and respiratory acidosis due to hypoventilation and hypercapnia [48]. The use of noninvasive ventilation (NIV) support to improve patient outcomes in ACS has been explored. A prospective, randomized study of 71 ACS episodes in 67 patients at one center demonstrated that NIV more rapidly decreased respiratory rate and improved gas exchange in ACS compared to oxygen alone [41]. However, NIV did not significantly reduce the number of hypoxemic patients at day 3 and was associated with decreased patient satisfaction and compliance. No differences were observed in pain relief, transfusions, or length of stay.
The National Acute Chest Syndrome Study Group found that 13 % of all ACS patients and 22 % of adults with ACS required the use of invasive mechanical ventilation (MV) during hospitalization, with a mean duration of MV of 4.6 days [6]. As previously discussed, there are several important risk factors influencing the need for invasive MV in ACS. These include platelet counts less than 200,000 cells/mm3 (likely indicative of the fat embolization syndrome), the number of lobes involved on chest radiography, and a self-reported or medical record history of cardiac disease [6]. The complications of heart disease are now thought to reflect the presence of occult pulmonary hypertension and cor pulmonale, as a recent study in 84 patients hospitalized with ACS found that 13 % manifested right heart failure [17]. Strikingly, this patient subgroup had the highest need for invasive MV and death, suggesting that pulmonary hypertension and right heart dysfunction is a major comorbidity during ACS.
Despite the aggressive nature of ACS, outcomes of patients requiring invasive MV are generally positive, with 81 % of patients recovering [6], compared to significantly lower recovery rates reported in patients with acute respiratory distress syndrome (ARDS). Strategies for the use of MV in ACS should follow similar strategies to treat acute respiratory distress syndrome (ARDS), including minimizing tidal volumes to prevent alveolar over-distension [60].
Given the significant morbidity and mortality associated with the development of ACS in SCD, significant measures can be taken to prevent the onset of ACS . These include the use of hydroxyurea therapy, chronic transfusion therapy, and hematopoietic cell transplantation.
The benefits of hydroxyurea therapy in SCD are far-reaching and well established, and were first demonstrated by the Multicenter Study of Hydroxyurea in Sickle Cell Anemia, a double-blind, placebo controlled trial in 299 adults with SCD [61]. Hydroxyurea has been shown to decrease the incidence of vaso-occlusive pain crises in SCD and reduce the risk ACS development by approximately 50 % when administered in the outpatient setting, and may also prevent splenic dysfunction, cerebral-artery damage, and secondary stroke [61, 62]. Importantly, hydroxyurea also significantly reduces the need for transfusion therapy and has been demonstrated to reduce overall mortality by 40 % in SCD. The beneficial mechanisms of hydroxyurea include increasing the number of RBCs containing high levels of HbF, (via stimulation of soluble guanylatecyclase and killing of cycling cells through inhibition of ribonucleotidereductase), as well as decreasing RBC membrane damage, sickling and vaso-occlusion [62] (Fig. 4.3). These factors can result in a significant reduction in ischemia, necrosis, hemolysis, and vascular damage. Given the known teratogenic effects of hydroxyurea, patients should not be treated during pregnancy or breast-feeding, and contraception should be used in patients receiving therapy. Before initiation of hydroxyurea therapy, baseline measures of complete blood counts, hepatic function, and renal function should be established to determine appropriate dosing. The myelosuppressive effects of hydroxyurea therapy should also be monitored with routine peripheral blood counts, and dose adjustment should be made as needed [62].
The pathophysiological effects of hydroxyurea therapy in sickle cell disease. (From: Platt OS. Hydroxyurea for the treatment of sickle cell anemia. New England Journal of Medicine. 2008;358(13):1362–9. [PMID: 18367739]). Mutations within the β-globin gene in sickle cell disease result in the production of sickle hemoglobin (HbS) within red blood cells (RBCs). Most RBCs produced in the bone marrow are derived from mature precursor cells and contain mostly HbS. Deoxygenation conditions induce HbS polymerization and morphological sickling of RBCs within the circulation, leading to pathologic vaso-occlusion and acute chest syndrome. HbS damages the RBC membrane through several mechanisms resulting in hemolysis, depletion of nitric oxide, and increased adherence to and damage of vascular cells. Hydroxyurea therapy induces γ-globin gene expression and can kill cycling cells, forcing more RBCs called F-cells to be produced, which are derived directly from primitive progenitor cells and contain high fetal hemoglobin (HbF) content. This can reduce pathologic RBC membrane damage, vaso-occlusion, ischemia, and necrosis. Hydroxyurea also produces nitric oxide, which may help to regulate vascular tone, and directly stimulates HbF production. Overall, hydroxyurea therapy leads to fewer symptoms in patients, less severe hemolytic anemia, fewer cases of acute chest syndrome, and lower mortality
As the natural history of ACS in SCD has evolved with modern diagnostic and therapeutic approaches, it has been established that a subset of patients are at very high risk for poor long-term outcomes and death. In addition to the described acute care strategies for ACS, several preventative measures may be employed in these patients. Hydroxyurea therapy is recommended for adult SCD patients with a history of ACS or frequent vaso-occlusive pain episodes, unless otherwise contraindicated, as described above [62]. In patients with multiple moderate to severe ACS episodes despite maximal hydroxyurea therapy, the use of chronic transfusion therapy to maintain a low percentage of RBCs containing HbS has been shown to decrease the rate of ACS and vaso-occlusive pain crises in SCD [63]. Careful risk-benefit assessments must be made in patients considered for chronic transfusion given the association of this therapy with a wide variety of adverse reactions. Myeloablative hematopoietic cell transplantation, currently the only cure for SCD , may be recommended for patients with severe symptoms that are unresponsive to hydroxyurea therapy or have a history of ACS and have a HLA-matched sibling available as a donor [64]. Despite the potentially curative outcome of transplantation in SCD, there is an associated risk of mortality of 7–10 % and relatively few studies done to address patient selection and criteria for transplant. The use of alternative donor sources and non-myeloablative transplant regimens are currently under investigation, but their utility in ACS remains uncertain.
Outcomes
Despite advances in therapy and our understanding of the pathophysiological mechanisms underlying ACS, it remains a leading cause of morbidity and mortality in patients with SCD.A higher incidence rate of ACS in adults with SCD is associated with an increased risk of death [2]. Multiorgan complications during ACS episodes are also prevalent, including vaso-occlusive crises, abdominal pain, and neurological, cardiac, gastrointestinal, and renal events [6]. The clinical features of ACS at the time of presentation are age-dependent due to differences in etiologies among age groups, with a striking difference in the overall rate of death per ACS episode between adults (4.3 %) and children (1.1 %) [36]. The onset of ACS is often preceded by vaso-occlusive crisis, chest pain, and dyspnea in adults, while fever and cough are more common in children. Though the majority of ACS cases occur in HbSS patients, a comparable rate of death per ACS episode has been observed in both HbSS and HbSC patients (1.9 and 1.6 %, respectively) [36].
In a large study conducted by the National Acute Chest Syndrome Study Group , the mean hospital stay for all ACS patients was found to be 10.5 days (12.8 days in adults), and that prolonged hospitalization was independently associated with an age of 20 years or more, a history of vaso-occlusive events, a platelet count of <200,000 cells/mm3 at diagnosis, pain in the arms and legs at presentation, extensive radiographic abnormalities, evidence of effusion on chest radiography, fever, transfusion therapy, and evidence of respiratory failure [6]. Of the 3 % of patients that died from ACS in this study, the most common causes of death were pulmonary emboli and infectious bronchopneumonia. Older patients were more likely to have complications and die during hospitalization for ACS, and respiratory failure, defined by the need for mechanical ventilation, occurred in 13 % of patients. The development of neurological events, including altered mental status, seizures, and neuromuscular abnormalities, occurred in 11 % of ACS patients, and 46 % of these patients had respiratory failure. Of the subset of patients with neurological complications and respiratory failure, 92 % received transfusion therapy and 23 % died [6]. Together, these findings highlight the significant sequelae associated with ACS, which contribute to poor patient outcomes.
Conclusion
ACS is a major cause of morbidity and mortality in adults and children with SCD and is associated with a multitude of multiorgan complications. The burden of this condition is likely to become more prevalent as the life expectancy of these patients continues to improve. A high index of suspicion is required to correctly diagnose ACS in SCD patients and improve outcomes. Though both acute and long-term strategies for the clinical management of ACS continue to advance, there is an imperative need for novel therapeutics, preventative strategies, and predictive measures for this devastating condition.
References
Ashley-Koch A, Yang Q, Olney RS. Sickle hemoglobin (HbS) allele and sickle cell disease: a HuGE review. Am J Epidemiol. 2000;151(9):839–45.
Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med. 1994;330(23):1639–44.
Wierenga KJ, Hambleton IR, Lewis NA. Survival estimates for patients with homozygous sickle-cell disease in Jamaica: a clinic-based population study. Lancet. 2001;357(9257):680–3.
Bunn HF. Pathogenesis and treatment of sickle cell disease. N Engl J Med. 1997;337(11):762–9.
Brittenham GM, Schechter AN, Noguchi CT. Hemoglobin S polymerization: primary determinant of the hemolytic and clinical severity of the sickling syndromes. Blood. 1985;65(1):183–9.
Vichinsky EP, Neumayr LD, Earles AN, Williams R, Lennette ET, Dean D, et al. Causes and outcomes of the acute chest syndrome in sickle cell disease. National Acute Chest Syndrome Study Group. N Engl J Med. 2000;342(25):1855–65.
Rother RP, Bell L, Hillmen P, Gladwin MT. The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin: a novel mechanism of human disease. JAMA. 2005;293(13):1653–62.
Gladwin MT, Sachdev V, Jison ML, Shizukuda Y, Plehn JF, Minter K, et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N Engl J Med. 2004;350(9):886–95.
Frei AC, Guo Y, Jones DW, Pritchard Jr KA, Fagan KA, Hogg N, et al. Vascular dysfunction in a murine model of severe hemolysis. Blood. 2008;112(2):398–405.
Hsu L, McDermott T, Brown L, Aguayo SM. Transgenic HbS mouse neutrophils in increased susceptibility to acute lung injury: implications for sickle acute chest syndrome. Chest. 1999;116(1 Suppl):92S.
Gladwin MT. Role of the red blood cell in nitric oxide homeostasis and hypoxic vasodilation. Adv Exp Med Biol. 2006;588:189–205.
Platt OS. Sickle cell anemia as an inflammatory disease. J Clin Invest. 2000;106(3):337–8.
Kaul DK, Hebbel RP. Hypoxia/reoxygenation causes inflammatory response in transgenic sickle mice but not in normal mice. J Clin Invest. 2000;106(3):411–20.
Klings ES, Farber HW. Role of free radicals in the pathogenesis of acute chest syndrome in sickle cell disease. Respir Res. 2001;2(5):280–5.
Hebbel RP. Ischemia-reperfusion injury in sickle cell anemia: relationship to acute chest syndrome, endothelial dysfunction, arterial vasculopathy, and inflammatory pain. Hematol Oncol Clin North Am. 2014;28(2):181–98.
Powars D, Weidman JA, Odom-Maryon T, Niland JC, Johnson C. Sickle cell chronic lung disease: prior morbidity and the risk of pulmonary failure. Medicine. 1988;67(1):66–76.
Mekontso Dessap A, Leon R, Habibi A, Nzouakou R, Roudot-Thoraval F, Adnot S, et al. Pulmonary hypertension and cor pulmonale during severe acute chest syndrome in sickle cell disease. Am J Respir Crit Care Med. 2008;177(6):646–53.
Thomas AN, Pattison C, Serjeant GR. Causes of death in sickle-cell disease in Jamaica. Br Med J. 1982;285(6342):633–5.
Minter KR, Gladwin MT. Pulmonary complications of sickle cell anemia. A need for increased recognition, treatment, and research. Am J Respir Crit Care Med. 2001;164(11):2016–9.
Siddiqui AK, Ahmed S. Pulmonary manifestations of sickle cell disease. Postgrad Med J. 2003;79(933):384–90.
Gaston M, Rosse WF. The cooperative study of sickle cell disease: review of study design and objectives. Am J Pediatr Hematol Oncol. 1982;4(2):197–201.
Steinberg MH, McCarthy WF, Castro O, Ballas SK, Armstrong FD, Smith W, et al. The risks and benefits of long-term use of hydroxyurea in sickle cell anemia: A 17.5 year follow-up. Am J Hematol. 2010;85(6):403–8.
Charache S, Scott JC, Charache P. “Acute chest syndrome” in adults with sickle cell anemia. Microbiology, treatment, and prevention. Arch Intern Med. 1979;139(1):67–9.
Ballas SK, Lieff S, Benjamin LJ, Dampier CD, Heeney MM, Hoppe C, et al. Definitions of the phenotypic manifestations of sickle cell disease. Am J Hematol. 2010;85(1):6–13.
Gladwin MT, Vichinsky E. Pulmonary complications of sickle cell disease. N Engl J Med. 2008;359(21):2254–65.
Platt OS. The acute chest syndrome of sickle cell disease. N Engl J Med. 2000;342(25):1904–7.
Miller AC, Gladwin MT. Pulmonary complications of sickle cell disease. Am J Respir Crit Care Med. 2012;185(11):1154–65.
Castro O, Brambilla DJ, Thorington B, Reindorf CA, Scott RB, Gillette P, et al. The acute chest syndrome in sickle cell disease: incidence and risk factors. The Cooperative Study of Sickle Cell Disease. Blood. 1994;84(2):643–9.
Dang NC, Johnson C, Eslami-Farsani M, Haywood LJ. Bone marrow embolism in sickle cell disease: a review. Am J Hematol. 2005;79(1):61–7.
George A, Benton J, Pratt J, Kim MO, Kalinyak KA, Kalfa TA, et al. The impact of the 2009 H1N1 influenza pandemic on pediatric patients with sickle cell disease. Pediatr Blood Cancer. 2011;57(4):648–53.
Strouse JJ, Reller ME, Bundy DG, Amoako M, Cancio M, Han RN, et al. Severe pandemic H1N1 and seasonal influenza in children and young adults with sickle cell disease. Blood. 2010;116(18):3431–4.
Vichinsky E, Williams R, Das M, Earles AN, Lewis N, Adler A, et al. Pulmonary fat embolism: a distinct cause of severe acute chest syndrome in sickle cell anemia. Blood. 1994;83(11):3107–12.
Maitre B, Habibi A, Roudot-Thoraval F, Bachir D, Belghiti DD, Galacteros F, et al. Acute chest syndrome in adults with sickle cell disease. Chest. 2000;117(5):1386–92.
Godeau B, Schaeffer A, Bachir D, Fleury-Feith J, Galacteros F, Verra F, et al. Bronchoalveolar lavage in adult sickle cell patients with acute chest syndrome: value for diagnostic assessment of fat embolism. Am J Respir Crit Care Med. 1996;153(5):1691–6.
Mekontso Dessap A, Deux JF, Abidi N, Lavenu-Bombled C, Melica G, Renaud B, et al. Pulmonary artery thrombosis during acute chest syndrome in sickle cell disease. Am J Respir Crit Care Med. 2011;184(9):1022–9.
Vichinsky EP, Styles LA, Colangelo LH, Wright EC, Castro O, Nickerson B. Acute chest syndrome in sickle cell disease: clinical presentation and course. Cooperative Study of Sickle Cell Disease. Blood. 1997;89(5):1787–92.
Ghosh S, Adisa OA, Chappa P, Tan F, Jackson KA, Archer DR, et al. Extracellular hemin crisis triggers acute chest syndrome in sickle mice. J Clin Invest. 2013;123(11):4809–20.
Bean CJ, Boulet SL, Ellingsen D, Pyle ME, Barron-Casella EA, Casella JF, et al. Heme oxygenase-1 gene promoter polymorphism is associated with reduced incidence of acute chest syndrome among children with sickle cell disease. Blood. 2012;120(18):3822–8.
Potoka KP, Gladwin MT. Vasculopathy and pulmonary hypertension in sickle cell disease. Am J Physiol Lung Cell Mol Physiol. 2015;308(4):L314–24.
Klings ES, Machado RF, Barst RJ, Morris CR, Mubarak KK, Gordeuk VR, et al. An official American Thoracic Society clinical practice guideline: diagnosis, risk stratification, and management of pulmonary hypertension of sickle cell disease. Am J Respir Crit Care Med. 2014;189(6):727–40.
Fartoukh M, Lefort Y, Habibi A, Bachir D, Galacteros F, Godeau B, et al. Early intermittent noninvasive ventilation for acute chest syndrome in adults with sickle cell disease: a pilot study. Intensive Care Med. 2010;36(8):1355–62.
Gladwin MT, Kato GJ, Weiner D, Onyekwere OC, Dampier C, Hsu L, et al. Nitric oxide for inhalation in the acute treatment of sickle cell pain crisis: a randomized controlled trial. JAMA. 2011;305(9):893–902.
Boyd JH, Macklin EA, Strunk RC, DeBaun MR. Asthma is associated with acute chest syndrome and pain in children with sickle cell anemia. Blood. 2006;108(9):2923–7.
Cohen RT, DeBaun MR, Blinder MA, Strunk RC, Field JJ. Smoking is associated with an increased risk of acute chest syndrome and pain among adults with sickle cell disease. Blood. 2010;115(18):3852–4.
Velasquez MP, Mariscalco MM, Goldstein SL, Airewele GE. Erythrocytapheresis in children with sickle cell disease and acute chest syndrome. Pediatr Blood Cancer. 2009;53(6):1060–3.
Desai PC, Ataga KI. The acute chest syndrome of sickle cell disease. Expert Opin Pharmacother. 2013;14(8):991–9.
Bhalla M, Abboud MR, McLoud TC, Shepard JA, Munden MM, Jackson SM, et al. Acute chest syndrome in sickle cell disease: CT evidence of microvascular occlusion. Radiology. 1993;187(1):45–9.
Howard J, Hart N, Roberts-Harewood M, Cummins M, Awogbade M, Davis B. Guideline on the management of acute chest syndrome in sickle cell disease. Br J Haematol. 2015;169(4):492–505.
Styles LA, Aarsman AJ, Vichinsky EP, Kuypers FA. Secretory phospholipase A(2) predicts impending acute chest syndrome in sickle cell disease. Blood. 2000;96(9):3276–8.
Hassell KL, Eckman JR, Lane PA. Acute multiorgan failure syndrome: a potentially catastrophic complication of severe sickle cell pain episodes. Am J Med. 1994;96(2):155–62.
Lechapt E, Habibi A, Bachir D, Galacteros F, Schaeffer A, Desvaux D, et al. Induced sputum versus bronchoalveolar lavage during acute chest syndrome in sickle cell disease. Am J Respir Crit Care Med. 2003;168(11):1373–7.
Feldman L, Gross R, Garon J, Nallari A, Kaur N, Motwani B, et al. Sickle cell patient with an acute chest syndrome and a negative chest X-ray: potential role of the ventilation and perfusion (V/Q) lung scan. Am J Hematol. 2003;74(3):214–5.
Mekontso Dessap A, Deux JF, Habibi A, Abidi N, Godeau B, Adnot S, et al. Lung imaging during acute chest syndrome in sickle cell disease: computed tomography patterns and diagnostic accuracy of bedside chest radiograph. Thorax. 2014;69(2):144–51.
Vichinsky EP. Current issues with blood transfusions in sickle cell disease. Semin Hematol. 2001;38(1 Suppl 1):14–22.
Francis Jr RB. Elevated fibrin D-dimer fragment in sickle cell anemia: evidence for activation of coagulation during the steady state as well as in painful crisis. Haemostasis. 1989;19(2):105–11.
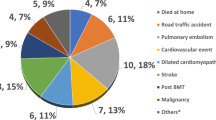
Manci EA, Culberson DE, Yang YM, Gardner TM, Powell R, Haynes Jr J, et al. Causes of death in sickle cell disease: an autopsy study. Br J Haematol. 2003;123(2):359–65.
Bellet PS, Kalinyak KA, Shukla R, Gelfand MJ, Rucknagel DL. Incentive spirometry to prevent acute pulmonary complications in sickle cell diseases. N Engl J Med. 1995;333(11):699–703.
Melton CW, Haynes Jr J. Sickle acute lung injury: role of prevention and early aggressive intervention strategies on outcome. Clin Chest Med. 2006;27(3):487–502. vii.
Vichinsky EP, Haberkern CM, Neumayr L, Earles AN, Black D, Koshy M, et al. A comparison of conservative and aggressive transfusion regimens in the perioperative management of sickle cell disease. The Preoperative Transfusion in Sickle Cell Disease Study Group. N Engl J Med. 1995;333(4):206–13.
The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. New Engl J Med. 2000;342(18):1301–8.
Charache S, Terrin ML, Moore RD, Dover GJ, Barton FB, Eckert SV, et al. Effect of hydroxyurea on the frequency of painful crises in sickle cell anemia. Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia. N Engl J Med. 1995;332(20):1317–22.
Platt OS. Hydroxyurea for the treatment of sickle cell anemia. N Engl J Med. 2008;358(13):1362–9.
Alvarez O, Yovetich NA, Scott JP, Owen W, Miller ST, Schultz W, et al. Pain and other non-neurological adverse events in children with sickle cell anemia and previous stroke who received hydroxyurea and phlebotomy or chronic transfusions and chelation: results from the SWiTCH clinical trial. Am J Hematol. 2013;88(11):932–8.
Shenoy S. Hematopoietic stem cell transplantation for sickle cell disease: current practice and emerging trends. Hematology. 2011;2011:273–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sysol, J.R., Machado, R. (2017). Sickle Cell Disease and Acute Chest Syndrome: Epidemiology, Diagnosis, Management, Outcomes. In: Lee, J., Donahoe, M. (eds) Hematologic Abnormalities and Acute Lung Syndromes. Respiratory Medicine. Humana Press, Cham. https://doi.org/10.1007/978-3-319-41912-1_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-41912-1_4
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-41910-7
Online ISBN: 978-3-319-41912-1
eBook Packages: MedicineMedicine (R0)