Abstract
Multiple sclerosis (MS) is a chronic disease of the central nervous system, which affects most often the young age. The disease has a social importance, as it leads to disability in active age. The course of the disease is individual and requires an adequate approach in selecting the appropriate treatment strategy. This requires periodic monitoring of the patients for early registration of the disease progression. Most commonly used tests are clinical investigation, brain MRI and other paraclinical methods, including neurophysiological assessment (usually evoked potentials). Evoked potential (EP) is a reliable method for quantifying the severity of damage to the white matter in patients with MS. The aim of this study is to develop a model for Generalized NET (GN)-registration of the direction of the course of disease based on neurophysiological evaluation of multimodal evoked potentials. Also, to make a comparison of the results obtained by the EP with the degree of disability as measured by the scale of Kurtzke (Expanded disability Status Scale-EDSS). We have followed up 48 patients with clinically definite MS over a period of 1 year. The patients were tested both clinically and neurophysiologically at Clinic of Neurology in MHAT- NHH, Sofia. The three main modalities evoked potentials were applied: visual evoked potentials with reversive pattern (VEPRP); Brainstem auditory evoked potentials (BAEP); Somatosensory evoked potentials (SSEP), taken during stimulation of median nerve. As a result it is established that the abnormalities of EP correlate significantly with the clinical findings. Based on the obtained results is developed a GN-model generating candidate predictive rules for the progression of the illness. In the end it has been found that abnormalities of EP significantly correlated with clinical findings. Based on the obtained results a GN model was developed. The model has a high sensitivity (SEN), specificity (SPE), PPV (Positive predictive value) and NPV (Negative predictive value) for the disease progression.
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Multiple sclerosis (MS) is an autoimmune, inflammatory, chronic and demyelinating degenerative disease of the central nervous system affecting young age [1]. The largest number of the patients is between 30 and 40 years of age. The onset of the disease was recorded in childhood in approximately 10 % of the patients. Susceptibility of the female to the disease is twice as much. Most affected are Caucasian subjects [2, 3]. The highest incidence of MS is set at the Orkney Islands north of Scotland-250/100, 000. A similar incidence of the disease is found in North America, Canada and New Zealand [4]. The incidence of MS is lowest in Japan 6/100 000 and in the other parts of Asia, sub-Saharan Africa and the Middle East. MS is a disease with social significance. The disease is chronic, with a duration of 10–15 years depending on the clinical form [5]. It was found a genetically predisposition, which in combination with certain environmental factors, leads to cascade of immune responses and disruption of the blood-brain barrier (BBB). As a result an inflammatory demyelination of the white matter in the CNS occurs due to activation of T-lymphocytes and macrophages. Impaired conduction of nerve impulses in the CNS, leading to clinical manifestation of the neurological deficit, appears [5]. Four different pathogenic mechanism of the disease are known, one of which is typical for each of the patients. This mechanism can be changed in time, which perhaps associated with different severity of disease [1, 6].
The disease is manifested clinically with multiple neurological dysfunctions from different systems (e.g., visual and sensory disturbances, weakness at limbs, gait disturbance, bowel and bladder disorders), followed by recovery or reinforcing of the disability.
According to the time profile of the disease, four major clinical forms of MS are distinguished.
- (1):
-
Relapsing-remitting form—affects approximately 65–85 % of the patients with MS. It is characterized with well identifiable attacks, expressed with neurological symptoms, which resolve for a period of few weeks or could lead to slow increase of disability. There is no progression between the attacks.
- (2):
-
Secondary-progressive form—when gradual accumulation of irreversible disability with or without separate attacks it occurs. After 6–10 years of the MS onset 4–70 % of patients with RRMS are passing into SPMS.
- (3):
-
Primary-progressive form—at about 10 % of the patients. When the symptoms of the disease got worse constantly and slowly from the beginning without distinct attacks, although there may be observed also plates and temporary improvement. Usually this form is related to early development of severe disability
- (4):
-
Progressive-remitting form—affects 5 % of the patients with MS. It is characterized by combination of attacks and progression in the early periods of the disease. There are pronounced attacks with or without full recovery. A gradual progression between relapses occurs. This form has a poor prognosis [5, 7].
Evoked potentials are routinely used in patients with MS [8–11]. They are included in supporting revised diagnostic criteria of MacDonald revision since 2005 [7, 12, 13]. EP are a reliable method for assessing the integrity of afferent and efferent pathways and to quantify the severity of damage of the white matter in MS [14]. It has been found that abnormalities of EP significantly correlates with clinical findings, while the majority of MRI-lesions are not associated with symptoms of the disease. Transverse and longitudinal studies have demonstrated that changes in the EP in MS are more closely associated with disability than MRI lesions [15]. This assumes that the EP could be useful in monitoring evolution of the disease and to serve as surrogate endpoints in clinical studies.
While MRI provides information on the spatial distribution of lesions at white matter, neurophysiological tests reflect their impact on the functions of the nervous system [16]. Neurodegeneration correlates with progression of MS and sensitive marker for its evaluation are still in process of searching.
Most often used EP modalities are: visual, somatosensory and brainstem auditory Abnormal visual evoked potentials with reversal pattern (VEPRP) typical for MS, are characterized with delayed latencies and less often- with altered waveforms [17, 18]. Brainstem auditory evoked potentials (BAEP) give information about the brainstem functioning. In MS, they are usually characterized with prolonged interpeak latencies (IPL) and/or abnormal amplitude ratios (AR) [19]. Somatosensory evoked potentials (SSEP) provide information about the presence of sensory damage as well as the topic of damage along the medial lemnisc system [20]. The values latencies in themselves do not carry information about the function of brain circuitry, but longitudinal changes in latencies during patient’s follow up shows deterioration of neurological dysfunction.
Importance of EP in monitoring the MS patients over the course of the disease is still a an object of investigation. Need to further investigate the role of multimodal EP in follow up the MS subjects is determined by insufficient data from previous studies.
2 Materials and Methods
For the purposes of this work 48 patients with clinically definite MS were tested twice at Clinic of Neurology at MHAT-NHH-Sofia. Demographic data concerning our sample are given on the following table:
Examined twice with multimodal EP and EDSS | 48 | |
Mean age | \(39.4 \pm 9.6\) | |
Male patients | 17 | 35 % |
Female patients | 31 | 65 % |
EDSS \(\le 3.5\) | 18 | 37 % |
EDSS \(> 3.5\) | 30 | 63 % |
The following 3 modalities EP were followed up:
-
\(\checkmark \) Visual evoked potentials with reverse pattern (VEPRP)
-
\(\checkmark \) Brainstem auditory evoked potentials (BAEP)
-
\(\checkmark \) Somatosensory EP, elicited by stimulation of mediane nerve (SSEP)
The reason for the this choice is the frequent involvement of the three sensory modalities in MS and possibility for an objective neurophysiological monitoring of their changes in the course of the disease. The main indicators that were taken into account in the analysis of the EP in this work are:
-
\(\checkmark \) latency, i.e. time from the stimulus to the wave response registration
-
\(\checkmark \) amplitudes, measuring the distance from peak to peak (especially informative in SSEP)
-
\(\checkmark \) configuration violations.
2.1 Visual Evoked Potentials (VEP)
VEP were performed with two-channel installation by applying reversive pattern in order to improve the the objectivity the results. Checkerboard pattern is used with frequency reversion 1 Hz, low-pass filter—1 Hz, high-pass filter—100 Hz, a band filter 50 Hz. Administration of sequential monocular foveolar (15’) and peripheral (60’) retinal stimulation for objectifying the function of the visual pathways starting from foveolar and peripheral retinal neurons. The epoch of analysis is 300 ms. One hundred averaging in each assay were done. The following parameters were recognized: Delayed latencies of N75 and P100 (L N75, L P100), Configuration violations, Interocular and interhemisphere asymmetry (IO A, IH A). On the next figure are given the graphical interpretation of VEP—examinations a healthy control and a patient with pathologically changed result (Fig. 1).
2.2 Brainstem Auditory Evoked Potentials (BAEP)
In BAEP stimulation monaural square click stimulus was used which lasts 100 \(\upmu \mathrm{{s}}\). The frequency of stimulation was 10 Hz, the intensity \(-90\) dB nHL and masking noise to the contralateral ear of 40 dB was applied. Polarity of stimulus: rarefaction-condensation. Band filter was used within the range of 100–2000 Hz. Epoch analysis is 10 ms. In each stimulation 2000 averaging were carried out. Two-channel apparatus was used. The following parameters were analyzed: interpeak latencies (IPL), amplitude ratios (AR), also mono-and binaural impairment was taken into account during interpretation of the results. Hearing impairment was excluded in all of the patients. The montage which we used is approved by the Recommended Standard for short latency EP of American Society of Clinical Neurophysiology (2009). On the following figure are given graphic results of BAEP-tests of healthy control and of a patient with pathologically changed result (Fig. 2).
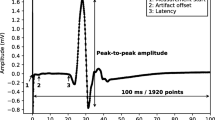
2.3 Somatosensory Evoked Potentials at Stimulation of Median Nerve
The functional state of the pathways of deep sensibility in the tested sample with MS was monitored by examining SSEP, elicited from sequential bilateral stimulation of mediane nerve. For this purpose, 4-channel montage was used which followed the requirements of the consensus of the American Association of Clinical Neurophysiology and the European standard for SSEP: epoch analysis \(-60\) ms, filter bandwidth: 20–2000 Hz, frequency of stimulation \(-5\) Hz, duration of the stimulus \(-0.2\) ms. We performed consistently stimulation median nerve on the left and on the right side, and the number of the averaged stimuli was 600. Were carried out two examinations in each side in order to obtain replication of the curves and greater reliability of results. In the analysis of the results we have considered latencies of the individual wave components at SSEP, which corresponds to the conduction velocity of the nerve impulses along the sensory pathways at certain levels, respectively: peripheral nerve structures, cervical myelon (posterior lemniscus and/or rear posterior horns for surface sensitivity), lemniscus medialis along the brainstem, thalamus, the primary somatosensory representation of the cortex. Were were taken into account latency of N9, N11, N13, P14, N20, that the order of listing correspond to the different levels of the system of deep sensation. For greater objectivity of the SSEP interpretation we have used interpeak latencies (IPL), as they minimize the impact of anthropometric factors. In the analysis of the data we have used IPL N9–N13, N13–N20 and N9–N20. Prolonged IPL were associated with impaired conduction within the range formed between the generators.
The following figure shows the graphic results of SSEP-examination of the control and of a patient with MS with deviations (Fig. 3).
For more objective assessment of the SSEP we have used total EP-score, which was calculated from individual EP scores from different modalities EP. Neurophysiological assessment is based on total EP score, which is a sum of the individual EP-scores of the three types of modalities.
VEP-score | BAEP-score | SSEP-score | |
|---|---|---|---|
0 | Normal result | Normal result | Normal result |
1 | Configuration abnormalities/ Interocular asymmetry/ interhemispheral asymmetry but preserved conduction time | At least one abnormal amplitude ratio (AR) at unilateral monoaural stimulation | Prolongation of 1 IPL at unilateral stimulation of median nerve |
2 | Prolonged latencies up to 20 ms | Prolonged IPL at monoaural unilateral stimulation and/or bilaterally impaired | Prolongation of \({\ge }2\) IPL and/or bilateral stimulation |
3 | Prolonged latencies within 20–40 ms | Both bilaterally impaired IPL at monoaural bilateral stimulation | Prolongation of 3 IPL at unilateral median nerve stimulation and abnormality of 1 IPL at contralateral stimulation, or lack of identification of 1 wave |
4 | Prolonged latencies \({>}40\) ms | Severe abnormalities and difficult identification of waves in up to 2 leads | Prolongation of both 3 IPL at unilateral median nerve stimulation and \({\ge }2\) IPL at contralateral stimulation, or impossible identification of 2 waves |
5 | Severe abnormalities and difficult identification of the waves | Severe abnormalities and impossible identification of waves bilaterally in all the leads | Severe abnormalities and impossible identification of waves bilaterally |
3 Generalized Net Model
The Generalized nets (GN) were introduced by Atanassov as an extension of the Petri nets see [21, 22]. We have used the previously established values for the Visual Evoked Potentials (see [23]). For the SSEP, the most indicative in the preliminary investigation proved to be the number of lesions and the interpeak latencies (IPL). The IPL N9–N13, N13–N20 and N9–N20 were investigated in the model. The BAEP were investigated mainly for the IPL III-V cross simulation and I/III amplitude ratio.
We have adopted the approach taken in [23]. In fact the rule established there for the VEPs is used here unchanged. The setup of the Generalized net is the following: the patients, represented by \(\alpha \)-tokens, are placed at \(L_4.\) The candidate rules represented by \(\beta \)-tokens are placed in places \(L_1,\) \(L_2\) and \(L_3\) and are initially passed to \(L_9\) where they form a \(\gamma \)-token with characteristic “list of current rules; counter for each of the current rules”. Places \(L_6,\) \(L_7,\) \(L_{8}\) are used to supply the current rules to the next transition and to split the \(\alpha \)-tokens representing the patients into three for estimation in the next transition. The next transition corresponds to the satisfaction of the rules and separating the patients in three possible classes (EDSS \(\le 3.5\)), (EDSS \(> 3.5\)) and failed to be classified, and also also assigning a score to all used rules (\(L_{19}\)), and sending feedback for the following rules to be created (Fig. 4).
The rules are of the kind: \(\wedge p*\vee \lnot p*\wedge q*\) with \(p \in P\), \(q \in Q\) and p* being conjunctions of predicates from P and q* being conjunctions of predicates from Q for the first class (EDSS \(\le 3.5\)), while for the second they are from the type \(\lnot p*\wedge \lnot q*\), where P is the set of predicates of the kind “Parameter value less or equal to a threshold value” and Q is the set of predicates of the kind “Parameter value greater or equal to a threshold value”.
For every parameter we consider the predicates p (or q) for 120 possible threshold values (i.e. \(p \le \) ((k + 1)/2)*MEAN(PARAM_VALUE)/60, with \(k = 0, 1\ldots , 119\)).
The generated rules were scored based on the values of calculated sensitivity and specificity.
The model has three transitions, nineteen places and three types of tokens—\(\alpha ,\) \(\beta \) and \(\gamma .\)
Below is a formal description of the transitions of the net.
where \(W_{9,8}=\) “New candidate rules are needed and not all rules have been tried.”
where
\(W_{5,10}=\) “there is no \(\beta \) token in place \(L_{10}\)”
\(W_{6,11}=\) “there is no \(\beta \) token in place \(L_{11}\)”
\(W_{7,12}=\) “there is no \(\beta \) token in place \(L_{12}\)”
\(W_{8,10}=\) “there is no \(\alpha \) token in place \(L_{10}\) \(\vee \) the current \(\beta \)-token needs to be replaced”
\(W_{8,11}=\) “there is no \(\alpha \) token in place \(L_{11}\) \(\vee \) the current \(\beta \)-token needs to be replaced”
\(W_{8,12}=\) “there is no \(\alpha \) token in place \(L_{12}\) \(\vee \) the current \(\beta \)-token needs to be replaced”
\( W_{14,10}=\) “the current \(\beta \)-token in place \(L_{10}\) has to be replaced”
\( W_{14,11}=\) “the current \(\beta \)-token in place \(L_{11}\) has to be replaced”
\( W_{14,12}=\) “the current \(\beta \)-token in place \(L_{12}\) has to be replaced”
\( W_{14,13}=\) “new \(\alpha \)-token is required”
where
\(W_{10,15}=\) “the current \(\alpha \) token satisfies the current BAEP rule for belonging to the class (EDDS \(\le 3.5\))”
\(W_{10,16}=\) “the current \(\alpha \) token satisfies the current BAEP rule for belonging to the class (EDDS \(> 3.5\))”
\(W_{10,17}=\) “\(\lnot W_{10,15} \wedge W_{10,16} \)”
\(W_{11,15}=\) “the current \(\alpha \) token satisfies the current SSEP rule for belonging to the class (EDDS \(\le 3.5\))”
\(W_{11,16}=\) “the current \(\alpha \) token satisfies the current SSEP rule for belonging to the class (EDDS \(> 3.5\))”
\(W_{11,17}=\) “\(\lnot W_{11,15} \wedge W_{11,16} \)”
\(W_{12,15}=\) “the current \(\alpha \) token satisfies the current VEP rule for belonging to the class (EDDS \(\le 3.5\))”
\(W_{12,16}=\) “the current \(\alpha \) token satisfies the current VEP rule for belonging to the class (EDDS \(> 3.5\))”
\(W_{12,17}=\) “\(\lnot W_{12,15} \wedge W_{12,16} \)”
\(W_{19,18} =\) “the generation of new rules is required (i.e. the number of identified by the current rules \(\alpha \)-tokens is divisible by 48.)”
The derived rules from the work of the net (all rules that fail to separate the patients in two classes were discarded) were the following:
For the SSEP:
-
EDSS\(> 3.5\) if \(p=\) (Number of spinal lesions \({>}3\)) \(\wedge \) (IPL N13–N20 \(> 5.7\) ms) \(\vee \) ((Number of spinal lesions \({\le }3\)) \(\wedge \) (IPL N9–N20 \(> 13.5\) ms))
-
EDSS\(\le 3.5\) if \(\lnot p.\)
For the BAEP:
-
EDSS\(> 3.5\) if \(p=\) (IPI III-V under cross stimulation \(> 2.18\) ms) \(\vee \) ((IPI III-V cross stimulation \(\le 2.18\) ms) \(\wedge \) (I/III amplitude ratio \(> 6.75\)))
-
EDSS\(\le 3.5\) if \(\lnot p.\)
For the VEP:
-
EDSS\(\le 3.5\) if \(q=\) ((Foveolar stimulation L N75 \(\le 86.56\)) \(\wedge \) (Foveolar stimulation I 100 \(\le 7.25\))) \(\vee \) ((Foveolar stimulation L N75 \(> 86.56\)) \(\wedge \) (Peripheral stimulation IH N75 \(\le 1.9\)) \(\wedge \) (Foveolar stimulation IH 100 \(\le 3.65\)) \(\wedge \) (Foveolar stimulation IH N75 \(\le 3.65\))) \(\vee \) ((Foveolar stimulation L N75 \(> 86.56\)) \(\wedge \) (Peripheral stimulation IH N75 \(> 1.9\)) \(\wedge \) (Foveolar stimulation I N75 \(\le 0.275\)))
-
EDSS\(< 3.5\) if \(\lnot q.\)
4 Results
The results from both clinical and neurophysiological examination from the baseline and follow up study were compared. The dynamics of the grade of disability is presented at the following figure:
The figure visualizes a linear relationship between the values of the total EP score and EDSS-score in both studies. It is evident that the higher the neurophysiological damage is associated with higher degree of disability. In the follow up study, the tangent-line trend is higher, which corresponds to largest values of the monitored scores, i.e. with deterioration of the patients (Figs. 5 and 6).
Following the suggestion of the GN model, if there are more than 3 demyelinating lesions in the cervical myelon (visualized by MRI study) and when IPL N13–N20 is greater than 5.7 ms, practically all patients from our sample are with high degree of disability, i.e. they belong to class 1 EDSS (EDSS \(> 3.5\)). At presence of MRI lesions in the cervical myelomas, while IPL N13–N20 is \({<}5.7\) ms, the classification of patients according to the severity of the disability is not reliable. At presence of less than three spinal lesions in MRI study whilst IPL N9–N20 is \(>13.4\) ms, almost all patients in our sample have a high degree of disabled, i.e. they belong to class 1 EDSS (EDSS \(> 3.5\)). If there are less than 3 spinal lesions, also IPL N9–N20 is \({\le }13.4\) ms, the majority of patients are with low degree of disability according to EDSS—class 0 (EDSS \(\le 3.5\)). The sensitivity (SEN), specificity (SPE), positive predictive value (PPV) and negative predictive value (NPV) of the elected rule were calculated. The calculation is made according to following formulas
where
-
TN (true negatives) the number of patients with low degree of disability defined as patients with low degree of disability (EDSS \(\le 3.5\)) in the course of the statistical analysis of the BAEP-results;
-
TP (true positives)—number of patients with high degree of disability (EDSS \(> 3.5\)) statistically defined as patients with high disability (EDSS \(> 3.5\));
-
FP (false positives)—number of patients with low disability (EDSS \(\le 3.5\)) statistically defined as patients with high degree of disability (EDSS \(> 3.5\));
-
FN (false negatives)—number of patients with high degree of disability (EDSS \(> 3.5\)) identified in the statistical processing of BAEP results as patients with low disability (EDSS \(\le 3.5\)).
Statistical analysis defined as true positive (TP) 17 patients from our sample. These are subjects whose pathological SSEP changes are associated with EDSS \({>}3.5\). Twenty two patients were classified as true negative (TN) their EDSS was \({\le }3.5\), and SSEP study revealed no abnormalities or minimal neurophysiological changes. As false positives (FP) are defined 0 of 48 patients studied, i.e. we did not find patients with a low level of disability and pathologically changed SSEP-scores above definitions in the course of statistical processing threshold. Statistical analysis classified 9 of the subjects as false negative (FN)—these are the patients with a high degree of disability, in which SSEP were normal or slightly disturbed).
Below are presented indicators sensitivity, specificity, positive predictive value, negative predictive value, calculated based on the above mentioned formulas
SEN | SPE | PPV | NPV | |
SSEP | 61 % | 70 % | 71 % | 67 % |
Statistical analysis of the results from the examined patients identified as leading neurophysiological criteria for prediction the severity of disability the following indicators: IPL III-V under cross-stimulation and AR I / III under ipsilateral stimulation. As “Class 0” are categorized the patients with a low degree of disability, i.e. with EDSS \(\le 3.5\) and as a “Class 1”—patients with a high degree of disability, i.e. with EDSS \(> 3.5\). In cases where the IPL III-V under cross stimulation is higher than 2.18 ms, 80 % of the patients have a high degree of disability. Where IPL III-V under cross stimulation is \({\le }2.18\) ms, the majority of cases have a low degree of disability (60 %). When IPL III-V under cross stimulation is \({\le }2.18\) ms and AR I/III under ipsilateral stimulation is \({>}6.75,\) 100 % of the patients express high degree of disability (EDSS \(> 3.5\)). In cases when IPL III-V under cross stimulation is \({<}2.18\) ms, whilst AR I/III under ipsilateral stimulation is \({\le }6.75\), 72 % of the examined revealed low degree of disability, i.e. their EDSS was less or equal to 3.5.
Below are presented indicators sensitivity, specificity, positive predictive value, negative predictive value, calculated based on the above mentioned formulas
SEN | SPE | PPV | NPV | |
BAEP | 70 % | 81 % | 77 % | 75 % |
We have developed a classification based on N75 latency under foveolar stimulation (respectively less or more than 86.6 ms) combined with other neurophysiological VEPRP-abnormalities can be predictive indicator to the degree of invalidity in the patients, respectively, low level (EDSS \(\le 3.5\)) and high (EDSS \(> 3.5\)). In the analysis of our results the greatest responsiveness of the latency of the early wave component N75 as a marker identifying the severity of the disease has been established, which was confirmed by other authors. Cuypers et al. found that N75 latency is more sensitive marker than P100 latency, when classifying the severity of MS, despite its great influence of age, gender and stimulus pattern [24]. The chart shows that if N75 latency under foveolar stimulation is \({>}86.6\) ms and interocular asymmetry of N75 (IOA N75) in peripheral stimulation is \({>}1.9\) ms, the patient probably has a disability over 3.5 points on the scale of Kurtzke. If N75 latency under foveolar stimulation is \({<}86.6\) ms , and interhemisphere asymmetry of P100 (IHA P100) at foveolar stimulation is \({\le }1.9\) ms, the probability of predicting disability is reduced. If N75 latency at foveolar stimulation is \({\le }86.6\) ms and interocular asymmetry of P100 (IOA P100) is \({>}7.25\) ms, most likely the patient belongs to Class 1, i.e. EDSS score is \({>}3.5\) If N75 latency at foveolar stimulation is \({\le }86.6\) ms, while interocular asymmetry of P100 (IOA P100) is \({\le }7.25\) ms, most likely the patient has a low degree of disability (EDSS score \(\le 3.5\)).
The following table shows the values for the VEP rule:
SEN | SPE | PPV | NPV | |
VEPRP | 100 % | 76 % | 83 % | 100 % |
5 Discussion
For the predictive value of pathologically changed VEPRP concerning the degree of disability in patients with MS it is possible to use lower threshold margins, e.g.:
\(\checkmark \) patients with low grade of disability (EDSS \(< 3\))
\(\checkmark \) patients with high grade of disability (EDSS \(\ge 3\))
The threshold set in relation to severity of disability assessed by EDSS may be chosen lower in VEPRP, as SSEP have changed earliest from all other modalities EP and often they register deterioration before reaching of significant clinical disability.
Parameters sensitivity and specificity of VEP calculated in the present work are close to the results obtained by other authors. Grover et al. set sensitivity 84.2 % and specificity 90 % VEP-study, using size to the boxes 60’ [25]. Ko calculated sensitivity to 100 % VEP [26]. Balnyte et al. determined 90.5 % sensitivity and 82.5 % specificity of VEP [27]. Gnezditskiy and Korepina calculated 72 % sensitivity and 100 % specificity of VEP [28]. Our study confirms the conclusion of most researchers that VEP are extremely sensitive method for assessing the degree of disability in MS and for prediction the course of the disease.
Regarding the sensitivity of the BAEP, the results in the literature are controversial. Burina et al. [29] revealed 95 % sensitivity of BAEP in terms of detection of brainstem lesions in a study of 60 patients. Berger and Blum [30] registered 46 % sensitivity of BAEP. The divergences are probably due to differences in methodology as well as various parameters for the evaluation; the majority of researchers prefer IPL measurement as a decisive criterion for evaluation. In our study the higher percentage of BAEP abnormalities includes mostly damaged AR and less frequent prolonged IPL. We assume that abnormal ARs are an early marker of brainstem abnormality and this may be a result from gray matter damage.
All of the above suggest using VEPs as leading method in the assessment of the progression of the disease with the other two EP used as an auxiliary tool to diminish the error in the estimate. Further investigation in this direction is currently in progress.
6 Conclusion
Safety, non invasiveness, relatively low cost of the study and the possibility of continuous monitoring make this neuropsychological test appropriate in assessing progression of the disease and the degree of involvement of different sensory systems. The study is informative in follow up the effect of immunomodulatory therapy, also the recovery after attack. The utilized Generalized net models allows for fast, cost efficient way of electing candidate rules to be reviewed and evaluated by the doctors in the course of their practice. If such rules prove to be reliable and have predictive nature, they can be used to alleviate some of the problems the patients experience.
References
Milanov, I.: Multiple sclerosis and demyelinating diseases, p. 242. Medicina i Fiskultura, Sofia (2010)
Pugliattia, M., Sotgiu, S., Rosati, G.: The worldwide prevalence of multiple sclerosis. Clin. Neurol. Neurosurg. 104, 182–191 (2002)
Pugliattia, M., Rosatia, G., Cartonc, H., et al.: The epidemiology of multiple sclerosis in Europe. Eur. J. Neurol. 13, 700722 (2006)
Taylor, B., Pearson, J., Clarke, G., et al.: MS prevalence in New Zealand, an ethnically and latitudinally diverse country. Mult. Scler. 16, 1422–1431 (2010)
Milanov, I.: National consensus for diagnosis and treatment of multiple sclerosis. Mov. Disord. (Bulgaria) 9(2), 40 (2012)
Lucchinetti, C., Bruck, W., Parisi, J., et al.: Heterogeneity of multiple sclerosis lesions: implications for the pathogenesis of demyelination. Ann. Neurol. 47, 707–717 (2000)
McDonald, W.I., Compston, A, Edan, G., Goodkin, D.: Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of multiple sclerosis. Ann. Neurol. 50(1) (2010)
Capra, R., Mattioli, F., Vignolo, L.A., et al.: Lesion detection in ms patients with and without clinical brainstem disorders: magnetic resonance imaging and brainstem auditory evoked potentials compared. Eur. Neurol. 29, 317–322 (1989)
Carter, J., Stevens, J.: Somatosensory evoked potentials. In: Jasper, D., Devon, R. (eds.) Clinical Neurophysiology, 3rd edn, pp. 18-257–268. Oxford University Press, New York (2009)
Carter, J.: Brainstem auditory evoked potentials in central disorders. In: Jasper, D., Devon, R. (eds.) Clinical Neurophysiology, 3rd edn, pp. 19-281–286. Oxford University Press, New York (2009)
Carter, J.: Visual evoked potentials. In: Jasper, D., Devon, R. (eds.) Clinical Neurophysiology, 3rd edn, pp. 22- 311–318. Oxford University Press, New York (2009)
Epstein, C.: Visual evoked potentials. In: Daly, D., Pedley, T. (eds.) Current Practice of Clinical Electroencephalography, 2nd edn, pp. 593–623. Raven Press, Ltd, New York (1990)
Frohman, E., Costello, F., Stüve, O., et al.: Modeling axonal degeneration within the anterior visual system. Arch. Neurol. 65(1), 26–35 (2008)
Haarmeier, T., Dichgans, J.: Die Wertigkeit der evozierten Potenziale in der Diagnostik der multiplen Sclerose. Evozierte Potenziale, 433–445 (2005)
Comi, G., Leocani, L., Medaglini, S., Locatelli, T., Martinelli, V., Santuccio, G., et al.: Measuring evoked responses in multiple sclerosis. Mult. Scler. 5, 263–267 (1999)
Rösler, K., Hess, C.: Conduction studies in multiple sclerosis. In: Kesselring, J., Comi, G., Thompson, A. (eds.) Multiple Sclerosis: Recovery of Function and Neurorehabilitation, 1: 1–10. Cambridge University Press (2010)
Gilbert, M., Sergott, R.: New directions in optic neuritis and multiple sclerosis. Curr. Neurol. Neurosci. Rep. 7, 259–264 (2007)
McDonald, I., Compston, A., Edan, G., et al.: Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of multiple sclerosis. Ann. Neurol. 50, 121–127 (2001)
Guideline 9C.: Guideline on short latency auditory evoked potentials. Am. Clin. Neurophysiol. Soc. (2008)
Movassat, M., Piri, N., AhmadAbadi, M.: Visual evoked potential study in multiple sclerosis disease. Iran. J. Ophthalmol. 21(4), 37–44 (2009)
Atanassov, K.: Generalized Nets. World Scientific, Singapore (1991)
Atanassov, K.: On Generalized Nets Theory. Prof. M. Drinov Academic Publishing House, Sofia (2007)
Todorova L., Vassilev, P., Ignatova, V.: A generalized net model for assessment of the degree of disability in patients with multiple sclerosis based on the abnormalities of visual evoked potentials. Issues in Intuitionistic Fuzzy Sets and Generalized Nets, vol 10, pp. 173–182 (2013)
Cuypers, M., Dickson, K., Pinckers, A., Thijssen, J., Hommes, O.: Discriminative power of visual evoked potential characteristics in multiple sclerosis. Doc. Ophthalmol. 90, 247–257 (1995)
Grover, L., Hood, D., Ghadiali, Q.: A comparison of mulrifocal and conventional visual evoked potential techniques in patients with optic neuritis/multiple sclerosis. Doc. Ophthalmol. 117(2), 121–128 (2008)
Ko, K.: The role of evoked potential and MR imaging in assessing multiple sclerosis: a comparative study. Singapore Med. J. 51(9), 716 (2010)
Balnyte, R., Uloziene, I., Rastenyte, D., et al.: Diagnostic value of conventional visual evoked potentials applied to patients with multiple sclerosis. Medicina (Kaunas) 47(5), 263–9 (2011)
Gnezditskiy, V.V., Korepina, O.S.: Atlas Po Vyzvannym Potentsialam Mozga, p. 532. PressSto, Ivanovo (2011)
Burina, A., Sinanovic, O., Smajlovich, D., et al.: Some aspects of balance disorder in patients with multiple sclerosis. Bosn. J. Basic Med. Sci. 8(1), 80–85 (2008)
Berger, J.R., Blum, A.S.: Somatosensory evoked potentials. The Clinical Neurophysiology Primer (2007)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Todorova, L., Ignatova, V., Hadjitodorov, S., Vassilev, P. (2016). Generalized Net Model for Monitoring the Degree of Disability in Patients With Multiple Sclerosis Based on Neurophysiologic Criteria. In: Angelov, P., Sotirov, S. (eds) Imprecision and Uncertainty in Information Representation and Processing. Studies in Fuzziness and Soft Computing, vol 332. Springer, Cham. https://doi.org/10.1007/978-3-319-26302-1_18
Download citation
DOI: https://doi.org/10.1007/978-3-319-26302-1_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26301-4
Online ISBN: 978-3-319-26302-1
eBook Packages: EngineeringEngineering (R0)