Abstract
Arterial switch operations undertaken in transposition of the great arteries (TGA) and Taussig Bing with ventricular septal defect (VSD) are complex. The association with an aortic arch obstruction (AAO), seen predominantly in Taussig-Bing increased significantly the complexity of the operation. One-stage neonatal repair has become the technique of reference. However, palliation remains indicated in newborns presenting with Swiss cheese VSDs, small birth weight and extra cardiac damages.
The increasing difficulties of the arterial switch operation in TGA/DORV-VSD are: the important diameter mismatch between the aorta and the pulmonary root, − the closure of the VSD, − the management of more complex coronary artery patterns, the association with AAO and the presence of a subaortic obstruction.
The ASO mortality, reported by the STS database congenital database is respectively 5 % for TGA/DORV-VSD without AAO and 12.6 % when an AAO is associated.
Late reoperations occur in 30 %, either: re-coarctation, right ventricular obstruction, aortic valve regurgitation, aortic root dilation and coronary stenosis. Long-term actuarial survival is 85 % at 15 years; nevertheless, close lifelong surveillance of these patients is necessary.
Complex arterial switch remain challenging and require a second learning curve.
Similar content being viewed by others
Keywords
- Congenital heart disease
- Congenital cardiac surgery
- Transposition of the great arteries
- Arterial switch operation
- Double outlet right ventricle
- Taussig-Bing
- Ventricular septal defect
- Aortic arch obstruction
- One stage repair
Background
This chapter will address the anatomical repair of complex switch, which include arterial switch undertaken in TGA-VSD and in Taussig-Bing with and without AAO.
The arterial switch operation (ASO), was first published by Adib Jatene [1, 2] in 1975 in two patients with transposition of the great vessels with ventricular septal defect (TGA-VSD). VSD is the most frequent associated lesion in complete transposition of the great arteries, with an incidence around 30 %. Taussig-Bing, defined as a double outlet right ventricle (DORV) subpulmonary VSD (see Chap. 23) is a more complex condition than TGA-VSD.
The association with an aortic arch obstruction (AAO) is seen in 20 % of TGA with VSD, and in 60 % of Taussig-Bing. AAO is also observed in 3 % of TGA with intact ventricular septum (TGA-IVS).
The association with AAO is a severe condition with a significant higher risk at repair. These complex lesions are today optimally treated by one stage neonatal ASO, requiring a well-experienced team. However palliation remains indicated in particular conditions.
Anatomic Classification
TGA- VSD
In TGA-VSD, the VSD can be located in any part of the inter-ventricular septum as in normally related great arteries; but is more frequently peri-membranous (Fig. 15.1a, b). Multiple and Swiss Cheese VSD represent 10 % and raise specific surgical issues. The aorta is usually anterior and to the right of the PA. Rarely the aorta can be partially located to the left of the PA [3]. There is always a significant aorto-pulmonary mismatch diameter, with the PA trunk being significantly larger than the diameter of the aorta. The PA is entirely located on the left ventricle and there is a mitro-pulmonary continuity. The coronary anatomy is similar to TGA-IVS (see Chap. 14).
Taussig-Bing (Figs. 15.2, 15.3, and 15.4)
DORV-TGA (Taussig Bing). Subpulmonary VSD. Cono-ventricular VSD above the anterior limb of the TSM. The great vessels are side by side. Large aorto-pulmonary diameter mismatch. Aortic arch obstruction. Shifting of the conal septum toward the subaortic conus. Double conus. The PA is partially “levoposed” on the left ventricle
Taussig Bing. Notice that the two great vessels are nearly 200 % on the right ventricle and that there is a mitro-pulmonary continuity. Anterior shifting of the conal septum. In green the ventricular septal defect with malaligned conal septum: the “hole” to close. In red the interventricular communication (RH Anderson): the “hole” not to close (Courtesy of Pr Yen Ho, Royal Brompton Hospital, London)
Taussig Bing (TB) is a form of DORV (see Chap. 23). The VSD is subpulmonary, close to the pulmonary annulus, and is located above the anterior limb of the trabecula septo marginalis (TSM) (Fig. 15.2). The aorta always arises totally from the RV and the pulmonary artery arises either partially [4, 5] or entirely [6] from the RV. There is constantly a double conus (Figs. 15.2 and 15.4). Mitro-pulmonary discontinuity is required for the diagnosis of TB [4, 6]. TB is different from DORV-non-committed VSD because in TB, the VSD is located close to the PA annulus and separated only by a distance less than an aortic annulus diameter [7]. The aorta is always located side by side to the PA with an important aorto-pulmonary diameter mismatch (Fig. 15.3). The coronary arteries patterns are more complex with frequent double looping courses (see Chap. 14). Either (Fig. 15.5a) with the RCA coming from the left-anterior sinus (sinus 1) and crossing in front of the aorta with the common left coronary trunk coming from the right-posterior sinus (sinus 2) and running behind the PA; sometimes named “inverted coronary arteries”. Or (Figs. 15.3 and 15.5b); with the LAD and RCA arising from the anterior sinus (sinus 1) and the circumflex arising alone from the posterior sinus (sinus 2) running behind the PA.
Double loop coronary artery patterns. Side by side vessels. (a) Inverted coronary arteries. RCA sinus 1: anterior loop. Common left trunk sinus 2: posterior loop. (b) RCA, LAD sinus 1: anterior loop. CX sinus 2: posterior loop. (c) The pulmonary trunk is transferred to the right PA to avoid a right coronary artery compression
The right ventricle is sometimes “smallish” (Fig. 15.3), but exceptionally hypoplastic in neonates in absence of associated organic tricuspid stenosis [12].
Multiple VSD are seen in 10 % of TB. Swiss cheese VSDs, defined as more than two VSD, should be detected prior to surgery because this association may contra-indicate one stage repair.
The two most specific cardiac associations in Taussig Bing are the presence of – an aortic arch obstruction and – a subaortic obstruction.
Aortic Arch Obstruction (AAO)
AAO is present in around 60 % of TB [8, 9] (Figs. 15.2 and 15.3). Less frequently, AAO is associated with TGA-VSD and TGA-IVS. The AAO is usually a coarctation with hypoplasia of the transverse arch or more rarely an interrupted aortic arch (10 %). The mismatch (Figs. 15.2 and 15.3) between the ascending aorta and the pulmonary artery is massive, with the pulmonary artery being twice or more than the diameter of the aorta.
Depending on publications, a subaortic obstruction is observed in 10 % [10] to 60 % [11], of the Taussig-Bing presenting with an AAO. It is in relation with: − a RVOT obstruction due the anterior shifting of the conal septum (Figs. 15.2 and 15.4) – and a potential hypoplasia of the aortic annulus. This subaortic obstruction will be “switched” into a subpulmonary obstruction after anatomical repair, which could require late reoperation [8].
Other Associated Lesions
Straddling AV valve is associated in 5 % of Taussig-Bing, involving either the tricuspid valve or the mitral valve. Only type C straddling [13] is an absolute contra-indication to anatomical repair.
Accessory mitral tissue, creating a subpulmonary obstruction is possible.
Di George syndrome with 22q11 deletion is observed in 10–20 %, and is more frequent in cases with aortic arch obstruction.
Imaging and Diagnosis
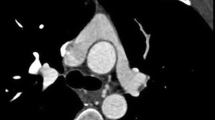
Echocardiography alone almost always provides a good anatomical evaluation of TGA-VSD [14] and Taussig Bing. The segmental and sequential analysis confirms the diagnosis of TGA. The location, size and numbers of VSD are defined. The diameter of the VSD is important information. When the VSD is less than 4 mm, the hemodynamics is similar to a TGA with intact septum, requiring an arterial switch within the first 2 weeks of life. The anatomy of the pulmonary valve is analyzed and the absence of LVOT obstruction confirmed. The magnitude of the trans-atrial shunting is assessed. An experienced echocardiography operator is able to describe with a good degree of accuracy the coronary anatomy and particularly detect the intramural courses.
In Taussig Bing [15], the echocardiography confirms: − the subpulmonary VSD, − the origin of both great vessels from the right ventricle and the partial levoposition of the PA when present, − the mitro-pulmonary discontinuity – and the presence of a double infundibulum.
The diagnosis of subaortic obstruction is only made by echography or CT scan, showing an anterior shifting of the conal septum toward the subaortic conus. The smallest size of the subaortic area is accurately measured to evaluate the severity of the subaortic stenosis. The catheterization will not show any obvious gradient, due to the large VSD shunt.
The diagnosis of aortic arch obstruction is also obtained by echocardiography. In newborn under Prostaglandin, the isthmus could be maintained open without evidence of isthmic coarctation. The presence of a hypoplasia of the transverse aortic arch is a clear landmark for an aortic arch obstruction.
Multiple or Swiss cheese VSD is a difficult diagnosis. It can be missed by the echocardiogram because the shunting from the large subpulmonary VSD masks any shunting in the muscular septum. Doppler could be misleading. The diagnostic of multiple muscular VSD relies on the presence of structural defects in analyzing all the muscular septum from the posterior to the anterior area, close to the anterior wall. Once suspected, the final diagnosis may require catheterization. CT scan could be also contributing.
Catheterization is useful to confirm multiple and Swiss cheese VSDs. It is requested in patients seen late, with suspicion of pulmonary vascular obstructive disease (see Chap. 16)
The indication of a Balloon Atrial Septostomy (BAS) depends on the quality of the atrial shunting and on the size of the VSD. In TGA-VSD without aortic arch obstruction (AAO), many centers perform a BAS and stop the Prostaglandin infusion in order to delay the surgery in insuring a good atrial mixing.
Prenatal diagnosis of TGA-VSD is achieved in more than half of the pregnancies. In utero transport, followed by delivery in a center close to a pediatric heart center, has decreased the mortality and the morbidity of the neonatal surgical repair [16]. Di George is frequent in presence of aortic arch obstruction.
Check List
-
Ventriculo arterial alignment (TGA or Taussig Bing)
-
Location of aorta (anterior and to the right, side by side)
-
Aorto-pulmonary diameter mismatch
-
Morphology of pulmonary valve
-
VSD location, diameter, VSDs number
-
Patency of ductus arteriosus
-
Coronary anatomy
-
Type of conus, mitro-pulmonary connection
-
Aortic arch obstruction, coarctation, hypoplastic arch, IAA
-
Subaortic obstruction: aortic valve and LVOT diameter
-
Straddling, overriding AV valves
-
Weight, prematurity, extra cardiac pathology
-
Di George
-
Irradiated blood
Surgical Techniques
Today the operation of reference for TGA-VSD and Taussig Bing, with or without AAO is a one-stage neonatal arterial switch operation (ASO) with VSD closure, with or without aortic arch repair. However, two stage operation remain indicated, depending on the center’s strategy, in presence of Swiss cheese VSD, very small weight and extracardiac damages.
Palliative Procedures
PA trunk banding by left thoracotomy [16] or sternotomy, has progressively been abandoned due to the risk of late aortic valve regurgitation after ASO [14, 15, 19]. It remains indicated in very small birth weight, or in patients presenting with associated extra cardiac lesions like intra cranial bleeding, necrotizing entero-colitis, major infections. It is contra-indicated in presence of subaortic obstruction.
The increased experience with PA branches banding, developed with the Hybrid type I palliation of HLHS, has been applied to TGA-VSD in order to preserve the future aortic valve. It has been used in presence of Swiss cheese VSD [20].
Aortic arch repair by left thoracotomy ± PA Banding was used at the beginning of the ASO experience in patients with TGA/DORV-VSD with aortic arch obstruction. The repair of the nearly constant hypoplasia of the aortic arch by thoracotomy is challenging and is frequently complicated by recurrent arch obstruction. The second stage ASO is often made more challenging. Due to the frequently associated subaortic obstruction, a PA banding is usually poorly tolerated.
Arterial switch with aortic arch repair associated with PA banding by sternotomy is the technique that we favor in case of Swiss Cheese VSD. See below.
One Stage Anatomical Repair of TGA-VSD and Taussig Bing
Cardio-Pulmonary Bypass (CPB) and Myocardial Protection
The CPB is run on full flow, with bicaval canulation and with antegrade cerebral perfusion when an arch repair is needed. The priming of the circuit today is less than 200 ml and includes packed red cells, plasma and/or albumin. Our preference is to use NTK-Custodiol crystalloid cardioplegia [12, 17]. Others favors warm blood cardioplegia and strict normothermia. Modified Ultra Filtration (MUF) is rarely used, while Conventional Ultra Filtration (CUF) is routinely applied.
ASO in TGA – VSD
The one stage repair is undertaken in the first 2 weeks of life.
The operation starts with the VSD patch closure. It is similar than in any VSD surgery. Perimembranous, outlet and mid trabecular VSD are closed through the tricuspid valve (Fig. 15.1). Different patch materials are used (Goretex, bovine pericardium, Dacron, etc…). Due to the fragility of the neonatal myocardium, a small needle is favored (7/0 Prolene, 6.5 needle, or 6/0 Prolene, 9 needle). Several pledgeted separate stitches, using 6/0 Premio ©, are useful. The rest of the patch is secured with a running suture. The ASO follows and needs to deal with an important mismatch in diameter between the aorta and the PA (See Chap. 14). TGA-VSD and Taussig Bing share the risk of late neo-aortic root dilation due to the large native pulmonary annulus. In this regard, we believe that the “trap-door” technique, which enlarges even more the neo-aortic root, should not be used.
ASO in Taussig Bing
The management of the VSD is clearly the most challenging part of the arterial switch operation. Due to the malalignement of the conal septum, the VSD is more difficult to treat. As shown in Fig. 15.4, the baffle patch needs to connect the left ventricle to the pulmonary artery, in closing the ventricular septal defect represented in green on Fig. 15.4; and not the interventricular communication, represented in red. Sometimes, the VSD could be closed through the tricuspid valve only. The trans-tricuspid approach, in incising the anterior tricuspid leaflet, offers a good access to the superior border of the VSD. In many instances, a double or triple approach is needed. We favor a technique with dual approach through the tricuspid and aortic valve after harvesting of the coronary buttons. Starting from the top, the superior part of the large patch is secured to the conal septum; then the operation is completed through the TV and the patch is secured to the inferior rim of the VSD with a running suture. We have abandoned the approach through the native pulmonary valve, which was associated with impairment of the neo-aortic valve [18].
The coronary transfer in Taussig-Bing is more complex due to the frequent presence of a double looping course (Fig. 15.5a, b). Due to the side by side vessels relationship, the right coronary (RCA) that is running in front of the reconstructed PA trunk, could be compressed. It is useful to transfer the pulmonary trunk to the right PA to prevent a compression of the RCA (Fig. 15.5c).
ASO in Taussig Bing with Aortic Arch Obstruction (Figs. 15.5 and 15.6)
Aortic arch repair. The coarctation is resected with all ductal tissue. The descending aorta is partially anastomosed directly to the transverse arch. A large patch of either pulmonary homograft or bovine pericardium is used to enlarge the arch and the ascending aorta so as to control the mismatch between the ascending aorta and the neo-pulmonary root
The one stage repair of ASO + AAA repair and VSD closure is undertalken in the first week of life, through sternotomy.
We routinely used antegrade cerebral perfusion and have abandoned circulatory arrest. The CPB is run around 20–25° Celsius at a flow of 50 ml/kg/min. The arch is repaired first. As shown in Fig. 15.6, a large patch of either homograft or bovine pericardium is used to enlarge together the transverse aortic arch and the ascending aorta; so as to normalize the diameter of the distal ascending aorta to fit the enlargement of the pulmonary artery.
The subaortic obstruction (Figs. 15.2 and 15.4) could be absent or reduced [8, 12] to small muscular bands in the subaortic infundibulum that are resected through the native aortic valve [10, 15, 17]. Elsewhere it can be important, requiring a right ventriculotomy with resection of the parietal band and patch enlargement of the infundibulum [12]. The challenge is major in some interrupted arch with hypoplasia of the aortic annulus. The presence of an anterior loop with the RCA crossing the infundibulum, close to the aortic annulus forbids a transection of the annulus and force is to place a small RV to PA conduit, usually a Goretex 5 [12]. In any case, the small aortic annulus will become a small PA annulus with ultimate risk of RVOT obstruction [12, 21].
Management of TGA/DORV with Multiple VSD
Apical muscular VSD and Swiss cheese VSD, defined as more than two VSDs, are very challenging to repair in neonates. Our strategy has been to perform a palliative first stage arterial switch. The ASO is performed, the arch is repaired accordingly and a PA banding on the reconstructed PA trunk is applied. The VSDs are left intact. There is a triple advantage of doing an arterial switch: − first the PA banding is placed on the final PA and preserve the neo-aortic valve, − second, the shifting of the conal septum is no more a contra-indication to PA banding and –third, a normal physiology and mixing are restored. The second stage, undertaken several months later, is to close the multiple VSD. The ultimate Swiss cheese VSD closure is frequently a hybrid procedure, with surgical closure of the cono-ventricular VSD and device closure of the muscular VSDs. Due to the PA banding, late re-operation on the RVOT could not be excluded.
The Case of TGA-IVS Associated with AAO
This association is rare and a source of complication. The presence of a coarctation could be “missed” because the isthmus is maintained opened under Prostaglandin. The only landmark of an associated coarctation could be some hypoplasia of the transverse arch and a smallish isthmus. The coarctation may then become obvious in the hours or days following the post-operative course, with elevated arterial pressure , absent of femoral pulses and low cardiac output syndrome. Urgent coarctation repair is requested by left thoracotomy without CPB.
This association is to be detected prior to the ASO. Our strategy to interrupt the Prostaglandin in TGA-IVS when the atrial mixing is satisfactory gives time for the isthmus to narrow and secure the diagnosis. When the SaO2 is to low, due to poor atrial mixing, a balloon atrial septostomy is routinely performed.
Kawashima Operation
This technique proposed for Taussig-Bing, which tunnelized the VSD to the aorta, requires the resection of the conal septum and is therefore very challenging in neonates. It was abandoned by most centers in favor of one-stage ASO [14, 15].
Outcomes
The hospital mortality of the arterial switch at the EACTS-ECHSA Congenital Database [22] (see Chap. 4), for the period 2010–2013, is: 2.6 % for TGA-IVS, 5 % for TGA-VSD and 11.3 % for TGA/DORV-VSD with AAO.
The striking five times increased mortality of TGA/DORV-VSD with AAO compared to TGA-IVS reflects the challenge of the ASO in presence of aortic arch obstruction. The two times elevated hospital mortality of ASO in TGA-VSD compared to ASO in TGA-IVS is believed to be related to the VSD closure particularly in Taussig-Bing [23].
In recent series, the hospital mortality of the ASO in TGA – VSD and Taussig Bing with and without AAO is below 5 % [17, 19]. Swiss cheese VSDs and small birth weight remain risk factors [23] for early mortality. The complexity of the coronary artery patterns is not anymore a risk factor in most centers [24].
The long term results of ASO for Taussig-Bing are today available [11, 19]. Survival is over 85 % at 15 years. Most patients are in NYHA class 1, they are in sinus rhythm and the biventricular function is preserved in 95 %. Nevertheless, the risk of reoperation either surgery or interventional cardiology, is significant and is around 30 %. Mainly due to RVOT obstruction [21], re-coarctation, coronary stenosis, aortic valve regurgitation. Aortic root dilation is favored by the aorto-pulmonary diameter mismatch [11, 25], it may require re-operation in the long term, No aortic rupture are so far described (see Chap. 34).
Performing a control coronarography or CT angiogram in patients with complex coronary anatomy (double loop and intramural course) is our current practice. Therefore, close lifelong surveillance of these patients is necessary.
References
Jatene AD, Fontes VF, Paulista PP, de Souza LC, Neger F, Galantier M, Souza JE. Successful anatomic correction of transposition of the great vessels. A preliminary report. Arq Bras Cardiol. 1975;28:461–4.
Jatene AD, Fontes VF, Paulista PP, Souza LC, Neger F, Galantier M, Sousa JE. Anatomic correction of transposition of the great vessels. J Thorac Cardiovasc Surg. 1976;72:364–70.
Houyel L, Van Praagh R, Lacour-Gayet F, Serraf A, Petit J, Bruniaux J, Planché C. Transposition of the great arteries [S, D, L]. Pathologic anatomy, diagnosis, and surgical management of a newly recognized complex. J Thorac Cardiovasc Surg. 1995;110:613–24.
Taussig HB, Bing RJ. Complete transposition of aorta and levoposition of pulmonary artery. Am Heart J. 1949;37:551–7.
Stellin G, Zuberbuhler JR, Anderson RH, Siewers RD. The surgical anatomy of the Taussig-Bing malformation. J Thorac Cardiovasc Surg. 1987;93:560–9.
Van Praagh R. What is the Taussig Bing malformation? Circulation. 1968;38:445–9.
Belli E, Lacour-Gayet F, Serraf A, et al. Double-outlet right ventricle with non-committed ventricular septal defect. Eur J Cardiothorac Surg. 1999;15:747–52.
Lacour-Gayet F, Serraf A, Galletti L, et al. Biventricular repair of conotruncal anomalies associated with aortic arch obstruction: 103 patients. Circulation. 1997;96(Suppl II):328–34.
Alsoufi B, Cai S, Williams WG, Coles JG, Caldarone CA, Redington AM, Van Arsdell GS. Improved results with single-stage total correction of Taussig-Bing anomaly. Eur J Cardiothorac Surg. 2008;33:244–50.
Comas JV, Mignosa C, Cochrane AD, Wilkinson JL, Karl TR. Taussig-Bing anomaly and arterial switch: aortic arch obstruction does not influence outcome. Eur J Cardiothorac Surg. 1996;10:1114–9.
Schwarz F, Blaschczok HC, Sinzobahamvya N, Sata S, Korn F, Weber A, Asfour B, Hraska V. The Taussig-Bing anomaly: long-term results. Eur J Cardiothorac Surg. 2013;44:821–7.
Lacour-Gayet F. Arterial switch operation with VSD and aortic arch reconstruction. Semin Thorac Cardiovasc Surg. 2007;19:245–8.
Piot JD, Rey C, Serraf A, Touchot A, Sousa Uva M, Lacour-Gayet F, Planché C. Transposition of great vessels with anomaly of the atrioventricular valves or chordae: echocardiographic aspects and surgical correlations. Arch Mal Coeur Vaiss. 1995;88:699–704.
Serraf A, Comas JV, Lacour-Gayet F, Bruniaux J, Bouchart F, Planché C. Neonatal anatomic repair of transposition of the great arteries and ventricular septal defect. Eur J Cardiothorac Surg. 1992;6:630–4.
Serraf A, Lacour-Gayet F, Bruniaux J, Losay J, Petit J, Touchot-Kone A, Bouchart F, Planche C. Anatomic repair of Taussig-Bing hearts. Circulation. 1991;84(5 Suppl):III200–5.
Bonnet D, Coltri A, Butera G, Fermont L, Le Bidois J, Kachaner J, Sidi D. Detection of transposition of the great arteries in fetuses reduces neonatal morbidity and mortality. Circulation. 1999;99:916–8.
Stoica S, Campbell D, Lacour-Gayet F, et al. Morbidity of the arterial switch operation. Ann Thorac Surg. 2012;93:1977–83.
Mohammadi S, Belli E, Aupecle B, Lacour-Gayet F, et al. Left-sided lesions after anatomic repair of transposition of the great arteries, ventricular septal defect, and coarctation: surgical factors. J Thorac Cardiovasc Surg. 2004;128(1):44–52.
Hayes D, Jones S, Bacha E, Richmond ME, Andrews HF, Glickstein JS, Chen JM, Liberman L. Primary arterial switch operation as a strategy for total correction of Taussig − Bing anomaly: a 21-year experience. Circulation. 2013;128:S194–8.
Weinstein S, Liveris A, Shenoy RU, Lacour-Gayet F. Bilateral pulmonary arterial banding for complex transposition of the great arteries. J Thorac Cardiovasc Surg. 2013;145(3):876–8.
Sinzobahamvya N, Blaschczok HC, Asfour B, Arenz C, Jussli MJ, Schindler E, Photiadis J, Urban AE. Right ventricular outflow tract obstruction after arterial switch operation for the Taussig-Bing heart. Eur J Cardiothorac Surg. 2007;31(5):873–8.
EACTS-ECHSA congenital database. Free access on line http://www.eactscongenitaldb.org/index.php?LANG=en&level=2&struct=14_1.
Lacour-Gayet F. Complexity stratification of the arterial switch operation: a second learning curve. Cardiol Young. 2012;22(6):739–44.
Lacour-Gayet F, Anderson RH. A uniform surgical technique for transfer of both simple and complex patterns of the coronary arteries during the arterial switch procedure. Cardiol Young. 2005;15(S1):93–101.
Koolbergen DR, Manshanden JS, Yazdanbakhsh AP, Bouma BJ, Blom NA, de Mol BA, Mulder BJ, Hazekamp MG. Reoperation for neoaortic root pathology after the arterial switch operation. Eur J Cardiothorac Surg. 2014;46(3):474–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Lacour-Gayet, F., Belli, E., Ghez, O. (2016). Arterial Switch for TGA or DORV and VSD, with and Without Aortic Arch Obstruction. In: Lacour-Gayet, F., Bove, E., Hraška, V., Morell, V., Spray, T. (eds) Surgery of Conotruncal Anomalies. Springer, Cham. https://doi.org/10.1007/978-3-319-23057-3_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-23057-3_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-23056-6
Online ISBN: 978-3-319-23057-3
eBook Packages: MedicineMedicine (R0)