Abstract
A great variety of applications for mobile devices are designed to support users during medical intake. One of these applications is ‘Medication Plan’ which aims at supporting regular and correct intake of medication and documentation of vital parameters. The purpose of this study is to examine the influence of demographic and health-related factors on user behavior and patterns of use. The application was available free of charge between 2010 and 2012 in the Apple™-App-Store™. The study is based on data collected via an online questionnaire. In total 1799 participants generated 1708 complete data sets. 69 % of the users (74 % male) with a median age of 45 applied ‘Medication Plan’ for more than one day. The mean duration of application increased substantially with age (< 21 years = 23.3 days; > 60 years = 103.9 days). However, other demographic factors (sex, educational status etc.) had no effect on usage intensity. Users with complicated medical treatment or aged > 60 years applied the application for 3 month on average. This is a promising trend towards the support treatment of chronic conditions with mobile applications.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Patients with chronic illnesses such as hypertension and chronic kidney disease are often burdened by high comorbidity and reduced awareness of their medical conditions, which creates a challenging environment in which to promote medication compliance [1]. Complexities of daily life, shifting priorities, and frequent poly-pharmacy likely contribute to patients’ inability to deal adequately with their medical conditions. Frequent encounters with the medical system, which result in dosage adjustments, add to the problems with medication compliance in these patients [2]. For the individual, non-adherence is associated with a number a safety issues such as increased risk of toxicity or more severe relapses [3]. For the health system in Germany alone, direct and indirect costs of non-adherence amount to approximately 7.5 to 10 billion Euros every year [4, 5]. Therefore novel strategies are required to address the needs of chronically ill patients and reduce. Mobile information technology may offer new system solutions to better meet these requirements. With more than 1 billion users having access to mobile broadband internet and a rapidly growing mobile app market, all stakeholders involved have high hopes that this technology may improve health care [6, 7]. Expectations range from overcoming structural barriers to access in low-income countries to more effective, interactive treatment of chronic conditions. Yet previous work suggests that even when sophisticated technology is available, older users (e.g., age 50 and above) find their initial experiences with medication applications frustrating [8]. The iNephro study introduced a “native” smartphone application (“Medication Plan”), which allowed users to maintain and alter personal drug therapy plans and document vital signs on their personal device [9]. Initial findings showed that the regular use of the application decreased considerably within the first 2 months. This paper presents a further analysis to better understand what is generally referred to as “attrition of app usage”.
Pre-specified endpoints were used to identify user data with regards to demographic- and health-related factors associated with “duration of usage” and “intensity of usage per day” of the mobile application “Medication Plan”.
2 Materials and Methods
The Department of Nephrology of the University Hospital Essen, Germany, developed and provided the “Medication Plan” application for the iOS platform in 2010 [10]. This native smartphone application allowed users to maintain and alter a drug therapy plan on their personal device (Fig. 1). Between December 2010 and January 2012 it was available free of charge for download in the German-language App Store™ by Apple™. Users were able to specify intake requirements according to the medication regimen issued by the prescribing physician and the patients’ own personal needs (see tutorial at http://www.youtube.com/watch?v=nui78JqwMHE). A reminder function and local push-notification alerts reminded users to take their medications at a pre-specified time. No permanent internet connection was necessary and all data were stored locally on the device itself, reducing the possibility of erroneous transmission of personal health information. Users could enter vital sign data, and trends were presented graphically. Prior to using the application, users had to give their consent to a disclaimer as well as an agreement for a subsequent anonymous analysis of user data and this was done via activation of a hyperlink (implementation by QUEST objects GmbH, Tübingen). Additionally, users were invited to voluntarily and anonymously complete an online questionnaire, which had to be actively accessed via an additional hyperlink. The unique identifier numbers (UDID) of the respective iPhones™ were irreversibly encrypted by a MD5 message-digest algorithm (MD5-Hash).
Generating a medication plan on the smartphone ([9])
The activity of the encrypted UDID was then tracked (“creation”, “modification”, or “deletion” of drug information, as well as the “confirmation” of drug adherence within the application “Medication Plan”). Activity of the respective, encrypted UDID addresses and if available, associated demographic information, were analyzed using self-implemented software of Fraunhofer ISST, Dortmund, Germany. Further statistical analysis was performed using SPSS® 21.0 (IBM®, U.S.A.): A multi-factorial analysis of variance (ANOVA) and chi-square test for the response variables with a significance level of 0.05 was conducted. The distributions of the groups were normal and the homogeneity of variances for the data analyzed was confirmed.
Following the APA guidelines the exact error probability p was specified for each analysis [11]. Dependent variables were “duration of long-term usage” (defined as use of > 1 per day; if no activity was recorded for > 10 days, this was rated as end of use) and “mean intensity of usage per day” during time of active usage.
Ethics: The Ethics Committee of the Medical Faculty of Essen University was consulted and a formal written waiver for the need of ethics approval was issued (13-5373-BO).
3 Results
Overall, activity of 1799 (1708 complete data sets) users was recorded between December 2010 and April 2012 (Table 1). More than two thirds of users (1183/1708) used “Medication Plan” for more than a day. There was a significant association between gender and amount of long-term and short-term users (χ2 (1, N = 1761) = 6.715, p < 0.010). Looking at the different age cohorts, there was a significant difference between age groups regarding the amount of long-term and short-term users (> 1 day) (χ2 (5, N = 1799) = 15.255, p < 0.001).
With rising age, the amount of long-term users rose from 50 % of those below 21 years of age to over 70 % for those aged 40 years or older, yet the effect was stronger in men for all age cohorts (Fig. 2).
The number of diseases for each user significantly affected duration of usage (χ2 (5, N = 1799) = 12.144, p = 0.030). While the proportion of individuals who stopped using the app after one day was 42 % for those that did not have to take any drugs, it was between 25 and 30 %, for those who were on regular medication. Similarly, the number of drugs significantly affected the duration of usage (χ2 (7, N = 1799) = 30.612, p < 0.001). This effect is not surprising, as for users without any medical condition or the need to take drugs on a regular schedule, only a fraction of the available functionality was still useful (e.g. keeping track of weight and vital parameters).
Variance analysis presented the following effects with respect to duration of usage: With a mean duration of usage of 23.3 days (SD = 36.9) by users < 21 years, there was a substantial increase over all age cohorts up to users of 60 years and above using the application for 103.9 days on average (SD = 20.7) (F = 2.581; df = 5; p = 0.025). For users aged 50 and older, the usage duration remained static.
A post hoc pairwise analysis with Bonferroni correction showed significant differences between all age groups concerning usage duration with a minimum age difference of 20 years. I.e. users aged 50 used the app substantially more than those aged 30. Mean duration of usage, for users who did not abandon the application within the first day, was 85.4 days (SD 138.6) (Fig. 3). Sex (F = 1.084; df = 1; p = 0.298) and educational attainment (F = 0.656; df = 2; p = 0.519) had no effect for those that did not cease to use the application after one day.
The number of medical conditions (F = 0.403; df = 5; p = 0.847) as well as the number of drugs taken per day on a regular schedule (F = 0.967; df = 7; p = 0.259) did not affect the duration of usage significantly.
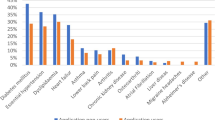
Interestingly, variance-analysis of the individual medical conditions showed a significant effect on duration of usage if the user suffered from cardiovascular disease (F = 14.098; df = 1; p < 0.001) or had received a transplant (F = 12.503; df = 1; p < 0.001) (Fig. 4).
In either case, people with these a diseases used the system on average about 50 % longer compared to people not suffering from the same condition. Diabetes (F = 2.699; df = 1; p = 0.101), lung disease (F = 0.411; df = 1; p = 0.522) and liver disease had no significant impact on duration of usage (F = 2.221; df = 1; p = 0.136).
With regard to usage intensity, the number of diseases tended to affect usage intensity (F = 1.974; df = 5; p = 0.080). The number of regularly taken drugs had significant impact on usage intensity (F = 4.017; df = 7; p < 0.001) and increased with the number of drugs taken per day (Fig. 5).
Demographic predictors such as sex (F = 0.874; df = 1; p = 0.350), age (F = 0.646; df = 5; p = 0.665) and educational attainment (F = 0.905; df = 2; p = 0.405) showed no significant effect.
4 Discussion
As far as we know our presented study is the first to describe the usage of a medication adherence-tool in a representative sample. More than 2/3 of users continued using “Medication Plan” after the first day. Over the entire study population, use of the application for more than one day grew with increasing age, yet the effect was greater in men over all age cohorts.
Once a user decided to log into the application, further factors (disease and associated medication) had an effect on the usage-duration and -intensity. Such findings may provide useful insights into behavioral-patterns of designated patient groups and assist in the design of effective interventions.
4.1 Brief Review of Findings and Comparison to Prior Studies
Thus far, most users of publicly available, health related, mobile communication services seem to have been “early adopters”: middle-aged, male, well-educated and comparatively healthy [9, 12–14]. Furthermore, high attrition rates for internet interventions were reported, which may reflect deficits in usability or an early interest in the novelty of the application, with a declining eagerness as the newness of the intervention wears off [9, 15, 16].
The question that arises is whether mobile technology to support drug adherence is indeed an appropriate tool to support elderly patients with polypharmacy. So far, this issue has mostly been assessed indirectly via questionnaires [17–19]. Direct assessment of user activity can offer objective and more accurate data on the usefulness of a mobile application. Our findings offer new insights into what has been termed the “digital divide” [13, 14], a term coined by developers, which implies, that compared with the younger generation, older individuals are less likely to make extensive use of digital technology [8, 20]. Whereas our data show a strong effect of the variables “age” and “disease” on amount of LT/ST users (actually it is the same as duration only in form of an ordinal variable), “polypharmacy” was identified as the primary influence for the intensity of usage. No effects were identified for educational status.
Our findings contradict any generalized assumption implying “digital disengagement of the elderly”. We have shown that for smartphone users, “increasing age” or “polypharmacy” are good predictors for acceptance of mobile technology when it comes to supporting adherence. The findings lead to the question whether drug adherence can eventually be improved for smartphone users. The Technology Acceptance Model suggests that acceptance depends on a user’s perception of the usefulness and ease of use of a system [21]. Similarly, the diffusion of innovation model emphasizes that a new technology needs to offer a “relative advantage” over the status quo [22].
Together with previous findings suggesting that increasing age [23–25] and polypharmacy [26] negatively affect adherence, one may assume that the use of applications like “Medication Plan” will eventually improve drug adherence. In our investigation the lack of perceived usefulness or relative advantage likely was the reason for relative early cessation of app usage by patients stating to be suffering from diabetes is a point in proof [27]. “Medication Plan” did not offer many of these users the required added value such as a combined documentation of blood sugar, bread units consumed or administered doses of insulin. This finding demonstrates how important it is to bear in mind specific needs of users to achieve acceptance [28].
Furthermore, the success of “Medication Plan” with its very practical aspects of drug regimen management supports the concept of ‘small data’ [29], suggesting that people mainly need technology to help them make sense of their health condition, and to offer actionable steps. On another note, even though the three main drivers of adherence to chronic disease medication were identified as perceived concerns about medications, perceived need for medications, and perceived affordability of medications [30], it appears that practical support and reminders, while not directly targeting those issues, can still go a long way toward self-reported drug adherence.
Lastly it seems that the focus of iNephro on practicality and its main purpose to help users overcome the current barriers to health literacy were recognized and are mirrored by our results [31].
4.2 Strengths and Limitations
Despite evidence from pilot studies, most mHealth interventions can be seen as the equivalent of black boxes [19]. The problem of these studies is that a particular style of a black box application is compared to a situation without any black box application. This study presents a novel approach to directly assess usage and acceptance of mobile technology in the context of drug adherence.
Our elderly iPhone™ users can be seen as technologically savvy in the first place and findings may not apply across the entire population [32]. Age-related changes in hearing, vision, cognition, and mobility require special consideration and application designers need to take this into account.
Elderly patients tend to be more reserved towards the use of technology since they usually feel barriers to start using it [33]. Unless they see a clear benefit for themselves, older adults are less likely to adopt new technology [28].
5 Conclusion
The famous statement by Dr. Everett Koop, former U.S. Surgeon General, “Drugs don’t work in patients who don’t take them” may also be true for mobile medication management applications [8]. We were able to show that elderly, technologically savvy users, requiring polypharmacy, relied on a mobile application to support drug adherence and that the degree of engagement depended on disease/therapy-related as well as demographic factors.
With this knowledge, similar tools could be valuable in the drug management of these patients. However, particularly in elderly patients, drug adherence is a complex problem, requiring not only a trust based doctor-patient relationship but rather multidimensional approaches. These range from simplified therapy-regimes and sustained understanding of the disease on the patients’ side to technological support including companion pillbox and communication devices.
Applications will have to be tailored closely to the specific demands of sick individuals to be accepted as part of their often complicated day-to day routines [34, 35]. Hence, interdisciplinary approaches and a profound understanding of the context and patients’ needs are vital for successful realization of technological solutions and investments in the field [7, 36].
References
Vrijens, B., Vincze, G., Kristanto, P., Urquhart, J., Burinier, M.: Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ 336, 1114–1117 (2008)
Osterberg, L., Blaschke, T.: Adherence to medication. N. Engl. J. Med. 353, 487–497 (2005)
De Geest, S., Sabaté, E.: Adherence to long-term therapies: evidence for action. Eur. J. Cardiovasc. Nurs. 2(4), 323 (2003)
Volmer, T., Kielhorn, A.: Kosten der non-compliance. Gesundheitsökonomisches Qualitätsmanagement 4, 55–61 (1999)
Gräf, M.: Die volkswirtschaftlichen Kosten der Non-Compliance: Eine entscheidungsorientierte Analyse. P.C.O.-Verlag, Bayreuth (2007)
Diamantidis, C.J., Becker, S.: Health information technology (IT) to improve the care of patients with chronic kidney disease (CKD). BMC Nephrol. 15(1), 7 (2014)
Becker, S., Miron-Shatz, T., Schumacher, N., Krocza, J., Diamantidis, C.J., Albrecht, U.-V.: mHealth 2.0: experiences, possibilities, and perspectives. JMIR mHealth uHealth 2(2), e24 (2014)
Grindrod, K.A., Li, M., Gates, A.: Evaluating user perceptions of mobile medication management applications with older adults: a usability study. JMIR mHealth uHealth 2(1), e11 (2014)
Becker, S., Kribben, A., Meister, S., Diamantidis, C.J., Unger, N., Mitchell, A.: User profiles of a smartphone application to support drug adherence-experiences from the iNephro project. PLoS ONE 8(10), e78547 (2013)
Charland, A., Leroux, B.: Mobile application development: web vs. native. Commun. ACM 54(5), 49–53 (2014)
APA - American Psychological Association: Publication Manual of the American Psychological Association, 6. Edition. American Psychological Association, Washington (2009)
Smith, A.: http://pewinternet.org/~/media/Files/Reports/2012/Smartphone%ownership%202012.pdf
Sarkar, U., Karter, A.J., Liu, J.Y., Adler, N.E., Nguyen, R., Lopez, A., Schillinger, D.: Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J. Am. Med. Inform. Assoc. 18(3), 318–321 (2011)
Lorence, D.P., Park, H., Fox, S.: Racial disparities in health information access: resilience of the digital divide. J. Med. Syst. 30(4), 241–249 (2006)
Boulos, M.N., Wheeler, S., Tavares, C., Jones, R.: How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed. Eng. Online 10, 24 (2011)
Consumer Health Information Corporation. http://www.consumerhealth.com/press/2008/NewsReleaseSmartPhoneApps.php
Free, C., Phillips, G., Galli, L., Watson, L., Felix, L., Edwards, P., Patel, V., Haines, A.: The effectiveness of mobile-health technology-based health behavior change or disease management interventions for health care consumers: a systematic review. PLoS Med. 10(1), e1001362 (2013)
Tomlinson, M., Rotheram-Borus, M.J., Swartz, L., Tsai, A.C.: Scaling up mHealth: where is the evidence? PLoS Med. 10(2), e1001382 (2013)
Lester, R.T., Ritvo, P., Mills, E.J., Kariri, A., Karanja, S., Chung, M.H., Jack, W., Habyari, J., Habyarimana, J., Sadatsafavi, M., Najafzadeh, M., Marra, C.A., Estambale, B., Ngugi, E., Ball, T.B., Thabane, L., Gelmon, L.J., Kimani, J., Ackers, M., Plummer, F.A.: Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya: a randomised trial. Lancet 376(9755), 1807–1808 (2010)
Olphert, W., Damodaran, L.: Older people and digital disengagement: a fourth digital divide? Gerontology 59(6), 564–570 (2013)
Davis, F.D., Bagozzi, R.P., Warshaw, P.R.: User acceptance of computer technology: a comparison of two theoretical models. Manage. Sci. 35(8), 982–1003 (1989)
Rogers, E.M.: Diffusion of Innovations, 5th edn. Free Press, New York (2003)
Morris, A.B., Li, J., Kroenke, K., Bruner-England, T.E., Young, J.M., Murray, M.D.: Factors associated with drug adherence and blood pressure control in patients with hypertension. Pharmacotherapy 26(4), 483–492 (2006)
Pechère, J.C., Hughes, D., Kardas, P., Cornaglia, G.: Noncompliance with antibiotic therapy for acute community infections: a global survey. Int. J. Antimicrob. Agents 29(3), 245–253 (2007)
Siegel, D., Lopez, J., Meier, J.: Antihypertensive medication adherence in the department of veterans affairs. Am. J. Med. 120(1), 26–32 (2007)
Bjerrum, L., Søgaard, J., Hallas, J., Kragstrup, J.: Polypharmacy: correlations with sex, age and druge regimen. a prescription database study. Euro. J. Clin. Pharmacol. 54(3), 197–202 (1998)
Heinz, M., Martin, P., Margrett, J.A., Yearns, M., Franke, W., Yang, H.-I., Wong, J., Chang, C.K.: Perceptions of technology among older adults. J. Geront. Nurs. 39(1), 42–51 (2013)
Or, C.K., Karsh, B.-T., Severtson, D.J., Burke, L.J., Brown, R.L., Brennan, P.F.: Factors affecting home care patients’ acceptance of a web-based interactive self-management technology. J. Am. Med. Inform. Assoc. 18(1), 51–59 (2010)
Hansen, M.M., Miron-Shatz, T., Lau, A.Y.S., Paton, C.: Big data in science and healthcare: a review of recent literature and perspectives. In: Contribution of the IMIA Social Media Working Group. IMIA (International Medical Informatics Association) Yearbook of Medical Informatics. Yearb Med Inform (2014)
McHorney, C.A.: The adherence estimator: a brief, proximal screener for patient propensity to adhere to prescription medications for chronic disease. Curr. Med. Res. Opin.® 25(1), 215–238 (2009)
Miron-Shatz, T., Elwyn, G.: To serve and protect? Electronic health records pose challenges for privacy, autonomy and person-centered medicine. Int. J. Patient Centered Med. 1, 405–409 (2011)
Hixon, T.: http://www.forbes.com/sites/toddhixon/2014/04/10/what-kind-of-person-prefers-aniphone
Tacken, M., Marcellini, F., Mollenkopf, H., Ruoppila, I., Szeman, Z.: Use and acceptance of new technology by older people. Findings of the international MOBILATE survey: ‘Enhancing mobility in later life’. Gerontechnology 3(3), 126–137 (2005)
Diamantidis, C.J., Zuckerman, M., Fink, W., Aggarwal, S., Prakash, D.: Usability testing and acceptance of an electronic medication inquiry system for CKD patients. Am. J. Kidney Dis. Official J. Nat. Kidney Found. 61(4), 644–646 (2013)
Diamantidis, C.J., Zuckerman, M., Fink, W., Hu, P., Yang, S., Fink, J.C.: Usability of a CKD educational website targeted to patients and their family members. Clin. J. Am. Soc. Nep. 7(10), 1553–1560 (2012)
Miron-Shatz, T., Shatz, I., Becker, S., Patel, J., Eysenbach, G.: Promoting business and entrepreneurial awareness in healthcare professionals: lessons from venture capital panels in medicine 2.0 conferences. J. Med. Internet Res. 16(8), e184 (2014)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this paper
Cite this paper
Mertens, A., Rasche, P., Theis, S., Wille, M., Schlick, C., Becker, S. (2015). Influence of Mobile ICT on the Adherence of Elderly People with Chronic Diseases. In: Zhou, J., Salvendy, G. (eds) Human Aspects of IT for the Aged Population. Design for Everyday Life. ITAP 2015. Lecture Notes in Computer Science(), vol 9194. Springer, Cham. https://doi.org/10.1007/978-3-319-20913-5_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-20913-5_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20912-8
Online ISBN: 978-3-319-20913-5
eBook Packages: Computer ScienceComputer Science (R0)