Abstract
An influenza epidemic is a complicated phenomenon influenced by numerous social and biological factors, including geography, climate, population, transport network, and biological statuses of humans and viruses, among others. To investigate the strength of these influences, we evaluated data from influenza epidemics that occurred in Japan between April 1999 and December 2014 using wavelet analysis. We calculated wavelet transform and phase difference, which was defined as the phase difference in a prefecture other than Tokyo. The time-averaged phase differences revealed the following: (1) the epidemics were earlier and more strongly synchronized in 7 prefectures in the Kanto region, which includes Tokyo, and in 7 prefectures in the Kinki region, which includes Osaka; (2) except for these urban regions, the epidemics propagated from western to eastern prefectures, and finally to northern prefectures; (3) epidemic jumps occurred in several prefectures (e.g., Miyagi Prefecture); and (4) epidemics occasionally occurred at different times in two adjacent prefectures (e.g., Yamanashi and Tokyo). We then attempted to qualitatively deduce the causes for these observations. This study is expected to be important for integrating knowledge to derive trends in epidemics, both nationally and internationally.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Spreading patterns of influenza epidemics, e.g., from city to city, are of great concern because they are important from the viewpoint of not only scientific interest, but also of public health [1, 2]. Public health is associated with intervention or control of epidemics, including vaccinations, masks, and the spatiotemporally precise distribution of drug stockpiles. Studies of spreading patterns may also be useful for outbreaks of new types or strains of influenza. Scientific interest primarily relates to the social sciences. The manner in which epidemics propagate must reflect the static and dynamic structures of a society, i.e., forms of human social interaction such as population distribution, transport networks, availability of medical services, and personal travel.
Although epidemic spread is likely affected by stochastic factors, some regularities are evident in the epidemic data. It is important to identify such regularities through quantitative analysis, and then to investigate the causes of these regularities. To date, spatiotemporal analyses of influenza epidemics have been performed in France [3, 4], Scotland [5], 20 European countries [6], Australia [4], Brazil [7], the United States [4, 8–11], China [12], and Japan [13, 14]. These studies identified several regularities in influenza epidemics: west-to-east spread of peak influenza activity, spatiotemporal epidemic synchrony, close correlation with movement of people, relation with mortality pattern, and so on.
Our concern here is whether we can also detect such regularities in influenza epidemics in Japan. If there are regularities, are they similar to or different from those found in other countries? It is interesting to investigate relations of influenza epidemics with effects of environmental characteristics in Japan (described in Sec. 15.2). While Sakai et al. examined the influenza epidemic data in Japan from 1992 to December 1999, using the Kriging method [13], the present study has investigated data from 1999 to 2014, using wavelet analysis. The difference of the data period and analysis is also intriguing. Only a few spatiotemporal studies of influenza epidemics have been performed, and thus the present study is expected to be valuable for integrating knowledge and exploring general regularities in influenza epidemics.
2 Materials and Methods
2.1 Case Report Data
The present study analyzed weekly case report data for influenza from 46 prefectures in Japan from April 1999 to December 2014 [15] (Okinawa Prefecture was excluded because it comprises remote islands and is located in a subtropical climate with epidemic patterns vastly different from those in the other prefectures). A few typical time series are depicted in Fig. 15.1. For data collection, we used sentinel (or fixed-point) reports: reports are provided by physicians in medical institutions that are assigned and obliged by the government to report how many cases they diagnose.
2.2 Wavelet Analysis
In contrast to Fourier analysis, wavelet analysis [16–18] derives transient relationships between non-stationary time series data. Long-term variations in demography and/or climate affect the epidemic spread of infectious diseases. A few previous studies have examined various diseases using this technique [19–22]. Influenza epidemics are also greatly affected by biological factors. The strain of influenza virus varies annually, and the force of infection depends on the strain. Therefore, the magnitude of infection is different each year. Due to these non-stationary effects, wavelet analysis is well suited to the analysis of influenza epidemics.
The wavelet transform reads
where x n , s, and δ t denote discrete time series (i.e., influenza case data), wavelet scale, and time interval of time-series (δ t = 1 week), respectively. While the choice of a wavelet ψ is wide, a continuous and complex wavelet was the best choice for our purposes in this study [19]. A wavelet such as this derives quantitative information about phase interactions between two time series. The present study employs the Morlet wavelet
where ω 0 is the non-dimensional frequency taken to be 6, and \(\eta \equiv (n - n^{{\prime}})\delta t/s\). The Morlet wavelet is continuous and complex, and is frequently used. For the Morlet wavelet, the relation between frequencies and wavelet scales is given by \(1/f = 4\pi s/(\omega _{0} + \sqrt{2 +\omega _{ 0 }^{2}}\) [18, 19]. When \(\omega _{0} \simeq 6\), the wavelet scale is inversely related to frequency, \(f \simeq 1/s\), which simplifies the interpretation of the wavelet analysis, and the wavelet scale can be replaced with the wavelength.
The wavelet transform W n (s) allows the calculation of a power spectrum | W n (s) | 2 and a phase as \(\tan ^{-1}\left [\mathfrak{I}\{W_{n}(s)\}/\mathfrak{R}\{W_{n}(s)\}\right ]\), where \(\mathfrak{I}\{W_{n}(s)\}\) and \(\mathfrak{R}\{W_{n}(s)\}\) are imaginary and real parts of the wavelet transform, respectively. A typical power spectrum is shown in Fig. 15.4a in the Appendix. Similar to the Fourier transform, the magnitude of the spectral power indicates the strength of the periodicity of time series data; however, this periodicity is transient and does not cover the entire time range. This point is illustrated in Fig. 15.4b, which integrates the power spectra from April 1999 to December 2014. The spectra changes with time, and this represents an advantage of wavelet analysis.
While the power spectra provide us with interesting information (the intensity of the epidemics and importance of the virus type), this paper highlights the timing of the epidemics in relation to limitations in space. We calculate phases of the wavelet transform at the wavelet scale s = 52, i.e., during a 52-week (1 year) periodicity of influenza epidemics. The phase of a given time series can be viewed as its position in the pseudo-cycle of the series, and is parameterized in radians ranging from −π to π [19]. Therefore, the phase is useful for characterizing phase relationships between two sets of time series data by computing the phase difference. The present study calculates the phase difference in each prefecture i compared with Tokyo, \(\delta \phi =\phi _{i} -\phi _{0}\), where ϕ i and ϕ 0 are the phases in prefecture i and Tokyo, respectively, and thereby compares and investigates the timing of the epidemics.
2.3 Supplementary Data
Other useful supplementary data are displayed in Fig. 15.2. Japan is peculiar in several respects. We consider the following environmental characteristics in this study Japan has abundant mountainous areas (70 % of the land area), but the population is concentrated in the plains (Fig. 15.2a). A large proportion of the population (more than 30 million) lives in metropolitan areas, and many cities border one another. Even though the northern and alpine regions of Japan are in a subarctic climate, most of the country is in a temperate climate (Fig. 15.2b). Japan also has a highly developed railway network that includes Shinkansen (high-speed railway) lines (Fig. 15.2c). In this study, we attempt to qualitatively deduce the effects of these factors on the spread of influenza epidemics.
(a) Schematic topographical map. (http://www.worldofmaps.net/en/asia/map-japan/topographic-map-japan.htm). (b) Average temperature in February. (http://www.data.jma.go.jp/obd/stats/data/mdrr/atlas/mean_temperature_02.pdf). The color bar indicates temperature in degrees Celsius. (c) Main railway network, including Shinkansen (high-speed railway) lines (red) and regular lines (orange). The line from Hakata to Kagoshima was gradually constructed starting in 2004. (http://airportguide.com/japan_rail_map.php). The URLs were accessed in December 2014
This study uses the standard classification of prefectures into eight regions in Japan (see Fig. 15.3b). Table 15.1 provides a brief summary regarding the population in these regions.
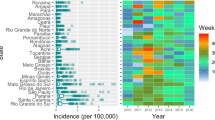
(a) Time-averaged phase differences for 46 prefectures in Japan with standard deviations. The unit of the phase difference is \(52/2\pi \simeq 8.3\) weeks. The broken line is a guide to eyes. (b) Map showing the prefecture ID numbers (http://imas.wikia.com/wiki/Amulet_Purchasing_and_Effects_Guide)
3 Results and Discussion
Figure 15.3a shows the time-averaged phase differences between 46 prefectures in Japan. The following points were notable.
In the Kanto and Kinki regions (urban regions), the phase differences were small, and had a small range of values. This indicates two important features. One is that the epidemics occurred earlier in these regions than in the others, and the other is that the epidemics were well synchronized. The epidemics in Aichi Prefecture (ID 23), which includes Nagoya, the 4th largest city in Japan, also occurred as early as those in the above two regions; however, strong synchrony was not seen between Aichi Prefecture and its adjacent prefectures (Gifu, Shizuoka in the Chubu region, and Mie). A geographical feature of the Chubu region is the Nobi Plain, which is similar to the Kanto Plain in the Kanto region and the Osaka Plain in the Kinki region (Fig. 15.2a); however, there is no city as large as Nagoya in this region (Table 15.1). Hence, the above results suggest that although epidemics begin in large cities, a clustering of large cities is required for strong synchronization.
The phase differences show that, in the regions other than Kanto and Kinki, the epidemics spread sequentially with time, likely in the approximate order of Kyushu, Shikoku, Chugoku, Chubu, Tohoku, and Hokkaido regions. Geographically, this indicates that epidemics spread from west to east, and then northeast (Fig. 15.3b), and also see typical time-series in Fig. 15.1b). This west-to-east spread was previously reported in studies from Europe [6] and the United States [10]. They suggested that the west-to-east spread of influenza is a general phenomenon, that is supported by the results of the present study. The former [6] mentioned numerous factors as causes of this spreading pattern (population, geography, climate, etc.), and the latter [10] pointed to major traffic pathways and local contact networks. Prevailing westerlies appear to play an important role in the case of Japan, which was noted by Sakai et al. [13]. The data used in that study were cases reported from 1992 to 1999, and the Kriging method was used for analysis. The present study therefore appears to confirm a west-to-east spread. Even though Sakai et al. showed epidemic patterns spreading in concentric circles from the west-central to the east, their result is not in conflict with ours if the fluctuations of the phase differences are considered. The European study [6] also observed occasional south-to-north spread, which coincides with the spread from the Kanto to the Tohoku and Hokkaido regions observed in the present study, suggesting the possibility that a south-to-north spreading pattern is also a general phenomenon. However, although influenza epidemics occur during winter, it remains unclear why they spread from high-temperature regions in the south to low-temperature regions in the north (Fig. 15.2b).
An interesting point is that the phase difference in Miyagi Prefecture (ID 4), which includes Sendai, the largest city in the Tohoku region (the 12th largest in Japan), was smaller than that in the other prefectures in this region. This indicates that the epidemic timing in Miyagi Prefecture is similar to that in Tokyo Prefecture, which is likely influenced by intercity travel e.g., via the Shinkansen line (Fig. 15.2c). The geographically discontinuous epidemic spread over a large distance or against geographic constraints can be referred to as “jump spread”. This result may agree with that from the study in the United States, in that the synchrony of epidemics between populous states is strong [8]. This epidemic jump can also be seen in Fukuoka (ID 40) and Kagawa (ID 37) Prefectures. The prefectural capital of Fukuoka is Fukuoka City, the 8th largest city in Japan, which is along the Shinkansen line (Fig. 15.2c). The Kyushu Shinkansen line was constructed gradually starting in 2004; hence, in the future, the value of the phase difference in the prefectures along the Kyushu Shinkansen line may converge in a small range. Although Kagawa Prefecture is separated by the Setonaikai Sea (Fig. 15.2a) and is not serviced by a Shinkansen line (Fig. 15.2c), it is directly connected to the Kinki region by highway, which illustrates the importance of personal travel in epidemic spread.
Another interesting point in the calculation of phase deference is that it may be in contrast to the cases mentioned above. Yamanashi Prefecture (ID 19) neighbors Tokyo Prefecture, and they are directly connected by a conventional railway line and highway. However, the phase difference between these two prefectures is larger than that in the other prefectures bordering Tokyo. Although Yamanashi Prefecture is not serviced by a Shinkansen line, this condition is identical to that in Chiba and Ibaragi Prefectures in the Kanto region. A probable explanation may be geographical in nature: Yamanashi Prefecture is not on the Kanto Plain, but rather in a mountainous area (Fig. 15.2a). This explanation can also be applied to Tottori (ID 31) and Shimane (ID 32) Prefectures. The southern area of these prefectures is mountainous, and forms a “wall” against Okayama (ID 33) and Hiroshima (ID 34) Prefectures (Fig. 15.2a). This wall can account for the larger phase difference in Tottori and Shimane Prefectures in the Chugoku region. These points indicate that simply attributing epidemic spread to personal travel requires caution, and a variety of heterogeneities must be considered collectively.
In the Chubu region, the fluctuation in the phase difference was small in each prefecture compared with the prefectures in the other regions. Fluctuations in phase differences indicate the interseasonal year-to-year variation of epidemic timing. In contrast, fluctuation was larger in the Tohoku and Hokkaido regions. This may be associated with the 2009 pandemic (the so-called “swine flu”), which began in Mexico and spread worldwide [23]. If these phase differences are averaged to include the values before 2009, the fluctuations in the Tohoku and Hokkaido regions are smaller (not shown). These problems regarding fluctuations in phase differences are connected with the type of virus and the emergence of antigenic variants [13]; hence, this paper only provides a brief mention of fluctuations in phase differences.
4 Concluding Remarks
The present study investigated the spread patterns of influenza epidemics in Japan using wavelet analysis. The phase differences were calculated for 46 prefectures. Our main findings were that epidemics occurred earlier and with greater synchronicity in the Kanto and Kinki regions, that epidemics spread west-to-east in the other regions, that epidemic jump occurred between prefectures, and that two adjacent prefectures occasionally had epidemics at different times. These results led us to deduce the following causes: personal travel, climate, and geographical constraints. The deductions presented in this paper are only qualitative, and therefore need to be confirmed by further analyses of newly available data, e.g., the number of Shinkansen passengers passing through each terminal. Although recent studies have been progressing in this direction [19], numerous factors are intercorrelated regarding the problem of epidemic spread, and careful examination is therefore necessary.
References
Lofgren E, Fefferman NH, Naumov YN, Gorski J, Naumova EN (2007) J Virol 81:5429
Lipsitch M, Viboud C (2009) Proc Natl Acad Sci 106:3645
Bonabeau E, Toubiana L, Flahault A (1998) Proc Biol Sci 265:2421
Viboud C, Bjornstad ON, Smith DL, Simonsen L, Miller MA, Grenfell BT (2004) Emerg Infect Dis 10:32
Mugglin AS, Cressie N, Gemmell I (2002) Stat Med 21:2703
Paget J, Marquet R, Meijer A, van der Velden K (2007) BMC Infect Dis 7:141
Alonso WJ, Viboud C, Simonsen L, Hirano EW, Daufenbach LZ et al (2007) Am J Epidemiol 165:1434
Viboud C, Bjornstad ON, Smith DL, Simonsen L, Miller MA, Grenfell BT (2006) Science 312:447
Wenger JB, Naumova EN (2010) PLoS ONE 5:e10187
Stark JH, Sharma R, Ostroff S, Cummings DAT, Ermentrout B, Stebbins S, Burke DS, Wisniewski SR (2012) PLoS ONE 7:e34245
Yu H, Alonso WJ, Feng L, Tan Y, Shu Y, Yang W, Viboud C (2013) PLoS Med 10:e1001552
Sakai T, Suzuki H, Sasaki A, Saito R, Tanabe N, Taniguchi K (2004) Emerg Infect Dis 10:1822
Onozuka D, Hagihara A (2008) Epidemiology 19:824
Infectious Disease Surveillance Center, in Infectious Diseases Weekly Report (IDWR) Japan, http://www.nih.go.jp/niid/en/of subordinate document. Cited 15 Jan 2015
Daubechies I (1992) Ten lectures on wavelets. SIAM monographs SIAM, Philadelphia
Torrence C, Compo GP (1998) Bull Am Meteorol Soc 79:61
Cazelles B, Chavez M, de Magny GC, Guegan J, Hales S (2007) J Roy Soc Interface 4:625
Yang L, Wong CM, Yau EHY, Chan KP, Ou CQ, Peiris JSM (2008) PLoS ONE 3(1):e1399
Centers for Disease Control and Prevention (CDC) (2009) MMWR Morb Mortal Wkly Report 8:467
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Appendix
Appendix
Figure 15.4a depicts a typical power spectrum for Tokyo Prefecture in the 1st week of 2010. The large peak around s = 52 indicates the epidemic mode of annual synchronization. The power spectra from April 1999 to December 2014 are integrated in Fig. 15.4b. Figure 15.4a is a cross section of Fig. 15.4b. Biennial and semiannual modes can also be seen around s = 104 and s = 26, respectively. It is possible that the former is related to type B influenza and the latter to the 2009 pandemic.
(a) Power spectrum for Tokyo prefecture in the 1st week of 2010. The spectral power is normalized by the variance of the time-series. (b) Contour plot of power spectra for Tokyo Prefecture from April 1999 to December 2014. The color bar indicates the spectral power. The broken lines denote the edge effect of the time-series (“cone of influence” [18]). The spectral information is less accurate in the edge regions marked by these lines
Rights and permissions
Open Access This book is distributed under the terms of the Creative Commons Attribution Non-commercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Copyright information
© 2015 The Author(s)
About this paper
Cite this paper
Omata, K., Takahashi, Y. (2015). Spatiotemporal Analysis of Influenza Epidemics in Japan. In: Takayasu, H., Ito, N., Noda, I., Takayasu, M. (eds) Proceedings of the International Conference on Social Modeling and Simulation, plus Econophysics Colloquium 2014. Springer Proceedings in Complexity. Springer, Cham. https://doi.org/10.1007/978-3-319-20591-5_15
Download citation
DOI: https://doi.org/10.1007/978-3-319-20591-5_15
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-20590-8
Online ISBN: 978-3-319-20591-5
eBook Packages: Physics and AstronomyPhysics and Astronomy (R0)