Abstract
External catheter collection systems are condom-type sheaths or receptacles that are externally applied over the penile shaft and connected to some type of drainage bag. They have been developed to meet the specific needs of patients, primarily male patients with urinary incontinence. The most popular are disposable male external catheters. Most are only in place for 24 h. They are reported to be the most comfortable, less painful, and less restrictive when compared to other urologic catheters. As with other urinary catheters, changes in design and material have been evolving. This chapter provides a detailed review of these devices.
References
Gray M, Skinner C, Kaler W. External collection devices as an alternative to the indwelling urinary catheter: evidence-based review and expert clinical panel deliberations. J Wound Ostomy Continence Nurs. 2016;43(3):301–7. doi:10.1097/WON.0000000000000220.
Geng V, Cobussen-Boekhorst H, Lurvink H, Pearce I, Vahr S. Evidence-based guidelines for best practice in urological health care: male external catheters in adults; urinary catheter managementEur Assoc Urol Nurs.2016. Available from http://www.uroweb.org/fileadmin/EAUN/guidelines/EAUN_MEC_Guidelines_EN_2008_LR.pdf
Fader M, Bliss D, Cottenden A, Moore K, Norton C. Continence products: research priorities to improve the lives of people with urinary and/or fecal leakage. Neurourol Urodyn. 2010;29(4):640–4. doi:10.1002/nau.20918.
Robinson J. Continence: sizing and fitting a penile sheath. Br J Community Nurs. 2006;11:420–7.
Pemberton P, Brooks A, Eriksen CM, Frost S, Graham S, Greenman L, et al. A Comparative study of two types of urinary sheath. Nurs Times. 2006;102(7):36–41.
Pomfret I. Penile sheaths: a guide to selection and fitting. J Community Nurs. 2006;20(11):14–8.
Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31(4):319–26. doi:10.1086/651091.
Conway LJ, Larson EL. Guidelines to prevent catheter-associated urinary tract infection: 1980 to 2010. Heart Lung. 2012;41(3):271–83. doi:10.1016/j.hrtlng.2011.08.001.
Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis Off Publ Infect Dis Soc Am. 2010;50(5):625–63.
Newman DK. Devices, products, catheters, and catheter-associated urinary tract infections. In: Newman DK, Wyman JF, Welch VW, editors. Core Curriculum for Urologic Nursing. 1st ed. Pitman, NJ: Society of Urologic Nurses and Associates Inc; 2017. p. 439–66.
Tenke P, Kovacs B, Bjerklund Johansen TE, Matsumoto T, Tambyah PA, Naber KG. European and Asian guidelines on management and prevention of catheter-associated urinary tract infections. Int J Antimicrob Agents. 2008;31(Suppl 1):S68–78. Epub 2007 Nov 14. Review
Cottenden A, Bliss D, Buckley B, Fader M, Gartley C, Hayer D, et al. Management using continence products. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence: 5th international consultation on incontinence. The Netherlands: ICUD-EAU; 2013. p. 1651–786.
Saint S, Kaufman SR, Rogers MA, Baker PD, Ossenkop K, Lipsky BA. Condom versus indwelling urinary catheters: a randomized trial. J Am Geriatr Soc. 2006;54(7):1055–61. doi:10.1111/j.1532-5415.2006.00785.x.
Hebel JR, Warren JW. The use of urethral, condom, and suprapubic catheters in aged nursing home patients. J Am Geriatr Soc. 1990;38(7):777–84.
Rogers MA, Mody L, Kaufman SR, Fries BE, McMahon LF, Saint S. Use of urinary collection devices in skilled nursing facilities in five states. J Am Geriatr Soc. 2008;56(5):854–61. doi:10.1111/j.1532-5415.2008.01675.x.
Saint S, Lipsky BA, Baker PD, McDonald LL, Ossenkop K. Urinary catheters: what type do men and their nurses prefer? J Am Geriatr Soc. 1999;47(12):1453–7.
Edlich RF, Bailey T, Pine SA, Williams R, Rodeheaver GT, Steers WD. Biomechanical performance of silicone and latex external condom catheters. J Long Term Eff Med Implants. 2000;10(4):291–9.
Fader M. Review of current technologies for urinary incontinence: strengths and limitations. Proc Inst Mech Eng H. 2003;217(4):233–41.
Fader M, Pettersson L, Dean G, Brooks R, Cottenden AM, Malone-Lee J. Sheaths for urinary incontinence: a randomized crossover trial. BJU Int. 2001;88(4):367–72.
Newman DK. Internal and external urinary catheters: a primer for clinical practice. Ostomy Wound Manage. 2008;54(12):18–35.
Newman DK, Wein AJ. Managing and treating urinary incontinence. 2nd ed. Baltimore, MD: Health Professions Press; 2009.
Wells M. Managing urinary incontinence with BioDerm external continence device. Br J Nurs. 2008;17(9):s24–9. doi:10.12968/bjon.2008.17.Sup4.29257.
Vaidyanathan S, Soni BM, Singh G, Sett P, Brown E, Markey S. Possible use of BioDerm External Continence Device in selected, adult, male spinal cord injury patients. Spinal Cord. 2005;43(4):260–1.
Lucas LM, Iseler J, Gale L. Evaluation of a new, novel male external urinary management device. Poster presented at: Cleveland Clinic’s Spring 2013 WOC Nursing Symposium; April 12, 2013; Cleveland, OH.
Newman DK, Fader M, Bliss DZ. Managing incontinence using technology, devices and products. Nurs Res. 2004;53(Suppl 6):S42–8.
Doherty W. The InCare Retracted Penis Pouch: an alternative for incontinent men. Br J Nurs. 2002;11(11):781–4. doi:10.12968/bjon.2002.11.11.781.
Johnson DE, O'Reilly JL, Warren JW. Clinical evaluation of an external urine collection device for nonambulatory incontinent women. J Urol. 1989;141(3):535–7.
Newman DK, Fader M, Bliss DZ. Managing incontinence using technology, devices and products. Nurs Res. 2004;53(6 Suppl):S42–8. PubMed PMID: 15586147.
Newman DK. Incontinence products and devices for the elderly. Urol Nurs. 2004;24(4):316–34.
Newman DK. The use of devices and products. Am J Nurs. 2003;3(Suppl):50–1.
Pieper B, Cleland V. An external urine-collection device for women: a clinical trial. J ET Nurs. 1993;20(2):51–5.
Steele N (University of Texas, Austin, TX). A female urinary diversion device for military women in the deployed environment. Bethesda (MD): TriService Nursing Research Program; 2011.Grant NO: HUOOO1-11-1-TS02 (N11-004).
Agarwal A, Subramaniam C. A comprehensive review of problems associated with long duration flying and some suggested remedies. Indian J Aerosp Med. 2008;52(2):21–6.
Steele N, Yoder LH. Military women’s urinary patterns, practices, and complications in deployment settings. Urol Nurs. 2013;33(2):61–71. 78 doi:10.7257/1053-816X.2013.33.2.61.
Hawley-Bowland C. “Lady J” and “Freshette Complete System”: A field trial for the active duty woman. El Paso (TX): William Beaumont Army Medical Center, Army Medical Research and Materiel Command (US); 1995. MIPR NO. 95MM5579.
Mitcha JL, Cornum KG, Cornum RL. Urination in aviation: Evaluation of urine collection equipment for female aviators. Brooks Air Force Base (TX): Armstrong Laboratory, Army Medical Research and Materiel Command (US); 1995. MIPR NO: 95MM5592
Von Thesling GH, Coffman CB, Hundemer GL, Stuart RP. In-flight urine collection device: efficacy, maintenance, and complications in U-2 pilots. Aviat Space Environ Med. 2011;82(2):116–22.
Chartier-Kastler E, Ballanger P, Petit J, Fourmarier M, Bart S, Ragni-Ghazarossian E, et al. Randomized, crossover study evaluating patient preference and the impact on quality of life of urisheaths vs. absorbent products in incontinent men. BJU Int. 2011;108(2):241–7. doi:10.1111/j.1464-410X.2010.09736.x.
Golji H. Complications of external condom drainage. Paraplegia. 1981;19(3):189–97. doi:10.1038/sc.1981.40.
Ouslander JG, Greengold B, Chen S. External catheter use and urinary tract infections among incontinent male nursing home patients. J Am Geriatr Soc. 1987;35(12):1063–70.
Grigoryan L, Abers Ba MS, Kizilbash QF, Petersen NJ, Trautner BW. A comparison of the microbiologic profile of indwelling versus external urinary catheters. Am J Infect Control. 2014;42:682–4. doi:10.1016/j.ajic.2014.02.028.
Bycroft J, Hamid R, Shah PJ. Penile erosion in spinal cord injury--an important lesson. Spinal Cord. 2003 Nov;41(11):643–4. doi:10.1038/sj.sc.3101523.
Milanesi N, Bianchini G, D'Erme AM, Francalanci S. Allergic reaction to condom catheter for bladder incontinence. Contact Dermatitis. 2013;69(3):182–3. doi:10.1111/cod.12083.
Ozkan HS, Irkoren S, Sivrioğlu N. Penile strangulation and necrosis due to condom catheter. Int Wound J. 2015;12(3):248–9. doi:10.1111/iwj.12102.
Kawoosa NU. Isolated gangrene of the penis in a paraplegic patient secondary to a condom catheter. Indian J Surg. 2011;73(4):304–6. doi:10.1007/s12262-011-0256-z.
Vaidyanathan S, Soni BM, Hughes PL, Mansour P, Singh G, Darroch J, et al. Localised necrosis of scrotum (Fournier’s gangrene) in a spinal cord injury patient - a case report. BMC Fam Pract. 2002;3:20.
Jayachandran S, Mooppan UM, Kim H. Complications from external (condom) urinary drainage devices. Urology. 1985;25(1):31–4.
Dwivedi AK, Singh S, Goel A. Massive urethral diverticulum: a complication of condom catheter use. Br J Nurs. 2012;21(9):S20–2. doi:10.12968/bjon.2012.21.Sup9.S20.
Al-Awadhi NM, Al-Brahim N, Ahmad MS, Yordanov E. Giant fibroepithelial polyp of the penis associated with long-term use of condom catheter. Case report and literature review. Can J Urol. 2007;14:3656–9.
Banerji JS, Shah S, Kekre NS. Fibroepithelial polyp of the prepuce: a rare complication of long-term condom catheter usage. Indian J Urol. 2008;24(2):263–4.
Fetsch JF, Davis Jr CJ, Hallman JR, Chung LS, Lupton GP, Sesterhenn IA. Lymphedematous fibroepithelial polyps of the glans penis and prepuce: a clinicopathologic study of 7 cases demonstrating a strong association with chronic condom catheter use. Hum Pathol. 2004;35(2):190–5.
Mason SE, Devilliers P, Andea AA. Lymphedematous fibroepithelial polyp of the penis associated with long-term condom catheter use: case report and review of the literature. J Cutaneous Pathol. 2009;36(8):906–9. doi:10.1111/j.1600-0560.2008.01133.x.
Yan H, Treacy A, Yousef G, Stewart R. Giant fibroepithelial polyp of the glans penis not associated with condom-catheter use: a case report and literature review. Can Urol Assoc J. 2013;7(9–10):E621–4. doi:10.5489/cuaj.506.
Paterson J, Dunn S, Kowanko I, van Loon A, Stein I, Pretty L. Selection of continence products: perspectives of people who have incontinence and their carers. Disabil Rehabil. 2003;25(17):955–63. doi:10.1080/096382809210142211.
Macaulay M, Broadbridge J, Gage H, Williams P, Birch B, Moore KN, et al. A trial of devices for urinary incontinence after treatment for prostate cancer. BJU Int. 2015;116(3):432–42. doi:10.1111/bju.13016.
Meddings J, Saint S, Fowler KE, Gaies E, Hickner A, Krein SL, Bernstein SJ. The Ann Arbor criteria for appropriate urinary catheter use in hospitalized medical patients: results obtained by using the RAND/UCLA appropriateness method. Ann Intern Med. 2015;162(9 Suppl):S1–34. doi:10.7326/M14-1304.
Smart C. Male urinary incontinence and the urinary sheath. Br J Nurs. 2014;23(9) S20, S22-5 doi:10.12968/bjon.2014.23.Sup9.S20.
Author information
Authors and Affiliations
Corresponding author
How to Use a Male External Catheter Patient Education Tool
How to Use a Male External Catheter Patient Education Tool
What Is an External Catheter?
An external catheter is used by a man to collect urine that leaks from the bladder (called “urinary incontinence ”). These catheters are also called “urisheath” or “condom” or “Texas” catheters . This catheter is used on the outside of the body, as it fits over the penis, and connects to a drainage bag.
Types of External Catheters
There are several types of catheters to choose from. They can be used once or reused many times.
-
1.
The most common type has adhesive on the inside of the catheter as shown in this picture. It is rolled on, over the penis, and the adhesive allows it to stick to the skin of the penis. This catheter must be replaced every 1–2 days or sooner if it falls off.

-
2.
Another type of disposable external catheter is called a male urinary pouch. This pouch has adhesive and a pouch that is attached to the drainage bag. The pouch can be used by men whose penis may have “retracted” (pulled in and shortened) or who cannot or will not be fitted by other external products.

-
3.
A third type is shown in pictures below. The catheter is held against your body with cloth underwear, a belt or with straps. This type can be washed and reused.

Putting on a Disposable External Catheter
First, read the manufacturer’s information. To find the correct catheter size, measure the diameter or circumference of your penis with a fitting or sizing guide like the one shown here. It is worth trying different systems to find the one that best fits your needs.
-
Wash your hands. Then gather your equipment: correctly-sized catheter, leg drainage bag with extension tubing, straps, manicure scissors, soap, washcloth, towel, and protective ointment.
-
Trim the hair on the base of your penis or any other hair so it won’t stick to the adhesive tape on the inside of the catheter. Do not shave your hair, clip it.
-
Before each catheter change, wash, rinse, and dry your penis. To protect your skin from urine, you may want to coat your penis with protective skin barrier product and let it dry (it will feel sticky). This skin product will protect your skin from perspiration and urine. Moisture softens your skin and makes it more likely to tear or open when you remove the catheter,
-
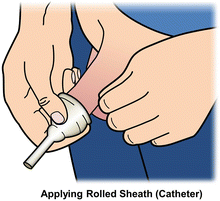
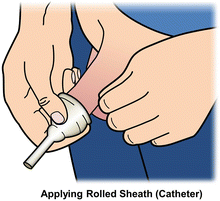
Make sure the sheath is tightly rolled to the edge of the connector tip, balloon-like part seen in this picture. You can squeeze the catheter below the adhesive part to make it easier to apply.
-
Next, hold your penis and place the catheter on the tip of your penis. Gently stretch your penis as you unroll the catheter over the head of your penis and down your penis.
-
Leave about half an inch of space between the tip of your penis and the end of the sheath at the connector tip, so your penis does not rub against the end of the catheter.
-
If you are not circumcised, leave your foreskin in place and roll the catheter over your foreskin. Your foreskin may swell if it is not kept over the head of the penis. The catheter should be snug when rolling it on. If it is loose, the catheter may be too large. If you are unable to unroll the catheter down the penis, the catheter may be too small.
When the catheter is unrolled, gently press it against your penis so that it sticks. Put pressure on your penis for several minutes to be sure any wrinkles are sealed together and to get rid of air bubbles .
-
Connect one end of the tubing to the open connector tip on the catheter and the other end to the extension tube attached to the drainage bag.
-
If the extension tube is too long, cut it to the length you want.
-
Leg bags come with elastic straps so attach the drainage bag to your thigh as shown in this picture or to your lower leg. Do not use too large a leg bag that is too large, because it will put too much weight on the catheter, causing it to fall off.
-
You may need to clean the bag twice a day.

-
The catheter is only used once and is to be discarded once removed. It will be need to be changed daily.
Solving Problems with Your External Catheter
-
If the catheter doesn’t stick, make sure your penis is completely dry before putting on the catheter. Use only ointments and adhesives prescribed by your doctor or nurse.
-
Don’t wash with Betadine because this can irritate your skin.
-
If urine leaks around the catheter, squeeze the catheter to get a better seal or consider a smaller size. A too large catheter will cause urine to leak out between the catheter and your penis.
-
If the catheter is too snug or tight, it may cause the skin of the penis to break open. If it is too tight, you may need a larger size. If it is loose or there are a lot of wrinkles, the catheter may be too large. That is why it is important to find the correct size for you.
-
If the catheter sheath wrinkles, it may be too large and you will need to select a smaller size.
-
Check your penis daily or more frequently for swelling or unusual color. If it feels uncomfortable or doesn’t look normal, take off the catheter and call your doctor or nurse.
-
Call your nurse or doctor if you:
-
Feel pain or burning when you urinate;
-
Have the urge to urinate very frequently;
-
Smell an unpleasant odor from your urine; or
-
See blood or pus in your urine.
© 2013 revs 2016 Diane K. Newman
-
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Newman, D.K., Wein, A.J. (2018). External Catheter Collection Systems. In: Clinical Application of Urologic Catheters, Devices and Products. Springer, Cham. https://doi.org/10.1007/978-3-319-14821-2_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-14821-2_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14820-5
Online ISBN: 978-3-319-14821-2
eBook Packages: MedicineMedicine (R0)