Abstract
Community-based occupational therapy for clients with dementia and their caregivers is a client-centered and family-centered intervention that enables clients with dementia to participate in meaningful activities of daily living (ADL) in their own environment. It enables caregivers to support these clients in these ADL activities and reduces the caregiver’s burden. Occupational therapists (OTs) achieve this outcome, first, by analyzing the life stories and the needs and motivations for meaningful daily activities of these clients and their caregivers in the past and present, second, by setting feasible goals together, third, by enabling clients with dementia to do meaningful activities in ways that will enhance their ability to participate by using strategies to compensate for their cognitive decline, and fourth, by modifying the client’s environment to better support participation. Caregivers are trained in supervision and problem solving, in using cognitive and behavioral strategies to change their coping behavior, and reduce their burden of care.
Look, he is happy doing the gardening by himself with these adaptations. Now, I don’ t feel helpless anymore and I have time to do my own activities.
A caregiver wife
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Alzheimer’s Disease International (2013) Global impact of dementia 2013–2050. www.alz.co.uk/research/G8-policy-brief. Accessed 7 Jan 2014
Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E (2011) Alzheimer’s disease. Lancet 377(9770):1019–1031
Berwick D (2003) Disseminating innovations in health care. J Am Med Assoc 289:1969–1975
Brodaty H, Green A, Koschera A (2003) Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatr Soc 51(5):657–664
Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Speigelhalter D, Tyrer P (2000) Framework for design and evaluation of complex interventions to improve health. BMJ 2000; 321:694–696
Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, Guthrie B, Lester H, Wilson P, Kinmonth AL (2007) Designing and evaluating complex interventions to improve health care. BMJ. 2007 Mar 3;334(7591):455–459.
Canadian Association of OTs (CAOT) Web site (2008) www.caot.ca. Accessed July 2008
Coen J (1998) Dementia and caregiving. J Health Gain 2:5–6
Dröes RM, van der Roest HG, van Mierlo L, Meiland FJ (2011a) Memory problems in dementia: adaptation and coping strategies and psychosocial treatments. Expert Rev Neurother 11(12):1769–1781, quiz 1782. doi:10.1586/ern.11.167 (Review)
Dröes RM, van der Roest HG, van Mierlo L, Meiland FJ (2011b) Memory problems in dementia: adaptation and coping strategies and psychosocial treatments. Expert Rev Neurother 11(12):1769–1781
Döpp CME, Graff MJL, Teerenstra S, Adang E, Nijhuis-van der Sanden RWG, OldeRikkert MGM, Vernooij-Dassen MJFJ (2011) A new combined strategy to implement a community occupational therapy intervention: designing a cluster randomized controlled trial. BMC Geriatr 11:13. doi:1086/1471–2318/11/13 (BMC geriatrics.com online April 24)
Döpp CM, Graff MJ, Teerenstra S, Nijhuis-van der Sanden MW, Olde Rikkert MG, Vernooij-Dassen MJ (2013a) Effectiveness of a multifaceted implementation strategy on physicians’ referral behavior to an evidence-based psychosocial intervention in dementia: a cluster randomized controlled trial. BMC Fam Pract 14(1):70
Döpp CM, Graff MJ, Olde-Rikkert MG, van der Sanden MW, Vernooij-Dassen MJ (2013b). Determinants for the effectiveness of implementing an occupational therapy intervention in routine dementia care. Implement Sci 8(1):131
Dutch Alzheimer Association (2011) Standard for Dementia Care. [Alzheimer Nederland. Zorgstandaard Dementie (in Dutch)]. Utrecht: 2011
Dutch Health Council (Raad voor de Volksgezondheid en Zorg, RVZ) (2002) Gezondheidsraad. Rapport: Dementie [Report: Dementia]. Den Haag: Gezondheidsraad, publication No. 2002/04 [in Dutch]
Dutch Health Council (Raad voor de Volksgezondheid en Zorg, RVZ) (2006) Arbeidsmarkt en zorgvraag. Achtergrondstudies [Labour Market and Care Demand. Background Studies.] Den Haag: RVZ
Folstein MF, Robins LN, Helzer JE (1983) The mini-mental state examination. Arch Gen Psychiatry 40(7):812
Gitlin LN (2005) Occupational therapy and dementia care. The home environmental skill-building program for individuals and families. AOTA, Bethesda
Gitlin LN, Corcoran M, Leinmiller-Eckhardt S (1995) Understanding the family perspective: an ethnographic framework for providing occupational therapy in the home. Am J Occup Ther 49(8):802–808
Gitlin LN, Corcoran M, Winter L, Boyce A, Hauck WW (2001) A randomized, controlled trial of a home environment intervention: effect on efficacy and upset in care givers and on daily functioning of persons with dementia. Gerontologist 41:4–14
Gitlin LN, Hauck WW, Dennis MP, Winter L (2005) Maintenance of effects of the home environmental skill-building programme for family care givers and individuals with Alzheimer’s disease and related disorders. J Gerontol A Biol Med Sci 60:368–374
Graff MJL (1998) Onderzoeksrapport: Het ontwikkelen en testen van de standaard ergotherapie voor de diagnostiek en behandeling van geriatrische patiënten met niet-ernstige cognitieve stoornissen [Research report: the development and testing of a guideline for the occupational therapy diagnosis and treatment of older persons with non-severe cognitive impairments]. UMC St. Radboud, Nijmegen [in Dutch]
Graff MJL, van Melick MBM (2000) The development, testing and implementation of an occupational therapy guideline. The guideline for the OT diagnosis and treatment of older persons with cognitive impairments. Ned Tijdschr Ergother 28:169–174 [in Dutch]
Graff MJL, Vernooij-Dassen MJFJ, Hoefnagels WHL, Dekker J, de Witte LP (2003) Occupational therapy at home for older individuals with mild to moderate cognitive impairments and their primary caregivers: a pilot study. Occup Ther J Res 23:155–164
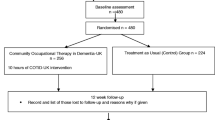
Graff MJL, Vernooij-Dassen MJM, Thijssen M, Dekker J, Hoefnagels WHL, OldeRikkert MGM (2006a) Effects of community occupational therapy in patients with dementia: a randomised controlled trial. Br Med J 333:1196. doi:10.1136/bmj.39001.688843.BE (BMJ online 2006)
Graff MJL, Vernooij-Dassen MJFJ, Zajec J, OldeRikkert MGM, Hoefnagels WHL, Dekker J (2006b) Occupational therapy improves the daily performance and communication of an older patient with dementia and his primary caregiver: a case study. Dementia 5:503–532
Graff MJL, Vernooij-Dassen MJM, Thijssen M, Dekker J, Hoefnagels WHL, OldeRikkert MGM (2007) Effects of community occupational therapy in care givers of patients with dementia: a randomised controlled trial. J Gerontol Med Sci A 62(9):1002–1009
Graff MJL, Adang EMM, Vernooij-Dassen MJM et al (2008) Community occupational therapy for older patients with dementia and their caregivers: a cost-effectiveness study. Br Med J 336:134–138. doi:10.1136/bmj.39408.481898.BE (BMJ online 2008)
Graff MJL, Melick M van, Thijssen M, Verstraten P, Zajec J (2010) Ergotherapie aan huis bij ouderen met dementie en hun mantelzorgers. EDOMAH programma. [Community occupational therapy for older people with dementia and their caregivers. The COTiD program]. Bohn Stafleu & van Loghum, Houten [In Dutch]
Graff MJL, Melick M van, Thijssen M, Verstraten P, Zajec J (2013) L’ergothérapie auprès domicile des personnes âgées atteintes de démence et leurs aidants [Community occupational therapy for older people with dementia and their caregivers. COTiD programme] Edition DeBoek, Bruxelles [In French]
Graff MJL, Melick M van, Thijssen M, Verstraten P, Zajec J (2014) Terapia occupazionale a domicilio per gli anziani con demenza e I loro caregiver. University of Modena, Modena [Manual in Italian language draft version translated in 2013; book in press]
Grol R, Wensing M (2004) Eccles M improving patient care: the implementation of change in clinical practice. Elsevier, Oxford
Hasselkus BR (1990) Etnografic interviewing: a tool for practice with family caregivers for the elderly. Occup Ther Pract 2:9–16
Jepson C, McCorkle R, Adler D, Nuamah I, Lusk E (1999) Effects of home care on caregivers’ psychosocial status. Image J Nurs Sch 31:115–120
Jönsson L, Eriksdotter Jönhagen M, Kilander L et al (2006) Determinants of costs of care for patients with Alzheimer’s disease. Int J Geriatr Psychiatry 21:449–459
Karlsson G, Wimo A, Jönsson B, Winblad B (1998) Methodological issues in health economic studies of dementia. In: Wimo A, Karlsson G, Jonsson B, Winblad B (eds) The health economics of dementia. Wiley, Chichester
Kenens RJ, Hingstman L (2003) Cijfers uit de registratie van ergotherapeuten [registration of occupational therapists] 2002. Nivel, Utrecht
Kielhofner G (2008) Model of human occupation: theory and application, 4th edn. Williams & Wilkins, Baltimore
Kielhofner G, Mallinson T, Crawford C, Nowak M, Rigby M, Henry A, Walens D (2004) A user’s manual for the occupational performance history interview (Version 2.1) (OPHI-II). University of Illinois, Chicago
Kuijper C, de Vries-Kempes W, Wijnties M (2006) Hoofdstuk 5: Betekenisvolle deelname van alledag: Wonen, werken en vrije tijd. [Meaningful participation in daily life: living, work and leisure time.] In: Kinébanian A, Le Granse M (eds) Grondslagen van de ergotherapie, 2e druk [Foundations of occupational therapy]. Elsevier, Maarssen [in Dutch]
Meerding WJ, Bonneux L, Polder JJ, Koopmanschap MA, van der Maas PJ (1998) Demographic and epidemiological determinants of healthcare costs in Netherlands: cost of illness study. Br Med J 317:111–115
Medical Research Council (2010) Developing and evaluating compleinterventions: new guidance. http://www.mrc.ac.uk/complexinterventionsguidance. Accessed 24 Nov 2010
Ministry of Housing, Regional Development and the Environment & Ministry of Public Health, Welfare and Sports (2007) Better (at) home in the community. Action plan: working together on housing, welfare and care 2007–2011. The Hague, Ministry VROM & VWS
NIVEL (2012) Overview of occupational therapy in the Netherlands. Utrecht (Report)
Olazarán J, Reisberg B, Clare L, Cruz I, Peña-Casanova J, Del Ser T, Woods B, Beck C, Auer S, Lai C, Spector A, Fazio S, Bond J, Kivipelto M, Brodaty H, Rojo JM, Collins H, Teri L, Mittelman M, Orrell M, Feldman HH, Muñiz R (2010) Nonpharmacological therapies in Alzheimer’s disease: a systematic review of efficacy. Dement Geriatr Cogn Disord 30(2):161–178
Orrell M, Wenborn J et al (2011) VALID research proposal. London: proposal NHR 2011, funded December 2011
Riopel-Smith R, Kielhofner G (1998) Occupational performance history interview II. University of Illinois, Chicago
Slobbe LCJ, Kommer GJ, Smit JM, Groen J, Meerding WJ, Polder JJ (2006) Kosten van Ziekten in Nederland 2003 [Costs of Illnesses in The Netherlands 2003]. RIVM, Bilthoven [in Dutch]
Smits CH, de Lange J, Dröes RM, Meiland F, Vernooij-Dassen M, Pot AM (2007) Effects of combined intervention programmes for people with dementia living at home and their caregivers: a systematic review. Int J Geriatr Psychiatry 22(12):1181–1193
Spijker A, Vernooij-Dassen M, Vase E, Adang E, Wollersheim H, Grol R, Verhey F (2008) Effectiveness of non-pharmacological interventions in delaying the institutionalization of patients with dementia: a meta-analysis. J Am Geriatr Soc 56(6):1116–1128
Steultjens EMJ, Dekker J, Bouter L, Jellema S, Bakker EB, vandenEnde CHM (2004) Occupational therapy for community dwelling elderly people: a systematic review. Age Ageing 33:453–460
van’t Leven N, Graff MJL, Kaijen M, de Swart BJM, Olde Rikkert MG, Vernooij-Dassen MJ (2012) Barriers to and facilitators for the use of an evidence-based occupational therapy guideline for older people with dementia and their carers. Int J Geriatr Psychiatry 27(7):742–748. doi:10.1002/gps.2782 (Epub 2011 Sep 27)
van Melick MBM, Graff MJL, Mies L (1998) Standaard ergotherapie voor de diagnostiek en behandeling van geriatrische patiënten met niet-ernstige cognitieve stoornissen [A guideline for the OT diagnosis and treatment of older persons with cognitive impairments.] UMC St. Radboud, Nijmegen [in Dutch]
van Melick MBM, Graff MJL (2000) Ergotherapie bij geriatrische patiënten. De standaard voor de ergotherapeutische behandeling van geriatrische patiënten met niet-ernstige cognitieve stoornissen. Ned Tijdschr Ergother 28:176–181
van Mierlo LD, Meiland FJM, Roest HG van der, Droës R (2012) Personalised caregiver support: effectiveness of psychosocial interventions in subgroups of caregivers of people with dementia. Int J Geriatr Psychiatry 27(1):1–14. doi:10.1002/gps.2694 (Epub 2011 April 25)
Voigt-Radloff S, Graff MJL, Reinhart L, Schornstein K, Vernooij-Dassen M, Huel M, Olde-Rikkert M (2011a) A multicenter RCT on community occupational therapy in Alzheimer’s disease: ten sessions are not superior to one consultation. Br Med J 1(1):e000096. doi:10.1136/Bmjopen-2011-000096
Voigt-Radloff S, Graff MJL, Reinhart L, OLde-Rikkert M, Huel M, Vernooij-Dassen M (2011b) Why did an effective Dutch complete psycho-social intervention for people with dementia not work in the German health care context? Lesson learned from a process evaluation alongside a multi-centre RCT. Br Med J 1(1):e000094. doi:10.1136/Bmjopen 2011–000094
Wenborn J, Graff MJL, Orrell M (2014) Community occupational therapy in Dementia UK (COTiD-UK) [Translated and adapted COTiD. Manual draft research version, 2013]. UCL, London (in press)
Wensing M, Grol RP (2007) Implementation: effective improvement of patient care (in Dutch & English version). In: Grol RP, Wensing M (eds) Elsevier, Maarssen
Wimo A, Jönsson B, Karlsson G, Winblad B (1998) Health economics approaches to dementia. In: Wimo A, Karlsson G, Jönsson B, Winblad B (eds) The health economics of dementia. Wiley, Chichester
Wimo A, Winblad B, Aguero Torres H, von Strauss E (2003) The magnitude of dementia occurrence in the world. Alzheimer Dis Assoc Disord 17:63–67 (World Federation of OTs (WFOT, 2008); Website: the definition of the WFOT of 2004)
Wimo A, Jonsson I, Winblad B (2006) An estimate of the worldwide prevalence and direct costs of dementia in 2003. Dement Geriatr Cogn Disord 21:175–181
World Federation of Occupational Therapy (WFOT) (2004) Definition of occupational therapy
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Appendices
Case Study
Mr. and Mrs. Smith learn to deal with the consequences of the dementia in daily life.
Keywords
Stories client and caregiver, setting goals together, effective strategies, problem solving
Introduction
The theme of this case study concerns teaching and supporting clients with dementia and their caregivers in daily functioning.
The students’ tasks include:
-
To make use of the principles of the evidence-based community occupational therapy in older people with dementia and their caregivers (COTiD) program.
As a starting point, students should use the following references to gather background information:
-
1.
Kielhofner G, Mallinson T, Crawford C, Nowak M, Rigby M, Henry A, Walens D (2004) A user’s manual for the occupational performance history interview (Version 2.1) (OPHI-II). Chicago, University of Illinois
-
2.
Nygard L (2004) Responses of persons with dementia to challenge in daily activities: a synthesis of findings from empirical studies. Am J Occup Ther 58(4):435–445
-
3.
Hasselkus BR (1990) Ethnographic interviewing: a tool for practice with family caregivers for the elderly. Occup Ther Prac 2(1):9–16
-
4.
Gitlin LN, Corcoran M, Leinmiller-Eckhardt S (1995) Understanding the family perspective: an ethnographic framework for providing occupational therapy in the home. Am J Occup Ther 49(8):802–808
-
5.
Scobbie L, Wyke S (2009) Identifying and applying psychological theory to setting and achieving rehabilitation goals. Clinical Rehab 23:321–333
-
6.
Graff MJL, Vernooij-Dassen MJFJ, Zajec J, OldeRikkert MGM, Hoefnagels WHL, Dekker J (2006b) Occupational therapy improves the daily performance and communication of an older patient with dementia and his primary caregiver: a case study. Dementia 5:503–532
-
7.
Graff MJL, Vernooij-Dassen MJM, Thijssen M, Dekker J, Hoefnagels WHL, OldeRikkert MGM (2006a) Effects of community occupational therapy in patients with dementia: a randomised controlled trial. Br Med J 333:1196. doi:10.1136/bmj.39001.688843.BE (BMJ online 2006)
Overview of the Content
Recently, the gerontologist psychiatrist referred Mr. Richard Smith to occupational therapy. The intervention aim, was defined in the referral to occupational therapy is:
to improve Mr. Smith’s daily living skills and to advise and train his caregiver in effectively supervising Mr. Smith in these daily activities.
Learning Objectives
By the end of studying this chapter, the learner will be able to understand the components of the COTiD program.
The Background History of the Clinical Case Study
Mr. Smith is 71 years old and lives with his wife in a self-built bungalow. Last week, he was told that he has mild dementia. Besides this, he has decreased mobility due to Parkinson’s disease, and he has hip problems. In the past, these were the reasons that he retired early, at the age of 55 years. After he retired, he built with a colleague, who is a friend of his, the adapted bungalow. Because the house is all on one level, only a few adaptations were needed to accommodate the limitations caused by his hip problems and Parkinson’s disease. He hopes that he and his wife can live independently for as long as possible in their own bungalow. His 70-year-old wife looks after him and provides the necessary care because they both do not want paid home carers coming to them. However, at the moment, his wife complains of back pain because she has too much to care for.
Mr. Smith says that he does not experience problems at the moment. However, he reports that he has problems with starting up activities, he is getting a bit slower than he used to be, and he says that he has problems with more complex activities, like driving a car and cooking a meal. He says that he takes life the way it comes, and he does not complain.
His wife reports that in some ways she feels better since being told about his diagnosis of dementia, as she now realizes that the disease is causing her husband’s problems that she had already noticed. However, she is finding it difficult to accept the diagnosis of dementia and its consequences. However, she is irritated by his loss of initiative and his slowness; and she does not know how to stimulate and supervise her husband in carrying out activities. She is afraid for the future.
Questions
What is the central message to the specific OT intervention? What information do you need more from Mr. and Mrs. Smith, and how will you collect this information?
Case Study Process
-
1.
Case formulation phase
The occupational therapist (OT) decides to first talk to Mr. Smith about his life story and makes use of the occupational performance history interview (OPHI). The OT wants to know who Mr. Smith is and who he was in the past, for example, what interests, habits, roles, norms, and beliefs he had in the past, and what these are now. The OT wants to know what meaning his daily routine and other leisure activities have now to him and had in the past. Also, the OT wants to know if he has goals for now and in the future and what these goals are. The OT tells him this shortly after she has explained to him what occupational therapy can offer. She tells him that she wants to talk to him separately, without his wife. She says that she will also talk with his wife separately, about how she finds caring for him, as well as her own needs and goals for the future. The OT explains also to his wife that she will visit her to talk with her separately. The OT will make use of the ethnographic interview when she talks with Mrs. Smith about her life story, meaningful activities, and how she experiences caring for her husband. The OT explains to both of them that after these separate talks, she accordingly will come back to observe some meaningful activities they are used to perform. The OT explains that once she has this information, together with Mr. and Mrs. Smith, she will be able to start setting goals for the occupational therapy intervention.
Questions
How would you set goals for Mr. and Mrs. Smith? What steps would you perform and what aids could you use?
-
2.
Goal-setting phase
The OT has made a list of interests and meaningful activities that Mr. and Mrs. Smith have each told her that they would like to do in the future. First, she summarizes them in the meeting with Mr. and Mrs. Smith together, using cards on which she already has written some of these meaningful activities. Mr. and Mrs. Smith can add if there are meaningful activities missing.
Mr. Smith’s interests are: gardening , singing in a choir, doing aspects of the housework, wood carving, horse riding, visiting friends, and playing with their grandchildren.
Mrs. Smith’s interests are: flower arranging, visiting friends, chatting to friends by phone, playing with their grandchildren, cycling, fitness classes, and cooking new recipes.
Second, the OT let Mr. and Mrs. Smith separately and accordingly together prioritize the most important meaningful activities they would like to work on in occupational therapy intervention and together with Mr. and Mrs. Smith, the OT formulated global goals.
Questions
What goals do you think Mr. and Mrs. Smith would formulate separately and what are shared goals?
The global goals Mr. Smith formulated are: to have a more meaningful life; and to continue living in their own bungalow for as long as possible.
The global goals Mrs. Smith formulated are: to have more time for herself; to know how to supervise her husband in daily activities and to motivate him to be less passive; to continue living in their own bungalow for as long as possible; to care for her husband without assistance from others.
Third, the OT writes the most important individual and/or joint goals (priorities) on a goal-setting form, as much specified as possible, which they all aim to work on in occupational therapy. Once these are agreed, she asks them to score their goals in terms of their current performance, and to rate their satisfaction with this performance. The caregiver also scores the goals of the client with dementia, from her perspective. She also has her own goals which she scores. The client with dementia only scores his own goals.
Questions
What were the goals and scores you think they prioritized to work on you think? Define the ways of achieving Mr. and Mrs. Smith’s goals and their shared goals and write them down. Accordingly, score these goals from the perspective of Mr. and/or Mrs. Smith.
These are the goals the OT defined together with Mr. and Mrs. Smith to work on in OT intervention:
-
Supervising Mr. Smith in an adequate way that he initiates a meaningful activity he wants to perform, and make effective preparations and adaptations to the activity with which he will be able to perform the activity independently.
-
Arrange more time for Mrs. Smith herself to make flower decorations by getting Mr. Smith started on a meaningful activity by using adaptation and instructions of the activity by Mr. Smith himself.
-
Making use of a whiteboard, agenda, and alarm for Mr. Smith to remember the gardening, meal preparation, and other important daily activities.
-
Doing tasks in the garden by Mr. Smith himself with the use of his effective strategies and with the use of a short instruction ahead given by his wife (or use of signs and written instructions/or verbal instructions or pictures) and adaptations in the physical environment in the garden (signs, alarm, chair half way to remember the break).
-
Preparing the vegetables for the meal by Mr. Smith himself in his own way and speed (describe what this is in his case).
-
Visiting friends together in a way Mr. Smith does not feel overwhelmed by their friends and will get enough time to explain what he wants to tell and will only be supported in his talk when he needs this, and that Mrs. Smith can talk to her friends separately.
Questions
What could be the intervention strategies the OT would propose to train Mr. and Mrs. Smith to reach the goals of?
3. Phase of Implementing the Intervention Plan
The OT’s proposed intervention strategies are:
-
Intervention aimed at improving Mr. Smith’s skills by using compensatory methods (including use of only effective strategies and adaptations in the physical and social environment), combined with improving Mrs. Smith’s supervision skills.
-
Intervention aimed at improving Mrs. Smith’s problem-solving skills and the ability to cope with the burden of care.
The implementation of the intervention plan phase will focus on:
-
Improving Mr. Smith’s skills through adaptation of the environment (like memory aids, instructions, simplifying the environment) and using his most effective strategies in an efficient way
-
Improving Mrs. Smith’s problem-solving and coping skills
Mrs. Smith is very committed but requires more information on her husband’s conditions—Parkinson’s disease and dementia. At the moment, there are many frustrations between the couple which might be improved with more knowledge of the conditions. The OT is planning on increasing Mrs. Smith’s insight in these diseases by:
-
Explaining the symptoms of both the diseases and their effect on daily life
-
Using concrete situations or behaviors during this phase to apply approaches that may be of use (for example during the vacuuming and cooking activities)
Mrs. Smith has always adopted the “grin and bear it” attitude. It is very important for her to have all her daily activities under control. It is important to adapt the intervention to fit in with her daily routine, to coach her in ways she could supervise her husband in managing his limitations, while, at the same time, being aware of the need to maintain her own occupational balance .
Question
How could you improve the problem-solving skills of Mrs. Smith? Which steps should you perform?
In order to improve Mrs. Smith’s problem-solving skills, the OT will use the consult method, which contains of eight steps. In this method:
-
1.
Mrs. Smith and the OT agree that Mrs. Smith is the expert of her own problem situation and that Mrs. Smith, together with the OT, is responsible to find a suitable solution for the problem they are faced with.
-
2.
Together with Mrs. Smith, the OT observes and analyses Mr. Smith’s daily activities (such as cooking)—what strategies he uses and which are effective strategies, how the task is carried out, and what his and Mrs. Smith’s emotions are about carrying out this activity.
-
3.
Following this, the OT meets with Mrs. Smith alone. In this session, the OT coaches Mrs. Smith to describe and analyze what the problem in this activity is.
-
4.
And to discuss what they have tried already, evaluate how it worked out.
-
5.
Accordingly, Mrs. Smith is asked to look for feasible alternatives to perform this activity in an effective way.
-
6.
After this, she is coached by the OT to find a possible solution, the OT therefore uses the sentence “How could you achieve that …” (= the HOCYA formula). Solutions can be effective ways of adapting or preparing the task, simplifying the environment, using effective cues and ways of approaching Mr. Smith.
-
7.
Accordingly, they decide to perform the activity to this possible solution.
-
8.
Afterward, they evaluate how this possible solution worked out. It is possible to use this consultation method more than once until Mrs. Smith is able to follow it through well.
The OT and Mrs. Smith work together very closely and at an equal level to find a solution that works for everyone.
The Student’s Report
The following guiding questions have been identified in developing possible solutions to Mr. and Mrs. Smith. These questions are generated from the references found in the literature search:
-
What are the interests, habits, routines, roles, experiences, and motives of Mr. and Mrs. Smith and what were these in the past? (What came out of the OPHI and ethnographic interview?)
-
What are meaningful activities for Mr. and/or Mrs. Smith? And which activities would they prefer to carry out in a more effective way? (Also, information from OPHI and ethnographic interview)
-
What are the problems they face when performing these activities? What did they tell you and what have you observed?
-
What are the important goals for Mr and/or Mrs. Smith? Describe the five most appropriate goals you formulated together with them.
-
What strategies of Mr. and of Mrs. Smith are effective in performing these meaningful activities and which are not?
-
What are the possible solutions to perform the preferred meaningful activities in an effective way? Describe what problems you analyzed together with Mrs. Smith in each of the prioritised activities, what she already had tried together with her husband, and formulate possible solutions you decided for together with Mrs. Smith. (Make use of the consult method).
Formulate the occupational therapy intervention plan for these five prioritized goals and solutions you formulated and describe how you would implement this intervention plan, which steps you would perform, and how you would supervise these people during the implementation of the intervention plan.
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Graff, M. (2015). Teaching and Supporting Clients with Dementia and Their Caregivers in Daily Functioning. In: Söderback, I. (eds) International Handbook of Occupational Therapy Interventions. Springer, Cham. https://doi.org/10.1007/978-3-319-08141-0_28
Download citation
DOI: https://doi.org/10.1007/978-3-319-08141-0_28
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-08140-3
Online ISBN: 978-3-319-08141-0
eBook Packages: MedicineMedicine (R0)