Abstract
The importance of appropriately recognizing and managing patients with cardiovascular and pulmonary comorbidities is underscored by the poor outcomes described in complex comorbid patients. Patients with chronic obstructive pulmonary disease (COPD) have an increased risk, up to one-third greater than the general population, of cardiovascular comorbidities including hypertension and diabetes [1].
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic obstruction pulmonary disease (COPD)
- Acute exacerbation
- Ischemic heart disease
- Heart failure
- Atrial fibrillation
- BNP
- Troponin
-
Cardiovascular disease and COPD commonly occur in the same patient and share both risk factors and common pathophysiologic mechanisms.
-
Diagnosis of cardiovascular comorbidities in patients with COPD can be challenging and requires a low threshold for investigation in accordance with disease-specific guidelines.
-
Patients with COPD and cardiovascular disease are at risk of being undertreated due to concerns regarding the safety of disease-specific therapies in comorbid patients; however, most therapies are safe.
-
Increased systemic inflammation during an exacerbation of COPD is associated with cardiac dysfunction, morbidity, and mortality.
-
Influenza vaccination reduces cardiovascular risk in COPD patients
-
Long-acting bronchodilators are safe in patients with COPD and comorbid cardiovascular conditions. They may even reduce the risk of cardiovascular events in select patients.
Introduction
The importance of appropriately recognizing and managing patients with cardiovascular and pulmonary comorbidities is underscored by the poor outcomes described in complex comorbid patients. Patients with chronic obstructive pulmonary disease (COPD) have an increased risk, up to one-third greater than the general population, of cardiovascular comorbidities including hypertension and diabetes [1]. Patients with COPD have higher rates of ischemic heart disease, heart failure, and arrhythmias with risks that are 2–5 times higher than those in age-matched control subjects [1, 2]. This presence of cardiovascular disease in patients with COPD leads to lower quality of life, increased rates of hospitalization, and death [3]. Patients with COPD are at a particularly high risk of cardiovascular events during acute exacerbations of COPD (AECOPD) [4]. Indeed, AECOPDs increase the risk of acute coronary events and stroke by 3–5-fold, a risk that can be mitigated by preventing exacerbations related to respiratory tract infections. Thus, understanding the common mechanisms and risk factors for COPD and cardiovascular disease, diagnostic and management challenges, and the interplay between comorbidities during episodes of an acute exacerbation of COPD is central for the clinical care of these complex patients.
COPD Exacerbations
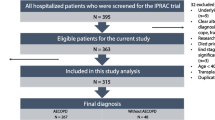
AECOPDs are defined by an increase in patient symptoms beyond the day-to-day variation, which leads to increase in pharmacologic therapy [5]. Currently, AECOPDs are diagnosed largely based on clinical acumen, irrespective of the etiology. As there are no reliable ways of phenotyping exacerbations (e.g., infectious versus noninfectious), all AECOPDs are empirically treated with systemic corticosteroids and/or broad-spectrum antibiotics, which likely leads to their overuse in the community [5]. The treatment and outcomes for AECOPD are far from optimal. Once patients are sick enough to come to emergency departments for AECOPD, 9 out of 10 patients will be admitted for treatment for an average length of hospital stay of 10 days [6]. One in 12 of these patients will die either in hospital or within 6 months of hospital discharge; 1 in 8 patients will require noninvasive or invasive mechanical ventilation, and 1 in 3 patients will suffer another exacerbation over 3–6 months of follow-up [6]. The treatment side effects are also substantial. During therapy, more than 50% patients will experience new or worsening hyperglycemia, 12–18% will develop new or worsening of hypertension, and 12% will experience other steroid-related adverse effects including adrenal insufficiency [6]. Incredibly, treatment for AECOPD has not changed over the past 30 years. Health care providers treat everyone with AECOPD with antibiotics despite good data suggesting that fewer than 50% of the episodes are associated with bacterial infections and with prednisone even though approximately 30% of the episodes are not associated with lung or systemic inflammation!
It is widely postulated, though not completely proven, that respiratory tract infections by microbial agents are the leading cause of AECOPD [5]. By using polymerase chain reaction on spontaneous sputum samples, Bafadhel et al. found that the prevalence of “virus”-associated exacerbation was 29% (with rhinovirus being the most common) and that of “bacteria”-associated exacerbation was more than 40% [7]. However, it should be noted that many patients with COPD demonstrate evidence of bacterial colonization even during clinical stability, whereas presence of viruses is distinctly rare except during exacerbations [7]. Thus, the clinical relevance of identifying bacterial species in spontaneous sputum of patients with COPD during exacerbations is uncertain.
Exacerbations and Cardiovascular Events
The multiple potentially reciprocal mechanisms through which either an exacerbation of COPD may potentiate cardiovascular decompensation or through which cardiac dysfunction can trigger an acute exacerbation of COPD are complex (Fig. 12.1) [8]. Multiple mechanisms are triggered during an AECOPD that lead to cardiovascular dysfunction and morbidity. Platelet activation, fibrinogen production, and interleukin-6, interleukin-8, and tumor necrosis factor α levels are elevated during an acute exacerbation of COPD, and these are pro-atherothrombotic. This cascade can lead to atherosclerotic plaque rupture and acute coronary syndrome as demonstrated in Fig. 12.2. The most important pathway appears to be related to inflammation. COPD patients have chronic lung inflammation which worsens during acute exacerbations [7]. Acute coronary syndromes can be associated with an AECOPD [4]. This increased risk seems most closely associated with respiratory infection and inflammation as an exacerbation trigger [9].
Causes of acute exacerbations of COPD. There are multiple causes of acute exacerbations of COPD (AECOPD). Although almost all clinically significant AECOPDs are treated with oral antibiotics and/or systemic corticosteroids, at least 30% of the AECOPDs are caused by noninflammatory, noninfectious causes. A significant number of cases are caused by cardiovascular events. In one study, approximately 20% of hospitalized AECOPDs were characterized by pulmonary edema on chest radiograph [82]
A proposed schema of how acute exacerbations of COPD may lead to acute cardiovascular events. We propose that respiratory tract infection leads to acute lung injury, resulting in lung inflammation and oxidant stress. This causes endothelial dysfunction and acute disruption of stable atherosclerotic plaques, resulting in the conversion of stable plaques into unstable (or vulnerable) ones. Vulnerable plaques are much more likely to rupture, causing acute myocardial infarction or stroke than stable plaques [83]. Neutrophilic inflammation appears to play a central role in this process [26]
Regardless of the etiology of the AECOPD, during AECOPD events, many patients experience myocardial injury and stress. Patel et al., for instance, found that approximately 16% of patients during AECOPD experienced a marked elevation in serum troponin, a biomarker of myocardial injury, and a similar number experienced a rise in N-terminal pro b-type natriuretic peptide (NT-proBNP ), a biomarker of myocardial stretch and failure. In their study, the levels of these blood cardiac biomarkers peaked at day 7 of the AECOPD event and then gradually returned to normal levels after 30–90 days post-event [10]. Increased troponins and electrocardiographic (ECG) changes have been reported in patients with COPD, in the absence of an acute coronary syndrome, which complicates making the correct diagnosis [11]. As a result, diagnosis of ST-elevation myocardial infarction (STEMI) is frequently delayed in patients with COPD [12]. Increased troponin in patients with acute exacerbation of COPD is an independent risk factor for mortality, even in the absence of acute coronary syndrome, and can be due to multiple factors [13]. The pathophysiology of increased troponin observed during an acute exacerbation of COPD may be related to the development of supply-demand mismatch to the myocardium due to tachycardia or coexisting left ventricular hypertrophy [8]. The hypoxemia and hypercapnia resulting from an acute exacerbation of COPD can also be pro-arrhythmogenic, leading to arrhythmias during an acute exacerbation of COPD which can in turn trigger heart failure decompensation [14]. Troponin may also be increased as a result of increased pulmonary pressures and right heart dysfunction during an exacerbation [8]. Natriuretic peptides are a useful tool in diagnosing acute heart failure in the setting of comorbid COPD as heart failure is unlikely with normal values (BNP < 100 pg/ml or NT-proBNP < 300 pg/ml) [15]. However, the appropriate cutoff value in patients with pulmonary disease is debated as associations between elevated plasma N-terminal proBNP (NT-proBNP) and decreased FEV1 have been described in patients without heart failure. Elevations of BNP or NT-proBNP in patients with an acute exacerbation of COPD predict worse cardiovascular outcomes and death [8]. BNP is released from ventricular myocytes due to either volume or pressure overload and resulting myocyte stretch. Changes in intrathoracic pressure during an acute exacerbation of COPD impact venous return, cardiac function, and pulmonary pressures leading to elevation of BNP [8].
During AECOPD, patients also demonstrate endothelial dysfunction systemically as evidenced by a significant increase in pulse wave velocity of the affected blood vessels. Most importantly, the risk of myocardial infarction (MI) and stroke increases substantially during the first few days of AECOPD. One study showed that the risk of MI increased by 2.27 times the baseline rate within 1–5 days of AECOPD, whereas the risk of stroke increased by 26% [4].
The relationship between acute respiratory tract infection and cardiovascular events is particularly notable and interesting. In the largest study of its kind, Kwong et al. evaluated 364 hospitalizations for MI between May 1, 2009, and May 31, 2014, in Ontario, Canada. They obtained nasal swab data using reverse-transcriptase polymerase chain reaction (rtPCR; monoplex or multiplex assays), viral culture, direct fluorescent antibody staining, and enzyme immunoassays on influenza A and B as well as other respiratory viruses including respiratory syncytial virus, adenovirus, coronavirus, enterovirus (such as rhinovirus), parainfluenza virus, and human metapneumovirus [16]. They found that during the first 7 days of the respiratory tract infection, the risk of MI was 6-fold higher than during “control” periods (i.e., weeks when they were infection-free). The highest risk period was within 1–3 days of the respiratory tract infection (relative risk, RR, of 6.30) with the risk sharply decaying by day 8 of the infection. In this study, most (82%) of the respiratory tract infections were caused by influenza A and only 31% of the cohort had received influenza vaccination prior to the study year.
These data are consistent with other studies including that by Warren-Gash et al. who showed by using the General Practice Research Database (GPRD) in the United Kingdom (UK) that the risk of MI was 4 times higher during the first 3 days of the infection compared with controlled periods with the risk gradually decaying over time and returning to baseline levels by 30–90 days postinfection [17]. Most importantly, in a secondary prevention trial of 439 patients who had been hospitalized with an acute coronary syndrome, Phrommintikul et al. showed that influenza vaccination therapy (versus no vaccination in the control group) resulted in 30% lower rate of combined major cardiovascular end points including death, rehospitalization for acute coronary syndrome or from heart failure, or stroke and a strong trend towards lower rate of cardiovascular mortality (hazard ratio, HR, 0.39; p = 0.088) [18]. It should also be noted that influenza vaccination or pneumococcal vaccination per se is not associated with any increase or decrease in cardiovascular events [9]. Thus, vaccination is safe.
The relationship between infection and cardiovascular events is not restricted to respiratory tract infections. Infection elsewhere in the body is also associated with increased risk of cardiovascular events. Minassian et al. showed using a Medicare beneficiary database that individuals who developed herpes zoster infection (i.e., shingles) experienced a 2.4-fold increase in the risk of ischemic stroke and 1.7-fold increase in the risk of MI within the first week of infection [19]. It should be noted, however, that while infection in other organ systems is associated with increased risk of cardiovascular events, the relationship between respiratory tract infections and cardiovascular events is particularly strong. For instance, Smeeth and colleagues showed using the UK GPRD database that the risk of MI in the first 3 days of a respiratory tract infection was 5.0-fold higher than that during controlled periods, whereas the relative risk for MI for urinary tract infections was only 1.7 [9]. Together these data suggest that respiratory tract infections are one of the most important triggers of MI and stroke and mitigation strategies to reduce these infections will not only decrease the risk of AECOPD but also prevent cardiovascular events.
Common Mechanisms and Risk Factors for Cardiovascular Disease and COPD
The mechanism by which AECOPD leads to cardiovascular events remains largely a mystery. COPD and cardiovascular disease such as heart failure, atrial fibrillation, and ischemic heart disease share common risk factors such as cigarette smoking and age [15]. However, independent of the risk imposed by smoking, reduced lung function, assessed by using decrease in FEV1, has been associated with mortality due to ischemic heart disease [20]. However, whether there exists a common mechanism or link beyond shared risk factors is an ongoing subject of debate.
Systemic inflammation has been observed in patients with COPD, ischemic heart disease, and atrial fibrillation and has been proposed as a potential mechanism leading to poor clinical outcomes [21, 22]. Smoking and alterations in the lung microbiome and elastin fiber have been implicated as potential sources of ongoing inflammation [23, 24]. Other environmental exposures including air pollution, viral and bacterial respiratory infection, and oral disease are thought to increase inflammation and contribute to inflammation associated with poor cardiovascular outcomes [25]. Although the precise pathways are unknown, animal studies suggest that inhalation of small particulate matter leads to chronic lung inflammation and systemic inflammation. This chronic inflammatory state is thought to contribute to the development of atherosclerotic disease, independent of dyslipidemia [25]. A proposed model for how this may occur is presented in Fig. 12.2.
Another important consideration is the effect of lung inflammation related to respiratory tract infection on the cardiovascular system. Jaw et al. modeled the effects of respiratory tract infection on the cardiovascular system using lipopolysaccharide (LPS) stimulation directly to the airways of mice, which were prone to atherosclerosis [26]. LPS is a bioactive component of gram-negative bacterial wall and induces local inflammation by stimulating toll-like receptor 4. In this model, instillation of LPS into the airways resulted in conversion of 68% of the atherosclerotic plaques from “stable” to “vulnerable” ones. In contrast, instillation of just saline into the airways led to 12% of the plaques becoming vulnerable (p = 0.0004). Repeating this experiment following temporary depletion of neutrophils using Ly6G antibodies prevented conversion of stable to vulnerable plaques related to LPS exposure. Interestingly, injection of LPS intraperitoneally to mimic infection outside of the thoracic cavity did not lead to any significant destabilization of atherosclerotic plaques. Together, these data suggest that acute respiratory tract infections induce neutrophilic inflammation locally and systemically that lead to disruption of stable plaques and cause acute myocardial and cerebrovascular events. These adverse effects may be prevented by reducing neutrophilic inflammation.
Does Prevention of AECOPD Reduce the Risk of Cardiovascular Events?
As noted above, influenza vaccination is effective in reducing the risk of significant cardiovascular events in patients with and without COPD. The effects of other drugs commonly used in the treatment of COPD patients on the risk of cardiovascular events are much more uncertain and controversial. The first line of therapy for COPD patients with persistent symptoms is long-acting muscarinic antagonist (LAMA) [5]. In the Understanding Potential Long-Term Impacts on Function with Tiotropium (UPLIFT) trial, the rate of serious cardiac adverse events was 16% lower in the group that was assigned to tiotropium (n = 2986) over 4 years compared with the group that was assigned to placebo (n = 3006; p < 0.05). This relative reduction was largely driven by lower rates of congestive heart failure (RR, 0.59) and myocardial infarction (RR, 0.71) [27]. However, these data should be interpreted cautiously as the primary end point, the rate of decline in lung function, was no different between tiotropium and placebo and the cardiac events were not fully adjudicated; thus, misclassification of events could have occurred. In a population-based study in Ontario, Canada, Gershon et al. demonstrated that elderly patients (66 years of age and older) who were newly prescribed a LAMA or a long-acting beta-2 agonist (LABA), another class of long-acting bronchodilator, had a 31% increase in the risk of cardiovascular events [28]. Another population-based study in the UK showed similar results with use of LAMA being associated with a small increase in the risk of stroke and MI and a significant reduction in total mortality [29]. LAMA in inhalation spray format, which leads to increased drug deposition in the small airways, has been associated with increased risk of cardiovascular events compared with LAMA in a dry powder formulation, which leads to increased drug deposition in the upper and larger airways [30]. However, in the largest clinical trial of its kind involving 17,135 patients with COPD, the use of tiotropium in inhalation spray format was not associated with any significant increase in the risk of major cardiovascular adverse effects compared with tiotropium in a dry powder formulation, though in the higher tiotropium spray dose (5 μg daily), there was a trend towards increased MI (RR, 1.41; p = 0.06) [31]. Collectively, these data suggest that long-acting bronchodilators are safe in patients with COPD and may in select patients reduce the risk of cardiovascular events, possibly by reducing the rate of exacerbations.
Inhaled corticosteroids (ICS) in combination with a LABA are also frequently used to prevent exacerbations in COPD. In one population-based study in Saskatchewan, Canada, the use of ICS was associated with a 32% reduction in the relative risk of MI [32]. However, a systematic review of randomized controlled trials did not demonstrate any significant association between ICS use and the risk of MI or other cardiovascular end points [33]. In the largest clinical trial of its kind (n = 16,485), the use of ICS or ICS/LABA was not associated with cardiovascular mortality or any other serious cardiovascular adverse events compared with placebo [34]. In aggregate, these data suggest that neither ICS alone nor ICS in combination with LABA has any salutary effects on cardiovascular events in patients with COPD.
Challenges in Cardiovascular Disease and COPD
Ischemic Heart Disease
COPD patients have an increased risk of ischemic heart disease (odds ratio [OR] 2.28, 95% confidence interval [CI] 1.76–2.96, p < 0.0001) compared to the general population [1]. Patients with ischemic heart disease similarly have high rates of COPD; however, it is often undiagnosed [35, 36]. Patients with coexisting airflow limitation and ischemic heart disease, as opposed to ischemic heart disease alone, have both a higher burden of COPD symptoms and cardiovascular risk [37]. Recognizing COPD in ischemic heart disease is important as it has been associated with worse short- and long-term outcomes compared to patients with ischemic heart disease alone [38, 39]. Cardiovascular death accounts for a large proportion of deaths in patients with COPD, with estimates of up to 20–30% [3, 40].
Patients with COPD or ischemic heart disease may present with a variety of symptoms including dyspnea, cough, sputum production, exertional chest pain, or decreased exercise tolerance. Symptoms such as shortness of breath and decreased exercise tolerance could be present in either COPD or ischemic heart disease and require appropriate investigation in order to confirm a diagnosis [1]. In the presence of ischemic heart disease, the diagnostic criteria of COPD are not altered and spirometry is required [5]. In patients with COPD, ischemic heart disease symptoms should be investigated in accordance with established guidelines [41].
Although some therapies for ischemic heart disease and COPD have previously been scrutinized for potential harm in patients with both diseases, standard medications are thought to be safe in comorbid patients [15]. Antiplatelet therapy for ischemic heart disease should be prescribed in accordance with established guidelines in patients with COPD [41]. Beta-blockers should not be withdrawn from patients with COPD, are generally safe, and decrease mortality [42]. Although the proposed common mechanism of systemic inflammation present in both ischemic heart disease and COPD raised the question of whether statin therapy may offer a benefit in COPD alone, statin therapy does not impact acute exacerbation risk, but is indicated in ischemic heart disease [39, 43]. Following invasive therapeutic interventions for ischemic heart disease, COPD patients experience more morbidity [44]. COPD patients undergoing percutaneous coronary intervention have increased rates of revascularization and death [44]. Strategies to reduce perioperative as well as longer-term morbidity following invasive therapies for ischemic heart disease in patients with coexisting COPD will require ongoing research.
Inhaled therapies for COPD including LABA, LAMA, and ICS are safe and effective in patients with coexisting ischemic heart disease [15]. In comparing LABA-LAMA or ICS-LABA combination therapies for COPD, rates of MI, unstable angina, and revascularization did not differ between treatment groups [45]. In another study that included patients with COPD and known ischemic heart disease or risk factors for ischemic heart disease, rates of MI and unstable angina were similar between groups treated with LABA-ICS, LABA, ICS, and placebo [34]. This evidence supports the safety of inhaled COPD therapies in patients with ischemic heart disease.
Heart Failure
Similar to ischemic heart disease, heart failure is more common in patients with COPD than the general population (OR 2.57, 95% CI 1.90–3.47, p < 0.0001) [1]. Patients with heart failure and concomitant COPD have higher mortality rates than patients with heart failure alone (HR 1.24–1.7) [46]. Given this increased mortality risk, making the appropriate diagnosis is especially important. Heart failure and COPD share risk factors, frequently occur in the same patient, and share similar presenting symptoms such as dyspnea and functional limitation. This makes distinguishing the presence of these diseases a clinical challenge. The diagnosis of COPD requires spirometry and should be performed with a low threshold in patients with established heart failure [5]. Heart failure with reduced ejection fraction (HFrEF) can result in an up to 20% reduction in both FEV1 and FVC; however, it does not affect the FEV1/FVC ratio, and spirometry therefore retains its diagnostic utility [47]. Establishing a diagnosis of heart failure also requires a low threshold for investigation with echocardiogram in COPD patients [48].
Despite accepted guidelines and mortality benefit of beta-blockers in HFrEF, clinicians underprescribe these medications in patients with COPD [49]. A large retrospective study demonstrated no difference in outcomes between heart failure patients with and without COPD taking cardioselective and nonselective beta blockers [50]. Retrospective analysis of patients from the STATCOPE and MACRO studies demonstrated no decrease in lung function overtime or increase in exacerbation rate attributable to beta-blocker use in patients with COPD [51]. The benefits of beta-blockers in heart failure outweigh potential risks, even in the context of severe COPD, and should be prescribed as indicated [15, 52]. Other heart failure medications including angiotensin-converting enzyme inhibitors, mineralocorticoid receptor antagonists, and ivabradine are recommended, as appropriate, in patients with COPD [53, 54].
Although the use of ICS and roflumilast to treat COPD has not been associated with an increased risk of cardiovascular events, the safety of inhaled bronchodilators in patients with COPD and heart failure has been controversial [55, 56]. Observational studies previously identified an increased risk of hospitalization or death with short-acting beta agonists in patients with HFrEF [57, 58]. However, other studies have not identified an independent risk of mortality with long-acting beta agonists in patients with heart failure [59]. Short-acting muscarinic agents have also been associated with an increased risk of heart failure [60]. Longer-acting agents such as tiotropium, glycopyrronium, aclidinium, and umeclidinium have not been associated with an increased risk of heart failure [61,62,63]. The cardiovascular safety of a combination long-acting bronchodilators, including LABA-LAMA combinations, are similar to the component medications and are generally safe [45, 64]. LABA and tiotropium use in patients with heart failure and COPD has been associated with an increased risk of emergency department visit and hospitalization for heart failure [28]. It may be reasonable, taking the evidence currently available into consideration, to preferentially choose LAMA agents over LABA bronchodilators; however, there is no specific evidence that COPD must be treated differently in the setting of heart failure [65]. It is recommended that patients with heart failure being started on bronchodilators be closely followed up in the two to three weeks following bronchodilator initiation for signs and symptoms of worsening heart failure [15].
Atrial Fibrillation
Atrial fibrillation is the most common arrhythmia in the general population and in patients with COPD [2]. The risk of cardiac dysrhythmia in patients with COPD is almost double that of the general population (OR 1.94, 95% CI 1.55–2.43, p < 0.0001) [15]. Prevalence of atrial fibrillation in COPD varies from 4.7% to 15% and up to 30% in severe COPD [66]. The severity of airflow obstruction is related to an increased prevalence of atrial fibrillation [67]. Outcomes of patients with COPD and coexisting atrial fibrillation are worse with increased risk of hospitalization, lower quality of life, and all-cause mortality [66].
Patients with COPD and atrial fibrillation may present with dyspnea due to either disease; however, co-occurring symptoms such as palpitations or cough may help to increase suspicion for atrial fibrillation or COPD, respectively [15]. The diagnosis of COPD in patients with atrial fibrillation can be made using spirometry, similar to the setting of coexisting ischemic heart disease or heart failure [5]. Atrial fibrillation can be diagnosed with an ECG, but may require 24-hour or longer recording devices to diagnose paroxysmal atrial fibrillation. The detection of atrial fibrillation in patients with COPD is important given the risk for worse outcomes in comorbid patients as well as stroke risk reduction and highlights a potential role for screening. However, screening for asymptomatic atrial fibrillation and mechanisms by which this would most effectively be achieved in patients with COPD has not been defined.
The presence of COPD in atrial fibrillation creates a challenge for atrial fibrillation management. COPD is associated with progression from paroxysmal to permanent atrial fibrillation, unsuccessful cardioversion, and recurrence following interventional catheter ablation [68]. General recommendations regarding atrial fibrillation treatment, including rate and rhythm control strategies and anticoagulation to reduce risk of thromboembolic disease, include patients with COPD [69]. Rate control strategies using non-dihydropyridine calcium channel blockers for patients with atrial fibrillation and COPD is recommended in major guidelines [69]. Cardioselective beta-blockers are also recommended for rate control and have been associated with lower mortality [70]. Use of nonselective beta-blockers for atrial fibrillation should be avoided in patients with severe airflow obstruction and COPD, although evidence for this recommendation is limited [71]. Recommendations for anticoagulation and stroke prevention can be applied to patients with COPD and atrial fibrillation in accordance with guidelines [69].
Concerns exist regarding the pro-arrhythmogenic properties of short-acting beta-agonist bronchodilators [72]. LAMA agents have demonstrated mixed results in increasing rates of atrial fibrillation. Tiotropium does not increase cardiac arrhythmias, but glycopyrronium has been associated with increased rates of atrial fibrillation compared to placebo [63, 73]. Despite evidence of these possible increased risks, LABA, LAMA, and ICS preparations can be safely used to treat COPD in patients with atrial fibrillation [31, 74].
Non-Pharmacologic Therapies
Given the shared risk factors and suspected common pathophysiological mechanisms, a holistic approach to non-pharmacologic management and interventions is important. Smoking cessation is key in the non-pharmacologic management of both COPD and ischemic heart disease [75]. Dietary modification can play a role in improving both cardiovascular and lung health [76]. Rehabilitation programs involving supervised exercise training, education, and support are important and help to improve outcomes in COPD [77]. These programs are also important in patients with ischemic heart disease and heart failure [78, 79]. Despite the benefits of rehabilitation programs in both COPD and cardiovascular disease, the existence of comorbidities is associated with a lower referral rate to rehabilitation programs [80, 81]. There is no evidence that the presence of comorbidities negatively affects patient outcomes and complex comorbid patients should still be referred for cardiopulmonary rehabilitation [81].
Conclusions
Systemic inflammation is common to both COPD and cardiovascular disease. Mechanisms contributing to chronic inflammation and cardiopulmonary disease development as well as the cascade of changes during acute exacerbations of COPD that can lead to decompensation of cardiovascular disease and increased morbidity and mortality are increasingly understood. Elucidating the complex mechanisms through which COPD and cardiovascular disease influence and modify each other will be important in developing therapies and strategies to reduce the burden of morbidity and mortality in these patients.
Cardiologists, respirologists/pulmonologists, internists, and primary care physicians must be attuned to the presence of coexisting cardiac and respiratory disease. Patients with cardiovascular disease and COPD should be investigated for COPD and cardiovascular disease, respectively. A low threshold for investigation is important in order to thoroughly assess presenting symptoms which these comorbidities share in common and reach the correct diagnosis. Therapeutic challenges in treating patients with COPD and cardiovascular disease including ischemic heart disease, heart failure, and atrial fibrillation have been hindered by concerns regarding the safety of disease-specific therapies in patients with complex comorbidities. However, patients with COPD and cardiovascular disease can safely be treated in accordance with major disease-specific guidelines. Given the complexity of diagnosis and management of patients with cardiovascular disease and COPD, models of care that can address the complex multimorbid patient must be developed.
References
Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med. 2015;3:631–9.
Mullerova H, Agusti A, Erqou S, Mapel DW. Cardiovascular comorbidity in COPD: systematic literature review. Chest. 2013;144:1163–78.
Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28:1245–57.
Donaldson GC, Hurst JR, Smith CJ, Hubbard RB, Wedzicha JA. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest. 2010;137:1091–7.
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M, Fabbri LM, Frith P, Halpin DM, Lopez Varela MV, Nishimura M, Roche N, Rodriguez-Roisin R, Sin DD, Singh D, Stockley R, Vestbo J, Wedzicha JA, Agusti A. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195:557–82.
Leuppi JD, Schuetz P, Bingisser R, Bodmer M, Briel M, Drescher T, Duerring U, Henzen C, Leibbrandt Y, Maier S, Miedinger D, Muller B, Scherr A, Schindler C, Stoeckli R, Viatte S, von Garnier C, Tamm M, Rutishauser J. Short-term vs conventional glucocorticoid therapy in acute exacerbations of chronic obstructive pulmonary disease: the REDUCE randomized clinical trial. JAMA. 2013;309:2223–31.
Bafadhel M, McKenna S, Terry S, Mistry V, Reid C, Haldar P, McCormick M, Haldar K, Kebadze T, Duvoix A, Lindblad K, Patel H, Rugman P, Dodson P, Jenkins M, Saunders M, Newbold P, Green RH, Venge P, Lomas DA, Barer MR, Johnston SL, Pavord ID, Brightling CE. Acute exacerbations of chronic obstructive pulmonary disease: identification of biologic clusters and their biomarkers. Am J Respir Crit Care Med. 2011;184:662–71.
MacDonald MI, Shafuddin E, King PT, Chang CL, Bardin PG, Hancox RJ. Cardiac dysfunction during exacerbations of chronic obstructive pulmonary disease. Lancet Respir Med. 2016;4:138–48.
Smeeth L, Thomas SL, Hall AJ, Hubbard R, Farrington P, Vallance P. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351:2611–8.
Patel AR, Kowlessar BS, Donaldson GC, Mackay AJ, Singh R, George SN, Garcha DS, Wedzicha JA, Hurst JR. Cardiovascular risk, myocardial injury, and exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;188:1091–9.
Chang CL, Robinson SC, Mills GD, Sullivan GD, Karalus NC, McLachlan JD, Hancox RJ. Biochemical markers of cardiac dysfunction predict mortality in acute exacerbations of COPD. Thorax. 2011;66:764–8.
Rothnie KJ, Smeeth L, Herrett E, Pearce N, Hemingway H, Wedzicha J, Timmis A, Quint JK. Closing the mortality gap after a myocardial infarction in people with and without chronic obstructive pulmonary disease. Heart. 2015;101:1103–10.
Pavasini R, d’Ascenzo F, Campo G, Biscaglia S, Ferri A, Contoli M, Papi A, Ceconi C, Ferrari R. Cardiac troponin elevation predicts all-cause mortality in patients with acute exacerbation of chronic obstructive pulmonary disease: systematic review and meta-analysis. Int J Cardiol. 2015;191:187–93.
Terzano C, Romani S, Conti V, Paone G, Oriolo F, Vitarelli A. Atrial fibrillation in the acute, hypercapnic exacerbations of COPD. Eur Rev Med Pharmacol Sci. 2014;18:2908–17.
Roversi S, Fabbri LM, Sin DD, Hawkins NM, Agusti A. Chronic obstructive pulmonary disease and cardiac diseases. An urgent need for integrated care. Am J Respir Crit Care Med. 2016;194:1319–36.
Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, Katz K, Ko DT, McGeer AJ, McNally D, Richardson DC, Rosella LC, Simor A, Smieja M, Zahariadis G, Gubbay JB. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378:345–53.
Warren-Gash C, Hayward AC, Hemingway H, Denaxas S, Thomas SL, Timmis AD, Whitaker H, Smeeth L. Influenza infection and risk of acute myocardial infarction in England and Wales: a CALIBER self-controlled case series study. J Infect Dis. 2012;206:1652–9.
Phrommintikul A, Kuanprasert S, Wongcharoen W, Kanjanavanit R, Chaiwarith R, Sukonthasarn A. Influenza vaccination reduces cardiovascular events in patients with acute coronary syndrome. Eur Heart J. 2011;32:1730–5.
Minassian C, Thomas SL, Smeeth L, Douglas I, Brauer R, Langan SM. Acute cardiovascular events after herpes zoster: a self-controlled case series analysis in vaccinated and unvaccinated older residents of the United States. PLoS Med. 2015;12:e1001919.
Hole DJ, Watt GC, Davey-Smith G, Hart CL, Gillis CR, Hawthorne VM. Impaired lung function and mortality risk in men and women: findings from the Renfrew and Paisley prospective population study. BMJ. 1996;313:711–5; discussion 715–6.
Pai JK, Pischon T, Ma J, Manson JE, Hankinson SE, Joshipura K, Curhan GC, Rifai N, Cannuscio CC, Stampfer MJ, Rimm EB. Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med. 2004;351:2599–610.
Gan WQ, Man SF, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax. 2004;59:574–80.
Lee SH, Goswami S, Grudo A, Song LZ, Bandi V, Goodnight-White S, Green L, Hacken-Bitar J, Huh J, Bakaeen F, Coxson HO, Cogswell S, Storness-Bliss C, Corry DB, Kheradmand F. Antielastin autoimmunity in tobacco smoking-induced emphysema. Nat Med. 2007;13:567–9.
Sze MA, Dimitriu PA, Hayashi S, Elliott WM, McDonough JE, Gosselink JV, Cooper J, Sin DD, Mohn WW, Hogg JC. The lung tissue microbiome in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185:1073–80.
Van Eeden S, Leipsic J, Paul Man SF, Sin DD. The relationship between lung inflammation and cardiovascular disease. Am J Respir Crit Care Med. 2012;186:11–6.
Jaw JE, Tsuruta M, Oh Y, Schipilow J, Hirano Y, Ngan DA, Suda K, Li Y, Oh JY, Moritani K, Tam S, Ford N, van Eeden S, Wright JL, Man SF, Sin DD. Lung exposure to lipopolysaccharide causes atherosclerotic plaque destabilisation. Eur Respir J. 2016;48:205–15.
Tashkin DP, Celli B, Senn S, Burkhart D, Kesten S, Menjoge S, Decramer M, UPLIFT Study Investigators. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359:1543–54.
Gershon A, Croxford R, Calzavara A, To T, Stanbrook MB, Upshur R, Stukel TA. Cardiovascular safety of inhaled long-acting bronchodilators in individuals with chronic obstructive pulmonary disease. JAMA Intern Med. 2013;173:1175–85.
Jara M, Wentworth C 3rd, Lanes S. A new user cohort study comparing the safety of long-acting inhaled bronchodilators in COPD. BMJ Open. 2012;2:e000841.
Verhamme KM, Afonso A, Romio S, Stricker BC, Brusselle GG, Sturkenboom MC. Use of tiotropium Respimat Soft Mist Inhaler versus HandiHaler and mortality in patients with COPD. Eur Respir J. 2013;42:606–15.
Wise RA, Anzueto A, Cotton D, Dahl R, Devins T, Disse B, Dusser D, Joseph E, Kattenbeck S, Koenen-Bergmann M, Pledger G, Calverley P, TIOSPIR Investigators. Tiotropium Respimat inhaler and the risk of death in COPD. N Engl J Med. 2013;369:1491–501.
Huiart L, Ernst P, Ranouil X, Suissa S. Low-dose inhaled corticosteroids and the risk of acute myocardial infarction in COPD. Eur Respir J. 2005;25:634–9.
Loke YK, Kwok CS, Singh S. Risk of myocardial infarction and cardiovascular death associated with inhaled corticosteroids in COPD. Eur Respir J. 2010;35:1003–21.
Vestbo J, Anderson JA, Brook RD, Calverley PM, Celli BR, Crim C, Martinez F, Yates J, Newby DE, SUMMIT Investigators. Fluticasone furoate and vilanterol and survival in chronic obstructive pulmonary disease with heightened cardiovascular risk (SUMMIT): a double-blind randomised controlled trial. Lancet. 2016;387:1817–26.
Arnett DK, Goodman RA, Halperin JL, Anderson JL, Parekh AK, Zoghbi WA. AHA/ACC/HHS strategies to enhance application of clinical practice guidelines in patients with cardiovascular disease and comorbid conditions: from the American Heart Association, American College of Cardiology, and U.S. Department of Health and Human Services. J Am Coll Cardiol. 2014;64:1851–6.
Soriano JB, Rigo F, Guerrero D, Yanez A, Forteza JF, Frontera G, Togores B, Agusti A. High prevalence of undiagnosed airflow limitation in patients with cardiovascular disease. Chest. 2010;137:333–40.
Franssen FM, Soriano JB, Roche N, Bloomfield PH, Brusselle G, Fabbri LM, Garcia-Rio F, Kearney MT, Kwon N, Lundback B, Rabe KF, Raillard A, Muellerova H, Cockcroft JR. Lung function abnormalities in smokers with ischemic heart disease. Am J Respir Crit Care Med. 2016;194:568–76.
Behar S, Panosh A, Reicher-Reiss H, Zion M, Schlesinger Z, Goldbourt U. Prevalence and prognosis of chronic obstructive pulmonary disease among 5,839 consecutive patients with acute myocardial infarction. SPRINT Study Group. Am J Med. 1992;93:637–41.
van Gestel YR, Hoeks SE, Sin DD, Simsek C, Welten GM, Schouten O, Stam H, Mertens FW, van Domburg RT, Poldermans D. Effect of statin therapy on mortality in patients with peripheral arterial disease and comparison of those with versus without associated chronic obstructive pulmonary disease. Am J Cardiol. 2008;102:192–6.
McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA, TORCH Clinical Endpoint Committee. Ascertainment of cause-specific mortality in COPD: operations of the TORCH Clinical Endpoint Committee. Thorax. 2007;62:411–5.
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL, King SB 3rd, Kligfield PD, Krumholz HM, Kwong RY, Lim MJ, Linderbaum JA, Mack MJ, Munger MA, Prager RL, Sabik JF, Shaw LJ, Sikkema JD, Smith CR Jr, Smith SC Jr, Spertus JA, Williams SV, Anderson JL, American College of Cardiology Foundation/American Heart Association Task F. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126:e354–471.
Salpeter SR, Ormiston TM, Salpeter EE, Poole PJ, Cates CJ. Cardioselective beta-blockers for chronic obstructive pulmonary disease: a meta-analysis. Respir Med. 2003;97:1094–101.
Criner GJ, Connett JE, Aaron SD, Albert RK, Bailey WC, Casaburi R, Cooper JA Jr, Curtis JL, Dransfield MT, Han MK, Make B, Marchetti N, Martinez FJ, Niewoehner DE, Scanlon PD, Sciurba FC, Scharf SM, Sin DD, Voelker H, Washko GR, Woodruff PG, Lazarus SC, COPD Clinical Research Network, Canadian Institutes of Health Research. Simvastatin for the prevention of exacerbations in moderate-to-severe COPD. N Engl J Med. 2014;370:2201–10.
Enriquez JR, Parikh SV, Selzer F, Jacobs AK, Marroquin O, Mulukutla S, Srinivas V, Holper EM. Increased adverse events after percutaneous coronary intervention in patients with COPD: insights from the National Heart, Lung, and Blood Institute dynamic registry. Chest. 2011;140:604–10.
Wedzicha JA, Banerji D, Chapman KR, Vestbo J, Roche N, Ayers RT, Thach C, Fogel R, Patalano F, Vogelmeier CF, FLAME Investigators. Indacaterol-glycopyrronium versus salmeterol-fluticasone for COPD. N Engl J Med. 2016;374:2222–34.
Rushton CA, Satchithananda DK, Jones PW, Kadam UT. Non-cardiovascular comorbidity, severity and prognosis in non-selected heart failure populations: a systematic review and meta-analysis. Int J Cardiol. 2015;196:98–106.
Guder G, Brenner S, Stork S, Hoes A, Rutten FH. Chronic obstructive pulmonary disease in heart failure: accurate diagnosis and treatment. Eur J Heart Fail. 2014;16:1273–82.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70:776–803.
Fisher KA, Stefan MS, Darling C, Lessard D, Goldberg RJ. Impact of COPD on the mortality and treatment of patients hospitalized with acute decompensated heart failure: the Worcester Heart Failure Study. Chest. 2015;147:637–45.
Mentz RJ, Wojdyla D, Fiuzat M, Chiswell K, Fonarow GC, O’Connor CM. Association of beta-blocker use and selectivity with outcomes in patients with heart failure and chronic obstructive pulmonary disease (from OPTIMIZE-HF). Am J Cardiol. 2013;111:582–7.
Duffy S, Marron R, Voelker H, Albert R, Connett J, Bailey W, Casaburi R, Cooper JA Jr, Curtis JL, Dransfield M, Han MK, Make B, Marchetti N, Martinez F, Lazarus S, Niewoehner D, Scanlon PD, Sciurba F, Scharf S, Reed RM, Washko G, Woodruff P, McEvoy C, Aaron S, Sin D, Criner GJ, NIH COPD Clinical Research Network and the Canadian Institutes of Health Research. Effect of beta-blockers on exacerbation rate and lung function in chronic obstructive pulmonary disease (COPD). Respir Res. 2017;18:124.
Creagh-Brown B. Benefits of beta blockers in chronic obstructive pulmonary disease and heart failure. BMJ. 2014;348:g3316.
Ekstrom MP, Hermansson AB, Strom KE. Effects of cardiovascular drugs on mortality in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187:715–20.
Bohm M, Robertson M, Ford I, Borer JS, Komajda M, Kindermann I, Maack C, Lainscak M, Swedberg K, Tavazzi L. Influence of cardiovascular and noncardiovascular co-morbidities on outcomes and treatment effect of heart rate reduction with ivabradine in stable heart failure (from the SHIFT trial). Am J Cardiol. 2015;116:1890–7.
White WB, Cooke GE, Kowey PR, Calverley PMA, Bredenbroker D, Goehring UM, Zhu H, Lakkis H, Mosberg H, Rowe P, Rabe KF. Cardiovascular safety in patients receiving roflumilast for the treatment of COPD. Chest. 2013;144:758–65.
Macie C, Wooldrage K, Manfreda J, Anthonisen N. Cardiovascular morbidity and the use of inhaled bronchodilators. Int J Chron Obstruct Pulmon Dis. 2008;3:163–9.
Au DH, Udris EM, Fan VS, Curtis JR, McDonell MB, Fihn SD. Risk of mortality and heart failure exacerbations associated with inhaled beta-adrenoceptor agonists among patients with known left ventricular systolic dysfunction. Chest. 2003;123:1964–9.
Au DH, Bryson CL, Fan VS, Udris EM, Curtis JR, McDonell MB, Fihn SD. Beta-blockers as single-agent therapy for hypertension and the risk of mortality among patients with chronic obstructive pulmonary disease. Am J Med. 2004;117:925–31.
Bermingham M, O’Callaghan E, Dawkins I, Miwa S, Samsudin S, McDonald K, Ledwidge M. Are beta2-agonists responsible for increased mortality in heart failure? Eur J Heart Fail. 2011;13:885–91.
Ogale SS, Lee TA, Au DH, Boudreau DM, Sullivan SD. Cardiovascular events associated with ipratropium bromide in COPD. Chest. 2010;137:13–9.
Tashkin DP, Leimer I, Metzdorf N, Decramer M. Cardiac safety of tiotropium in patients with cardiac events: a retrospective analysis of the UPLIFT(R) trial. Respir Res. 2015;16:65.
Verhamme KM, Afonso AS, van Noord C, Haag MD, Koudstaal PJ, Brusselle GG, Sturkenboom MC. Tiotropium Handihaler and the risk of cardio- or cerebrovascular events and mortality in patients with COPD. Pulm Pharmacol Ther. 2012;25:19–26.
D’Urzo AD, Kerwin EM, Chapman KR, Decramer M, DiGiovanni R, D’Andrea P, Hu H, Goyal P, Altman P. Safety of inhaled glycopyrronium in patients with COPD: a comprehensive analysis of clinical studies and post-marketing data. Int J Chron Obstruct Pulmon Dis. 2015;10:1599–612.
Calzetta L, Rogliani P, Matera MG, Cazzola M. A systematic review with meta-analysis of dual bronchodilation with LAMA/LABA for the treatment of stable COPD. Chest. 2016;149:1181–96.
Jara M, Lanes SF, Wentworth C 3rd, May C, Kesten S. Comparative safety of long-acting inhaled bronchodilators: a cohort study using the UK THIN primary care database. Drug Saf. 2007;30:1151–60.
Divo M, Cote C, de Torres JP, Casanova C, Marin JM, Pinto-Plata V, Zulueta J, Cabrera C, Zagaceta J, Hunninghake G, Celli B, BODE Collaborative Group. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186:155–61.
Buch P, Friberg J, Scharling H, Lange P, Prescott E. Reduced lung function and risk of atrial fibrillation in the Copenhagen City Heart Study. Eur Respir J. 2003;21:1012–6.
de Vos CB, Pisters R, Nieuwlaat R, Prins MH, Tieleman RG, Coelen RJ, van den Heijkant AC, Allessie MA, Crijns HJ. Progression from paroxysmal to persistent atrial fibrillation clinical correlates and prognosis. J Am Coll Cardiol. 2010;55:725–31.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW, American College of Cardiology/American Heart Association Task Force on Practice G. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:e1–76.
Bhatt SP, Wells JM, Kinney GL, Washko GR Jr, Budoff M, Kim YI, Bailey WC, Nath H, Hokanson JE, Silverman EK, Crapo J. Dransfield MT and investigators CO. beta-Blockers are associated with a reduction in COPD exacerbations. Thorax. 2016;71:8–14.
Mainguy V, Girard D, Maltais F, Saey D, Milot J, Senechal M, Poirier P, Provencher S. Effect of bisoprolol on respiratory function and exercise capacity in chronic obstructive pulmonary disease. Am J Cardiol. 2012;110:258–63.
Wilchesky M, Ernst P, Brophy JM, Platt RW, Suissa S. Bronchodilator use and the risk of arrhythmia in COPD: part 2: reassessment in the larger Quebec cohort. Chest. 2012;142:305–11.
Hohlfeld JM, Furtwaengler A, Konen-Bergmann M, Wallenstein G, Walter B, Bateman ED. Cardiac safety of tiotropium in patients with COPD: a combined analysis of Holter-ECG data from four randomised clinical trials. Int J Clin Pract. 2015;69:72–80.
Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, Crim C, Willits LR, Yates JC, Vestbo J, TORCH Investigators. Cardiovascular events in patients with COPD: TORCH study results. Thorax. 2010;65:719–25.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corra U, Cosyns B, Deaton C, Graham I, Hall MS, Hobbs FD, Lochen ML, Lollgen H, Marques-Vidal P, Perk J, Prescott E, Redon J, Richter DJ, Sattar N, Smulders Y, Tiberi M, van der Worp HB, van Dis I, Verschuren WM, Binno S, ESC Scientific Document Group. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315–81.
Jacobs DR Jr, Kalhan R. Healthy diets and lung health. Connecting the dots. Ann Am Thorac Soc. 2016;13:588–90.
Casaburi R, ZuWallack R. Pulmonary rehabilitation for management of chronic obstructive pulmonary disease. N Engl J Med. 2009;360:1329–35.
Kwan G, Balady GJ. Cardiac rehabilitation 2012: advancing the field through emerging science. Circulation. 2012;125:e369–73.
Ades PA, Keteyian SJ, Balady GJ, Houston-Miller N, Kitzman DW, Mancini DM, Rich MW. Cardiac rehabilitation exercise and self-care for chronic heart failure. JACC Heart Fail. 2013;1:540–7.
Evans RA, Singh SJ, Collier R, Loke I, Steiner MC, Morgan MD. Generic, symptom based, exercise rehabilitation; integrating patients with COPD and heart failure. Respir Med. 2010;104:1473–81.
Salzwedel A, Nosper M, Rohrig B, Linck-Eleftheriadis S, Strandt G, Voller H. Outcome quality of in-patient cardiac rehabilitation in elderly patients–identification of relevant parameters. Eur J Prev Cardiol. 2014;21:172–80.
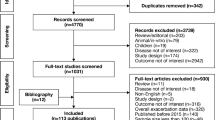
Alotaibi NM, Chen V, Hollander Z, Hague CJ, Murphy DT, Leipsic JA, DeMarco ML, FitzGerald JM, McManus BM, Ng RT, Sin DD. Phenotyping COPD exacerbations using imaging and blood-based biomarkers. Int J Chron Obstruct Pulmon Dis. 2018;13:217–29.
Kullo IJ, Edwards WD, Schwartz RS. Vulnerable plaque: pathobiology and clinical implications. Ann Intern Med. 1998;129:1050–60.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Milne, K., Sin, D.D. (2020). Acute Exacerbations of Chronic Lung Disease: Cardiac Considerations. In: Bhatt, S. (eds) Cardiac Considerations in Chronic Lung Disease. Respiratory Medicine. Humana, Cham. https://doi.org/10.1007/978-3-030-43435-9_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-43435-9_12
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-43434-2
Online ISBN: 978-3-030-43435-9
eBook Packages: MedicineMedicine (R0)