Abstract
Chronic Obstructive Pulmonary Disease (COPD) is a severe lung illness that causes a progressive deterioration in the function and structure of the respiratory system. Recently, COPD became the fifth cause of mortality and the seventh cause of morbidity in Canada. The advancement of context-aware technology creates a new and important opportunity to transform the standard shape of healthcare services into a more dynamic and interactive form. This research project design and validates a rule-based ontology-reasoning framework that provides a context-aware system for COPD patients. The originality of the proposed approach consists in its methodology to prove the efficiency of this model in simulated examples of real-life scenarios based on collaborative data analysis, recognized by specialized medical experts.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
COPD has a significant impact on individuals and society. Moreover, COPD represents an economic burden on the health care system. Statistics Canada [1], ranked COPD as the fifth cause of death in the country. Studies show that people with COPD are vulnerable to many natural events, environmental factors, and sudden worsening of the common signs and symptoms. Recent years have witnessed a widespread increase in the number of telemedicine projects in this domain. This kind of intervention will help COPD patients to avoid severe problems and lengthy hospital admissions [2]. Most research focuses on post exacerbation reactions, but what if we took a step back, and look for ways to avoid exacerbation as much as possible. This task requires working on three different levels, first, find the safe range of environmental factors, second, adjust the normal limits of relevant biomarkers, and third, figure the external influences (e.g. excessive physical effort, climatic factors) on the patient’s body. The originality of this approach resides in the intelligent monitoring and control of persistent changes in the physiological parameters and the ambient environment. This work was part of a concentrated effort to create safe adaptive ranges for the personalized biomarkers where the normal values of these vital signs are often affected by the medical profile, the type of current exercise, the place, and the weather. Environmental factors are also one of the COPD irritants, where cumulative exposure to the multitude of climate hazards such improper humidity levels or extreme weather temperatures, both indoor and outdoor air pollution, in addition to the abnormal concentrations of oxygen in the atmosphere may threaten patient lung health. Developing dynamic alarm thresholds is an important contribution because that would promote the services provided and increase the value of telemonitoring in self-management. Moreover, a customized threshold will help to decrease the proportion of false alarms and differentiate between true exacerbation and normal variation. To achieve these goals, there is an important need to develop a comprehensive representation of knowledge to capture the real context of the patient to avoid misdiagnosis and allow dynamic reconfiguration of health disorders threshold. Rule-based ontology to support context-aware systems offers potential solutions to the multi-scale nature of COPD. In a previous work [3] we designed an ontological reasoning framework that provides a rules-driven context-aware system for COPD patients. In this article, we will present the validation process of that proposition, proving its results by specialized medical experts, and demonstrating its efficiency in simulated examples of real-life scenarios through empirical data about environment, activities, symptoms and physiological parameters.
2 Related Works
Almost two decades ago, the use of medical ontologies was no longer limited to define medical terminologies such as Systematized Nomenclature of Medicine - Clinical Terms (SNOMED CT) or Unified Medical Language System (UMLS), but also it has become one of the powerful solutions to tackle serious health problems and support the management of complex and large data. The ontologies have been also used in hundreds of research projects concerned with medical issues such as diagnosis, self-management, and treatment [4]. The ontological approach proved its effectiveness in the remote healthcare arena, for instance, Lasierra et al. [5] and Larburu et al. [6] have presented robust examples of ontology usage in the telemonitoring domain for generic and specific chronic diseases. Lasierra proposed an autonomic computing ontology for integrated management at home using medical sensors. Rubio provides a formal representation of knowledge to describe the effect of technological context variations in the clinical data quality and its impact on a patient’s treatment. Another example can be found in [7], Benyahia developed a generic ontology for monitoring patients diagnosed with chronic diseases. The proposed architecture aims to detect any anomalies or dangerous situations by collecting physiological and lifestyle data. Hristoskova et al. [8] presented an ontology-based ambient intelligence framework that supports real-time physiological monitoring of patients suffering from congestive heart failure. Ryu [9] proposed a ubiquitous healthcare context model using an ontology; the model extracts the contextual information for implementing the healthcare service taking into consideration the medical references and environments. Kim [10] has designed an interactive healthcare system with wearable sensors that provides personalized services with formal ontology-driven specifications. In the same setting, an ontology-based context-aware framework for customized care has been presented by Ko et al. [11] as a form of wearable biomedical technology. An interesting projection of ontology in this domain can be found in [12] that builds a context-aware mobile service aiming at supporting mobile caregivers and sharing information to improve quality of life of people living with chronic diseases. In addition to this obvious interest in ontology, most of health care projects related to computer-assisted medical decision-making, are often modelled using rule-based approaches. The Semantic Web Rule Language (SWRL) has emerged over existing OWL axioms to promote expressiveness of Semantic Web. In the medical environment, there are several uses of rules, for example, but not limited, the IF-THEN rules can be used for chaining or mapping ontology properties to achieve Knowledge Integration. By applying rules, the pattern of behaviors of all entities can be expressed, which would produce new facts and tailored services. The use of the ontology in COPD is only restricted to certain aspects of patients’ lives. For example, authors in [13] developed an ontology inspired by the autonomic computing paradigm that provides configurable services to support home-based care. Authors in [6] proposed a predictive model to extract relevant attributes and enable the early detection of deteriorations but the proposed ontology aims at describing the basic structure of the application. Although a significant amount of research has been done studying the importance of telehealth in COPD, the concept of integrated care services is still in its infancy. The use of semantic mapping between the physiological parameters, environmental factors, symptoms, physical activity and patient-specific data to construct a telemonitoring system for COPD using ontologies was not found in the literature. This work will be the first building block for creating a comprehensive primary e-health care delivery system, capable of organizing various daily life scenarios for COPD patients in a healthy and safe environment.
3 Proposed System
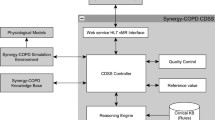
In our previous work, we proposed an ontology-based approach to keep track of the physical status of patients, suggest recommendations and deliver interventions in a timely manner. The proposed system provides an intelligent monitoring infrastructure guided by rules. This process involves observing and controlling the behavior of physiological parameters and the surrounding environment. Consequently, the system adapts the safe ranges for the vital signs in proportion to demographic factors, medical profile, physical activity, and external ambiance. The main contribution of that work consists in proposing a specific domain architecture for COPD. This architecture is designed and implemented in four distinct layers: the acquisition layer is dedicated for collecting and properly transmitting different sorts of data, such as the medical profile of COPD patient, biomarkers and environmental information whether gathered from wearable or fixed monitoring sensors. The semantic layer or the ontological schema has been used to interpret complex information and translate the real context of the patient into machine-understandable and accessible language. At the macro level, the telemonitoring system aims to detect all the possible hazardous events that could influence COPD patient. Since OWL has expressivity limitations on representing many types of contextual information, especially IF-THEN statement, our ontologies have been extended with forward-chaining rules. These rules were expressed in the Semantic Web Rule Language (SWRL) to describe all implications and consequences. The proposed rules are extracted from data analysis, existing medical guidelines and opinions of pneumologists. Practically, these rules are used by an inference engine to derive new facts, detect events, and predict the potential risk. The novelty of these rules lies in its dynamic structure, which has the capacity to configure and re-configure the secure boundaries according to the current circumstances and contexts.
Figure 1 above provides an explanation of the relationships between the constituent entities of the system in a simplified manner. In the next section, we will learn about the methods of extracting the medical rules of COPD.
4 COPD Rules
In preparation for rules extraction, we performed data analysis, reviewed medical guidelines, interviewed experts and examined published sources to map biomarkers of COPD patients to various real-life patterns. A rule, on the other hand, is a description of how a patient is affected by internal bodily characteristics and external environmental factors.
4.1 Biomarkers Rules
In clinical therapy, each patient must be recognized as individuals with a unique health state. However, grouping patients with a similar medical profile is an excellent solution to treat diseases. Unlike previous works and based on this scientific principle, we studied all relevant factors according to the personal and medical profile, which includes the demographic information and the clinical chart of patients. Hurst et al. [14] and Rajeh et al. [15] identified the main physiological parameters and symptoms to be monitored. Understanding the maximum possible extent of change for each variable in different scenarios is a crucial need for the early detection of pulmonary exacerbations. In the next section, we will try to find out how these parameters change with COPD patient in different medical profiles and during common daily life activities. Profile differences help to explain discrepancies in medical care received by COPD patients. Having considered the guidelines, it is recommended dividing the population of patients into groups or quartiles according to age, gender, stage, BMI, smokers, medication, and comorbidity. Identifying factors that may indicate if something is wrong with COPD patients is about to happen was a daunting task and took a long time. This study has established 11 physical parameters must be monitored namely, body temperature, blood pressure, heart rate, partial pressure oxygen (PaO2), oxygen saturation (SpO2), partial pressure carbon dioxide (PaCO2), oxygen consumption (VO2), respiration rate, PH, HCO3, and FEV1. Understanding the role of these biomarkers and their normal ranges in the stable COPD patients with all potential scenarios grants us the ability to sense imminent danger. Patients were separated horizontally by gender, age and stage, these groups have been then reclassified vertically according to the effects of BMI, smoking, medication, and comorbidities on the vital signs. To illustrate this point, we will provide an example to explain changes in heart rate with different profiles.
4.1.1 Heart Rate Rules
Analysis of data obtained from medical records [16, 17, and 18] finds that heart rate in women can be slightly different from men. Figure 2 shows that females have a higher heart rate compared with males at all ages, as this difference increases in the early middle age and decreases in late adulthood. In contrast, the overall analysis shown a remarkable decline in the normal resting heart rate (Fig. 3).
Resting heart rate was also associated with both obese and all inhaler medication across all stages of COPD (p < 0.004 and p < 0.003). The change in heart rate was only associated with four comorbidities, CHF, anemia, PH, and asthma. One of the key factors that change heart rate is activity. Heart rate differs from person to person during exercise or when doing any physical effort, this variation is determined by mathematical equations with an acceptable degree of accuracy. In summary, this evidence-based analysis proves that heart rate varies depending on the medical profile of the patient, which in turn will affect the stable ranges of this vital sign during physical activities. The same analytical methodology has been used on the other physiological parameters mentioned above.
4.2 Indoor and Outdoor Rules
According to Healthy Environments and Consumer Safety Branch (HECSB), Canadians spend approximately 90% of their life indoors [19] often, due to the extreme nature of the climate conditions. Therefore, it’s very important to pay attention to the quality of that indoor air, temperature, humidity, and pressure, especially as COPD patients must fully live in a safe environment, away from any kind of exacerbation irritants. Unlike the internal environment, we cannot control the external environmental factors. There are six main factors that affect the patient outside of the ordinary indoor ambient, these factors must include outdoor temperature, humidity, wind speed, precipitation, atmospheric pressure, and air quality but in terms of air compounds and outdoor pollutants. The proposed rules must provide customized protection against all the inappropriate environmental factors.
5 Dataset
Gatherings such different kinds of data from real sensors are subject to some practical limitations such as ethical approval, financial costs, and deployment time. Hence, researchers suggest an alternative experimental method using intelligent simulation. There are three basic data sources to build such scenarios, (1) medical information, (2) daily life activities, and (3) the environmental conditions.
5.1 Real-Life Activities
There are relatively many published studies about the simulation of activities. Based on previous findings, we attempted to extend the existing indoor scenarios proposed by Mshali [20]. Using the same approach which is built upon Markovian models. Many other scenarios have been built upon the Markovian models, we created new sequences of expected activities including outdoor actions that can be performed by COPD patients. These scenarios took into consideration the levels of severity and disabilities as provided for in the international classification of functioning (ICF). These daily life activities of COPD patients have been divided into six successively sequences associated with six-time periods from sunrise to sunset. Each one of these sequences consists of a set of coordinated activities with a random duration created through transition probabilities matrices.
5.2 Environmental Conditions
Unlike the patient activity dataset, challenges in assembling environmental data were easier, where we found many open sources that describe environmental conditions of indoor and outdoor spaces at long intervals. One of the most interesting outdoor datasets for environmental information is published by the ministry of environment and climate change strategy in British Columbia in Canada [21]. These data sets contain continuous readings of meteorological and pollutants index from air quality monitoring stations across the province from 1980 till the end of 2017. Simulation of the internal environment is also important where the patient spends most of his time at home. The indoor data is tracked via GAMS indoor air quality monitor [22].
5.3 Medical Records
Medical profiles are a vital asset in ensuring the validation process. In this context, we have collected thousands of electronic medical records, hospital admission data, and measures of the outcome in clinical studies from different medical sources ([16] Al-Sahel hospital and MIR clinic [17]).
6 Implementation
The experimental dataset consists of the activities that have been generated using the MATLAB, the environmental conditions which are captured by real sensors and the biomarkers that obtained from medical sources. The simulated scenarios revolve around creating sequential records over 12 months period for COPD patients with different levels of disease severity and autonomy. In this section, we briefly describe the implementation steps of this project using protégé (Fig. 4).
The initial implementation of the project will be done in the following manner: (1) the simulated data stored in Excel spreadsheet files will be uploaded directly to Ontology-based knowledge using Cellfie plugin. (2) The SPARQL query engine accesses to the Knowledge Base to retrieve information of patient’s profile, current location, and activity, etc. (3) SWRL rule reasoner adds additional information such as normal ranges, and appropriate environment to the Knowledge Base. Moreover, SWRL rule reasoner performs reasoning on the updated Knowledge Base of COPD domain and new inferred facts are added to the Knowledge Base. (4) The SPARQL query engine accesses to the Knowledge Base to retrieve the notifications and the recommendations according to the patient’s context. We constructed eight ontologies for monitoring COPD patient to represent machine-understandable Knowledge Base. The developed ontologies consist of concepts related to personal and medical profile, physical examinations, laboratory tests, location, activity, environment, time, recommendations, and disease [3] (Fig. 5).
Thousands of SWRL rules were used to manage the safe conditions of almost 600 COPD medical profiles in various circumstances. Based on the medical information found in the guidelines and other information provided by physicians, we created 20,328 rules using forward chaining of inference. These rules use concepts/axioms defined in our ontology. These rules are set to achieve different goals such as (i) verify the profile of patients (ii) detect the location and environment (iii) evaluate the patient’s status and surrounding conditions, (iv) provide the corresponding service for patients. For more details, please refer to the reasoning section of our previous work [3]. Having reasoning techniques of ontologies and rules that contain the asserted and inferred statements, we used SPARQL to retrieve, and derive contextual information from the knowledge base. The aim of this query is to retrieve any information relating to an identified instance, such as a sign, symptom, treatment, alarm, recommendation, decision, etc. To illustrate the use of the model, we will present some examples. Let’s consider the scenario of a COPD patient being remotely monitored after diagnosis. The patient vital signs, activity, and environmental parameters are continuously monitored (Fig. 6).
The presented simulations have handled a great amount of data of possible situations. The generated alarms have been classified into four main categories: vital signs, activity, pollution, and weather. The system applies continuous monitoring and detects a total of 2,817 abnormal situations.
7 Evaluation
This section will explore partially the performance of our system using a confusion matrix. Performance measurement refers to information that quantifies accuracy, sensitivity, specificity, and the probability of predicting a dangerous change in physiological parameters in COPD patients. The purpose of this evaluation is to measure the diagnostic performance of technical and clinical accuracy.
A master file was created in MS Excel® that contains 1200 patients records, biometric readings for each patient have been extracted from the results inferred from ontology in different scenarios. This information was presented to physicians. This data is used to calculate the confusion matrices for the physician’s report outcomes. There are four possible outcomes, true positive (TP), true negative (TN), false positive (FP), and false-negative (FN). The confusion matrix contains information about the predicted classifications identified by our ontology and the opinions of medical experts. Categories in this research are defined as follows (Table 1):
-
1.
TP is an alarm with a hospitalization.
-
2.
FN has no alarm with a hospitalization.
-
3.
TN has no alarm and no hospitalization.
-
4.
FP has an alarm with no hospitalization.
The results refer that our system reaches an accuracy of 88% in a set of 1200 clinical cases. Sensitivity and specificity have high values, denoting the ability of the system to detect warning signs. The positive predictive value (PPV) is defined as the probability of intervention for positive test results while the negative predictive value (NPV) describes the probability of being healthy for negative test results (Table 2).
8 Conclusion
The proposed model involves a qualitative leap in the healthcare systems that supports COPD because it establishes new obligations that will limit many of the potential hazards at different levels, both physiological and environmental. The system can recognize any important changes in biometrics and environment based on a personalized threshold. The protection process aims to adjust the thresholds around the normal state to avoid exacerbation triggers. Our findings proved that dynamic thresholds can enhance the existing telemonitoring systems and make a valuable contribution identify the health status of COPD patients. Many conclusions can be drawn from this experimental simulation. Firstly, the ontology-based system can provide a more efficient way to deal with medical data. Secondly, adding an SWRL layer of experts’ rules on top of OWL can handle various types of context and suggest reliable recommendations. Thirdly, the results support the importance of context where it demonstrates that context variables have a strong influence on the accuracy of decisions. For future research, this study will have to be evaluated through real implementation and crossover trial to assess patients’ experiences and measure their effectiveness and usability.
References
Public Health Agency of Canada Report from the Canadian Chronic Disease Surveillance System: Asthma and Chronic Obstructive Pulmonary Disease (COPD) in Canada, Ottawa (2018). ISBN 978-0-660-09274-4
Segrelles, G., Gómez-Suárez, C., Soriano, J.B., Zamora, E., Gónzalez-Gamarra, A., et al.: A home telehealth program for patients with severe COPD: the PROMETE study. Respir. Med. 108, 453–462 (2014)
Ajami, H., Mcheick, H.: Ontology-based model to support ubiquitous healthcare systems for COPD patients. Electronics 7, 371 (2018)
Button, K., van Deursen, R.W., Soldatova, L., Spasić, I.: TRAK ontology: defining standard care for the rehabilitation of knee conditions. J. Biomed. Inform. 46(4), 615–625 (2013). https://doi.org/10.1016/j.jbi.2013.04.009. [PMID: 23665300]
Lasierra, N., Alesanco, A., Guillen, S., Garcia, J.: A tree stage ontology-driven solution to provide personalized care to chronic patients at home. J. Biomed. Inform. 46, 516–529 (2013)
Larburu, R., Bults, R.G., Van Sinderen, M.J., Hermens, H.J.: An ontology for telemedicine systems resiliency to technological context variations in pervasive healthcare. IEEE J. Transl. Eng. Health Med. 3, 10 (2015). https://doi.org/10.1109/JTEHM.2015
Benyahia, A.A., Hajjam, A., Hilaire, V., Hajjam, M.: E-care ontological architecture for telemonitoring and alerts detection. In: 5th IEEE International Symposium on Monitoring & Surveillance Research (ISMSR): Healthcare-Safety-Security (2012)
Hristoskova, A., Sakkalis, V., Zacharioudakis, G., Tsiknakis, M., De Turck, F.: Ontology-driven monitoring of patient’s vital signs enabling personalized medical detection and alert. In: Nikita, K.S., Lin, J.C., Fotiadis, D.I., Arredondo Waldmeyer, M.-T. (eds.) MobiHealth 2011. LNICST, vol. 83, pp. 217–224. Springer, Heidelberg (2012). https://doi.org/10.1007/978-3-642-29734-2_30
Ryu, J.-K., et al.: Ontology based context information model for u-healthcare service. In: 2011 International Conference on Information Science and Applications, pp. 1–6 (2011)
Kim, J., Lee, D., Chung, K.: Ontology driven interactive healthcare with wearable sensors. Multimed. Tools Appl. 71, 827–841 (2012)
Ko, E.J., Lee, H.J., Lee, J.W.: Ontology-based context modeling and reasoning for U-HealthCare. IEICE Trans Inf. Syst. E90-D(8), 1262–1270 (2007)
Paganelli, F., Giuli, D.: An ontology-based system for contextaware and configurable services to support home-based continuous care. IEEE Trans. Inf. Technol. Biomed. 15, 324–333 (2011)
Valls, A., Gibert, K., Snchez, D., Batet, M.: Using ontologies for structuring organizational knowledge in home care assistance. Int. J. Med. Inform. 79(5), 370–387 (2010)
Hurst, J.R., et al.: Susceptibility to exacerbation in chronic obstructive pulmonary disease. New Engl. J. Med. 363, 1128–1138 (2010)
Al Rajeh, A., Hurst, J.: Monitoring of physiological parameters to predict exacerbations of chronic obstructive pulmonary disease (COPD): a systematic review. J Clin. Med. 5, 108 (2016)
AL Sahel Hospital. Beirut, Lebanon (2018)
Medical International Research (MIR), clinical laboratory. Beirut, Lebanon (2018)
Simulated patient cases, training and validation dataset. https://doi.org/10.1371/journal.pone.0188532.s004
Ventilation and the Indoor Environment. Water and Air Quality Bureau Healthy Environments and Consumer Safety Branch, March 2018. http://publications.gc.ca/collections/collection_2018/sc-hc/H144-54-1-2018-eng.pdf
Mshali, H., Lemlouma, T., Magoni, D.: Context-aware adaptive framework for e-health monitoring. In: IEEE International Conference on Data Science and Data Intensive Systems, Sydney, Australia, pp. 276–283, December 2015
Outdoor air quality dataset. https://catalogue.data.gov.bc.ca/dataset/air-quality-monitoring-verified-hourly-data
GAMS Indoor Air Quality Dataset. https://github.com/twairball/gams-dataset
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2019 The Author(s)
About this paper
Cite this paper
Ajami, H., Mcheick, H., Mustapha, K. (2019). Ubiquitous Healthcare Systems and Medical Rules in COPD Domain. In: Pagán, J., Mokhtari, M., Aloulou, H., Abdulrazak, B., Cabrera, M. (eds) How AI Impacts Urban Living and Public Health. ICOST 2019. Lecture Notes in Computer Science(), vol 11862. Springer, Cham. https://doi.org/10.1007/978-3-030-32785-9_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-32785-9_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-32784-2
Online ISBN: 978-3-030-32785-9
eBook Packages: Computer ScienceComputer Science (R0)