Summary
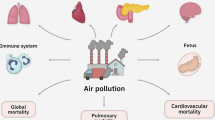
Epidemiological data has shown that air pollution accounts for at least six million deaths per year worldwide. Cardiovascular disease ranks first among the causes of death from pollution, yet it is largely neglected. There is compelling evidence from studies in different world regions showing a causal relationship between air pollution and cardiovascular disease, but this information has not reached the scientific community at large and much less the general public. Gaseous and particle pollutants access the circulation through the lungs and accelerate atherosclerosis by altering blood pressure, lipids, oxidative processes, and insulin resistance. They affect all individuals from the maternal uterus to old age. Almost the entire population in Asian countries is exposed to severely elevated levels of pollutants and most other countries have vascular-damaging levels. More than 80% of the affected individuals belong to emerging regions. The use of N95 masks reduces the exposure to PM2.5, the most damaging particle. Physicians should consider air pollution as a recognized risk factor for vascular disease and act accordingly with patients exposed to different levels of pollutants. The only way to limit the worsening levels of pollution worldwide is to increase the joint efforts among science, governments and other leadership to generate a climate change conscious society and increase efforts to reach a decarbonized world by mid-century.
“It was the best of times, it was the worst of times, it was the age of wisdom, it was the age of foolishness, it was the epoch of belief, it was the epoch of incredulity…”
Charles Dickens, A Tale of Two Cities
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Background
Climate change and air pollution pose a direct threat to human life on earth. The amount of data supporting this notion is compelling and encompasses a broad spectrum of disciplines, including energy, hydrology, physics, chemistry, anthropology, medicine, biology, economics, and philosophy, among others. Yet this is likely the most neglected menace to humanity. In the popular quote that opened the chapter, Dickens eloquently expresses the opposing forces of love and odium, seemingly in a rather equal balance. Can we humans working as a group tilt these apparently matched forces?
This is the era of communications and of the ubiquity of knowledge. So, why are most of the data and messages about climate change and diseases caused by air pollution missing their targets? Probably because we mostly preach to those who already know and want to listen. Most of the world is simply not aware of this self-caused health catastrophe. Air pollution is an epidemic and the medical community is looking the other way. Breathing during our daily personal, working, and leisure time accelerates the occurrence of heart and brain infarction, cognitive decline and serious lung diseases, ranging from infections to cancer. The result is the occurrence of millions of preventable deaths. Despite this appalling statistic, air pollution is a significant risk factor for death that every human faces with indifference. Is this the result of some form of misinformation? We are now celebrating 30 years since evidence-based medicine radically changed “eminence”-based anecdotes and opinions into information based on well-designed research. Those of us with a specific knowledge in topics that most people fail to fully grasp and comprehend ought to disseminate this information in a scientific, reliable, complete, and clear message. In this chapter, I describe the data that show how air pollution damages the vascular system and thus becomes a leading risk factor for cardiovascular disease and death.
The Impact of Cardiovascular Disease Worldwide
Cardiovascular disease leads to 50,000 deaths every day, representing a third of all deaths worldwide. Such deaths include coronary heart disease (myocardial infarction), cerebrovascular disease (stroke), aortic aneurysm, peripheral vascular disease of the legs, vascular kidney failure, and others. Coronary heart disease is the first cause of death worldwide (Mozaffarian, Benjamin, Go, et al., 2015). In 2013, stroke was the second cause of death globally, with 25.7 million people who survived a stroke and 6.5 million people who died from stroke (Feigin, Norrving, & Mensah, 2017). Vascular disease is also a leading cause of cognitive decline and dementia, affecting up to a third of patients with cerebrovascular disease (Mijajlović, Pavlović, Brainin, et al., 2017).
More than 85% of strokes occur in developing regions, where prevalence of the disease is lower compared to developed countries because case fatality rates are higher due to suboptimal health systems. Cardiovascular disease incidence has increased 100% in the developing world over the last decade (Feigin, 2005). A study in 44 nations revealed that vascular risk factors are similarly distributed and largely undertreated (Bhatt, Steg, Ohman, et al., 2006).
Stroke occurs one to two decades earlier in individuals in emerging countries compared to developed countries with up to 50% of events affecting people under 70 years of age (20% in developed regions) (Strong, Mathers, Leeder, & Beaglehole, 2005).
The aforementioned data suggest that cardiovascular disease could be a straightforward problem to tackle (Yusuf, Hawken, Ounpuu, et al., 2004). Supporting this, various studies have shown that by following vascular disease management guidelines, adhering to treatment, avoiding cigarette smoking, having an appropriate nutritional intake and exercising, up to 80% of vascular events could be avoided (Chiuve, McCullough, Sacks, & Rimm, 2006; Hackam & Spence, 2007).
However, between 2005 and 2016, incidence of ischemic heart disease and stroke increased by 53% and 25%, respectively (Global Burden of Disease 2015 Risk Factors Collaborators, 2016). Unfortunately, most patients do not receive adequate treatment (as an example, 80% of treated hypertensive patients are not controlled!).
Air Pollution: A Poorly Recognized Vascular Disease Risk Factor
Although the deleterious effects of air pollution on human health were reported almost three decades ago, this major health risk factor has only recently come to the attention of the general medical community (Dockery, Pope, Xu, et al., 1993). In a recent analysis, Feigin et al. studied all modifiable vascular risk factors included in the Global Burden of Disease Study in 188 countries carried out from 1990 to 2013 (Feigin, Roth, Naghavi, et al., 2016). They analyzed the population attributable fraction (PAF) of all risk factors to define their individual contribution to stroke. More than three-quarters of the stroke burden could be avoided by controlling behavioral and metabolic risk factors. Smoking, poor nutrition and sedentary habits had a PAF of 74%. Hypertension, diabetes, cholesterol, and a high body mass index accounted for 72% of the burden. However, the authors found an unexpected 29% of the stroke burden attributed to air pollution, which was most significant in emerging regions (and highest in sub-Saharan Africa and South Asia) (Feigin et al., 2016).
Interestingly, when considering the health consequences of air pollution, cognitive decline and dementia are rarely mentioned. However, population-based data suggest that seven modifiable vascular risk factors accelerate cerebrovascular disease, which account for 50% of dementia cases. Because disease of the cerebral microcirculation has been associated with the risk of Alzheimer disease, those same modifiable risk factors have been shown to account for one-third of Alzheimer dementia (Ashby-Mitchell, Burns, Shaw, & Anstey, 2017; Norton, Matthews, Barnes, Yaffe, & Brayne, 2014). Cognitive disease should be included when measuring the total disease burden associated with air pollution.
The World Health Organization (WHO), the American Heart Association (AHA) and the European Cardiology Society have all formally declared air pollution as a risk factor for vascular disease (Brook, Rajagopalan, Pope, et al., 2010; Newby, Mannucci, Tell, et al., 2015).
Particulate Matter
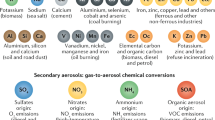
Air pollution consists of a gaseous phase composed of carbon monoxide, ozone, sulfur dioxide, and nitrogen dioxide, and a particulate phase that encompasses 10, 2.5, and 0.1 μm particle matter (PM). Fuel combustion accounts for 85% of PM and 100% of the gaseous toxins.
Different estimates reveal that ten million people die worldwide from all causes of pollution, including air, water, soil, and occupational. Of them, between five and six million died from air pollution in 2015; for approximately 60%, the cause of death was cardiovascular disease (the remainder died from lung cancer, chronic obstructive pulmonary disease, and respiratory infections). By 2050, the number of deaths will have increased by 50% (Lelieveld, Evans, Fnais, et al., 2015). Air pollution currently represents the fifth leading cause of death, accounting for 7.6% of all deaths; 92% of the affected population is located in low- and middle-income countries (Cohen, Brauer, Burnett, et al., 2017). It is also the fifth most common vascular disease risk factor following hypertension, smoking, diabetes, and obesity (Global Burden of Disease 2015 Risk Factors Collaborators, 2016). Available data show an association between acute and chronic exposure to air pollution and different forms of cardiovascular disease, such as congestive heart failure, myocardial infarction, stroke, arrhythmias and sudden death (Brook et al., 2010; Ensor, Raun, & Persse, 2013; Link, Luttmann-Gibson, Schwartz, et al., 2013; Newby et al., 2015).
PM Toxic Levels: How Low is Harmless?
The WHO air quality guidelines suggest that a PM2.5 concentration of 10 μg/m3 is “safe” to avoid a causal role with vascular and lung disease. However, if these particles are pathogenic, then only a zero level can be considered safe, just as any number of cigarettes above zero is associated with disease caused by smoking. However, beyond the fact that reaching a zero PM level is probably practically impossible, the most recent estimation for the lowest mean PM2.5 concentrations that could be considered a minimum risk exposure level is 4.2 ± 1.8 μg/m3 (Lelieveld et al., 2019). This threshold value is significantly lower than that accepted by WHO and the 8.8 μg/m3 advised by the Global Burden of Disease study, which explains the significantly larger proportion of PM2.5-related deaths with current calculations (Lelieveld et al., 2015; Lim, Vos, Flaxman, et al., 2012).
Worldwide Air Pollution
During the period from 1990 to 2015, the overall population-weighted exposure to PM increased from 39.7 to 44.2 μg/m3. Air pollution’s toxic effects are most significant in Southeast Asia, where 99% of the population is exposed to levels that are beyond WHO air quality guidelines (van Donkelaar, Martin, Brauer, & Boys, 2015). New Delhi and Beijing show averages of 100 μg/m3 with peaks of 1000 μg/m3. India (with a population-weighted exposure of 74 μg/m3) and China (58 μg/m3) alone account for at least 50% of all PM-related cardiovascular deaths.
In the USA, improvements have been achieved with an average exposure of 8.4 μg/m3 reached in 2015 from an average 14 μg/m3 in 2000, reflecting a 40% decrease in PM2.5 concentration (Cohen et al., 2017). If this improvement were to be replicated worldwide, deaths from air pollution would decrease by approximately 46% (Morishita, Thompson, & Brook, 2015). A 10 μg/m3 reduction results in a half-year increase in life expectancy. A recent study in the USA that evaluated 61 million individuals showed that increases of 10 μg/m3 were associated with a 7.3% increase in mortality. Racial minorities and people with low incomes were most affected (Di, Wang, Zanobetti, et al., 2017). When Cohen et al. in the Global Burden of Disease study evaluated worldwide trends of average PM2.5 concentrations from 1990 to 2015, all countries had values above the WHO air quality guidelines of 10 μg/m3. Many (mostly in Asia) reached five to almost ten times the average reported in the USA, with evolution curves that have become steeper since 2010 in the most populated countries (Bangladesh, China and India); only Nigeria showed a trend above the standard but with a decreasing projection (Cohen et al., 2017). Multiple efforts with varying results have been made to fight and control air pollution in the USA. In some areas, these efforts are counterbalanced; for example, in California, according to the strength and direction of winds, 10–20% of air pollution may come from China across the Pacific (Lin, Pan, Davis, et al., 2014).
Is PM2.5 Inhalation Currently Preventable?
The use of N95 breathing masks is the only method that has proven effective to decrease particle inhalation by more than 95% (Münzel et al., 2017). One study showed a significant reduction in mean blood pressure and electrocardiogram changes in individuals wearing N95 masks (Langrish, Wang, Lee, et al., 2012). A study to measure the stress hormonal response to air pollution was performed in Shanghai in 55 healthy college students (Li, Cai, Chen, et al., 2017). A double-blind, crossover analysis was performed using indoor air filter purifiers and sham purifiers for 9 days with a 12-day wash-out period. The filters resulted in a 50% decrease in PM, from 53 to 24 μg/m3. The students underwent measurements of glucocorticoids, catecholamines, free fatty acids, blood pressure, and insulin resistance to convey data on systemic inflammation and blood circulation status. The comparison between students revealed that those not breathing purified air had changes in most biomarkers indicative of increased oxidative stress, inflammation, thrombosis and increased blood pressure. A relevant concern of this study is whether the 50% reduction noted is enough, because the resulting PM levels are still significantly above a safe threshold.
How Does Air Pollution Reach the Vascular System?
Fossil fuel emissions contribute to most of the PM associated with cardiovascular disease. The gaseous contributors ozone and nitrogen oxide double the pathogenic effects of PM. These toxins cause endothelium dysfunction due to increased reactive oxygen species and decreased nitric oxide, increased blood pressure and insulin resistance, abnormal lipid concentrations and arrhythmias that lead to increased thrombosis (Brauer, Freedman, et al., 2016; Ostro, Hu, Goldberg, et al., 2015; Shah, Lee, McAllister, et al., 2015). Arrhythmias may also lead to cardiac embolism to the brain, and an increased sympathetic tone correlates with an abnormal cerebrovascular resistance that impairs cerebral blood flow. PM2.5 is one-third the size of red blood cells and enters the body’s circulation via the lung alveoli; by directly translocating across the lung–vessel barrier or by entering macrophage cells, they penetrate this barrier into the circulating blood to cause the aforementioned endothelial changes (Nemmar, Vanbilloen, Hoylaerts, et al., 2001).
What Is the Evidence Linking Air Pollution and Cardiovascular Disease?
The effect of PM2.5 on atherosclerosis has been shown in animal models. In one study, 28 mice were fed with normal or high-fat chow and exposed to PM2.5 or filtered air for 6 h/day, 5 days a week for 6 months. A significant increase in the amount of atherosclerosis, vasoconstrictor response and vessel inflammation was measured in the mice aorta exposed to PM2.5 (Sung, Wang, Jin, et al., 2005). The Multi Ethnic-Study of Atherosclerosis and Air Pollution (MESA) was conducted over 10 years in nine locations from six USA states. A greater degree of coronary calcification in multi-slice CT was determined in subjects exposed to PM2.5 and nitrogen dioxide. Hypertensive and older subjects were the most vulnerable (Kaufman, Adar, Allen, et al., 2012; Kaufman, Adar, Barr, et al., 2016). Significant changes in forearm blood flow have been shown with smoking, which are exacerbated when another variable such as high cholesterol is also present (Heitzer, Yla-Herttuala, Luoma, et al., 1996). In another study, 31 subjects were exposed to PM2.5, ozone, their combination, or filtered air. Diastolic blood pressure was lowest in the filtered air group and most significantly elevated in the PM plus ozone group (Brook, Urch, Dvonch, et al., 2009). In a double-blinded, crossover study, Kristen et al. exposed 45 nonsmoking subjects (age 18–49) to diesel exhaust PM for 2 h or to filtered air (exposure times were separated by 2 weeks). Blood pressure was measured every 30 min during exposure and four times during the first 24 h. Systolic blood pressure was significantly and rapidly increased in the diesel group compared to controls despite the short exposure time (Kristen, Cosselman, Krishnan, Oron, et al., 2012). Short-term exposure to air pollution outside the laboratory has also been shown to cause acute vascular events. A French study of the gaseous phase of air pollution showed that people aged 55–64 years without prior clinically evident vascular disease, exposed for 1–2 days to increased concentrations of ozone, had a significantly higher risk of developing an acute coronary event (Ruidavets, Cournot, Ferrières, et al., 2005). Other studies provide extensive evidence of the association between air pollution and hospital admissions and emergency room consults for vascular events, myocardial infarction, stroke, arrhythmias, and congestive heart failure (Brook, Franklin, Cascio, et al., 2004; Claeys, Rajagopalan, Nawrot, & Brook, 2017; Forastiere & Agabiti, 2013; Gold & Samet, 2013; Link & Dockery, 2010; Mustafić, Jabre, Caussin, et al., 2012; Stafoggia, Cesaroni, Peters, et al., 2014).
Epidemiological data also show that when deaths are compared for each month of the year before and after smoke-free legislation was passed in the USA, a significant reduction in the number of deaths was noted (Pell, Haw, Cobbe, Newby, et al., 2008). Shah et al. performed a meta-analysis to assess exposure to air pollutants and acute stroke (Shah et al., 2015). The authors reviewed approximately 100 articles reporting 6.2 million vascular events in 28 countries. A robust association was found between admissions/death from stroke with both PM and gaseous air pollutants (except for ozone); the strongest association occurred on the day of exposure to PM2.5. The most significant findings were seen in low- and middle-income countries. Previous studies had shown an association between long-term PM exposure and stroke (Dockery et al., 1993; Miller, Siscovick, Sheppard, et al., 2007; Pope, Burnett, Krewski, et al., 2009). A recent review analyzed the association between air pollution and stroke focusing on the specific subtypes of stroke (hemorrhagic, small and large vessel, cardioembolic), patient’s age, effect of temperature in the cold and warm season, types of pollutants, duration of exposure, and the presence of vascular risk factors or previous vascular events (Estol, 2019).
The Global Burden of Stroke study by Feigin et al. revealed a significant loss of stroke disability-adjusted life-years (DALYs) from air pollution among metabolic and behavioral risk factors (Feigin et al., 2016). The importance of the authors’ findings was showing that 90% of stroke burden is due to modifiable risk factors. Air pollution was the third largest contributor to stroke burden, with 33 million stroke-related DALYs in 2013. Although the world average of stroke burden attributed to air pollution was 30%, it ranged from 34% in low- to middle-income countries to 10% in high-income countries. Cohen et al. showed that stroke and coronary heart disease represent a large proportion of deaths due to PM2.5 and have shown a steady and significant increase since 1990 (Cohen et al., 2017).
The 2017 report by the Lancet Commission on pollution and health provides data in support of pollution being the most important environmental cause of disease and premature death worldwide (Landrigan, Fuller, Acosta, et al., 2017). Air pollution causes more deaths than water, occupational and soil pollution combined; it results in three times more deaths than HIV, tuberculosis and malaria combined and 15 times more deaths than those caused by war and other violence. In 2015, air pollution accounted for 26% of coronary heart disease deaths and for 23% of stroke deaths, reflecting 21% of cardiovascular deaths overall (Landrigan et al., 2017). These deaths have an age peak in children under the age of 5 years, although the largest absolute number of deaths occurs over 55 years of age. Because of the significant number of years in age expectancy, the largest number of DALYs lost affect children.
Air Pollution and Congenital Heart Disease
The fetus offers the most vulnerable state for pathogenic effects of toxin exposure and is exposed to a higher relative toxin dose compared to the mother. The most robust correlation was found between the air pollutant nitrogen oxide and coarctation of the aorta, Fallot tetralogy, and ventricular and atrial septal defects (Jerrett, McConnell, Wolch, et al., 2014; Mao, Sun, Zhang, et al., 2017). The causative mechanism appears to be DNA hypomethylation from the interaction of nitrogen oxide and methionine. It is also feasible that due to cardiac structural changes and a greater incidence of metabolic syndrome, exposed fetuses remain predisposed to have a higher risk of cardiovascular events (Chen, Zmirou-Navier, Padilla, & Deguen, 2014).
Conclusions
The health costs of air pollution are hidden behind a myriad of heart attack and stroke hospital admissions. A vast proportion of affected patients admitted for a first episode have no known common vascular risk factors, so they are labeled as heart or brain infarctions “of unknown etiology.” I have provided ample evidence to support the causality between acute and chronic exposure to air PM2.5 (and other pollutants) and the occurrence of acute myocardial infarction and stroke. However, this is rarely considered causative by physicians providing hospital care to patients and much less by clinic administrators and politicians who are responsible for generating and implementing legislation for air pollution control. Air pollution accounts for at least 6% of global health care expenses (Landrigan et al., 2017). However, the increasing costs of health care, and especially those related to the growing epidemic of noncommunicable diseases (led by heart disease and stroke) are easily identified in hospital financial statements.
Investments in air pollution control are largely cost effective. Following the 1970 Clean Air Act in the USA, air pollution decreased by 70% with a greater than 210% related GDP increase (U.S. EPA, n.d.). In contrast, in California for every 10 μg/m3 increase in PM, there is an associated 6% decrease in productivity. The myth promoting the idea that pollution is an unavoidable consequence in the transition to economic development, the so-called Kuznets hypothesis, has long been proven wrong (Kuznets, 1955). The problem is large and complex enough that different government areas, including financial, health, and environmental agencies, must coordinate efforts to effectively tackle this enormous challenge. Efforts to educate the general public and the medical community need to evolve in parallel with government, multinational, and corporate decisions to decrease the causes of air pollution and climate change as different components of the same problem that directly endanger human life. In the encyclical letter “Laudato Si,” Pope Francis makes a thorough analysis of the threat and danger posed to our planet by current human behavior (Francis, 2015). The Holy Father reminds us that several popes before him expressed concern about an ongoing destructive attitude of humanity towards our “common home.” Pope Francis made an “urgent appeal” for dialogue about the future of our planet dominated by a “throwaway culture” while being converted in an “immense pile of filth.”
By thoroughly covering the broad spectrum of climate change, air pollution and health, this book ought to be the tipping point to help reverse the present course of this avoidable disaster facing both the current and future human generations.
References
Ashby-Mitchell, K., Burns, R., Shaw, J., & Anstey, K. J. (2017). Proportion of dementia in Australia explained by common modifiable risk factors. Alzheimer’s Research Therapy, 9, 11.
Bhatt, D. L., Steg, P. G., Ohman, E. M., et al. (2006). International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. Journal of the American Medical Association, 295, 180–189.
Brauer, M., Freedman, G., & Frostad, J., et al. (2016). Ambient air pollution exposure estimation for the global burden of disease 2013. Environmental Science & Technology, 50, 79–88.
Brook RD, Franklin B, Cascio W, et al., for the Expert Panel on Population and Prevention Science of the American Heart Association (2004). Air pollution and cardiovascular disease: A statement for healthcare professionals from the expert panel on population and prevention science of the American Heart Association. Circulation, 109, 2655–2671.
Brook, R. D., Rajagopalan, S., Pope, C. A., et al. (2010). Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation, 121, 2331–2378.
Brook, R. D., Urch, B., Dvonch, J. T., et al. (2009). Insights into the mechanisms and mediators of the effects of air pollution exposure on blood pressure and vascular function in healthy humans. Hypertension, 54, 659–667.
Chen, E. K., Zmirou-Navier, D., Padilla, C., & Deguen, S. (2014). Effects of air pollution on the risk of congenital anomalies: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 11, 7642–7668.
Chiuve, S. E., McCullough, M. L., Sacks, F. M., & Rimm, E. B. (2006). Healthy lifestyle factors in the Primary prevention of coronary heart disease among men: Benefits among users and nonusers of lipid lowering and antihypertensive medications. Circulation, 114, 160–167.
Claeys, M. J., Rajagopalan, S., Nawrot, T. S., & Brook, R. D. (2017). Climate and environmental triggers of acute myocardial infarction. European Heart Journal, 38, 955–960.
Cohen, A. J., Brauer, M., Burnett, R., et al. (2017). Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet, 389, 1907–1918.
Di, Q., Wang, Y., Zanobetti, A., et al. (2017). Air pollution and mortality in the Medicare population. New England Journal of Medicine, 376, 2513–2522.
Dockery, D. W., Pope, C. A., Xu, X., et al. (1993). An association between air pollution and mortality in six U.S. cities. New England Journal of Medicine, 329, 1753–1759.
Ensor, K. B., Raun, L. H., & Persse, D. (2013). A case-crossover analysis of out-of-hospital cardiac arrest and air pollution. Circulation, 127, 1192–1199.
Estol, C. J. (2019). Is breathing our polluted air a risk factor for stroke? International Journal of Stroke, 14, 340–350.
Feigin, V. L. (2005). Stroke epidemiology in the developing world. Lancet, 365, 2160–2161.
Feigin, V. L., Norrving, B., & Mensah, G. A. (2017). Global burden of stroke. Circulation Research, 120, 439–448.
Feigin, V. L., Roth, G. A., Naghavi, M., et al. for the Global Burden of Diseases, Injuries, and Risk Factors (2016). Global burden of stroke and risk factors in 188 countries, during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013 and Stroke Experts Writing Group. Lancet Neurology, 15, 913–924.
Forastiere, F., & Agabiti, N. (2013). Assessing the link between air pollution and heart failure. Lancet, 382, 1008–1010.
Pope Francis. (2015). Laudato Si’: On Care for Our Common Home [Encyclical].
Global Burden of Disease 2015 Risk Factors Collaborators (2016). Global, regional, and national comparative risk assessment of 79 behavioral, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet, 388, 1659–1724.
Gold, D. R., & Samet, J. M. (2013). Air pollution, climate, and heart disease. Circulation, 128, e411–e414.
Hackam, D. G., & Spence, J. D. (2007). Combining multiple approaches for the secondary prevention of vascular events after stroke: A quantitative modeling study. Stroke, 38, 1881–1885.
Heitzer, T., Yla-Herttuala, S., Luoma, J., et al. (1996). Cigarette smoking potentiates endothelial dysfunction of forearm resistance vessels in patients with hypercholesterolemia. Circulation, 93, 1346–1353.
Jerrett, M., McConnell, R., Wolch, J., et al. (2014). Traffic-related air pollution and obesity formation in children: A longitudinal, multilevel analysis. Environmental Health, 13, 49.
Kaufman, J. D., Adar, S. D., Allen, R. W., et al. (2012). Prospective study of particulate air pollution exposures, subclinical atherosclerosis and clinical cardiovascular disease: The Multi-Ethnic Study of Atherosclerosis and Air Pollution (MESA Air). American Journal of Epidemiology, 176, 825–837.
Kaufman, J. D., Adar, S. D., Barr, R. G., et al. (2016). Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the Multi-Ethnic Study of Atherosclerosis and Air Pollution): A longitudinal cohort study. Lancet, 388, 696–704.
Kristen, E., Cosselman, K. E., Krishnan, R. M., Oron, A. P., et al. (2012). Blood pressure response to controlled diesel exhaust exposure in human subjects. Hypertension, 59, 943–948.
Kuznets, S. (1955). Economic growth and income equality. American Economic Review, 45, 1–28.
Landrigan, P. J., Fuller, R., Acosta, N. J. R., et al. (2017). The Lancet Commission on pollution and health. Lancet, 391, 462–512. https://doi.org/10.1016/S0140-6736(17)32345-0
Langrish, L. X., Wang, S., Lee, M. M., et al. (2012). Reducing personal exposure to particulate air pollution improves cardiovascular health in patients with coronary heart disease. Environmental Health Perspectives, 120, 367–372.
Lelieveld, J., Evans, J. S., Fnais, M., et al. (2015). The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature, 525, 367–371.
Lelieveld, J., Klingmuller, K., Pozzer, A., et al. (2019). Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. European Heart Journal, 40, 1590–1596. https://doi.org/10.1093/eurheartj/ehz135
Li, H., Cai, J., Chen, R., et al. (2017). Particulate matter exposure and stress hormone levels: A randomized, double-blind, crossover trial of air purification. Circulation, 136, 618–627.
Lim, S. S., Vos, T., Flaxman, A. D., et al. (2012). A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet, 380, 2224–2260.
Lin, J., Pan, D., Davis, S. J., et al. (2014). China’s international trade and air pollution in the United States. Proceedings of the National Academy of Sciences of the United States of America, 111, 1736–1741.
Link, M. S., & Dockery, D. W. (2010). Air pollution and the triggering of cardiac arrhythmias. Current Opinion in Cardiology, 25, 16–22.
Link, M. S., Luttmann-Gibson, H., Schwartz, J., et al. (2013). Acute exposure to air pollution triggers atrial fibrillation. Journal of the American College of Cardiology, 62, 816–825.
Mao, G., Sun, Q., Zhang, X., et al. (2017). Individual and joint effects of early-life ambient PM2.5 exposure and maternal prepregnancy obesity on childhood overweight or obesity. Environmental Health Perspectives, 125, 067005. https://doi.org/10.1289/EHP261
Mijajlović, M. D., Pavlović, A., Brainin, M., et al. (2017). Post-stroke dementia—A comprehensive review. BMC Medicine, 15, 11.
Miller, K. A., Siscovick, D. S., Sheppard, L., et al. (2007). Long-term exposure to air pollution and incidence of cardiovascular events in women. New England Journal of Medicine, 356, 447–458.
Morishita, M., Thompson, K. C., & Brook, R. D. (2015). Understanding air pollution and cardiovascular diseases: Is it preventable? Current Cardiovascular Risk Reports, 9, 30.
Mozaffarian, D., Benjamin, E. J., Go, A. S., et al. (2015). Heart disease and stroke statistics. 2016 update. A report from the AHA. Circulation, 138, e38–e360.
Münzel, T., Daiber, A., Steven, S., Tran, L. P., Ullmann, E., et al. (2017). Effects of noise on vascular function, oxidative stress, and inflammation: Mechanistic insight from studies in mice. European Heart Journal, 38, 2838–2849.
Mustafić, H., Jabre, P., Caussin, C., et al. (2012). Main air pollutants and myocardial infarction: A systematic review and meta-analysis. Journal of the American Medical Association, 307, 713–721.
Nemmar, A., Vanbilloen, H., Hoylaerts, M. F., et al. (2001). Passage of intratracheally instilled ultrafine particles from the lung into the systemic circulation in hamster. American Journal of Respiratory and Critical Care Medicine, 164, 1665–1668.
Newby, D. E., Mannucci, P. M., Tell, G. S., et al.. for the ESC Working Group on Thrombosis, European Association for Cardiovascular Prevention and Rehabilitation, ESC Heart Failure Association (2015). Expert position paper on air pollution and cardiovascular disease. European Heart Journal, 36, 83–93.
Norton, S., Matthews, F. E., Barnes, D. E., Yaffe, K., & Brayne, C. (2014). Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurology, 13, 788–794.
Ostro, B., Hu, J., Goldberg, D., et al. (2015). Associations of mortality with long-term exposures to fine and ultrafine particles, species and sources: Results from the California Teachers Study Cohort. Environmental Health Perspectives, 123, 549–556.
Pell, J. P., Haw, S., Cobbe, S., Newby, D. E., et al. (2008). Smoke-free legislation and hospitalizations for acute coronary syndrome. New England Journal of Medicine, 359, 482–491.
Pope, C. A., Burnett, R. T., Krewski, D., et al. (2009). Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: Shape of the exposure-response relationship. Circulation, 120, 941–948.
Ruidavets, J. B., Cournot, M., Ferrières, J., et al. (2005). Ozone air pollution is associated with acute myocardial infarction. Circulation, 111, 563–569.
Shah, A. S. V., Lee, K. K., McAllister, D. A., et al. (2015). Short term exposure to air pollution and stroke: Systematic review and meta-analysis. British Medical Journal, 350, 1295.
Stafoggia, M., Cesaroni, G., Peters, A., et al. (2014). Long-term exposure to ambient air pollution and incidence of cerebrovascular events: Results from 11 European cohorts within the ESCAPE project. Environmental Health Perspectives, 122, 919–925.
Strong, K., Mathers, C., Leeder, S., & Beaglehole, R. (2005). Preventing chronic diseases: How many lives can we save? Lancet, 366, 1578–1582.
Sung, Q., Wang, A., Jin, X., et al. (2005). Long term air pollution exposure and acceleration of atherosclerosis and vascular inflammation in an animal model. Journal of the American Medical Association, 294, 3003–3010.
U.S. EPA. (n.d.). Comparison of Growth Areas and Emissions, 1980–2013.
van Donkelaar, A., Martin, R. V., Brauer, M., & Boys, B. L. (2015). Use of satellite observations for long-term exposure assessment of global concentrations of fine particulate matter. Environmental Health Perspectives, 123, 135–143.
Yusuf, S., Hawken, S., Ounpuu, S., et al. (2004). Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study). Lancet, 364, 937–952.
Acknowledgements
The author is grateful to Sarah MacKenzie, Ph.D., for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Estol, C.J. (2020). Air Pollution and Cardiovascular Disease: A Proven Causality. In: Al-Delaimy, W., Ramanathan, V., Sánchez Sorondo, M. (eds) Health of People, Health of Planet and Our Responsibility. Springer, Cham. https://doi.org/10.1007/978-3-030-31125-4_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-31125-4_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-31124-7
Online ISBN: 978-3-030-31125-4
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)