Abstract
People affected by the frozen shoulder syndrome show limited shoulder mobility which is often accompanied by pain. The frozen shoulder syndrome often lasts from months to years, and mostly affects people in the age group of 40 to 70 years. The frozen shoulder syndrome severely reduces the quality of life and the ability to work. A common treatment method is physiotherapy. Patients are referred to a physiotherapist, who selects specific exercises adapted for the specific patient. Physiotherapy requires patient compliance, time, and effort. Correct exercise performance and compliance are the main issues in physiotherapy. A smartphone app could support patients by providing detailed exercise instructions and motivation through exercise logging, as is common for fitness and sport. In this work, such an app for frozen shoulder syndrome, the ShoulderApp, is evaluated in two user studies. The main contribution is that the user studies were conducted in an ambulatory assessment setting, which allows to draw conclusions about real-world usage, usability and user acceptance. The app was regularly used and study participants were satisfied. Additionally, we researched the usability and usage of interactive 3D and multi-modal exercise instructions, motivational aspects, exercise correctness and the interplay of physiotherapy and app usage. Measurements of shoulder mobility are the key assessment tool for the state and progress of the frozen shoulder syndrome. A smartphone sensor-based measurement tool, which only required a simple band in addition to the smartphone, was developed and evaluated. Interventions with the ShoulderApp were evaluated in a three-week short-term intervention and an 18-week midterm evaluation with 5 patients each. For the evaluation of the results, we used standardized questionnaires, SUS, TAM-2, and USE. In addition, semi-structured interviews and automatic logging of user-interactions in the app were included as the outcome measurements. Overall, the results for both the short-term and mid-term user studies showed that the ShoulderApp could support physiotherapy for frozen shoulder patients. The positive results of the studies show the potential of a generalization of the ShoulderApp concept to the large group of musculoskeletal disorders such as lower back pain and knee injuries.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Patients with frozen shoulder syndrome show a decreased mobility of the upper extremities often accompanied by severe pain. Frozen shoulder syndrome may occur in one or both shoulders. The incidence of the frozen shoulder syndrome is reported to be 2–5% in the general population [25] and patients in the age group between 40 and 70 are affected more frequently [8]. The frozen shoulder syndrome is diagnosed by a physician, often patients are then referred to shoulder specialists for diagnosis. A common treatment option is physiotherapy, including mobilization and strength exercises [15]. In most cases, mobilization and strength exercises are conducted at home and not under the constant supervision of a physiotherapist. However, even with treatment the frozen shoulder syndrome is long lasting and patients may require years to fully recover and in some cases limitations in the range of motion persist.
Physiotherapy is often prescribed for a limited number of sessions (around 10) as health insurance does not cover more sessions (at least in Austria). Patients with frozen shoulder syndrome are thus likely to pinball between physicians (prescribing physiotherapy) and physiotherapists (conducting physiotherapy) in the course of their disease, which leads to gaps in treatment and information.
Home-based physiotherapy has two main issues: correct exercise performance and compliance [12, 13]. In [36] non-compliance rates as high as 70% are reported and in [19] it is reported that the majority of patients are not performing the home-exercises correctly two weeks after their initial instruction. In previous work, a smartphone app that supports patients during therapy in order to reduce the problems of exercise compliance and correctness has been proposed and evaluated in a short-term intervention. The app used a 3D avatar to show the correct exercise conduct and also provided text and audio descriptions of the exercises. Compared to traditional methods for home-instructions, which are either paper-based (text and illustrations) or videos [29], 3D animations allow better communication of complex 3D movements. Even for interactive video-based physiotherapy, the 2D representation complicates the understanding of 3D body movements [1], because of the missing depth information. Exercises that are performed by a 3D avatar allow the user to freely adjust the view point. Thus depth and therefore exact body movements can be perceived and the animated exercise allow vicarious learning. Additionally, the app for frozen shoulder patients offers more functionality such as an exercise diary and progress assessment, which support the patient exercising compliance.
Home-exercising requires a significant behavior change. According to Fogg’s behavior model (FBM) [22], successful behavior change depends on three main factors, motivation, ability and triggers. While frozen shoulder patients have an intrinsic motivation to perform home-based exercises to improve their condition, a study context is expected to raise motivation and provide extrinsic motivation by regular supervision and follow-up meetings. A main contribution of an app is towards the factor ability in FBM. The app increases the ability to perform the home-based exercises correctly as it provides the patients with precise instructions on how to perform the exercises. Additionally, the permanent availability of a smartphone and the included diary and progress monitor provide constant triggers.
A user study in a short-term intervention (3 weeks) showed great potential of the app as support system for home-based physiotherapy. However, the frozen shoulder syndrome is a long-term disease and thus a short-term success is only a precondition for an evaluation over a longer period. In this work, the results of a short-term and a mid-term intervention (18 weeks) are presented and thoroughly analysed in order to answer whether an app can support physiotherapy and whether an app is general feasible in the context of home-based physiotherapy. The main focus is on the analysis of the interviews of the patients and the physiotherapists with respect to usability, 3D interaction and multimodal exercise instructions, motivation, mobility measurements in the app, and the interplay of physiotherapy and app usage.
The implemented study design did not require a formal approval by the ethics committee as the regular treatment remained unchanged and the app did not classify as a medical device (see Sect. 3.5).
2 Related Work
There has been a tremendous interest in industry of assistance technology of fitness and well-being of the general (healthy) population, e.g., by major companies, such as Google (Google Fit) and Apple (Apple Health). Apart from general health and fitness, several specific medical and rehabilitation issues have been addressed in the HCI and the medical community. Among these issues were stroke rehabilitation [6], Parkinson’s disease [34], cerebral palsy [16], autism [28] and, most importantly for the focus of this work, musculoskeletal disorders (MSDs) [12, 13] including disorders of the knee [5] and the shoulder [21, 27].
A smartphone app could tackle important obstacles for physiotherapy at home in the context of musculoskeletal disorders: comprehensible and easily accessible exercise instructions, compliance and progress monitoring as established by Chandra et al. [12, 13].
Previous work can be classified in terms of the used technology and hardware, which ranges from the application of professional tracking hardware to everyday smartphones.
Professional tracking systems capable of precisely tracking patient motion have been used by Tang et al. for physiotherapy at home [39, 40]. The application of virtual reality systems to support physiotherapy was proposed by Gourlay et al. [23] and by Yim et al. [43]. Augmented reality head sets for physiotherapy were investigated by Dezentje et al. [17] and in follow-up work by Cidota et al. [14]. Liu et al. employed a humanoid robot in an interactive training system of motor learning [28].
Also the application of the Kinect body tracking system for physiotherapy was proposed by Nixon et al. [31], Anderson et al. [4], by Zhao et al. [44], by Smeddinck et al. [37] and by Fikar et al. [21].
The Nintendo Wii system was investigated by Deutsch et al. [16] and off-the-shelf Nintendo Wii Fit exer-games were evaluated with respect to the retention of motor skills of patients with Parkinson’s disease by do Santos Mendes et al. [34].
Doyle et al. proposed an IMU-sensor based system for exercises [18]. A wearable device for knee rehabilitation was proposed by Ananthanarayan et al. [3] and by Ayoade et al. [5]. Huang et al. proposed a cap with an IMU (Sense-Cap) to monitor balance exercises [24]. Schönauer et al. proposed an IMU-based system to provide motion guidance [35].
Buttussi et al. proposed a mobile system for fitness training [10, 11]. Op den Akker gave an overview of user-tailored activity coaching systems [2]. Smartphone apps were investigated for physiotherapy by Postolache et al. [33]. A reminder app for stroke patients was proposed by Micalle et al. [30]. Vorrink et al. developed and evaluated a mobile phone app to encourage activity in COPD patients [42].
The strength of our contribution is that actual patients used the system in their everyday setting over an extended period of time. This strength is especially noteworthy with respect to most related contributions of the HCI community which mostly focus on laboratory studies. Laboratory studies are not able to capture the complexities which arise out of actual systems in real life application settings.
3 Methods
In this work the results of a three-week short-term intervention and an 18-week mid-term evaluation of home-based physiotherapy supported with an smartphone app, the ShoulderApp, are presented. The app was developed with the support of a shoulder surgeon and four physiotherapists from the department of physiotherapy.
3.1 ShoulderApp
The ShoulderApp starts with the main screen (see Fig. 1a), which shows five buttons for the five different screens of the app.
Training Mode. The most frequent task of a user affected by the frozen shoulder syndrome, exercising, is supported by a training mode. Pressing the first button starts the training mode (“Trainingsmodus”), in which an animation with audio description shows the exercises selected for the user (see Fig. 1b). A basic exercise is repeated several times, usually 10–20 times, in a set. After each set the patient confirms the set, by pressing the ok button (see Fig. 1b in the bottom right of the screen). 2–3 sets are commonly selected by physiotherapists. After the last set, the app returns to the main screen.
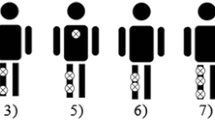
Sensor-Based Mobiltiy Measurement. The second button starts the mobility measurement (“Beweglichkeitstest”). Shoulder mobility is measured along four different movement axes (see Fig. 2). These measurements are the key metrics to track the progress and monitor the course of the frozen shoulder syndrome.
The patient could choose between two methods of assessing the mobility by pressing the corresponding button (see Fig. 3a). In the manual input mode, the patient uses a slider to adjust the avatar’s arm position (see Fig. 2). In the sensor-based mobility measurement, the smartphones IMU (inertia measurement unit) is used. The smartphone is placed in a common smartphone band, which is commonly used for exercising, e.g. running (see Fig. 4). This approach needs minimal additional hardware, only a very cheap band is additionally necessary. The patient puts the band with the smartphone on the upper-arm (for the lateral and frontal arm lift) and on the forearm (for the lateral rotation and the back scratch). The patient presses the large start button (see Fig. 3b), moves the arm into the starting position and waits for an audible beep (3 s after pressing the start button). The patient should move the arm to the maximal extent without pain. The maximum extent of movement, i.e. the maximum angle, is recorded and the next measurement along a different axis is started.
Calendar Overview. The third button starts a calendar overview of the performed trainings and the mobility measurements (see Fig. 5a). Left and right arrow allow to change the month. The home button returns to the main screen.
Exercise Configuration. The fourth button starts the planning view, in which the patient or the physiotherapist can choose exercises and the number of sets appropriate for the patient (see Fig. 5b). Left and right arrow allow to change the exercise. The numer of sets can be by the minus and plus buttons. The home button returns to the main screen.
3.2 Study Design
The studies were designed as an ambulatory assessment where the participants were briefed before the intervention [20]. The main motivation for this design choice was to get as closely as possible to real at-home usage as possible within the study. The studies were conducted using a within-subject design [26]. While the percentage of people affected by the frozen shoulder syndrome in a life time is relatively high (around 10% are reported), the percentage of people affected by frozen shoulder syndrome at any given moment is comparably low (2–5% are reported). Participants were acquired by a physician among his/her patients diagnosed with frozen shoulder. Inclusion criteria were a diagnosis of frozen shoulder and the willingness to voluntarily participate in the study. Exclusion criteria were other chronic diseases, which would rule out the idiopathic nature of the shoulder stiffness. Different patients were used for the short-term intervention and the mid-term intervention. As one of the main issues in the treatment of frozen shoulder is the long duration of the disease, fewer patients and longer study durations were chosen.
The plan was to start with a user study based on 3 week short-term intervention and in the case of success, extend the duration to gain more insights in the long-term usage. After the success of the first short-term user study, the length of the second mid-term intervention user study was extended to 18 weeks.
The main focus of the user studies was the long-term usage and the assessment of the general feasibility of an app in the context of home-based physiotherapy.
Usage, Usability, and 3D Interaction and Multi-modality. It was unclear whether the patients and the physiotherapists would accept an app to support the treatment of the frozen shoulder syndrome. The question was in particular whether an app can support the home-based therapy over an extended period. Also, it was not clear whether patients would accept the interaction with animated 3D content and which modality is suited to communicate physiotherapy exercises.
Correct Exercise Performance and Concordance of Physiotherapy and App. A main question was whether the exercises are performed correctly, which can only be assessed by a professional physiotherapist. Also, the concordance and inter-relations between standard physiotherapy sessions and app usage was considered an interesting topic in the study design. In the first study, the patients continued their individual physiotherapy with their own therapists (who were not part of the study team). In the second study, the participants were provided with physiotherapy sessions from the study team. They discontinued the therapy with their own therapists. All participating physiotherapists were under supervision of a leading physiotherapist, who provided guidelines for the physiotherapy sessions. This design decision assured the concordance of physiotherapy and app intervention.
Mobility Measurement. As mobility measurements of the joint are the main clinical parameters in the assessment of the state/progress of the frozen shoulder treatment, these measurements are of great importance. Therefore, mobility measurements were part of the physiotherapy sessions and were included in the app as well. The focus of the study of the app measurements was not accuracy, but whether patients would actually perform such measurements with a band at home. We found that accuracy was not an issue if high-quality smartphones were used. Given the trend towards mobile augmented and virtual reality, the accuracy of the IMU sensors will improve anyway in the near future. Therefore, accuracy is not interesting in this context, but the question whether patients accept this method with the smartphone in a band at all is crucial.
Motivation. A further interest in the studies was patient motivation: which elements of the intervention and the app increase patient motivation and motivate them to conduct the exercises accurately and regularly at home.
Further Improvements and Pain Logging. We wanted to know which ideas for improvements, especially to increase motivation for regular exercising, were derived by the patients during their experience with the provided app. Specifically, we were interested whether patients would like to integrate the possibility to log pain. Nightly pain often causes severe sleep deprivation for frozen shoulder patients. Regular nightly pain over an extended period would in fact be an argument for surgical intervention.
3.3 Study Flow
The first step was the design, conduct and evaluation of a short-term intervention.
Short-Term Intervention. In the first meeting patients were instructed by the physiotherapist and the app was made available for the following three weeks. In the second meeting, the outcome measures were evaluated (usability questionnaires and individual semi-structured interviews (for details see Sect. 3.4).
Mid-Term Intervention. After the successull short-term intervention, the study duration was significantly extended to 18 weeks. The study was again designed as an ambulatory assessment where the participants were briefed before, in-between and after the intervention [20]. Additionally, weekly physiotherapy session were provided. The outcome measures were evaluated in the second and the third (final) session (see Sect. 3.4).
In the first meeting with the patients, patients were informed about the study and its goals. The ShoulderApp was made available. The exercises and the app usage were explained by a physiotherapist and a computer scientist.
A patient information sheet, including study goals and details, the voluntary participation, the data collected by the app and a privacy statement was signed. Patients were instructed to use the app daily to log the training, and to conduct at least one mobility assessment per week. In order to rule out interference with their regular physiotherapist, physiotherapy was provided by the department of physiotherapy at most twice per week. The physiotherapy sessions were provided under the supervision of the leading physiotherapist. However, the app and the exercises in the app were deliberately not part of these physiotherapy sessions in order to get insight into the stand-alone app usage over a longer period. Furthermore, the study period over Christmas lead to around three weeks without seeing a physiotherapist and to app usage and home-exercising in a usually rather unstructured period for the patients (public holidays and Christmas vacations).
In the second meeting (in-between) and third meeting (final) with the patients, standardized questionnaires were evaluated and a personal semi-structured interview with each patient was conducted.
In the second meeting, patients were instructed to use the app only if they wanted and to continue therapy with their regular physiotherapist.
3.4 Outcome Measures
The outcome measures included standardized questionnaires, automatic logging of user-interactions in the app, and semi-structured interviews. The interviews were recorded (audio) and a qualitative content analysis (see [32]) was performed.
Usage, Usability, and 3D Interaction and Media. For the evaluation of the participants’ satisfaction we conducted the System Usability Scale (SUS) by [9]. Additionally, selected parts (intention to use, perceived usefulness, perceived ease of use) of the revised Technology Acceptance Model (TAM-2) [38, 41], and the USE (Usability, Satisfaction, and Ease of use) questionnaire which was used in previous work [42], were evaluated. For the interpretation of SUS scores we referred to [7].
The app tracks usage details in log files. The log files from the participants’ smartphones were collected and analysed in order to gain insight into the actual usage in everyday life.
Participants were asked about their interactions with the app (e.g., did you change the view port?, did your read the instructions?) and their app usage contexts, e.g. alone at home.
Mobility Measurement. Mobility measurements are recorded in the log files of each user. As the short-term intervention revealed usability issues of the mobility measurement with smartphone sensors, this part of the app was revised and optimized (more explanation and an in-detail walk-through for the user of the necessary steps). Additionally, the USE: Ease of Learning questionnaire was rephrased such that questions 3 and 4 were specific to the sensor-based measurement routine.
Motivation. Our semi-structured interviews contained questions on the motivating effects of individual app aspects.
Correct Exercise Performance and Concordance of Physiotherapy and App. The physiotherapists assessed the correctness of the exercise performance in both interventions.
In the mid-term intervention we asked whether the app could replace actual physiotherapy sessions. The physiotherapists assessed the correctness of patients’ exercise performance (of the exercises shown in the app). The leading physiotherapist was interviewed twice in the mid-term intervention.
Improvements and Pain Logging. To gather app improvement possibilities we asked each participant open questions about what they liked and what they disliked about the intervention and the app. We asked for suggestions for improvements in the overall conduct of the study and whether the initial personal instructions about how to use the app were necessary.
Specifically we asked whether patients would like to add a pain logging module.
3.5 Ethics Committee
We have informed the ethics committee of the county of Salzburg of the studies, however, the implemented study design did not require a formal approval by the ethics committee. A formal approval of a study from the ethics committee is needed if (a) regular treatment is changed (b) a medical device is tested. In the presented studies, the physician and physiotherapists and physicians assured, that only patients were selected for which the app was completely in line with their regular treatment. Based on the recommendation of the ethics committee we have carefully reviewed EU directive on medical devices (MEDDEV 2.1/6) to determine wether the evaluated app is a medical device. According to the definitions in the guidance document, the app is “stand-alone software”. However, the software (app) does not perform an action on data different from storage, archival, communication or simple search (see Figure 1 of the Guidance Document MEDDEV 2.1/6 July 2016). The ShoulderApp stores the 3D instructions for home-based exercises (which would commonly just be explained by the physiotherapists) and provides exercise and mobility logging (which would commonly be done individually by the patients using their preferred tools, such as a paper or online calendar). Therefore, to the best of our assessment, the app is not covered by the medical device directive and not considered a medical device and standalone medical software. Therefore, a formal ethics committee approval process was determined to be not applicable.
3.6 Patient Recruitment
The patients were selected from the patient pool of the physician. Patients meeting the inclusion criteria were selected from the patient database of the head shoulder surgeons practice and contacted by the office of the head shoulder surgeon. Special care was taken that the regular treatment plan of the included patients was in line with the implemented treatment with app support in the studies. The patients were informed of the outline of the study, the timeline and their eligibility for free and voluntary participation.
4 Results
A short-term intervention was conducted in July 2016 for a duration of three weeks. Five patients (4f, 1m) with the frozen shoulder syndrome participated voluntarily. One physiotherapist was part of the study execution.
A mid-term intervention with 5 patients (3f, 2m) was conducted from December 21 2016 to April 24 2017. For this study, the instructions for the mobility measurement with sensors were improved in the app. On December 21 the user study started with a personal meeting of the patients and the leading physiotherapist (FH) and the computer scientist (TS) who was responsible for the app development. Patients were provided with physiotherapy sessions up to two times a week, which were conducted by 6 physiotherapists in training under the supervision of the leading physiotherapist. After the second in-between session (Feb 20), patients continued their regular treatment with their own therapists and were free to use the app and its exercises. A third and final session on April 24 was held to gather information on the app usage “in the wild” without accompanying measures by the study team. Four patients showed up to the third and final session (one patient did not show up).
4.1 Usage, Usability, 3D Interaction and Multi-modality
In the short-time intervention, patients reported that they used the app almost daily to get instructions and to track exercising. Their statements were confirmed by the usage log files. The results of standardized questionnaires (SUS, TAM-2, USE) are given in Table 1. Overall, these results indicate a usable and well-accepted system that is easily learnt.
Also in the in-between evaluation of the mid-term intervention, patients reported that they used the app almost daily to get instructions and track exercising. Their statements were confirmed by the usage log files, but mobility measurements were only conducted a few times except for one patient. The results of standardized questionnaires (SUS, TAM-2, USE) are given in Table 2. Overall, these results indicate again a usable and well accepted system that is easily learnt.
Even when the patients were free to continue to use the app after the in-between meeting, only one patient stopped using the app, as her condition had very much improved. Three patients reported that they had continued to use the app almost daily, which was again confirmed by the log files. These three patients are considered for the standardized questionnaires. The results are given in Table 3 and indicate again a usable and well-accepted system that is easily learnt.
Patients reported that they usually performed the exercises at home and mostly alone, either in the morning or the evening. One patient added that he performed the exercise alone in his hotel room on a business trip in the evening.
3D Interaction and Media. All patients of the short-time intervention changed the view port in order to view the exercises from different angles and to have better control of their own conduct of the exercise. Only two patients reported that they did not read the instructions at all, three patients and one partner used the text instructions. In the mid-term evaluation, two patients reported that they changed the view port of the animation. One of these two patients reported that “I have rotated the animation in order to see exactly how to correctly perform the exercise”. The other said, “that he prefers a 3D animation compared to video or illustrations, because one can zoom-in on the interesting parts”. The other three patients watched the 3D animations from the default view port. All patients reported that the avatar was sufficient and that they did not require further options, e.g., a female avatar.
In the short-term intervention, three patients said the audio was helpful. Two patients and the partner of a patient did not find the audio instructions helpful. Three patients reported that the audio description helped a lot at the beginning, while two patients did not find the audio description of the animation helpful. In the mid-term intervention, three patients did not read the exercise description (3D animation and audio was sufficient), but two read the description several times at the beginning. In the mid-term evaluation, one patient said that he really liked the visualization/animation of the exercises, which made it easy to understand how to perform the exercises.
4.2 Motivation
In the short-term intervention, one patient said that she liked that the app motivated her to regularly and properly conduct the exercises. One patient reported that she especially liked a certain exercise (stretching in the door). One patient reported that she liked the simplicity of the program and that the app would even be usable for someone with no smartphone usage experience. The introduction to the app and the exercises in the first meeting were positively mentioned as well. All patients reported that they found the support of physiotherapy with an app useful. One patient asked to use the app after the study, because she found the app motivating.
In the mid-term intervention’s in-between interview, one patient remarked that she liked the intervention because it is nice that you are taken seriously. Another patient liked that the app helps remembering the exercises and gives an overview of the conducted trainings. Another patient liked the detailed explanation and the strict schedule imposed by the app. That patient remarked: “I know that I can make the entries without doing the exercises, but I liked the feeling of control/empowerment when I could check off a training”. In the mid-term intervention’s final evaluation, one patient noted, that “I liked to see the improvements in the mobility measurements over time. This motivated me to keep on exercising.” All four patients found the study/mid-term intervention useful. One patient added that “also the intervention itself, the study context, motivated me”.
Asked about an outlook and improvements for the app, one patient noted that she would be motivated by the physiotherapist looking into her app data.
4.3 Mobility Measurement
In the short-time intervention, one patient reported that they conducted the manual mobility measurement (without sensors) together and that the joint usage of the app was enjoyable. Another patient said that the instructions for the mobility measurement were insufficient. One patient reported that a different choice of bands would be recommended, which allow the usage on the upper arm und forearm without adjustment. One patient said that the current manual mobility measurement required a second person. Three patients used the measurement with the sensors. One did not know how to conduct the measurements and one smartphone did not support the sensor measurement. Furthermore one patient slightly misunderstood the measurement process, which made it more cumbersome, as she thought she had to press the accept measurement button at the maximum angle of movement (which does no not lead to repeatable results). Two patients reported that the sensor-based mobility measurement would benefit from better instructions in the first meeting and in the app. One patient recommended that at least one measurement should be done by the patient in the first meeting. In the mid-term intervention’s in-between evaluation, we investigated whether the improvements of the sensor-based measurements were successful. However, a closer look at the results for the sensor-based mobility measurement (see Table 5 and compare to the results of the short-term study in Table 4) shows that the improvements of this module were not successful. The patients did not find the sensor-based mobility measurement easy to learn (Table 6).
Four patients did not use the sensor-based measurements regularly, only one patient did. This patient did the mobility measurements with the help of her partner (as one patient of the short-term intervention did). This patient reported that “[the partner] put it on me [the smartphone] and pressed the button for me.” Two patients said that the sensor-based mobility measurement on the back was too complicated. Another patient explained that she did not do the measurements, as the physiotherapist did the measurement in the session and she preferred it that way. Also, more time to learn the sensor-based assessment did not help to improve the acceptance of the sensor-based measurement module.
In the final interview of the mid-term intervention, three patients stated that they would prefer it if the physiotherapist conducted the mobility measurements.
4.4 Correct Exercise Performance and Concordance of Physiotherapy and App Usage
In the short-term intervention patients we were able to perform the exercises almost flawlessly after three weeks of initial instruction. Only minor differences to the optimal exercise conduct were present, e.g. one patient did not bend the legs in a lying-down exercise, which did not affect the shoulder movement strongly.
In the mid-term intervention, all but one patient performed the exercises almost flawlessly. In four patients only minor differences to the optimal exercise conduct were present, but one patient made significant errors in the exercises. In the mid-term intervention we asked whether app instruction could replace the provided physiotherapy sessions. All patients answered that they did not believe that the app could have replaced the provided physiotherapy sessions. The exact results were on average 1 on a five-item Likert scale (1: strongly disagree to 5: strongly agree) for the statement: “I could have skipped the physiotherapy sessions because of the app.” The leading physiotherapist noted that “all patients liked the intervention”. He pointed out that the pain situation is a major factor and that especially one patient had severe pain over the Christmas weeks. At this time the patient was unhappy with the intervention, but when the pain was reduced and the patient had a much more positive outlook on the intervention. The physiotherapist’s main concern was the appropriate choice of exercises and how to adapt the exercises to the current state of patients. He noted that two patients were already too fit for the selected exercises. In the final interview of the mid-term intervention, all patients answered that they did not believe that the app could have replaced their regular physiotherapy sessions. The exact results were on average 1.5 on a five-item Likert scale (1: strongly disagree to 5: strongly agree) for the statement: “I could have skipped the physiotherapy sessions because of the app.” At the end of the final session, the physiotherapist stated that all patients were satisfied with the intervention and the exercises, but that it is a longer process to adjust the exercises, especially in the painful stages. The physiotherapist concluded that at the start of the intervention, more supervision for the exercises would be recommended. The physiotherapist added that the app was a useful support tool, especially after finishing the personal sessions with a physiotherapist.
4.5 Further Improvements and Pain Logging
In both interventions we asked for possible improvements of the app and the overall intervention. One patient noted that changes in the training regime (e.g., 2 times daily) are not well-reflected by the current app design (training can only be confirmed once per day). Another patient noted that checking off the exercises is only possible on the same day, but: “when I have forgotten to enter the performance of the exercises, I could not add them later”. Another patient remarked that the “timing [of the exercises] is not clear, is it exactly the same timing as I should perform the exercise, can I do it faster?”. This patient continued that “feedback on exercise correctness is missing \(\ldots \) I did perform the exercises too rigorously so pain followed in the night”. The feedback on correct exercise performance was mentioned by a second patient as well: “Feedback on exercise correctness would be nice in the app”. One patient stated that “the app could be used when explained by a physiotherapist or someone like a medical assistant, but not without explanation.” Another patient noted that “I am interested in the other different exercises [included the planning mode of the app]”. Another patient missed feedback in physiotherapy sessions on exercise performance (of the exercises presented in the app). Two patients stated that reminders in the app would be appreciated. One patient added that intelligent reminders coupled with geo-location would be a nice feature, such that one is reminded when arriving at home. The same patient also thought that gamification would be nice, with achievements and weekly goals.
One patient noted that a simple check-off of the entire exercises (all exercises and all sets) would be sufficient after a few times.
In both interventions, we asked specifically whether patients would like a module in the app to report pain. In the short-term intervention, three patients and one partner did not wish to document pain. Two patients wished to document pain, but did not have a proposal how they would like to do it. In the mid-term intervention, three patients found the idea to integrate a tool to log pain in the app interesting, two patients were strongly opposed. These patients argued that they did not want to be reminded of their pain at all, but tried hard to ignore it.
5 Discussion
A weakness of the study is the limited number of patients. However, the results are very similar for both the short-term and the mid-term intervention and thus the number of patients (overall 10) is believed to be sufficient to draw preliminary conclusions.
In both the short-term and the mid-term intervention, the scores in the standardized questionnaires were high, e.g. the SUS score was consistently in the range of 88 to 89, which indicates a very usable system [7]. The app was used almost daily in the 3-weeks and in the first 9 weeks (of the 18 weeks) by all patients and even when app usage became optional, the majority of patients continued to use the app almost daily. Therefore, the conclusion is that the app can successfully support physiotherapy for frozen shoulder patients in a mid-term time frame. 3D interaction and mulitmodal exercise instructions were appreciated.
During the mid-term intervention, patients noticed significantly more possible improvements for the app, e.g., with respect to different training regimes (twice daily) and the ability to check-off exercises in the following days.
The mobility measurements are of significant interest for physicians and shoulder surgeons, but are not well-accepted in its current implementation in the app by the patients. Most patients felt more comfortable if a physiotherapist conducted these measurements. Overall, one conclusion of the studies is that the consideration of the physiotherapists as users of the system needs to be more intensively researched, e.g. band with separate IMUs such as smart watches.
Most patients would also appreciate a joint usage with the physiotherapist, especially for the mobility measurements. Also, some patients would like to share their app usage data with the physiotherapist and believe that this sharing would increase their motivation.
An interesting question was whether patients would think that an app alone would suffice. Patients in the mid-term study firmly stated that the usage of the app without support from physiotherapy sessions would not be sufficient.
Overall, we believe that patients benefit from an app that supports home-based physiotherapy. However, in the further design the role of the physiotherapist as user of the system has to be carefully revisited in order to design a satisfying and usable system for all user groups. Also, the interaction with the physician in the long-term usage of the system needs to be clarified. If conservative treatment (physiotherapy and pain medication) fails, the physician has to decide if an operation is necessary. A well-documented course of the disease can greatly support the physician in the decision, i.e., the reliable and continuous mobility measurements and records of pain over the last years would be helpful.
6 Conclusion
Patients with frozen shoulder syndrome used an app to support their home-based physiotherapy in a short-term and a mid-term intervention. Both interventions showed that an app can sustainably support physiotherapy for the frozen shoulder syndrome as shown by the feasibility over a short-term and a mid-term period. Furthermore, the studies show that the ShoulderApp-based intervention was well accepted by the frozen-shoulder users over a short-term and a mid-term period. Patients would appreciate automatic feedback on their progress, but the usability of the automatic mobility measurement process has to be improved. The evaluation of novel hardware, such as smartwatches, is a promising new direction for that end. Most musculoskeletal disorders have similar characteristics and are treated with home-based physiotherapy as well. Therefore, we believe our results can be generalized for a large group of musculoskeletal disorders, which e.g. includes lower back pain and knee injuries. The analysis of the presented studies also showed the complexities which arise in the design of systems with multiple user-groups, in this case patients, physiotherapists and physicians. The role of the physiotherapists and physicians as co-users of the system has to be subject of further research. This work provides insights into their requirements, motivations, and needs. The inclusion of novel results from persuasive technology and habit formation is a promising line of research as well.
Overall, long-term and larger studies, such as RCTs (Randomized Controlled Trials) to research improvements on medical relevant outcomes, are warranted.
References
Aggarwal, D., Ploderer, B., Vetere, F., Bradford, M., Hoang, T.: Doctor, Can You See My Squats? In: Proceedings of the 2016 ACM Conference on Designing Interactive Systems - DIS 2016, pp. 1197–1208. ACM Press, New York (2016). https://doi.org/10.1145/2901790.2901871
op den Akker, H., Jones, V.M., Hermens, H.J.: Tailoring real-time physical activity coaching systems: a literature survey and model. User Model. User-Adap. Inter. 24(5), 351–392 (2014). https://doi.org/10.1007/s11257-014-9146-y
Ananthanarayan, S., Sheh, M., Chien, A., Profita, H., Siek, K.: Pt Viz. In: Proceedings of the conference on human factors in computing systems - CHI 2013, p. 1247 (2013). https://doi.org/10.1145/2470654.2466161
Anderson, F., Grossman, T., Matejka, J., Fitzmaurice, G.: YouMove. In: Proceedings of Symposium on User Interface Software and Technology - UIST 2013, pp. 311–320. ACM Press, New York (2013). https://doi.org/10.1145/2501988.2502045
Ayoade, M., Baillie, L.: A novel knee rehabilitation system for the home. In: Proceedings of the Conference on Human Factors in Computing Systems - CHI 2014, pp. 2521–2530. ACM Press, New York (2014). https://doi.org/10.1145/2556288.2557353
Balaam, M., et al.: Rehabilitation centred design. In: Proceedings of the Conference on Human Factors in Computing Systems, Extended Abstracts - CHI EA 2010, p. 4583. ACM Press, New York (2010). https://doi.org/10.1145/1753846.1754197
Bangor, A., Kortum, P.T., Miller, J.T.: An empirical evaluation of the system usability scale. Int. J. Hum.-Comput. Inter. 24(6), 574–594 (2008). https://doi.org/10.1080/10447310802205776
Bridgman, J.F.: Periarthritis of the shoulder and diabetes mellitus. Ann. Rheum. Dis. 31(1), 69–71 (1972)
Brooke, J.: Sus - a quick and dirty usability scale. In: Jordan, P.W., Thomas, B., Weerdmeester, B.A., McClelland, I. (eds.) Usability evaluation in industry, pp. 189–193. Taylor and Francis, London (1996)
Buttussi, F., Chittaro, L.: MOPET: a context-aware and user-adaptive wearable system for fitness training. Artif. Intell. Med. 42(2), 153–163 (2008). https://doi.org/10.1016/j.artmed.2007.11.004
Buttussi, F., Chittaro, L., Nadalutti, D.: Bringing mobile guides and fitness activities together. In: Proceedings of the Conference on Human-Computer Interaction with Mobile Devices and Services - MobileHCI 2006, p. 29. ACM Press, New York (2006). https://doi.org/10.1145/1152215.1152222
Chandra, H., Oakley, I., Silva, H.: Designing to support prescribed home exercises. In: Proceedings of the Nordic Conference on Human-Computer Interaction Making Sense Through Design - NordiCHI 2012, p. 607. ACM Press, New York (2012). https://doi.org/10.1145/2399016.2399108
Chandra, H., Oakley, I., Silva, H.: User needs in the performance of prescribed home exercise therapy. In: Proceedings of the Conference on Human Factors in Computing Systems, Extended Abstracts - CHI EA 2012, p. 2369. ACM Press, New York (2012). https://doi.org/10.1145/2212776.2223804
Cidota, M.A., Lukosch, S.G., Dezentje, P., Bank, P.J., Lukosch, H.K., Clifford, R.M.: Serious gaming in augmented reality using HMDs for assessment of upper extremity motor dysfunctions. i-com 15(2), 155–169 (2016). https://doi.org/10.1515/icom-2016-0020
Dennis, L., Brealey, S., Rangan, A., Rookmoneea, M., Watson, J.: Managing idiopathic frozen shoulder: a survey of health professionals’ current practice and research priorities. Shoulder Elbow 2(4), 294–300 (2010). https://doi.org/10.1111/j.1758-5740.2010.00073.x
Deutsch, J.E., Borbely, M., Filler, J., Huhn, K., Guarrera-Bowlby, P.: Use of a low-cost, commercially available gaming console (wii) for rehabilitation of an adolescent with cerebral palsy. Phys. Ther. 88(10), 1196–1207 (2008). https://doi.org/10.2522/ptj.20080062
Dezentje, P., Cidota, M.A., Clifford, R.M., Lukosch, S.G., Bank, P.J., Lukosch, H.K.: designing for engagement in augmented reality games to assess upper extremity motor dysfunctions. In: International Symposium on Mixed and Augmented Reality - Media, Art, Social Science, Humanities and Design - ISMAR MASH’D, pp. 57–58. IEEE, September 2015. https://doi.org/10.1109/ISMAR-MASHD.2015.24
Doyle, J., Bailey, C., Dromey, B., Scanaill, C.N.: BASE - an interactive technology solution to deliver balance and strength exercises to older adults. In: Proceedings of the 4th International ICST Conference on Pervasive Computing Technologies for Healthcare. IEEE (2010). https://doi.org/10.4108/ICST.PERVASIVEHEALTH2010.8881
Faber, M., Andersen, M.H., Sevel, C., Thorborg, K., Bandholm, T., Rathleff, M.: The majority are not performing home-exercises correctly two weeks after their initial instruction - an assessor-blinded study. PeerJ 3, e1102 (2015). https://doi.org/10.7717/peerj.1102
Fahrenberg, J., Myrtek, M. (eds.): Progress in Ambulatory Assessment - Computer-Assisted Psychological and Psychophysiological Methods in Monitoring and Field Studies. Hogrefe, Seattle (2001)
Fikar, P., Schönauer, C., Kaufmann, H.: The Sorcerer’s Apprentice: A serious game aiding rehabilitation in the context of Subacromial Impingement Syndrome. In: Proceedings of the ICTs for Improving Patients Rehabilitation Research Techniques, pp. 327–330. IEEE (2013). https://doi.org/10.4108/icst.pervasivehealth.2013.252224
Fogg, B.: A behavior model for persuasive design. In: Proceedings of the 4th International Conference on Persuasive Technology, Persuasive 2009, pp. 40:1–40:7. ACM, New York (2009). https://doi.org/10.1145/1541948.1541999
Gourlay, D., Lun, K.C., Lee, Y., Tay, J.: Virtual reality for relearning daily living skills. Int. J. Med. Inform. 60(3), 255–261 (2000). https://doi.org/10.1016/s1386-5056(00)00100-3
Huang, K., et al.: A technology probe of wearable in-home computer-assisted physical therapy. In: Proceedings of the Conference on Human Factors in Computing Systems - CHI 2014, pp. 2541–2550. ACM Press, New York (2014). https://doi.org/10.1145/2556288.2557416
Kelley, M.J., et al.: Shoulder pain and mobility deficits: adhesive capsulitis. J. Orthop. Sports Phys. Ther. 43(5), A1–A31 (2013). https://doi.org/10.2519/jospt.2013.0302
Keren, G.: Between- or Within-Subjects Design - A Methodological Dilemma, chap. 8, pp. 257–272. Psychology Press, New York (1993)
Liu, S.F., Lee, Y.L.: A simple and reliable health monitoring system for shoulder health: proposal. J. Med. Internet Res. 16(2), e11 (2014). https://doi.org/10.2196/resprot.2584
Liu, X., et al.: An interactive training system of motor learning by imitation and speech instructions for children with autism. In: Liu, H., Jo, K., Manic, M. (eds.) 9th International Conference on Human System Interactions (HSI), pp. 56–61. Institute of Electrical and Electronics Engineers (IEEE), Los Alamitos (2016). https://doi.org/10.1109/hsi.2016.7529609
May, M.A.: The psychology of learning from demonstration films. J. Educ. Psychol. 37(1), 1–12 (1946). https://doi.org/10.1037/h0058528
Micallef, N., Baillie, L., Uzor, S.: Time to exercise! In: Proceedings of the Conference on Human-computer Interaction with Mobile Devices and Services - MobileHCI 2016, pp. 112–123. ACM Press, New York (2016). https://doi.org/10.1145/2935334.2935338
Nixon, M.E., Howard, A.M., Chen, Y.P.: Quantitative evaluation of the Microsoft Kinect for use in an upper extremity virtual rehabilitation environment. In: 2013 International Conference on Virtual Rehabilitation (ICVR), pp. 222–228. IEEE, August 2013. https://doi.org/10.1109/ICVR.2013.6662131
Patton, M.Q.: Qualitative Research & Evaluation Methods - Integrating Theory and Practice, 4th edn. Sage, Thousand Oaks (2015)
Postolache, G., Girao, P.S., Postolache, O.: Applying smartphone apps to drive greater patient engagement in personalized physiotherapy. In: 2014 IEEE International Symposium on Medical Measurements and Applications (MeMeA), pp. 1–6. IEEE, June 2014. https://doi.org/10.1109/MeMeA.2014.6860094
dos Santos Mendes, F.A., et al.: Motor learning, retention and transfer after virtual-reality-based training in parkinson’s disease - effect of motor and cognitive demands of games: a longitudinal, controlled clinical study. Physiotherapy 98(3), 217–223 (2012). https://doi.org/10.1016/j.physio.2012.06.001
Schönauer, C., Fukushi, K., Olwal, A., Kaufmann, H., Raskar, R.: Multimodal motion guidance. In: Proceedings of the International Conference on Multimodal Interaction - ICMI 2012, p. 133. ACM Press, New York (2012). https://doi.org/10.1145/2388676.2388706
Sluijs, E.M., Kok, G.J., van der Zee, J.: Correlates of exercise compliance in physical therapy. Phys. Ther. 73(11), 771–782 (1993)
Smeddinck, J.D., Herrlich, M., Malaka, R.: Exergames for Physiotherapy and Rehabilitation. In: Proceedings of the Conference on Human Factors in Computing Systems - CHI 2015, pp. 4143–4146. ACM Press, New York (2015). https://doi.org/10.1145/2702123.2702598
Szajna, B.: Empirical evaluation of the revised technology acceptance model. Manag. Sci. 42(1), 85–92 (1996). https://doi.org/10.1287/mnsc.42.1.85
Tang, R., Alizadeh, H., Tang, A., Bateman, S., Jorge, J.A.: Physio@Home: exploring visual guidance and feedback techniques for physiotherapy exercises. In: Proceedings of the Conference on Human Factors in Computing Systems, Extended Abstracts - CHI EA 2014, pp. 1651–1656 (2014). https://doi.org/10.1145/2559206.2581197
Tang, R., Bateman, S., Yang, X.D., Jorge, J., Tang, A.: Physio @ Home : Exploring Visual Guidance and Feedback Techniques for Physiotherapy Exercises. In: Proceedings of the Conference on Human Factors in Computing Systems - CHI 2015, pp. 4123–4132. ACM Press, New York (2015). https://doi.org/10.1145/2702123.2702401
Venkatesh, V., Davis, F.D.: A theoretical extension of the technology acceptance model: four longitudinal field studies. Manag. Sci. 46(2), 186–204 (2000). https://doi.org/10.1287/mnsc.46.2.186.11926
Vorrink, S.N., Kort, H.S., Troosters, T., Lammers, J.W.J.: A mobile phone app to stimulate daily physical activity in patients with chronic obstructive pulmonary disease: development, feasibility, and pilot studies. JMIR mHealth uHealth 4(1), e11 (2016). https://doi.org/10.2196/mhealth.4741
Yim, J., Graham, T.C.N.: Using games to increase exercise motivation. In: Kapralos, B., Katchabaw, M., Rajnovich, J. (eds.) Proceedings of the 2007 Conference on Future Play, pp. 166–173. ACM, New York (2007). https://doi.org/10.1145/1328202.1328232
Zhao, W., Feng, H., Lun, R., Espy, D.D., Reinthal, M.A.: A kinect-based rehabilitation exercise monitoring and guidance system. In: 5th International Conference on Software Engineering and Service Science, pp. 762–765. IEEE, Los Alamitos, June 2014. https://doi.org/10.1109/icsess.2014.6933678
Acknowledgments
Thomas Stütz was responsible for writing the paper; he was the project leader and responsible for the conduct of the studies. He implemented prototypes of the app. Gerlinde Emsenhuber implemented the final version of the app. Nicholas Matis (shoulder surgeon) provided the medical background for the app, the studies, and was responsible for patient acquisition. He also provided the initial idea for an app for Frozen Shoulder patients. Daniela Huber and Felix Hofmann (physiotherapists) lead the team of physiotherapists. Daniela Huber co-designed the studies. Michael Domhardt performed the analysis of the log files of the first study (not part of this paper) and reviewed the study design of the mid-term study.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 IFIP International Federation for Information Processing
About this paper
Cite this paper
Stütz, T. (2019). (How) Can an App Support Physiotherapy for Frozen Shoulder Patients?. In: Lamas, D., Loizides, F., Nacke, L., Petrie, H., Winckler, M., Zaphiris, P. (eds) Human-Computer Interaction – INTERACT 2019. INTERACT 2019. Lecture Notes in Computer Science(), vol 11746. Springer, Cham. https://doi.org/10.1007/978-3-030-29381-9_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-29381-9_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-29380-2
Online ISBN: 978-3-030-29381-9
eBook Packages: Computer ScienceComputer Science (R0)