Abstract
The high suicide rate among doctors is a significant issue in many countries, especially among female doctors, for whom the rate is more than two times that of the general population. Compared to many countries, Taiwan has a much lower proportion of female physicians relative to male physicians, which has been suggested as a negative factor in affecting the suicide rate. Previous studies of female physician stressors are few and focus mainly on occupational stress. Nonwork stress has not been well-researched. This study aims to explore the feasibility of providing a comprehensive evaluation of all stressors in female doctors’ daily lives by examining a cohort of Taiwanese female doctors. Maslach burnout inventory (MBI) and the Brief Symptom Rating Scale (BSRS-5) are used to screen participants for occupational stress and depressive attributes respectively. In this study, an interview is conducted with a participant, and factors contributing to lifestyle and occupational stress are identified. The study results indicate that family issues, primarily child-rearing, acts as the largest stressor in the participant’s life, outweighing even traditionally studied occupational stressors for female physicians.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Studies show that physicians have a higher risk of suicide, which is about 1 to 3 times for male physicians and 2 to 6 times for female physicians when compared to the normal population [1]. There is only few research about suicide in Taiwan, one study shows the risk is 2 times for physicians aged 25–44 years compared with the general population [2]. From previous research, we found that the most important evidence-based risk factors for suicide are psychiatric disorders (mostly depression and schizophrenia), past or recent social stressors, suicide in the family or among friends or peers, low access to psychological help, and access to methods for committing suicide [3]. Several studies have emphasized the importance of depression on suicide risk, particularly for female physicians [4, 5]. In a study of more than 1300 male medical graduates from Johns Hopkins University, the lifetime prevalence of depression was found to be 12.00% [6]. An analogous study of 4500 female physician manifests the prevalence is 19.50% [4]. The above statistics imply the gender difference regarding the issue of physicians’ stress. Although the etiologies of depression haven’t totally been understood yet, stress has been found to be an impactful factor on depression which changes many mechanisms in the human body [7].
One might expect physicians to have excellent access to mental healthcare services and medication. However, postmortem toxicology testing of physicians who committed suicide shows low rates of antidepressant use. They are more likely to use self-prescribed medication like antipsychotics, benzodiazepines and barbiturates. Inadequate medical treatment and increased problems related to job stress are potentially modifiable risk factors that can reduce suicidal death among physicians [8]. Nevertheless, there are barriers which prevent physicians from seeking help, including confidentiality, discrimination in medical licensing, hospital privileges, concerns about the impact on professional advancement, and the risk of being stigmatized [5, 9].
Numerous studies describe occupational stress as one of the foremost causes of physician mental illness and depress [10,11,12]. Imbalance among job, family, and personal growth is mentioned but few studies have been done to understand physicians’ nonwork stress. Existing studies also tend to focus on male physicians, who have traditionally been much more prevalent in the healthcare system. Social and occupational roles for male and female physicians can be very different. There are also significant differences between male and female physicians in the statistics of suicide and depression prevalence. These factors, in addition to the dearth of previous research on female physicians, lead us to specifically study both occupational and nonwork stress of female physicians.
We first discuss occupational stress. Although physicians with different genders have similar missions in their jobs, careers and opportunity structures, power, benefits, and occupational networks can be significantly different, so gender differences in physician stress are expected. Due to female physicians’ minority status/prejudice, they may experience a lack of role models/mentors/sponsors and role strain. Sixty-sixpercent of female physicians indicated at least one very difficult period in their lives [13]. According to OECD Health Statistics in 2016 [14], only 21.02% of doctors are women in Japan. Most countries have a proportion of female physicians that is less than half. In Taiwan, the proportion of female positions is much less, only 19.80% in 2018 [15]. The differences diminished when the members of minority become more, so we can guess the problem is more serious in Taiwan. Ann et al. [16] identified that work stressors may increase the risk of suicide for female physicians. Taiwan has a much lower proportion of female physicians relative to male physicians, which has been suggested as a negative factor in affecting the suicide rate. Previous studies of female physician stressors are few and focus mainly on occupational stress.
There are significant gender-related differences in nonwork stressors as well. Grace et al. [17] mentioned that among women, family role stressors are more strongly correlated to mental illness, especially depression, when compared to work-related stressors. For men, work-related stressors have a more significant impact on mental health than family role stressors, indicating that overall, women are more vulnerable to the negativity of family stress. Studies [17] also found that women show a higher level of depression than men due to marital dissatisfaction. Also, women’s primary responsibility for the wellbeing of others, especially children, causes poorer mental health of women [17]. The multitude of roles that women must fulfil has traditionally also been a source of stress for women. The environment of high demands and low control by the mother, in contrast to one of the low demands and high control by the father, is one of the reasons that women can be more stressed than men [18]. Therefore, to research female physicians’ stressors, nonwork stressors cannot be ignored.
Previous studies about female physicians are few and mainly focus on clinical job settings. However, female physicians face more challenges than male physicians regarding work-family balance [19]. This research aims to understand the stressors thoroughly in female physicians’ daily lives, including occupational stressors, nonwork stressors, stress relievers, and the interrelation between all of them. By understanding the stressors in the whole picture, we can prevent physician suicide in the very early beginning.
2 Materials and Method
There are three steps in our research method. First, we screened participants via a questionnaire. Second, Day Reconstruction Method (DRM) [20] was used, followed by interviewing participants. Finally, we conducted qualitative analysis by ATLAS.ti CLOUD [21] to code the interview data [22].
In the questionnaire, several types of demographic data of female physicians were collected, including residency, age, salary, department, working hours, working organization, working years, and family members, etc. The questionnaire was only open to licensed female physicians from Taiwan, who were trained in western medicine, thus excluding interns, eastern medicine doctors, and dentists. The Chinese version of the Brief Symptom Rating Scale (BSRS-5) [23, 24] and Maslach burnout inventory (MBI) [25] were used to evaluate physicians’ general mental health and occupational stress.
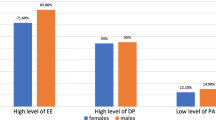
BSRS-5 is designed to capture general mental health status in order to prevent suicide. Based on the results of a study that shows the high overlap between burnout and depression [26], we chose MBI to record participants’ occupational stress. MBI measures three dimensions of burnout: emotional exhaustion, depersonalization, and personal accomplishment. High scores indicate a greater extent in each dimension, greater burnout in emotional exhaustion and depersonalization, and less burnout in personal accomplishment. For this case study, we selected one physician to be interviewed based on the results of a screening questionnaire.
In the second step, we conducted Daily Reconstruction Method by sending out a format of multiple diary tables, in which participants jot down, for one week, every event and the concurrent emotion and stress level. The interview will be conducted based on those events, and the diary table will be reviewed by participants as a reference. Participants can choose to keep the diary for privacy or have it returned to researchers. The set of interview questions is as follows:
-
Please describe your life this week.
-
Why do you have that emotion in this event?
-
What’s the main stressor in your life?
-
What do you like to do to relieve yourself of stress?
-
If you had the ability to change anything in your current life, what would you change?
The interview was also voice recorded. We typed the whole conversation word for word after the interview.
In the third step, we do qualitative analysis by coding to indexing what the participants said in order to establish a framework for this female physician’s stressors.
3 Result
The participant is an attending physician working in a physical medicine and rehabilitation clinic for about 25 h per week. She lives with her physician husband and her 4 years and 8 months old child. More demographic details are shown in Table 1. Her results on the Brief Symptom Rating Scale and Maslach burnout inventory are as Table 2.
Overall, the participant emphasized that children are the main stressor in her current life as an attending physician. She spent more than half of the interview duration speaking about things related to her children.
“Most of my stressors come from children.”
“I like to have shifts because it’s possible to have overnight sleep, which is impossible when I stay home because I have to wake up at night and breastfeed my baby.”
“The most frustrating thing that happened last week is that my child cheated, which conflicts my upbringing principle.”
“I feel that I was being misunderstood when my brother suggested another way to educate my child.”
When asked about the childcare related issues shared by the physician couple, the participant professed to take more responsibilities for their children.
“I have to wake up once every night for breastfeeding. My husband has tried that before, but he needs much sleep and can’t wake up. I’ve tried to wake my husband up, but he is too slow and the child burst into tears. It’s better and more efficient that I do it alone.”
“Children wake up early and my husband cannot, so I have to wake up even when I’ve been interrupt when sleeping for breastfeeding.”
“When the baby was sick and couldn’t breathe smoothly, I’m afraid that the sputum blocked his airway so I would wake up to check my baby if his breathing sound was abnormal. My husband sleeps very deeply so I’m the one who wakes up.”
As shown in the MBI score (Table 3), the participant scores high in personal achievement, which agrees with the interview results. She is in general satisfied with her current job. She only feels frustrated when her patients’ treatment didn’t meet expectation.
“If I can find what I want to learn in my job and apply it, I’ll be happy, and this is what I like to do. I would feel satisfied if my current job continues, because it’s hard to find a boss who has the same values as you and is willing to support you. Many bosses here don’t want to buy an ultrasound, but my boss did. Ultrasound is my key technique, so I can do what I want to do here.”
“There was a patient on Friday who complained and questioned my decision. I had explained things before treatment, but she still felt the result didn’t meet her need. It’s hard to communicate.”
When asked what most stressful aspects of being a doctor are, she mentioned two of her biggest stressors: night shifts in internal medicine department during postgraduate year-1(PGY), and having a child in residency.
“The most unforgettable stressors in my life would be two things; one is the night shifts in the internal medicine department in PGY. It was very terrible… because I was the front-line resident. The biggest stressor is the fear of being sued. Senior residents were often doing CPR in intensive care centre, so the backup support is not enough. I was very afraid of malpractice and being sued.”
“Another one is having children in residency. There are so many things that have to be done as a resident. If your child has issues that you need to spend additional time on, such as refusing to go to bed on time or getting sick. You don’t know when you can start your own work, which makes me anxious. That’s so terrible”
According to the interview, her medical career thus far can be divided into three periods: PGY, residency, and attending physician. Her occupational stress went down after being an attending physician. However, her primary source of nonwork stress, her children, has remained a constant source of stress. (Figure 1) The stress in residency comes not only from the responsibilities of childcare but also from her job, so the occupational and nonwork stress are both high in her residency.
“When you are a resident, you need to react based on the head of the department. At times, he would say something threatening. For example, he would say‘when I was a resident, a young couple wouldn’t dare become pregnant during residency. You may need to stay one more year if you delay too much.’”
“I was lucky because senior residents in my department supported me a lot. They were really kind and didn’t badmouth me. I would do things they didn’t want to do like paperwork as a return.”
The Participant’s values and personality are also shown in the interview.
“My principle is seeking the truth from facts. When my son has questions, I’ll try my best to answer him right. I won’t say it’s ok if we don’t know the answer. Instead, I’ll say let’s try to find out the answer together.”
“When there are patients that could be treated by new skills therapists don’t want to learn, I feel this attitude conflicts with my principles, seeking the truth from facts. Why don’t we do it if it’s doable with more effort?”
“By my educational values, girls are the same as boys. I would not educate my children differently based on their gender.”
For stress relief, the participant likes to read books about patient treatment or upbringing in her free time. She also mentioned that she feels happy sometimes when she can leave children for a while, such as when she has shifts, which means her husband will take care of the children. Also, the support from senior residents helped release her stress in residency.
Figure 2 shows the relationship between stress and stressors for this participant. During her medical career, the occupational stressors are incongruent of treatment expectation between her and the patients, the lack of skill in clinical practice, lack of support for clinical work, and lack of support when pregnant; the nonwork stressor are children related issues, including her children’s education, health, concern for other issues, such as when her children are negatively affecting others.
Her primary forms of occupational stress relief come from the support of her colleagues and from breaks from the working space. Her relief from nonwork, mostly childcare stress, comes from the support of her husband, and from opportunities to take temporary breaks from taking care of her children. Other forms of stress relief, such as her hobby, reading the books on medical treatment and education, relieve both of her occupational and nonwork stress. The participant also mentioned that nonwork stress affected her job more than occupational stress affected her family.
4 Discussion
In this case study, we found that nonwork stress from the participant’s children is the main stressor in her current life, and that although job stress appears sometimes, her job satisfaction is high. This finding is consistent with Gail et al.’s review [19] that although female physicians face multiple stressors, they are generally satisfied with their careers. Barnett [18] also found that being a mother, especially of pre-school-aged or multiple children, has a more negative effect on the overall wellbeing of a woman, when compared to working and marriage. The participant loves her children and misses her children when working. However, she also feels happy when she can transfer the responsibility of children to her husband. Other research has also shown that both employment and career advancement are correlated with positives outcomes in women’s health [18]. From our study, the amount of time for our female physician participant to pursue her own goal is important to relieve her nonwork stress. The goal is from two roles, as a physician, and as a mother. The participant takes more responsibilities for childcare than her husband does. This stressor can be relieved with support from others and from the enjoyment of her own hobbies. Thus the support of the husband in child-rearing is highly important for the mental health of employed women [27]. For mothers, learning to manage one’s expectations for children and expressing these feelings in a healthy and productive way can also lower childcare related stress.
Lack of support in clinical practice is the participant’s main occupational stressor. The types of support she seeks can be categorized as support for pregnancy-related needs and support for her clinical work. Marjorie et al. mentioned that minority status/prejudice/discrimination is one stressor of female physicians [13]. With more and more female physicians nowadays, some parts of the situation have gradually improved. The participants’ male doctor coworkers helped her during her pregnancy because they also have physician wives and can be more empathetic. However, the head of the department who judged her based on his own cultural values for residency caused pressure on her. Such instances of cultural friction between superiors and employees have gradually lessened, also resulting in a working environment that is friendlier than before for female physicians. A previous study shows that meetings to discuss stressful situations at work appear to offer a protective factor for physicians in different residencies, and thus should be implemented as a regular event in healthcare institutions [16].
Previous studies about physician suicide show certain personality traits in physicians, i.e. perfectionism, workaholic, and type A personality, are associated with mental illness. When these traits show up with long work hours and unsmooth family relationships, physicians may be more vulnerable to life stress than people in the same situation but without the traits [28, 29]. Additionally, type A behaviour is more prevalent in women than in men [30]. The participant tends to do her best in jobs and childcare, but her working hours are short and family relationship is smooth. For further suicide prevention studies, understanding the relationship between personality, working hours, and family relationships are suggested. Also, the upper limit of working hours in physicians should be strictly applied by institutions for both patients’ and physicians’ safety.
5 Conclusion
To improve the suicide issue for physicians, female physicians should be discussed separately from male physicians due to differences in the family and professionally in the healthcare system. In the professional setting, female physicians are a minority group and thus also face unique workplace issues related to this. The Taiwanese healthcare system is a useful setting for this investigation, particularly because it has a much smaller proportion of female physicians when compared to other countries. From this case study, the occupational stressors are lack of support for clinical work, lack support for pregnancy-related issues, and the incongruent treatment expectations between doctor and patient. The nonwork stressor, which is this female attending physician’s current main stressor, mainly come from her child-rearing responsibilities. Both occupational and nonwork stressors can be relieved by support from others and by the enjoyment of her own hobbies. Other suggestions for stress relief are provided based on previous studies. Further research with more participants is needed to get a comprehensive picture of female physicians’ stress model.
References
Schernhammer, E.S., Colditz, G.A.: Suicide rates among physicians: a quantitative and gender assessment (meta-analysis). Am. J. Psychiatry 161, 2295–2302 (2004)
Chen, I.M., Liao, S.C., Lee, M.B.: Physician suicide in Taiwan: a nationwide retrospective study from 2000–2013. Aust. J. Psychiatry Behav. Sci. 1, 1008 (2014)
World Health Organization: Prevention of mental disorders: effective interventions and policy options. World Health Organization (2004)
Frank, E., Dingle, A.D.: Self-reported depression and suicide attempts among U.S. women physicians. Am. J. Psychiatry 156, 1887–1894 (1999)
Center, C., et al.: Confronting depression and suicide in physicians: a consensus statement. JAMA 289, 3161–3166 (2003)
Ford, D.E., Mead, L.A., Chang, P.P., Cooper-Patrick, L., Wang, N., Klag, M.J.: Depression is a risk factor for coronary artery disease in men: The precursors study. Arch. Int. Med. 158, 1422–1426 (1998)
Yang, L., Zhao, Y., Wang, Y., Liu, L., Zhang, X., Li, B., Cui, R.: The effects of psychological stress on depression. Curr. Neuropharmacol. 13, 494–504 (2015)
Gold, K.J., Sen, A., Schwenk, T.L.: Details on suicide among US physicians: data from the national violent death reporting system. Gen. Hosp. Psychiatry 35, 45–49 (2013)
Schwenk, T.L., Gorenflo, D.W., Leja, L.M.: A survey on the impact of being depressed on the professional status and mental health care of physicians. J. Clin. Psychiatry 69, 617–620 (2008)
Wang, L.-J., Chen, C.-K., Hsu, S.-C., Lee, S.-Y., Wang, C.-S., Yeh, W.-Y.: Active job, healthy job? Occupational stress and depression among hospital physicians in Taiwan. Ind. Health 49, 173–184 (2011)
May, H.J., Revicki, D.A., Jones, J.G.: Professional stress and the practicing family physician. South. Med. J. 76, 1273–1276 (1983)
Balch, C.M., Freischlag, J.A., Shanafelt, T.D.: Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch. Surg. 144, 371–376 (2009)
Bowman, M.A., Allen, D.I.: Female physician stress. In: Bowman, M.A., Allen, D.I. (eds.) Stress and Women Physicians, pp. 129–141. Springer, New York (1990). https://doi.org/10.1007/978-1-4684-0267-4_9
OECD: Health Care Resources: physicians by age and gender. OECD (2016)
The Gender Equality Committee: Gender statistics of various medical personnel in Taiwan. Ministry of Health and Welfare, Taipei (2019)
Fridner, A., Belkic, K., Marini, M., Minucci, D., Pavan, L., Schenck-Gustafsson, K.: Survey on recent suicidal ideation among female university hospital physicians in Sweden and Italy (the HOUPE study): cross-sectional associations with work stressors. Gend. Med. 6, 314–328 (2009)
Baruch, G.K., Biener, L., Barnett, R.C.: Women and gender in research on work and family stress. Am. Psychol. 42, 130 (1987)
Barnett, R.C., Biener, L., Baruch, G.K.: Gender and Stress. Free Press, New York (1987)
Robinson, G.E.: Stresses on women physicians: consequences and coping techniques. Depress. Anxiety 17, 180–189 (2003)
Kahneman, D., Krueger, A.B., Schkade, D.A., Schwarz, N., Stone, A.A.: A survey method for characterizing daily life experience: the day reconstruction method. Science 306, 1776–1780 (2004)
ATLAS.ti Scientific Software Development GmbH: ATLAS.ti CLOUD. vol. BETA. ATLAS.ti Scientific Software Development GmbH (2018)
Hwang, S.: Utilizing qualitative data analysis software: a review of Atlas.ti. Soc. Sci. Comput. Rev. 26, 519–527 (2008)
Lee, M.-B., et al.: Development and verification of validity and reliability of a short screening instrument to identify psychiatric morbidity. J. Formos. Med. Assoc. 102, 687–694 (2003)
Lu, I.C., Yen Jean, M.-C., Lei, S.-M., Cheng, H.-H., Wang, J.-D.: BSRS-5 (5-item Brief Symptom Rating Scale) scores affect every aspect of quality of life measured by WHOQOL-BREF in healthy workers. Q. Life Res. 20, 1469–1475 (2011)
Maslach, C., Jackson, S.E., Leiter, M.P., Schaufeli, W.B., Schwab, R.L.: Maslach Burnout Inventory. Consulting Psychologists Press, Palo Alto (1986)
Bianchi, R., Schonfeld, I.S., Laurent, E.: Burnout–depression overlap: a review. Clin. Psychol. Rev. 36, 28–41 (2015)
Belle, D.: Gender differences in the social moderators of stress. In: Monat, A., Lazarus, R.S. (eds.) Stress and Coping: An Anthology, pp. 257–277. Columbia University Press, New York (1991)
Wallace, J.E., Lemaire, J.B., Ghali, W.A.: Physician wellness: a missing quality indicator. Lancet 374, 1714–1721 (2009)
Gunter, T.: Physician death by suicide: problems seeking stakeholder solutions (2016)
Sorensen, G., Jacobs, D.R., Pirie, P., Folsom, A., Luepker, R., Gillum, R.: Relationships among type a behavior, employment experiences, and gender: The Minnesota heart survey. J. Behav. Med. 10, 323–336 (1987)
Acknowledgments
This work was supported in part by the Ministry of Science and Technology of Taiwan, ROC under Contracts MOST 106-2628-H-182-002-MY3 and MOST 108-2622-8-003-001-TM1. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this paper
Cite this paper
Cheng, KT., Tseng, K.C. (2019). Occupational and Nonwork Stressors Among Female Physicians in Taiwan: A Single Case Study. In: Antona, M., Stephanidis, C. (eds) Universal Access in Human-Computer Interaction. Multimodality and Assistive Environments. HCII 2019. Lecture Notes in Computer Science(), vol 11573. Springer, Cham. https://doi.org/10.1007/978-3-030-23563-5_35
Download citation
DOI: https://doi.org/10.1007/978-3-030-23563-5_35
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-23562-8
Online ISBN: 978-3-030-23563-5
eBook Packages: Computer ScienceComputer Science (R0)