Abstract
Determining the asthma health status of a person is a relevant task in the application of context-awareness and case-based reasoning for asthma management. As there are no devices that can track the asthma health status of a person constantly, it is necessary to use a Human-in-The-Loop (HiTL) approach for creating a solution able to associate their health status with context-related data. This research work proposes a system that implements the Asthma Control Questionnaire (ACQ) for determining the asthma health status of a person. The system links this health status to context-related data the person is exposed, and creates the cases to be used by the CBR component of the system. The system is then evaluated by users from a usability perspective through the Health IT Usability Evaluation Model (Health-ITUEM).
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
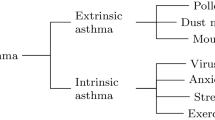
People with asthma suffer from an airway inflammation causing expiratory airflow limitation and respiratory symptoms such as wheeze, shortness of breath, chest tightness and cough that vary over time and intensity [5]. There is no cure for asthma but it can be treated based on a self-management approach [4, 31, 32]. Context-awareness (C-AR) can support the personalisation of asthma management plans, which is required to address the high heterogeneity level of asthma that makes people to have different triggers and symptoms [29, 30].
Context can be defined as “the information which is directly relevant to characterise a situation of interest to the stakeholders of a system". C-AR is then defined as “the ability of a system to use contextual information in order to tailor its services so that they are more useful to the stakeholders because they directly relate to their preferences and needs". Unlike Dey’s definitions of context and C-AR [2, 16] that go from the system to the user, these are more linked to a person-centric approach that goes from the user to the system.
Case-based reasoning (CBR) is a branch of artificial intelligence [1] that has already been applied in health sciences showing promising results [10, 12]. CBR replicates “the use of old experiences to understand and solve new problems" [23]. It has been shown that CBR can be used together with C-AR to solve problems involving multidimensional context-related data [22]. Moreover, CBR is able to support the personalisation of local/personal restrictions by adapting medical knowledge and reasoning strategies based on contextual information [24].
Asthma can benefit from the synergy between CBR and C-AR because its heterogeneity requires patients to adapt their lifestyle to the constraints defining their asthma. They need to discover the triggers provoking their exacerbations and the symptoms shown when it occurs. They also need to adapt their management plans because the characteristics of their condition may change over time, or they may be exposed to environments with triggers they have not experienced before. Nevertheless, there are challenges to tackle before being able to exploit the synergy between CBR and C-AR for personalised asthma management.
This research work addresses an issue of using CBR/C-AR for asthma, which is how to determine the asthma health status of a person. This is important because the health status is highly relevant to define the context of a person with asthma and to complete the CBR cycle aiding their asthma management process. As there are no devices able to monitor the health status of a person constantly [30], a Human-in-The-Loop (HiTL) approach shall be used to create a solution able to determine and store the asthma health status of a person.
The main contribution of the research is a solution allowing people to determine their asthma health status through a system implementing the Asthma Control Questionnaire (ACQ) [18,19,20,21]. It is a mobile application using the ACQ to complete and store context-related data in form of cases to be used by the CBR component of the system. The design of the mobile application as a system showing explicit information [28] is described and then evaluated from a usability perspective.
The paper is divided as follows. Section 2 presents the state-of-the-art on the subject, Sect. 3 describes the methodology used in the research, Sect. 4 explains the benefits of using CBR and C-AR together for asthma management, and the challenge of determining the health status of a person. Then, the system to determine the health status and its validation are described in Sect. 5. The discussion of the outcomes and conclusions are presented in Sects. 6 and 7.
2 State-of-the-Art
C-AR is important for pervasive/ubiquitous computing [7, 27] as it aids to personalising services based on contextual and situational information [3, 9]. C-AR as part of Intelligent Environments has been applied to Transportation, Education, Production places, Smart offices, Intelligent supermarkets, Energy conservation, Entertainment, and Health [7]. In the health area, C-AR can aid people suffering from chronic conditions requiring lifestyle management [17]. C-AR solutions have been developed to support people suffering from high blood pressure [33], diabetes [14], cardiovascular conditions [15], among others.
A survey on C-AR for asthma condition management shows a lack of solutions allowing the personalisation of management plans [30]. This is important to highlight because personalisation is the key to implement effective asthma management plans given the high heterogeneity of the condition [31, 32]. An approach to develop C-AR solutions allowing personalised asthma management is proposed as an attempt to close this gap [29]. It proposes to use three types of indicators in order to facilitate the description of patients’ contexts and provide a more comprehensive support for complex decision-making processes like CBR.
CBR solves a new problem by reusing knowledge from previously solved problems that are similar to the new one [1]. This problem-solving paradigm can handle issues related to health sciences better than other techniques [11, 12] and has already been used in several tasks including treatment planning, knowledge acquisition/management, among others [10]. CBR can be used together with C-AR in order to solve problems that are not completely understood, like adapting to evolving context adaptation [22] and personal constraints [24]. An example of the benefits from using CBR and C-AR together is shown in [26].
Monitoring the asthma health status of a person is an issue to tackle for allowing the application of CBR/C-AR in asthma management. This is challenging as there are no devices that can monitor the asthma health status of a person constantly [30]. Addressing this issue is important because it is needed to associate the context the person is exposed to their health status. Otherwise, it will not be possible to know whether a situation is dangerous or not, nor to determine what situations led to a health deterioration in the past for using them in the prediction of current and future risky situations.
This research work proposes to use a HiTL approach for implementing a C-AR system that determines the asthma health status of a person, relates it with the context the person is exposed, and creates/stores cases that can be used to apply CBR in asthma management. The system is a mHealth application whose HCI components gathering the asthma health status of a person is built based on the ACQ [18]. The HiTL approach takes human interaction into consideration, and makes humans a key part of the system [25].
3 Methodology
The research is led by the User-Centric Intelligent Environment Development Process, whose aim is to ensure the acceptance of technology by involving stakeholders in all the stages. It has been used to develop technology helping people with special needs [6, 8]. Figure 1 summarises the methodology process.
The 1. Literature review showed a lack of C-AR solutions supporting personalised asthma management. Then, 2. Interviews were held for having a better understanding about the necessities of people affected by asthma. From the outcomes of steps 1 and 2, an initial approach to develop C-AR solutions supporting personalised asthma management was proposed [29], and a questionnaire for defining more specific C-AR features of solutions supporting asthma management was developed. A partnership with Asthma UK [5] was formed, and they helped to spread the questionnaire among their representative sample of volunteers including patients and carers, gathering 42 responses.
A prototype was then developed considering the approach proposed in step 3 and the results of step 4. It includes an Asthma Control Assessment Component that aids to determining the asthma health status of a person. This component was evaluated by 5 people with asthma and 4 carers of people with asthma that interacted with the prototype. They were asked to answer a questionnaire based on the Health IT Usability Evaluation Model (Health-ITUEM) [13].
This research work mainly reports on steps 5 and 6 of the methodology described above. However, it also shows the results of the HCI-related questions that were included in the questionnaire spread in step 4 (Sect. 3.1).
3.1 Results of the Questionnaire Spread by Asthma UK
This section shows the results of the HCI-related questions that were included in the questionnaire spread by Asthma UK. Figures 2 and 3 show the assessment done by the respondents to some C-AR features of solutions supporting asthma management. Most of them assessed the features with 4 and 5: providing instructions in case of emergency (71.4%), showing a map highlighting near emergency centres (71.4%), reminding users about their medication intake (64.3%), and notifying patients’ next of kin in case of emergency (69.0%). They were also asked to suggest other features, pointing out the following keywords covering their suggestions: asthma plan management (6 related-responses), medication management (5), notifying others when there is an emergency (2), nutrition management (1), and notifying when there is good weather (1).
Figure 4 summarises the stakeholders the respondents would like to contact in case of emergency, and how they would like to contact them. The axis No in Fig. 4 shows how many respondents do not want to contact each of the stakeholders listed. It suggests that the person to contact should be personalised depending on the scenario of the person with asthma. This statement is supported by respondents recommending different stakeholders to be notified when they were asked to suggest stakeholders that were not part of the response options. Among others, they suggested to notify the emergency department, general practitioners, doctors, work colleagues, and siblings, depending on their circumstances.
Figure 4 shows the preferred ways to contact the stakeholders in case of emergency. Showing a notification (alert) on the stakeholder’s smartphone (47) is more preferred way to contact over using SMS (40), other messaging service (32) - like WhatsApp, Facebook Messenger, or Telegram, or other ways to contact them (8). The respondents could choose choosing more than one way of contacting each stakeholder. This means that a respondent could have chosen to contact their parents using a notification, SMS and Other MS all together.
Respondents were also asked about the information that should be send in case of emergency. 88.0% of them consider that the details of the emergency and the location of the person having the emergency are important information to send to the stakeholders when an emergency situation occurs. 66.67% of them consider that contact details is another important information to send. Finally, one person recommended to send Information about allergies.
4 CBR for Personalised Asthma Management
Figure 5 describes the CBR cycle for personalised asthma management, which has been adapted from the CBR cycle proposed by Aamodt and Plaza [1]. A New problem is a new case (\(C_x\)) to be analysed, which includes the context to which the person with asthma is or has been exposed. This context is made of the patient’s, indoor and outdoor environmental indicators [29]. \(C_x\) goes then to the retrieval stage, which is the first stage of CBR whose aim is finding the most similar case to \(C_x\) (\(C_s\)) that is stored in the database of previous cases.
\(C_s\) is the basis of the reuse stage that attempts predicting the possible outcome of \(C_x\), considering the real outcome of \(C_s\). The predicted and real outcome of a case is the predicted and real health status of the person with asthma when they are exposed to the context represented by that case. The health status is normal when the context does not affect them, and deterioration when the context negatively affects them. The predicted health status is defined in the reuse stage of the CBR, and the real health status is defined later in the revise stage by assessing the health status of the person with asthma.
The final stage is the retain stage in which the completely defined \(C_x\) - that is represented by
 - is stored in the database of previous cases to be used in the future to assess other cases. Hence, CBR predicts the health status of a person that is exposed to a specific context by using the real health status the person experienced when they were exposed to a similar context in the past. Then, CBR confirms the real health status of the person for knowing the accuracy of its prediction and storing the new case to be used in future predictions.
- is stored in the database of previous cases to be used in the future to assess other cases. Hence, CBR predicts the health status of a person that is exposed to a specific context by using the real health status the person experienced when they were exposed to a similar context in the past. Then, CBR confirms the real health status of the person for knowing the accuracy of its prediction and storing the new case to be used in future predictions.
4.1 The Challenge of Determining the Real Asthma Health Status
One of the issues of applying CBR for asthma management is defining the real health status of a person when is exposed to a specific context. It specially challenging as there are no commercial devices that can monitor the asthma health status of a person constantly [30]. This process is highly relevant because the real health status is needed to complete the case to store (retain stage), and to be used to predict the outcomes of future cases (reuse stage). Hence, if the revision is not completed, the accuracy of the prediction cannot be determined, and it will not be possible to use the knowledge of that case for future predictions.
This research work addresses the challenge of determining the asthma health status of a person by proposing a system that is based on the diary version of the ACQ [18,19,20,21]. The ACQ is made of questions that are answered using a scale of 7 (from 0 to 6). The average of the responses is used to assess if the asthma of the person is ‘well-controlled’ or ‘not well-controlled’ [19]. Four versions of the ACQ have been proposed and evaluated, concluding that the measurement properties of all four are almost identical [21]. The system implements the four versions: (1) assessing patient’s symptoms, Peak Expiratory Flow (PEF) and rescue bronchodilator usage, (2) assessing patient’s symptoms and rescue bronchodilator usage, (3) assessing patient’s symptoms and PEF, and (4) assessing only patient’s symptoms. Initially, the ACQ encourages to use the Forced Expiratory Volume in one second (FEV\(_1\)), however it is suggested to use the PEF for the diary version as it is more accessible for people [19].
The proposal is a HiTL system presenting explicit information about the new or updated context to the user, who then defines their health status and makes a decision considering this context [28]. Thus, the system will ask the user to assess their health status when they wake up, before going to sleep and whenever the user feels like in order to create new cases for the databases of previous cases, and when the CBR detects a potentially threatening context in order to revise this prediction. The system allows the application of CBR for personalised asthma management through a GUI permitting to determine the real health status of a person. This is important because it is the needed when the CBR uses the real health status of \(C_s\) to predict the health status of \(C_x\) (reuse), confirms the real health status of \(C_x\) (revise), and stores
 (retain).
(retain).
5 A HiTL System Allowing the Application of CBR for Asthma Management
The system is an Android mobile application developed using Android Studio and SQLite database engine. The first version was developed as an illustration of how to use an approach allowing the personalisation of C-AR applications supporting asthma management [29]. It allows users to configure the indicators to track and the features they need according to the specific characteristics of their asthma management plans. This research work adds a feature to this system, which is based on the explanation provided in Sect. 4.
5.1 System Architecture
The system architecture is shown in Fig. 6. The Personalisation module allows users to personalise the indicators to monitor, and some features like who to notify and how to notify them in emergencies. The Report Generator shows reports considering the personalisation done by the user [29]. The behaviour of the system for when it analyses context-related data is shown in Fig. 7, where the interaction between the Case-Based Reasoner (CB) and the Context-Aware Reasoner (CA) is illustrated. This behaviour occurs when the user configures the system for analysing context using the CB to discover potentially risky situations they are not aware of. If they do not activate this option, then the system will use the CA only, and not the CB, to analyse the context to which they are exposed.
The push approach in Fig. 7 shows how the system behaves when it analyses data in the background and discovers that the user is exposed to a potentially risky context. For this, the Data Collectors send data to the Data Handler (1.1), which interacts with the Database. The Data Handler stores this data and activates (1.2) the CA for it to assess the data that has been gathered. The CA gets the require data for the analysis (1.3, 1.4), and activates the CB (1.5) that assesses the new case (1.6) and sends the results back to the CA (1.7). The CA also analyses the context-related data considering the rules set up by the user (1.8), and activates the Notification Engine (1.9) that sends a notification to the user through the GUI (1.10, 1.11) asking them to assess their real health status in order to confirm whether there is a deterioration or not (1.12). The CA gets this response (1.13), stores it in the Database (1.14, 1.15), and activates the Notification Engine (1.16) that ask the GUI to show the user the outcome of their health assessment (1.17, 1.18). After this, the user can choose what to do. For instance, they may decide just to take their medication, or to use the system to deploy the emergency notification protocol that is explained in [29].
The pull approach in Fig. 7 shows the behaviour of the system when the user chooses to assess their asthma health status. In this case, the user assesses their health status through the GUI of the system (2.1). This information is sent to the CA (2.2) that analyses the data entered by the user to define their health status (2.3). Then, the CA performs two different actions. The first one is sending the real health status to the Data Handler (2.4) that will create a case by gathering the context-related data of the case from the Data Collectors (2.4.1, 2.4.2), getting the predicted outcome for that case (2.4.3, 2.4.4), and storing it in the collection of previous cases (2.4.5). The second one is showing the result of the health assessment to the user through the GUI (2.5, 2.6).
5.2 The Asthma Control Assessment Component of the GUI
This section describes the Asthma Control Assessment Component, which is the part of the system GUI allowing to determining the health status of a person with asthma. This component is based on the ACQ explained in Sect. 4.1, and is used in the activities 1.11, 1.12 and 2.1 presented in Fig. 7. The main screens of Asthma Control Assessment Component are shown in Fig. 8, 9, 10 and 11.
Figure 8 shows the notification that appears (push approach) (1) when the user wakes up, (2) before they go to sleep, and (3) when the system detects a potentially threatening context. When the user taps on the notification, the system takes them to the screen shown in Fig. 9 where they can assess their asthma health status. Here, the user enters the value for their PEF test, the number of rescue bronchodilator puffs they have used in the past 24 hours, and the answer for the other questions of the ACQ. The PEF and number of rescue bronchodilator puffs values can be left in blank because not all of them have access to the PEF meter at all times, and they might not remember the number of rescue puffs. This flexibility lets users to choose implicitly among the four versions of the ACQ explained in Sect. 4.1.
The system also allows users to assess their asthma health status whenever they want (pull approach). For this, they have to open the mobile application, and the main screen will be shown (Fig. 10). Here, the “Control test" option leads them to the screen shown in Fig. 11 where they can check the history of their control test, and edit them by tapping on any of them. The option “New Control Test" (Fig. 11) takes users to the screen shown in Fig. 9, where they can assess their asthma health status. After the assessment, a confirmation message is displayed before redirecting users to the screen shown in Fig. 11.
5.3 Asthma Control Assessment Component Usability Evaluation
This section reports on the usability evaluation of the Asthma Control Assessment Component described in Sect. 5.2. The evaluation was based on the Health-ITUEM, which assesses nine usability-related concepts in order to evaluate the usability of health information technology [13]. The Health-ITUEM have been used to evaluate mobile health technology [13, 30].
The evaluation included four people with asthma and five people that take care of people with asthma. They were asked to use the Asthma Control Assessment Component of the system, and to interact with it by simulating the pull and push behaviours (Sect. 5.2). Then, they were asked to answer a questionnaire made of nine closed and two open questions. One closed question asked about how useful the respondents perceive the idea of using previous risky situations for predicting future risky scenarios. Two closed questions assessed the overall GUI design and user-friendliness. The other six closed questions assessed six Health-ITUEM concepts. The open questions asked about the frequency the system should ask users to complete their asthma control assessment, and about the improvements the respondents would do to the system.
The scenario mapping the Health-ITUEM concepts for the evaluation of the Asthma Control Assessment Component (Table 1) was used to write the Health-ITUEM-related questions. The questionnaire did not include two Health-ITUEM concepts because the Asthma Control Assessment Component of the system was considered simple enough to avoid assessing its Flexibility and Error prevention. A Likert scale going from 0 (very low) to 4 (very high) was used for the closed questions. Figure 12 shows the average of the responses for these questions.
The analysis of the open questions shows that personalisation is highly important to define the frequency of showing the notification reminding to perform the Asthma Control Assessment. Six of them (66.67%) explicitly suggested that the frequency of the notifications should be defined considering the characteristics of the person with asthma. The other three suggested to show the notification two times a day, three times a day, and every 10–12 h.
The proposed improvements are mostly about enhancing the GUI. It was suggested to make the GUI more intuitive (2 respondents), and instructive about how to do the PEF test (1) and what to do if the outcome of the test is “not-well-controlled" (1). Two of them recommended using colours to differentiate the outcomes of the previous tests shown on Fig. 11. One suggestion was about providing an alternative version with simpler instructions for children (1). One respondent proposed to allow users to input data about previous risky situations in order to provide the system with a baseline for future predictions. Another one recommended to integrate the system with activity monitoring devices (e.g. smart watches) for gathering more data about the person’s state.
6 Discussion
Figure 12 shows that the average of the responses for the quantitative questions are between 3 and 4, which are the two highest possible responses in the Likert scale that was used. It is also important to point out that all respondents assessed the idea of using previous risky situations for predicting future risky ones with 4 points, the highest possible response. This supports the idea of using CBR in personalised C-AR solutions supporting asthma management.
The number of positive, neutral and negative responses for the closed questions is another interesting outcome. A negative response has a value of 0 (very bad) or 1 (bad), a neutral one has a value of 2, and a positive one has a value of 3 (good) or 4 (very good). Memorability and Performance got only positive responses. Information needs, User-friendliness and Learnability got 8 positive and 1 negative responses. Competency got 8 positive and 1 neutral responses. Design of the screen and Completeness got 7 positive and 2 neutral responses.
The responses associated with the frequency of showing the notification asking users to assess their asthma control level differs in terms of absolute values. The difference among these responses could be related to their specific contexts but this should be further investigated. Nevertheless, there is evidence suggesting there is no unique frequency that can satisfy the requirements of the users. Hence, another valuable outcome is the need for allowing users to set up the frequency of these notifications according to their specific situations.
7 Conclusions
This research works describes the HCI components of a solution implementing the ACQ in order to determine the asthma health status of a person. The interaction between the HCI and the CBR components of the solution is also explained. The benefits of this interaction are presented as a way of addressing an issue of using CBR for asthma management, which is linking the asthma health status to specific context-related data for creating the cases for the CBR. The solution was evaluated by users from a usability perspective showing positive results and pointing out some key points of improvement.
References
Aamodt, A., Plaza, E.: Case-based reasoning: foundational issues, methodological variations, and system approaches. AI Commun. 7(1), 39–59 (1994). https://doi.org/10.3233/AIC-1994-7104
Abowd, G.D., Dey, A.K., Brown, P.J., Davies, N., Smith, M., Steggles, P.: Towards a better understanding of context and context-awareness. In: Gellersen, H.-W. (ed.) HUC 1999. LNCS, vol. 1707, pp. 304–307. Springer, Heidelberg (1999). https://doi.org/10.1007/3-540-48157-5_29
Acampora, G., Cook, D.J., Rashidi, P., Vasilakos, A.V.: A survey on ambient intelligence in healthcare. Proc. IEEE 101(12), 2470–2494 (2013). https://doi.org/10.1109/JPROC.2013.2262913
Asthma Australia: An Asthma Australia Site (2016). http://www.asthmaaustralia.org.au
Asthma UK: Asthma UK (2016). http://www.asthma.org.uk
Augusto, J., Kramer, D., Alegre, U., Covaci, A., Santokhee, A.: The user-centred intelligent environments development process as a guide toco-create smart technology for people with special needs. Univ. Access Inf. Soc. 17(1), 115–130 (2018). https://doi.org/10.1007/s10209-016-0514-8
Augusto, J.C., Callaghan, V., Cook, D., Kameas, A., Satoh, I.: Intelligent environments: a manifesto. Hum.-Centric Comput. Inf. Sci. 3(1), 12 (2013). https://doi.org/10.1186/2192-1962-3-12
Augusto, J.C., et al.: Personalized smart environments to increase inclusion of people with down’s syndrome. In: Augusto, J.C., Wichert, R., Collier, R., Keyson, D., Salah, A.A., Tan, A.-H. (eds.) AmI 2013. LNCS, vol. 8309, pp. 223–228. Springer, Cham (2013). https://doi.org/10.1007/978-3-319-03647-2_16
Augusto, J.C., et al.: Handbook of Ambient Assisted Living, Ambient Intelligence and Smart Environments, vol. 11. IOS Press, Amsterdam (2012)
Begum, S., Ahmed, M.U., Funk, P., Xiong, N., Folke, M.: Case-based reasoning systems in the health sciences: a survey of recent trends and developments. IEEE Trans. Syst. Man Cybern. Part C (Appl. Rev.) 41(4), 421–434 (2011). https://doi.org/10.1109/TSMCC.2010.2071862
Bichindaritz, I.: Case-based reasoning in the health sciences: why it matters for the health sciences and for CBR. In: Althoff, K.-D., Bergmann, R., Minor, M., Hanft, A. (eds.) ECCBR 2008. LNCS (LNAI), vol. 5239, pp. 1–17. Springer, Heidelberg (2008). https://doi.org/10.1007/978-3-540-85502-6_1
Bichindaritz, I., Montani, S.: Advances in case-based reasoning in the health sciences. Artif. Intell. Med. 51(2), 75–79 (2011)
Brown, W., Yen, P.Y., Rojas, M., Schnall, R.: Assessment of the health IT usability evaluation model (health-ITUEM) for evaluating mobile health (mHealth) technology. J. Biomed. Inform. 46(6), 1080–1087 (2013). https://doi.org/10.1016/j.jbi.2013.08.001
Chang, S., Chiang, R., Wu, S., Chang, W.: A context-aware, interactive m-health system for diabetics. IT Prof. 18(3), 14–22 (2016). https://doi.org/10.1109/MITP.2016.48
Chatzitofis, A., et al.: Hearthealth: a cardiovascular disease home-based rehabilitation system. Proc. Comput. Sci. 63, 340–347 (2015). https://doi.org/10.1016/j.procs.2015.08.352
Dey, A.K.: Understanding and using context. Pers. Ubiquit. Comput. 5(1), 4–7 (2001). https://doi.org/10.1007/s007790170019
Isakovic, M., Cijan, J., Sedlar, U., Volk, M., Bester, J.: The role of mHealth applications in societal and social challenges of the future. In: 2015 12th International Conference on Information Technology - New Generations, pp. 561–566 (2015). https://doi.org/10.1109/ITNG.2015.94
Juniper, E., O’Byrne, P., Guyatt, G., Ferrie, P., King, D.: Development and validation of a questionnaire to measure asthma control. Eur. Respir. J. 14(4), 902–907 (1999). http://erj.ersjournals.com/content/14/4/902
Juniper, E.F., Bousquet, J., Abetz, L., Bateman, E.D.: Identifying ‘well-controlled’ and ‘not well-controlled’ asthma using the asthma control questionnaire. Respir. Med. 100(4), 616–621 (2006). https://doi.org/10.1016/j.rmed.2005.08.012
Juniper, E.F., O’Byrbe, P., Ferrie, P.J., King, D.R., Roberts, J.: Measuring asthma control. Clinic questionnaire or daily diary? Am. J. Respir. Crit. Care Med. 162(4), 1330–1334 (2000). https://doi.org/10.1164/ajrccm.162.4.9912138
Juniper, E.F., Svensson, K., Mörk, A.C., Ståhl, E.: Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir. Med. 99(5), 553–558 (2005). https://doi.org/10.1016/j.rmed.2004.10.008
Khan, N., Alegre, U., Kramer, D., Augusto, J.C.: Is ‘Context-Aware Reasoning = Case-Based Reasoning’? In: Brézillon, P., Turner, R., Penco, C. (eds.) CONTEXT 2017. LNCS (LNAI), vol. 10257, pp. 418–431. Springer, Cham (2017). https://doi.org/10.1007/978-3-319-57837-8_35
Kolodner, J.L.: An introduction to case-based reasoning. Artif. Intell. Rev. 6(1), 3–34 (1992). https://doi.org/10.1007/BF00155578
Montani, S.: How to use contextual knowledge in medical case-based reasoning systems: a survey on very recent trends. Artif. Intell. Med. 51(2), 125–131 (2011). https://doi.org/10.1016/j.artmed.2010.09.004
Nunes, D.S., Zhang, P., Silva, J.S.: A survey on human-in-the-loop applications towards an internet of all. IEEE Commun. Surv. Tutor. 17(2), 944–965 (2015). https://doi.org/10.1109/COMST.2015.2398816
Ospan, B., Khan, N., Augusto, J., Quinde, M., Nurgaliyev, K.: Context aware virtual assistant with case-based conflict resolution in multi-user smart home environment. In: 2018 International Conference on Computing and Network Communications (CoCoNet), pp. 36–44 (2018). https://doi.org/10.1109/CoCoNet.2018.8476898
Perera, C., Zaslavsky, A., Christen, P., Georgakopoulos, D.: Context aware computing for the internet of things: a survey. IEEE Commun. Surv. Tutor. 16(1), 414–454 (2014). https://doi.org/10.1109/SURV.2013.042313.00197
Qin, X., Tan, C.-W., Clemmensen, T.: Context-awareness and mobile HCI: implications, challenges and opportunities. In: Nah, F.F.-H., Tan, C.-H. (eds.) HCIBGO 2017. LNCS, vol. 10293, pp. 112–127. Springer, Cham (2017). https://doi.org/10.1007/978-3-319-58481-2_10
Quinde, M., Khan, N., Augusto, J.C.: Personalisation of context-aware solutions supporting Asthma management. In: Miesenberger, K., Kouroupetroglou, G. (eds.) ICCHP 2018. LNCS, vol. 10897, pp. 510–519. Springer, Cham (2018). https://doi.org/10.1007/978-3-319-94274-2_75
Quinde, M., Khan, N., Augusto, J.C., van Wyk, A., Stewart, J.: Context-aware solutions for asthma condition management: a survey. Univ. Access Inf. Soc. (2018). https://doi.org/10.1007/s10209-018-0641-5
The British Thoracic Society: British guideline on the management of asthma: a national clinical guideline. Technical report (2016). http://www.brit-thoracic.org.uk
The Global Initiative for Asthma: Global strategy for asthma management and prevention. Technical report (2018). http://www.ginasthma.org
Wagner, S., Toftegaard, T., Bertelsen, O.: Increased data quality in home blood pressure monitoring through context awareness. IEEE (2012). https://doi.org/10.4108/icst.pervasivehealth.2011.245968
Acknowledgement
We thank Asthma UK for spreading the questionnaire (Section 3.1), among their representative network of people with asthma and carers. The Context and Context-awareness definitions in Section 1were provided by J.C. Augusto.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this paper
Cite this paper
Quinde, M., Khan, N., Augusto, J.C., van Wyk, A. (2019). A Human-in-The-Loop Context-Aware System Allowing the Application of Case-Based Reasoning for Asthma Management. In: Duffy, V. (eds) Digital Human Modeling and Applications in Health, Safety, Ergonomics and Risk Management. Healthcare Applications. HCII 2019. Lecture Notes in Computer Science(), vol 11582. Springer, Cham. https://doi.org/10.1007/978-3-030-22219-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-22219-2_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-22218-5
Online ISBN: 978-3-030-22219-2
eBook Packages: Computer ScienceComputer Science (R0)