Abstract
One of the most important parameters of sagittal pelvic alignment is the pelvic incidence (PI), which is commonly measured from sagittal X-ray images of the pelvis as the angle between the line connecting the midpoint of the femoral head centers with the center of the sacral endplate, and the line orthogonal to the sacral endplate. In this paper, we present the results of a fully automated measurement of PI from X-ray images that is based on the deep learning technologies. In each sagittal X-ray image of the pelvis, regions of interest (sacral endplate and both femoral heads) are first automatically defined, and then landmarks are detected within these regions, i.e. the anterior edge, the center and the posterior edge of the sacral endplate that define the line of the sacral endplate inclination, and the centers of both femoral heads with the corresponding midpoint representing the hip axis. From the hip axis, and the line along the sacral endplate and its center, PI is computed. Measurements were performed on X-ray pelvic images from 38 subjects (15 males/23 females; mean age 71.1 years), and statistical analysis of reference manual and fully automated measurements revealed a relatively good agreement, with the mean absolute difference ± standard deviation of \(5.1\,{\pm }\,4.4^\circ \) and Pearson correlation coefficient of \(R\,=\,0.82\) (p-value below \(10^{-6}\)), with the paired t-test revealing no statistically significant differences (p-value above 0.05). The differences between reference manual and fully automated measurements were within the repeatability and reliability of manual measurements, indicating that PI can be accurately determined by the proposed fully automated approach.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Pelvic incidence (PI) is one of the most important parameters of sagittal pelvic alignment, and is represented by the angle between the line connecting the hip axis (i.e. the midpoint of the centers of both femoral heads) with the center of the sacral endplate, and the line orthogonal to the sacral endplate [1, 2]. As such, it describes the relative position of the sacral endplate against the femoral heads, and therefore the anatomical characteristics of the pelvis in the sagittal plane and the balance of the lumbar spine that rests on the sacrum. The mean PI for a healthy population is \(47^\circ \) – \(57^\circ \) with a standard deviation (SD) of around \(10^\circ \) [2], nevertheless, a very low PI (\(35^\circ \) – \(44^\circ \)) means that the femoral heads are positioned just below the sacral endplate with the pelvis being narrow horizontally and large vertically (i.e. a vertical pelvis), while a very high PI (\(75^\circ \)–\(85^\circ \)) means that the femoral heads are position ahead of the midpoint of the sacral endplate with the pelvis being narrow vertically and large horizontally (i.e. a horizontal pelvis) [3]. Measurement of PI is most commonly performed in sagittal X-ray images of the pelvis (Fig. 1), however, it represents a relatively tedious and subjective task, mostly because of the quality of the acquired images and their projective nature [4,5,6]. Although several software packages exist for computerized measurement of PI [4, 7,8,9,10], the resulting measurements are still based on manually defined points, geometrical constructs and statistical modeling, and therefore are not fully automated. In this paper, we present the results of a fully automated measurement of PI from X-ray images of the pelvis.
(a) A sagittal X-ray of the pelvis. (b) The parameters of the pelvic incidence (PI) as the angle between the line connecting the hip axis (HA, the midpoint between the centers of both femoral heads) with the first sacral (S1) endplate center and the line orthogonal to the S1 endplate, sacral slope (SS) as the angle between the line along the S1 endplate and the horizontal reference, and pelvic tilt (PT) as the angle between the line connecting the HA with the S1 endplate center and the vertical reference. The following relationship is established: SS + PT = PI.
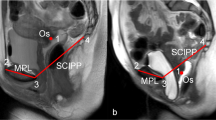
Fully automated measurement of pelvic incidence. (a) The region of interest (ROI) for the first sacral (S1) endplate and for both femoral heads (FH1, FH2), with landmarks within each ROI: the anterior edge, the center and the posterior edge on the S1 endplate, and the centers of both femoral heads. (b) The sacral slope is determined by fitting a line to the landmarks. The hip axis (HA) is determined as the midpoint between the centers of the femoral heads.
2 Methodology
The automated measurement of PI from X-ray pelvic images is based on deep learning and consists of three stages,Footnote 1 i.e. the identification of the regions of interest (ROIs), determination of distinctive points or landmarks, and measurement of PI (Fig. 2). The first stage (Fig. 2(a)) is the automated identification of ROIs that contain the observed anatomical structures, i.e. the first sacral (S1) endplate and each individual femoral head, in the given X-ray image. For this purpose, we designed a special architecture of convolutional neural networks (CNNs) [11] that was trained on a set of X-ray images with predefined ROIs. The second stage (Fig. 2(a)) is the automated determination of landmarks, i.e. the center of each femoral head and the anterior edge, the center and the posterior edge of the S1 endplate, within the corresponding ROIs obtained in the first stage. For this purpose, we designed a second CNN architecture [12] that was trained on a set of X-ray images with predefined landmarks. The third stage (Fig. 2(b)) is the automated determination of the line along the S1 endplate, which is obtained by least square fitting to the landmarks defined on the S1 endplate in the second stage, and the determination of the hip axis as the midpoint between the centers of both femoral heads. From the acquired data, we can measure PI as the sum of SS and PT.
3 Results
The automated measurement of PI was evaluated on sagittal X-ray images of the pelvis from 44 subjects (16 males/28 females; mean age 71.5 years, age range 49–85 years) that were acquired at Charité University Hospital (Berlin, Germany) by the Kodak Elite CR and Kodak DRX-Evolution scanners (Carestream Health; Rochester, New York, USA) for purposes not related to this retrospective study. For each image, reference manual measurements of PI, SS and PT were obtained, which allowed for a statistical comparison with the fully automated measurements. However, reference manual measurements could not be reliably performed in six out of 44 X-ray images because of the partially visible femoral heads in two cases, and ambiguities in the determination of the center and inclination of the S1 endplate in four cases. As a result, these images were excluded from statistical comparison, which was in the end performed for images of 38 subjects (15 males/23 females; mean age 71.1 years, age range 49–85 years). The results are presented in terms of the mean absolute difference (MAD), the corresponding SD and the Pearson correlation coefficient (R). Statistical significance was observed through the paired t-test, with the level of significance set to \(p\,{<}\,0.05\).
Reference manual measurements amounted to \(54.4\,{\pm }\,11.8^\circ \) (mean ± SD) for PI, \(35.0\,{\pm }\,8.7^\circ \) for SS and \(19.4\,{\pm }\,8.5^\circ \) for PT, which is in accordance with existing population studies [2]. With the described fully automated approach we then successfully measured the same parameters, which amounted to \(54.0\,{\pm }\,10.4^\circ \) for PI, \(34.3\,{\pm }\,8.6^\circ \) for SS and \(19.6\,{\pm }\,8.5^\circ \) for PT. Statistical analysis of the agreement between manual and automated measurements is presented in Table 1 and Fig. 3.
4 Discussion
The determination of PI from X-ray images is a relatively demanding process because the projective nature of X-ray imaging causes a virtual superposition of the anatomical structures of interest. Moreover, different characteristics that originate from the natural biological variability of the human anatomy may also introduce ambiguities in the measurement process. Software packages that allow for computerized measurement of PI by manually drawing geometrical constructs (e.g. points, lines, circles) [4, 7,8,9,10] proved to be more reproducible and reliable than measurements from plain X-ray films, as Vialle et al. [7] reported a mean reproducibility of \(R\,=0.86\) (\(p\,=\,0.014\)) and \(R\,=0.96\) (\(p\,<\,0.001\)), and a mean reliability of \(R\,=0.65\) (\(p\,=\,0.024\)) and \(R\,=0.99\) (\(p{<}0.001\)) respectively for manual measurements of PI from plain X-ray films and digital X-ray images. Dimar II et al. [8] reported an even worse agreement, as they obtained a mean reproducibility of \(R\,=\,0.65\), 0.71 and 0.55 and a mean reliability of \(R\,=\,0.29\), 0.61 and 0.44 respectively for PI, SS and PT, while the agreement with computerized measurements was estimated to \(R\,=\,0.59\), 0.72 and 0.63, respectively. Although computerized approaches improved the reproducibility and reliability, the measurement itself remains a relatively time-consuming and subjective task that highly depends on the experience of the observer. On the other hand, a fully automated measurement approach has not been yet presented, mostly because it represents a challenging problem from the perspective of automated analysis of X-ray images.
The described approach solves, to a certain degree, the afore mentioned problem. Statistical analysis (Table 1) revealed that there are no statistically significant differences between reference manual and fully automated measurements of PI, as well as of SS and PT. We can also conclude that the fully automated measurements are in agreement with reference manual measurements in the reliability range of classical and computerized manual measurements [7, 8], as the correlation was good (\(0.7\,{<}\,R\,{<}\,0.9\)) in the case of PI and SS, and very good (\(0.9\,{<}\,R\,{<}\,1.0\)) in the case of PT. Nevertheless, high correlation and a relatively low MAD do not necessarily mean that the fully automated measurements are correct, moreover, a difference of around \(5^\circ \) may originate from the reproducibility and reliability of manual measurements [2]. The high agreement of reference manual and fully automated measurements results from applying the state-of-the-art deep learning technologies. It is also important to note that the proposed approach does not make use of already implemented techniques, but is refined with a detailed knowledge of CNN architectures, corresponding criterion functions and methods of supervised learning, as well as a detailed knowledge of spine and pelvis anatomy, and measurement of geometrical parameters from medical images.
5 Conclusion
In this paper, we presented the results of a fully automated measurement of PI from sagittal X-ray images of the pelvis. The results indicate that by this approach, it is possible to accurately determine PI, as the differences against reference manual measurements were within the range of the reproducibility and reliability of manual measurements. Nevertheless, the proposed fully automated approach cannot completely replace the visual review and confirmation of the measured values by an observer, as the differences may be in certain cases quite large, mostly due to the natural biological variability of the human anatomy and the characteristics induced by X-ray imaging.
Notes
- 1.
Due to a copyright agreement, we cannot entirely disclose the technical details of our methodology. We therefore invite the reader to focus on the clinical application and the obtained results.
References
Duval-Beaupère, G., Schmidt, C., Cosson, P.: A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann. Biomed. Eng. 20(4), 451–462 (1992). https://doi.org/10.1007/BF02368136
Vrtovec, T., Janssen, M., Likar, B., Castelein, R., Viergever, M., Pernuš, F.: A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment. Spine J. 12(5), 433–446 (2012). https://doi.org/10.1016/j.spinee.2012.02.013
Le Huec, J., Aunoble, S., Leijssen, P., Pellet, N.: Pelvic parameters: origin and significance. Eur. Spine J. 20(Suppl 5), S564–S571 (2011). https://doi.org/10.1007/s00586-011-1940-1
Berthonnaud, E., Labelle, H., Roussouly, P., Grimard, G., Vaz, G., Dimnet, J.: A variability study of computerized sagittal spinopelvic radiologic measurements of trunk balance. J. Spinal Disord. Tech. 18(1), 66–71 (2005). https://doi.org/10.1097/01.bsd.0000128345.32521.43
Tyrakowski, M., Yu, H., Siemionow, K.: Pelvic incidence and pelvic tilt measurements using femoral heads or acetabular domes to identify centers of the hips: comparison of two methods. Eur. Spine J. 24(1), 1259–1264 (2015). https://doi.org/10.1007/s00586-014-3739-3
Yamada, K., Aota, Y., Higashi, T., Ishida, K., Numura, T., Saito, T.: Accuracies in measuring spinopelvic parameters in full-spine lateral standing radiograph. Spine 40(11), E640–E646 (2015). https://doi.org/10.1097/BRS.0000000000000904
Vialle, R., Ilharreborde, B., Dauzac, C., Guigui, P.: Intra and inter-observer reliability of determining degree of pelvic incidence in high-grade spondylolisthesis using a computer assisted method. Eur. Spine J. 15(10), 1449–1453 (2006). https://doi.org/10.1007/s00586-006-0096-x
Dimar II, J., Carreon, L., Labelle, H., Djurasovic, M., Weidenbaum, M., Brown, C., et al.: Intra- and inter-observer reliability of determining radiographic sagittal parameters of the spine and pelvis using a manual and a computer-assisted methods. Eur. Spine J. 17(10), 1373–1379 (2008). https://doi.org/10.1007/s00586-008-0755-1
Lafage, R., Ferrero, E., Henry, J., Challier, V., Diebo, B., Liabaud, B., et al.: Validation of a new computer-assisted tool to measure spino-pelvic parameters. Spine J. 15(12), 2493–2502 (2015). https://doi.org/10.1016/j.spinee.2015.08.067
Maillot, C., Ferrero, E., Fort, D., Heyberger, C., Le Huec, J.C.: Reproducibility and repeatability of a new computerized software for sagittal spinopelvic and scoliosis curvature radiologic measurements: Keops®. Eur. Spine J. 24(7), 1574–1581 (2015). https://doi.org/10.1007/s00586-015-3817-1
Lin, T., Goyal, P., Girshick, R., He, K., Dollár, P.: Focal loss for dense object detection. In: Proceedings of the IEEE International Conference on Computer Vision, ICCV 2017, pp. 2999–3007. IEEE (2017). https://doi.org/10.1109/ICCV.2017.324
Krizhevsky, A., Sutskever, I., Hinton, G.: ImageNet classification with deep convolutional neural networks. In: Pereira, F., et al. (eds.) Proceedings of the Neural Information Processing Systems, NIPS 2012, vol. 25, pp. 1097–1105. NIPS (2012)
Acknowledgements
This work was supported by Raylytic GmbH, Leipzig, Germany, partly by the Slovenian Research Agency under grants P2-0232 and J2-7118, and partly by the German Research Foundation (DFG) under project number PU 510/2-1.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this paper
Cite this paper
Korez, R., Putzier, M., Vrtovec, T. (2019). Automated Measurement of Pelvic Incidence from X-Ray Images. In: Vrtovec, T., Yao, J., Zheng, G., Pozo, J. (eds) Computational Methods and Clinical Applications in Musculoskeletal Imaging. MSKI 2018. Lecture Notes in Computer Science(), vol 11404. Springer, Cham. https://doi.org/10.1007/978-3-030-11166-3_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-11166-3_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-11165-6
Online ISBN: 978-3-030-11166-3
eBook Packages: Computer ScienceComputer Science (R0)