Abstract
There are three reasons why we must look far back in time when predicting future mortality trends. Firstly, the mortality decline that we can observe today has its roots in improvements achieved long ago in living standards and diet, public health institutions, medicine, and other areas relevant to the physical well-being of the population. Speaking in general terms, living conditions improve from one period to the next. Such improvements are called period factors, since they relate to living conditions for the entire population during one specific period.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
There are three reasons why we must look far back in time when predicting future mortality trends. Firstly, the mortality decline that we can observe today has its roots in improvements achieved long ago in living standards and diet, public health institutions, medicine, and other areas relevant to the physical well-being of the population. Speaking in general terms, living conditions improve from one period to the next. Such improvements are called period factors, since they relate to living conditions for the entire population during one specific period.
Secondly, the health and remaining life span for people living today is determined not only by contemporary period factors but also by living conditions earlier in life. Since even conditions in the foetal stage have an influence on longevity, improvements during early childhood could have an effect on mortality trends today. These are called cohort factors, since they relate to the conditions for a certain cohort, often birth cohort, while previous cohorts are unaffected. Since the oldest people living today were born a hundred or more years ago, we have to consider cohort factors far back in time in predicting future mortality.
Thirdly, predicting future mortality trends also requires a multivariate point of departure. No single factor, but a variety of factors, determines health and remaining life span, and we do not know a priori which one is the most important. Thus, predicting future mortality trends calls for a long-term multivariate, causal approach, in which both period and cohort factors are taken into account. This kind of holistic view has not always been in favour. Early in the twentieth century, cohort factors were considered most important, while multivariate period factors became more popular later on, followed in turn by a preference for single-period factors as the main determinant of the great mortality decline since the mid-eighteenth century. Now we are once again discussing cohort factors.
Thus, there has been a shift over time in our explanations for the mortality decline (Bengtsson 1998). Below I shall develop the reasons why I think we need to take a multivariate, period, and cohort approach. I will start with an overview of the great mortality decline, commencing several hundred years ago, and then move on to discuss how the explanations for the historical decline have changed over time.
Over the past 300 years, human physiology has undergone profound changes. These were made possible by numerous advances whereby humans have gained an unprecedented degree of control over their environment. The changes include increases in body size by over 50%, in length of life by over 100%, and in time lived in retirement by several hundred per cent, with obvious implications for expenditures on pensions and health care. The extension of the human life span has been gradual, starting a long time ago with what now is called the great mortality decline.
The timing of the great mortality decline was strikingly similar in the countries of Western and Northern Europe despite differences in economic structure and development. It started in the mid-eighteenth century, levelled off for a couple of decades in the mid-nineteenth century, and then continued. Over this period, life expectancy at birth rose from some 35 years to more than 70 years. The development in North America was similar.
Few scholars today will argue that the great mortality decline was due solely or primarily to a single factor. Economic growth, for example, was probably not a major determinant before or during the initial stages of the great mortality decline, and its effect may be far less than expected during later stages of the decline. Instead, the causes are multi-factorial and vary from the start to the end of the decline.
In countries for which long historical series of age-specific mortality rates (England, France, and some others, including the Nordic countries) are available, we know that the increase in life expectancy began with a fall in the rates of infant and child mortality. This was mainly due to a reduction in deaths from smallpox, which was a very common childhood disease in the eighteenth century.
While infant mortality continued to decline in Sweden throughout the nineteenth century, it levelled off in England and remained stable until the end of the nineteenth century, when it again dropped rapidly, as was the case in all other Western countries. Childhood mortality in both countries actually increased in the mid-nineteenth century before commencing a persistent decline. This exemplifies two patterns of the historical decline in infant and childhood mortality: a northern pattern with declines essentially throughout the nineteenth century, and a western one with a levelling off during the nineteenth century and a further decline after the 1880s (Perrenoud 1984).
Adult and old-age mortality started to decline gradually at the beginning of the nineteenth century, possibly earlier for England. The decrease was generally sharper in the later years of the nineteenth century and even more so after the First World War, as was the case with mortality at all other ages. The decline slowed for adults and the elderly around 1950 but accelerated again in the 1970s.
With the great mortality decline followed a change in the leading causes of death, from pestilence, to receding pandemics, and then to man-made diseases (Omran 1971). In his theory of epidemiological transition, Omran identified three different development patterns: the classical or western pattern, described above, the accelerated pattern, and the delayed pattern. They are distinguished by differences in timing and speed. The decline that took 200 years in the West started 150–200 years later in the Third World but then took less than 50 years to complete. In many countries, the great mortality decline has not yet occurred, and the gains from low mortality are still to be reaped.
The great mortality decline can be viewed in light of two approaches, one based on period factors, the other on cohort factors. Most studies focus largely on period factors. In addition, factors based almost entirely on human actions should be distinguished from those beyond deliberate human control. One widely accepted multi-factorial explanation (United Nations 1953) is based on period factors that depend upon human activity: these include public health reforms, advances in medical knowledge, improved personal hygiene, and rising income and standards of living. This explanation is highly similar to the demographic-transition theory (Davis 1945; Notestein 1953; Bengtsson and Ohlsson 1994).
On a broader front, McKeown (1976) questioned the multi-factorial explanation of the great mortality decline. He argued that a single factor – better nutrition – could almost entirely explain the great mortality decline. His criticism was based on a study of cause-specific mortality in England and Wales from 1838 to 1947, where he observed that two-thirds of the mortality decline was due to a reduction in infectious diseases. In later work, he also analysed mortality rates and economic development for other countries and further back in time, though not in such detail as for England and Wales.
McKeown argued that medical advances had little influence on mortality trends before the breakthrough of sulphonamides and antibiotics in the 1930s and 1940s. Previously, the only curable disease had been diphtheria. Very few deaths, however, were due to diphtheria, and its incidence was already receding when the antitoxin came into use around 1900. For periods before 1838, McKeown held that inoculation and vaccination for smallpox had little or no impact on the general mortality decline. Vaccination started in England at the end of the eighteenth century, but it did not become widespread until after 1840, when it was made available at public expense. The history of vaccination in the Nordic countries is similar. There, smallpox mortality was declining even before vaccination started in the first years of the nineteenth century and well before it became common in the 1820s. However, not all scholars agree on this interpretation. Easterlin (1999) downplays the role of economic development and better diet, contending that advancement in medical knowledge is the principal reason for the mortality decline from the mid-nineteenth century onwards.
The improvement of personal hygiene may have had some effect on mortality in England and Wales after about 1880, when the incidence of intestinal infections declined, probably because of substantial improvements in water supply and sewage control at that time. Prior to 1870, the decrease in intestinal infections accounted for only a small part of the general decline in mortality, and according to McKeown, neither better personal hygiene nor measures to improve public health had any significant impact on the overall decline before 1870. Other public-health measures, such as the breast-feeding campaigns in Sweden in the 1830s and thereafter, were not discussed by McKeown. Fridlizus (1984) has argued that while these campaigns might well have had an impact on infant mortality in Sweden, they began much later than the decline in mortality. In fact, childhood mortality went up somewhat at the time of the first breast-feeding campaigns.
In 1957, Helleiner argued that the population of Western Europe must have increased from the mid-eleventh century to the late thirteenth century and from the mid-fifteenth century to the end of the sixteenth century (Helleiner 1957). The population increase observed in the eighteenth century was therefore unique only in that the mortality decline started from a higher level and went on longer than before. Helleiner and other scholars have contended that these changes in mortality were spontaneous (natural), and in 1973 the UN added natural factors as a fifth determinant of the great mortality decline (United Nations 1973). Later, others like Fridlizus (1984), Perrenoud (1984) and Schofield (1984) asserted that a change in the virulence of pathogens initiated the great mortality decline. Their basic assumption was that the virulence of pathogens changes spontaneously over time. Virulence in a pathogenic organism is generally understood as its ability to overcome host defences. At this point, it is important to note that some pathogens develop more quickly in a malnourished host, whereas others do not depend on a weakening of the host to produce very high mortality.
McKeown’s main argument on this subject, though not proved, is that the initial development of mortality in the late eighteenth century was an integral part of the great mortality decline. Since the decline continued for the next two centuries, it cannot be due to a spontaneous reduction in the virulence of pathogens; thus, according to McKeown, the only explanation left is better nutrition. Improved nutrition would explain not only the decline in infectious diseases from the mid-nineteenth century onwards, but also the initial decline. This reasoning is part of McKeown’s attempt to find one single explanation for the entire mortality decline.
Fogel (1994) criticized McKeown’s reasoning for considering only nutritional intake, or diet, while ignoring the needs of the body to maintain itself and build up cells. Thus, McKeown only took into account gross nutrition, rather than net nutrition; the latter must be more closely related to health and mortality. I will come back to this issue shortly.
Cohort explanations for the mortality decline refer to factors that initially affect only certain young age groups but may have a long-lasting impact on these groups. Such factors would consist mainly of improvements in childhood conditions, or even conditions during the foetal stage, that have lasting effects on health and on the life span. Net nutrition is seen as the principal determinant of cellular development, which is most rapid during the foetal stage and gradually diminishes until the body is fully developed around the age of 20. Net nutrition is what is left for the development of cells after the nutritional requirements of other life-sustaining functions and work have been met. Thus, low net nutrition could be due either to low nutritional intake or to additional, disease-related needs of the body for nutrition. Moreover, many diseases not only claim nutrients but also make it more difficult for the body to absorb nutrients in general, as is the case with infectious diseases. If cells and organs consequently fail to develop properly, a child’s growth and development may be inhibited, and the child may be less healthy in general. Thus, we can differentiate between two basic types of cohort explanations for the mortality decline, namely (i) increased nutritional intake during the foetal stage and/or early years of life, and (ii) decreased needs for nutrition during the foetal stage or early years of life owing to less disease in the mother or the child.
The importance of early childhood conditions for later life has probably been well known since time immemorial. It is often assumed that each generation shows the same relative mortality from childhood to old age. Kermack, McKendrick and McKinley adopted this assumption in 1934 when scholars were starting to become aware of the great mortality decline (Kermack et al. 1934). Strangely enough, cohort factors were out of fashion when the UN in 1953 and 1973 made its synthesis of the causes of the great mortality decline. Over the last couple of decades, both medical and historical research on this matter has expanded rapidly (for an overview, see Elo and Preston 1992).
In this connection, the work by Barker (1994 and elsewhere) has been of major importance. He has summarised the medical evidence showing the importance of foetal and neonatal nutrition for adult health. In historical research, Fogel (1996) is probably the leading advocate of these ideas. In addition, Preston and van de Walle (1978) for urban France, and Fridlizius (1989) for Sweden, emphasised the importance of cohort factors for the mortality decline. Bengtsson and Lindström found that exposure to disease from airborne infections has a strong effect on mortality among the elderly (Bengtsson and Lindström 2000, 2001).
Steckel (1983) and Fogel (1996 and previous work) use final body height as a measure of net nutrition and health during childhood. Individuals who have had well-nourished and healthy mothers, and thus have been well nourished themselves during the foetal stage, have a lower risk of death during infancy. If they are well nourished and healthy, their cells and organs develop better, they grow taller, and they live longer. Since health is determined by net nutrition and not gross nutrition, there is no direct link between gross nutrition and height attained. Improvements in health and height may be due either to better nutrition (better diet) or to more limited claims on nutrition from disease. Thus, a decline in the prevalence of smallpox, for example, has a positive effect on height and extends the life span, everything else being equal. The problem is to evaluate how much of the improvement in health is due to diet and how much is due to less disease. Calculating diets for pre-modern populations is a difficult task (Fogel 1996), and it is even harder to calculate disease-related claims on nutrition. Still, historical records show similarities between trends in height and gross consumption of nutrition (Fogel 1994, 1996), indicating that trend in disease-related claims has been of minor importance. If that is the case, then McKeown’s focus on gross nutrition may be justified.
Whether due to a low or badly composed nutritional intake, or to greater claims on nutrition from diseases, undernourishment may stunt growth in height or weight and lead to illness, disease and mortality later in life more than in the immediate future. The immediate relationship, or period link, between the economy and mortality, therefore, is much weaker than Malthus believed, according to Fogel. The rather tenuous short-term relationship often found between prices and deaths for many European countries, as shown by Lee (1981, 1993), Galloway (1988) and others, supports this interpretation (Fogel 1994). Thus, cohort factors matter more to the mortality decline than period factors, according to Fogel.
To summarise, few scholars today will argue that any single factor is the primary determinant of the great mortality decline. Of course, it is no coincidence that the vast growth in resources resulting from the transformation of our economies in the eighteenth and nineteenth centuries was concurrent with the great mortality decline and with the fertility transition as well. In a millennial perspective, these events took place at about the same time. This is not to say, however, that there is a close relationship between the economy and the great mortality decline. On the contrary, economic growth has probably not been a major determinant, either before the great mortality decline or in its initial stages, and its impact may have been far less than expected during later stages of the decline. Instead, the causes are multi-factorial and vary from the start to the end of the decline.
Initially, the decline may well have been partly due to pure luck, for example spontaneously less aggressive smallpox pathogens as part of an old demographic pattern rather than the result of a modernisation process. Later development and compulsory use of vaccine surely prevented the re-emergence of the more aggressive virus. Improvements in nourishment and in the care of mothers and children had long-lasting effects on life span. Advancements in water supply and sanitation as well as better housing contributed to the decline from the second part of the nineteenth century onwards. Medical progress in the twentieth century prolonged life. The fact that health is determined by net nutrition – intake of nutrition minus claims on nutrition – and that claims are partly disease-related, makes it difficult to evaluate the determinants of the mortality decline. The influence of conditions in childhood – including temporary ones – on mortality at older ages adds further complexity. The impact of each individual factor is therefore very difficult to measure; to do so would require a long series of high-quality data. Several variables, such as the virulence of pathogens and the claims on nutrients due to disease can at best be estimated indirectly, if at all. The analyses based on highly aggregated longitudinal data have identified the problems and directed us toward the solutions. It is more doubtful, however, whether solutions will be found at that level of analysis. Perhaps the use of longitudinal micro data will serve as valuable complement, as it has in other areas.
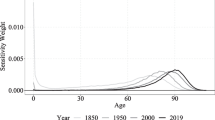
In my opinion, the development of theories about the great mortality decline can be summarised in Fig. 8.1, which also could give us some guidance for the future.
Thus, the cause of the great mortality decline is clearly multi-factorial, and the importance of the various factors changes over time. Both period and cohort factors must be taken into account in analysing the decline. A longterm perspective is essential in predicting future mortality trends. Combining longitudinal information for individuals with information at the societal level is likely to provide important information about mortality determinants in the past and may be useful for predicting future trends as well. Previously, both population and mortality projections were based largely on periodic information about demographic trends. The use of demographic cohort information in the 1990s was a considerable advancement. The question now is whether we are ready to take a great step forward by using multivariate causal models that combine information at the individual and societal levels.
References
Barker, D. J. P. (1994). Mothers, babies and disease in later life. London: BMJ.
Bengtsson, T. (1998). The great mortality decline: Its causes and consequences. In C.-E. Núñez (Ed.), Debates and controversies in economic history. Madrid: Fundación Ramón Areces.
Bengtsson, T., & Lindström, M. (2000). Childhood misery and disease in later life: The effects on mortality in old-age of hazards experienced in early life, southern Sweden, 1760–1894. Population Studies, 54(2), 263–277.
Bengtsson, T., & Lindström, M. (2001, November). Airborne infectious diseases in infancy and mortality in later life, southern Sweden 1766–1894. Paper presented at the Social Science History Association conference in Chicago.
Bengtsson, T., & Ohlsson, R. (1994). The demographic transition revised. In T. Bengtsson (Ed.), Population, economy, and welfare in Sweden. Berlin: Springer.
Davis, K. (1945). The world demographic transition. Annals of the American Academy of Political and Social Sciences, 237, 1–11.
Easterlin, R. A. (1999). How beneficent is the market? A look at the modern history of mortality. European Review of Economic History, 3(3), 257–294.
Elo, I., & Preston, S. (1992). Effects of early-life conditions on adult mortality: A review. Population Index, 59(2), 186–212.
Fogel, R. W. (1994). The relevance of Malthus for the study of mortality today: Long-run influences on health, mortality, labour force participation, and population growth. In K. Lindahl-Kiessling & H. Landberg (Eds.), Population, economic development, and the environment. Oxford: Oxford University Press.
Fogel, R. W. (1996). The Escape from hunger and premature death 1700–2100: Europe, America and the Third World. The 1996 Ellen McArthur Lectures, Cambridge.
Fridlizius, G. (1989). The deformation of cohorts: Nineteenth century mortality decline in a generational perspective. Scandinavian Economic History Review, 37(3), 3–17.
Fridlizus, G. (1984). The mortality decline in the first phase of the demographic transition: Swedish experiences. In T. Bengtsson, G. Fridlizius, & R. Ohlsson (Eds.), Pre-industrial population change: The mortality decline and short-term population movements (pp. 71–114). Lund: Amqvist & Wiksell International.
Galloway, P. R. (1988). Basic patterns in annual variations in fertility, nuptiality, mortality and prices in pre-industrial Europe. Population Studies, 42, 275–302.
Helleiner, K. F. (1957). The vital revolution reconsidered. Canadian Journal of Economics and Political Science, 23, 1–9.
Kermack, W. O., McKendrick, A. G., & McKinley, P. L. (1934, March). Death rates in Great Britain and Sweden: Some regularities and their significance. The Lancet, 223, 698–703.
Lee, R. D. (1981). Short-term variation: Vital rates, prices and weather. In E. A. Wrigley & R. S. Schofield (Eds.), The population history of England, 1541–1871: A reconstruction. London: Edward Arnold.
Lee, R. D. (1993). Inverse projections and demographic fluctuations: A critical assessment of new methods. In D. Reher & R. S. Schofield (Eds.), Old and new methods in historical demography. Oxford: Oxford University Press.
McKeown, T. (1976). The modern rise of population. London: Edward Arnold.
Notestein, F. W. (1953). Economic problems of economic change. In Proceedings of the eight international conference of agricultural economics, London.
Omran, A. R. (1971). The epidemiological transition. A theory of the epidemiology of population change. Millbank Memorial Fund Quarterly, 49(4), 509–538.
Perrenoud, A. (1984). The mortality decline in a long term perspective. In T. Bengtsson, G. Fridlizius, & R. Ohlsson (Eds.), Pre-industrial population change: The mortality decline and short-term population movements. Almqvist & Wiksell International: Lund.
Preston, S. H., & van de Walle, E. (1978). Urban French history in the nineteenth century. Population Studies, 32, 275–297.
Schofield, R. S. (1984). Population growth in the century after 1750: The role of mortality decline. In T. Bengtsson, G. Fridlizius, & R. Ohlsson (Eds.), Pre-industrial population change. Almqvist & Wiksell International: Lund.
Steckel, R. (1983). Height and per capita income. Historical Methods, 16, 1–7.
United Nations. (1953). The determinants and consequences of population trends (Population Studies, No 17). New York.
United Nations. (1973). The determinants and causes of population trends (Population Studies, No 50). New York.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Bengtsson, T. (2019). The Need for Looking Far Back in Time When Predicting Future Mortality Trends. In: Bengtsson, T., Keilman, N. (eds) Old and New Perspectives on Mortality Forecasting . Demographic Research Monographs. Springer, Cham. https://doi.org/10.1007/978-3-030-05075-7_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-05075-7_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-05074-0
Online ISBN: 978-3-030-05075-7
eBook Packages: Social SciencesSocial Sciences (R0)