Abstract
Recommendations on the management of infections in patients with sepsis and septic shock are mainly derived from studies on bacterial sepsis in high-income settings and are not necessarily applicable elsewhere due to differences in etiology and diagnostic or treatment capacity. In this chapter, we provide recommendations on infection management in resource-limited ICUs, taking into account relevant contextual factors such as the availability, affordability, and feasibility of interventions.
We recommend empirical antibiotic therapy in patients with sepsis should cover all expected pathogens and likely resistance patterns, based on locally acquired epidemiological data as large regional variations exist. Limited availability of certain classes of antibiotics can complicate implementation of this. We suggest that research groups in collaboration with stakeholders provide microbiological data from sentinel sites throughout resource-limited settings to guide local empirical antibiotic choices.
There is weak evidence from resource-limited settings suggesting timely administration of antibiotics is beneficial. Observational data suggest that, in many resource-limited settings, the administration of antibiotics to most patients within 1 h of sepsis or septic shock recognition is feasible. Therefore, given biological plausibility and evidence from resource-rich settings, we recommend appropriate antibiotics should be given within the first hour following sepsis or septic shock recognition. In resource-limited settings, microbiological laboratory facilities are often restricted, but there was evidence from these settings that taking blood cultures was associated with improved outcome in sepsis and septic shock and with improved appropriateness of antibiotics. We recommend that blood cultures should be taken before the administration of antibiotics in locations where this is possible. Ideally, two sets of blood cultures should be obtained, although the additional yield has not been assessed in resource-limited settings. It is realized that in many hospitals, routine blood culture is unfeasible and expanding microbiological laboratory capacity could improve care.
Identification of an infection source and source control are additional challenges in resource-limited settings and are affected by the facilities available. There was weak evidence of reasonable sensitivity of both chest radiography and ultrasound in the diagnosis of abdominal hollow viscus perforation (mainly studied in typhoid or tuberculosis) and abscesses in melioidosis. We found weak evidence that timely surgery was beneficial in typhoidal gastrointestinal perforations. Because of lack of published evidence, we do not provide specific recommendations on the use of chest radiography or ultrasound in resource-limited settings. We suggest that source control is carried out within 12 h of admission to hospital, except in the specific case of pancreatic necrosis, where there is evidence from resource-rich settings that delay in surgical intervention may be beneficial.
Combination antimicrobial therapy increases healthcare costs and toxicity. Current SSC guidelines only recommend combination therapy in specific situations, such as when the chances of multidrug resistance are high. Evidence in multidrug-resistant or extensively drug-resistant bacteria was confined to studies of Acinetobacter baumannii infection, where combination therapy was beneficial. Where the chances of multidrug resistance are high, combination antibiotics should be considered. Choice of combination therapy should be guided by local epidemiology and known effective combinations. Antimicrobial therapy should be de-escalated whenever possible. It is recognized that without microbiological information, de-escalation is difficult. The use of biomarkers such as procalcitonin to guide de-escalation of antimicrobial therapy is promising but needs further assessment in resource-limited settings before a recommendation can be made.
In conclusion, large variations in disease etiology and high rates of antimicrobial resistance combined with restricted choice of antibiotics and limited microbiological data pose significant challenges in the management of septic patients in resource-limited settings. Increased use of combination therapy and broad-spectrum antibiotic risks increases antimicrobial resistance. Enhanced surveillance necessitates better collaboration between stakeholders and improved microbiological facilities, which in turn requires significant investment. However, newer technologies which negate the need for specialist staff and equipment may become more available. This would not only improve the management of individual patients but, by providing high-quality epidemiological data, may help combat the global threat of antimicrobial resistance.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
8.1 Introduction and Definitions
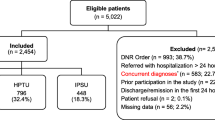
Although there are only limited data available, studies indicate that sepsis and septic shock in resource-limited settings are at least as common as in resource-rich settings. There are important differences in the causative pathogens of sepsis and septic shock between resource-rich and resource-limited settings. Staffing, diagnostic facilities, therapeutic options, and other factors also differ in resource-limited settings, which makes that the Surviving Sepsis Campaign (SSC) guidelines on sepsis management derived from high-income settings are not necessarily directly applicable to these settings [1]. In this chapter, SSC recommendations that were deemed warranting additional evaluation for their use in resource-limited settings were reviewed specifically relevant evidence generated in resource-limited settings. During this exercise the European Society of Intensive Care Medicine’s and the Society of Critical Care Medicine’s Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) were published [2]. For the purposes of this article, where published studies have used former definitions of severe sepsis and septic shock to characterize patients, these have been left as originally published. For further clarification, we refer readers to the SSC guidelines and the article in this series examining sepsis recognition [3, 4]. Resource-limited settings were defined as those within low- or middle-income countries according to the World Bank [5] or described as “resource-limited” or “developing countries” by authors of the referenced studies. A flowchart summarizing the approach to the management of patients with sepsis or septic shock in resource-limited setting is provided in Fig. 8.1.
8.2 Factors Guiding the Choice of Empiric Antibiotic Choice in Sepsis and Septic Shock in Resource-Limited Settings
Hospital- and especially ICU-related infections are more likely to be caused by multidrug-resistant organisms, and previous antibiotic use is a risk factor for antibiotic resistance. Misdirected initial antibiotic therapy is associated with poor outcome [6, 7], but there is a paucity of epidemiological data in most resource-limited settings. The aim of empirical antibiotic therapy is to treat the causative pathogen in the septic patient before definitive microbiological results are available. General principles guiding the choice of initial empirical antibiotic therapy apply to both resource-rich and resource-limited settings [8, 9] and should take into consideration the pathogens and resistance patterns most likely to be encountered. This will depend on the suspected site and focus of the infection as well as healthcare setting and geographical location. Increasing evidence in both resource-rich settings and resource-limited settings shows that inappropriate initial antibiotics are associated with worse outcome [10].
Specific issues to consider in resource-limited settings include the different causative microorganisms in these often tropical countries, sparse epidemiological data because of limited microbiological laboratory capacity, and a greater degree of antimicrobial resistance, driven by poor stewardship especially in the private health and agricultural sectors. In some settings the range of available antibiotics may be reduced, and, compared to resource-rich settings, cost of treatment plays a larger role in the choice of the empirical drug as antibiotic costs are often disproportionately high compared to other therapies [11].
We found only three studies from resource-limited settings that specifically examined the causative organisms of severe sepsis and septic shock (using previous SSC definitions [12]) [9, 13, 14]. We therefore included other studies describing causes of sepsis in resource-limited settings, which were thought representative of potential pathogens encountered. The collected evidence is presented below.
8.2.1 Bacterial Pathogens
A retrospective study from a tertiary referral hospital in Turkey described pathogens and likely sources of infection from all cases of sepsis, including patients with severe sepsis and septic shock, between 2002 and 2003. Gram-negative bacteria, particularly Klebsiella spp. and Escherichia coli, were the most commonly isolated organisms from blood cultures (27 out of 41 isolates) and E. coli from urine culture (14 out of 63 samples). The respiratory tract was most frequently identified as the likely source of sepsis [9]. Similar results were reported from a prospective study of severe sepsis and septic shock in ICU patients in Thailand conducted between 2004 and 2006. Out of 390 patients, 241 patients had microorganisms isolated from any site, and 106 had positive blood cultures [14]. The main pathogens were Klebsiella pneumoniae (19.9%) and E. coli (14%). Again, the respiratory tract was the most common source of infection. In surgical ICUs in China, 381 cases of severe sepsis and septic shock in 10 units across 6 provinces were studied prospectively between 2004 and 2005. The majority (53.8%) of cases were caused by Gram-negative bacteria, but in a significant proportion of cases (28.3%), fungi were isolated. In this series, the commonest organisms isolated were Acinetobacter baumannii and Candida albicans, with the abdomen being the most frequent site of infection [13].
In addition to these studies, several other authors have reported the causes of bacteremia in resource-limited settings. Causative organisms varied according to location and between environments. Compared to many high-income settings, Gram-negative organisms were identified as particularly important causes of community-acquired bacteremia with distinct geographical differences, for example, non-typhoid Salmonella in sub-Saharan Africa, Salmonellae typhi and paratyphi in South and Southeast Asia, and Burkholderia pseudomallei in Southeast Asia [14,15,16]. The Gram-positive Streptococcus suis was reported to be a relatively common cause of sepsis in Southeast Asia [17].
A meta-analysis of community-acquired bloodstream infections across Africa involving 58,296 patients showed that in non-malarial bloodstream infections, the commonest isolate was Salmonella enterica (mainly non-typhoidal species), although among the five studies in adults that used mycobacterial culture techniques, Mycobacterium tuberculosis was the commonest pathogen isolated, in 33.8% of isolates.
Coexisting infection is an important factor in resource-limited settings. In the study above, HIV prevalence was 24% and was associated with increased likelihood of M. tuberculosis or non-typhoidal Salmonella bloodstream infection (OR 23.4 and 8.2, respectively) [15]. Malaria predisposes infected individuals to invasive bacterial infection, and in areas with high-malarial burden, it is a significant risk factor for bacteremia. In a case-control study of childhood bacteremia in Kenya, underlying malaria occurred in 62% of cases of bacteremia [18]. Secondary invasive bacterial infection is also a common complication of late-stage visceral leishmaniasis but is also associated with geographical variation. In one series of sepsis associated with visceral leishmaniasis in Ethiopia, 69% of cases were due to Staphylococcus aureus in contrast to elsewhere in Africa where Gram-negative bacteria were more commonly reported [15, 19].
The distinction between community- and healthcare-associated infection is, as expected, also an important determinant of the predicted causative organism. In the study from Turkey described above [9], blood culture isolates from community-acquired infection were more likely to be Gram-positive organisms (56% cases), whereas Gram-negative organisms accounted for 80% of cases of hospital-acquired isolates. In a study of bloodstream infections in South Africa [20], non-fermenting Gram-negative bacteria and Enterobacteriaceae were the most commonly isolated organisms from hospital-acquired bloodstream infections, whereas Gram-positive bacteria were most common in community-associated infections. Within the healthcare environment, A. baumannii was almost exclusively associated with ICU infection, but S. aureus, E. coli, and K. pneumoniae were associated with infections from other healthcare settings. Similar differences were shown in the prospective studies in Thailand and China described above [13, 14].
8.2.2 Antimicrobial Resistance
In a review of 83 studies examining antibiotic susceptibility of bacteria causing infections in sub-Saharan Africa and Asia, the authors concluded that only limited data were available to guide antibiotic treatment which show considerable variation in resistance patterns, both regionally and locally [21].
In the study from South Africa, described above, all community isolates of S. aureus were cloxacillin-sensitive compared to only 52% of hospital isolates. Increased antibiotic resistance was also noted in hospital isolates of Enterobacteriaceae compared to community isolates. Similarly, in 98 patients with S. aureus bloodstream infections in Thailand, community isolates were all methicillin-sensitive. Methicillin-resistant S. aureus (MRSA) was only associated with hospital-associated infection, particularly in ICU [22]. However, in a different series of Thai ICU patients with severe sepsis and septic shock due to respiratory infection, 22% community-acquired S. aureus infections were found to be methicillin-resistant [14]. Across 55 ICUs in 8 developing settings, 84% of S. aureus intravascular device-associated nosocomial infections were due to MRSA [23]. In a review of S. aureus epidemiology across Asia, hospital-acquired MRSA rates in general clinical samples collected between 1993 and 2011 were usually in excess of 20% (Vietnam, Thailand, Indonesia, Malaysia, China) and in some instances over 80% (India, Sri Lanka) [24]. In samples from community-acquired infection, MRSA rates were also variable, ranging from 3.2% (Malaysia 2009) to 39% (Sri Lanka 2004–2006) [24]. Most studies were laboratory-based surveillance studies lacking clinical data, and many of the community isolates were from superficial skin infections; thus, the relationship to organisms causing sepsis and septic shock was not clear.
Levels of Gram-negative bacterial resistance in resource-limited settings are often high and increasing, particularly in Asia, but there remain significant geographical variations [25, 26]. Extended-spectrum beta-lactamase (ESBL)-producing E. coli were reported in 9% of E. coli isolates from blood cultures in Laos between 2004 and 2009 [27]. In Cambodia between 2007 and 2010, ESBL rates were 49% in Enterobacteriaceae causing bloodstream infections in adults (mostly E. coli) [28]. 2008 data showed rates of ESBL-producing bacteria causing significant abdominal infections to be 2.9% in Malaysia compared to 59% and 61% in China and India, respectively [25]. More recently, nosocomial-acquired ESBL rates above 80% in India and more than 60% in China have been reported [29]. Between 2011 and 2012, 51.6% of ICU patients with bacterial sepsis in Mongolia were infected by at least one resistant bacterium, the majority of which were Gram-negative organisms [30].
In Asia and the Middle East, increased carbapenem use due to high-ESBL rates has resulted in the appearance of carbapenem resistance. While community-acquired infection data are limited, data from hospitals show that carbapenem-resistant organisms causing hospital-acquired infection are an increasing concern. In Asia K. pneumoniae carbapenemase (KPC)-related resistance was first noted in China in 2004. New Delhi metallo-β-lactamase-1 (NDM-1)-associated resistance was first reported in 2008 in a patient initially treated in India [26]. In India data indicate that 5–8% of hospital-related Enterobacteriaceae infections are carbapenem-resistant organisms [31]. In one neonatal intensive care unit in Pakistan, rates of imipenem-resistant K. pneumoniae causing late-onset sepsis increased from 0% to 72% of isolates over a 2-year period between 2009 and 2011 [32].
The situation in Africa has been described in a recent systematic review [33]. This describes a recent rapid emergence of carbapenem resistance throughout the region, although data are more limited. Of note is that even in countries without access to carbapenems, resistance has still emerged due to use of other antibiotic classes, as shown by the emergence of OXA-23 carbapenemase-resistant A. baumannii in Madagascar [34].
Several authors examined risk factors for antimicrobial resistance in resource-limited settings. A study of patients with Klebsiella spp. and E. coli bloodstream infections in India identified previous antibiotic use and transfer from other healthcare settings as risk factors for ESBL production [35]. In patients with febrile neutropenia in Lebanon, previous broad-spectrum antibiotic use was a risk factor for bacteremia with multidrug-resistant organisms [36]. Previous use of carbapenems was found to be the sole risk factor for adult patients with pan-resistant Pseudomonas aeruginosa bacteremia in Brazil [37].
8.2.3 Appropriateness of Antibiotic Choices
Two studies [6, 7] assessed the impact of inappropriate antibiotic use on outcome. In a single-center study in Brazil [6], prescription of appropriate empiric antibiotics was associated with survival benefit (odds ratio (OR) for death = 0.536 (95%) confidence interval [0.314–0.916]; p = 0.023). In a study of nosocomial infections in Thailand comparing combination therapy to monotherapy, combination therapy was more successful, in part due to increasing the chances of the bacteria being susceptible to the antibiotics [7].
8.2.4 Costs
Since antibiotic therapy is usually paid out of pocket by the patient or their relatives, cost is an important factor guiding antibiotic choice. For many antibiotics, generic products are available at a much lower price; however, the quality of these drugs is not always guaranteed [38]. In a study in India where ciprofloxacin, artesunate, and rifampicin were purchased from 100 different outlets, 43% samples fell below the 90% of stated content [39]. A review of published and unpublished studies of antimalarial drugs across sites in Southeast Asia and Africa showed 35% of samples failed chemical analysis [40]. In a systematic review of 66 studies of substandard pharmaceuticals (mainly antibiotics) conducted in Africa and Southeast Asia, 91% of studies found products to be substandard, and 44% showed evidence of counterfeiting [38].
8.2.5 Availability, Feasibility, Affordability, and Safety
There are significant differences in likely pathogenic organisms in resource-limited settings compared to resource-rich settings but also a high degree of variation between and within resource-limited settings. Hospital- and particularly ICU-related infections are more likely to be caused by multidrug-resistant organisms, and previous antibiotic use is a significant risk factor for resistance. Inappropriate antibiotic treatment is associated with worse outcome.
Ideally local epidemiological data should be used when choosing empiric therapy as large variations exist within regions. Establishment of well-chosen sentinel sites for monitoring of prevailing pathogens and their resistance patterns is suggested. The choice of empiric treatment is evidently dependent on the common causative pathogens and the resistance patterns of that area or hospital. Examples for community-acquired infections include Northeast Thailand, where 20% of sepsis is caused by B. pseudomallei, and therefore ceftazidime or a carbapenem should be included. In areas in Asia where scrub typhus is a common cause of severe fever and sepsis, doxycycline should be added to the empirical antibiotic regimen. Local resistance patterns should inform whether in areas with a high incidence of S. typhi bacteremia, fluoroquinolones are still usable. For hospital-acquired infections, examples include the current concerning spread beyond India of carbapenemase-producing Gram-negative bacteria. A policy used in some hospitals is to avoid carbapenems as empirical treatment when prevalence increases above 20% of Gram-negative bacteria. However, in most resource-limited settings, there is limited microbiological data to guide therapy, and the microbiological laboratory capacity of most resource-limited settings is unlikely to improve soon.
Based on the presented evidence, the following recommendations were derived. As poor outcome is associated with inappropriate initial antibiotic therapy, we recommend that empirical antibiotic therapy should cover all expected pathogens and likely resistance patterns (1C) based on locally acquired epidemiological data, as large regional variations exist (ungraded). We recognize that in settings with a limited range of antibiotics, this may be challenging. We suggest that research groups in collaboration with stakeholders provide microbiological data from sentinel sites throughout resource-limited settings to guide empirical antibiotic treatment (ungraded) (Table 8.1).
8.3 Timing of Antibiotic Treatment
Rapid elimination of causative microorganisms should help to prevent further pathological injury in severe sepsis and septic shock. Several, mainly retrospective, studies from resource-rich settings have shown an association between delay in antibiotic administration and worse outcome in sepsis and septic shock [41,42,43]. However, retrospective designs and the confounding effects of variable fluid resuscitation and assessment of appropriateness of antibiotics mean that interpretation of results is complex. A recent meta-analysis examining both prospective and retrospective studies failed to show significant benefit of antibiotic administration within 3 h of emergency department triage or 1 h of shock recognition [41]. Against a background of increasingly rapid antibiotic administration, recent discussion has focused on whether delaying treatment to ensure appropriate antibiotics are administered is beneficial.
In resource-limited settings, it may be more difficult to administer appropriate antibiotics within the first hour of sepsis recognition as limited staff have to prioritize multiple tasks. The subgroup members therefore wanted to consider whether antibiotic administration within the first hour was an important and feasible goal in resource-limited settings.
Reviewing the literature, we identified two studies involving patients from mixed-resource settings and three studies from resource-limited settings. A retrospective study included patients from both high- and middle-income countries (total 17,990 patients, with approximately 12% from South American ICUs) and examined the time from sepsis recognition to antibiotics in patients with severe sepsis and septic shock [44]. After adjustment for sepsis severity, geographical location, and admission source of sepsis, delay in antibiotic administration at hourly intervals up to 6 h was associated with increased mortality for both severe sepsis and septic shock.
A survey of SSC resuscitation and management bundle compliance across 150 ICUs in Asia (approximately 56% patients from resource-limited settings) reported that antibiotic administration <1 h (or <3 h from emergency department arrival) was associated with significant survival benefit (OR for death 0.76 [0.58–0.99]; p = 0.02) [45].
Another study compared outcome and timing of antibiotic therapy in a single center in Brazil [6]. This retrospective study of 1279 patients with severe sepsis and septic shock, where mean time to antibiotics was 2.5 h, showed broad-spectrum antibiotic administration within 1 h was not associated with improved outcome compared to >1 h in multivariate analysis (OR for death 0.77 [0.59–1.01]; p = 0.06). In the 358 patients with positive blood cultures, appropriate antibiotic therapy was an independent predictor of mortality, whereas antibiotic administration <1 h was not.
A prospective cohort study of 145 patients with sepsis in Iran evaluated the effect on outcome of time from arrival in the emergency department to administration of antibiotics and showed a significant relationship between mortality and hourly delay in antibiotic administration up to >2 h. Subgroup analysis showed that this relationship was strongest in patients with APACHE II scores >20 [46].
In a study of 104 patients with typhoidal ileal perforation in Tanzania, inadequate antibiotic therapy prior to admission was associated with increased mortality (OR 3.1 [1.45–7.86]; p = 0.006) [47].
8.3.1 Availability, Feasibility, and Affordability
The SSC states that the administration of appropriate antibiotics within an hour of severe sepsis or shock recognition is a goal rather than standard of care. Observational data from resource-limited settings suggests that in many settings, the administration of antibiotics to the majority of patients within 1 h is feasible, for example, in China 98% of patients received antibiotics within 1 h, and in Brazil 68% patients received the antibiotics within 1 h of sepsis recognition [48]. In Iran, 18% received antibiotics within 1 h of arrival at the emergency department, but 74% were treated within 2 h [46]. We found weak evidence from resource-limited settings suggesting timely administration of antibiotics is beneficial. Nevertheless, in one study that evaluated timely administration and appropriateness of antibiotics, appropriate initial antibiotic therapy was the only independent predictor of outcome [6]. Based on the provided evidence, we recommend appropriate antibiotics should be given within the first hour following recognition of sepsis and septic shock (1C).
8.4 Importance of Blood Cultures Before Initiation of Empirical Antibiotic Treatment
Definitive identification and sensitivity testing of causative organisms of sepsis and septic shock allow de-escalation of treatment and ensure that appropriate antibiotic therapy is given. Currently it is recommended that, if this does not delay administration of antibiotics, two sets of blood cultures should be taken, one of which should be drawn through an intravascular device (if one has been present for more than 48 h), as this may help determine the origin of the infection. Obtaining blood cultures is strongly recommended to aid microbiological identification, also in resource-limited settings [4]. However, setting specific evidence on the added value of blood cultures on patient outcome is important, since in resource-limited settings laboratory access may be restricted and additional costs of tests must be justified. Cultures taken before antibiotic administration are more sensitive, but in settings with limited numbers of staff, the benefits must be weighed against time diverted from performing other initial resuscitation measures.
In the literature search, we identified two relevant studies from resource-limited settings and one from mixed-resource settings assessing blood cultures and outcome in severe sepsis or septic shock. A prospective study from China in 212 patients with severe sepsis or septic shock and community-acquired pneumonia reported that obtaining blood cultures before antibiotic treatment was associated with a reduced risk of mortality (OR for death 0.46, [0.211–0.997]; p = 0.039) [48].
A large retrospective study from Brazil of 1279 patients with severe sepsis and septic shock reported that taking blood cultures was associated with lower mortality (OR 0.38, 95% CI [0.265–0.546]; p < 0.001), whereas antibiotic administration within 1 h was not [6].
A study examining compliance with SSC bundles in Asian ICUs found that taking of blood cultures before antibiotics was associated with improved survival (OR death 0.72, [0.54–0.95]; p = 0.02) [45].
8.4.1 Availability, Feasibility, and Affordability
We found evidence from resource-limited settings that taking blood cultures was associated with improved outcome in sepsis and septic shock, although observational data cannot exclude confounding by better prognosis due to a less cryptic presentation of sepsis as an explanation for this finding. Definitive microbiological diagnosis allows the administration of appropriate antibiotics. A prospective survey of 72 adults with severe sepsis or septic shock with S. aureus bacteremia in Thailand reported 78% patients were empirically treated with appropriate antibiotics, but after culture result, 98% were given effective antibiotic therapy [49]. In addition, as discussed above, by detecting infections such as tuberculosis or melioidosis, the necessary treatment to prevent relapse or resistance can be given.
In resource-limited settings, there may be no facilities for blood culture analysis. In other locations where there is some laboratory capability, manual methods using self-made broth and manual inoculation of plates are an alternative to more expensive-automated culture systems. Delay in sample processing may occur due to distance from laboratory facilities or lack of trained staff. There is no definitive data to guide temporary storage, but if it is not possible to process samples straightaway, then bottles should be stored at ambient temperature, not refrigerated (expert opinion).
We could not identify studies addressing the economic aspects of costs of implementation of microbiological capacity, versus the gains in disability-adjusted life years (DALYs), or restriction of antibiotic use. We also did not find any evidence to quantify the additional benefit of taking a second set of blood cultures.
Based on the presented evidence, we recommend that blood cultures should be taken before the administration of antibiotics in locations where this is possible (1B). Ideally two sets of blood cultures should be obtained. It is realized that in many hospitals, routine blood culture is unfeasible, but a recommendation of expanding microbiological laboratory capacity is beyond the scope of this article.
8.5 Source Control
Source control is generally understood as including “all physical measures taken to control a focus and modify factors in the infectious milieu that promote microbiological growth or impair host antimicrobial defenses” [50]. Initial identification of a focus of infection requires a combination of clinical examination and specialist investigations. Source control methods should have maximum efficacy and cause minimum physiological upset. In resource-rich settings, inadequate source control has been shown to be an independent predictor of mortality in patients with sepsis or septic shock [51,52,53]. However in some situations, e.g., peripancreatic necrosis, there is moderate evidence suggesting delay in surgical source control is more appropriate [54].
In resource-limited settings, source control may be affected by the different infections encountered as well as limited access to specific diagnostic or surgical modalities. When considering source control, the subgroup wished to particularly focus on evidence for conditions commonly encountered in resource-limited settings and not considered in current guidelines.
We searched the literature and identified seven papers from resource-limited settings regarding source control. We also included one study from a resource-rich setting that was specifically concerned with an important cause of sepsis and septic shock in resource-limited countries. Six of the studies concerned source identification. Three studies reported the use of chest radiography and ultrasound in source diagnosis of typhoid or tuberculoid gastrointestinal perforations, reporting the presence of pneumoperitoneum in 70–75% of cases on chest radiography and fluid collections in 70–97% of cases on abdominal ultrasound [47, 55,56,57]. In a retrospective Australian study of 78 cases of prostatic abscesses due to melioidosis, 85% of cases were detectable with ultrasound compared to a “gold standard” of computerized tomography (CT) [58]. In a prospective cohort study of 230 patients in Thailand, ultrasonography identified abdominal abscesses in 33% of patients (and 38% or those with positive blood cultures) although no comparison was made with CT [59].
Three studies examined timing of source control in typhoid gastrointestinal perforation. An early series in India reported an increased mortality rate associated with delay in surgery in a series of 100 consecutive cases of typhoidal ileac perforation [60]. Another study from India reported a nonsignificant reduction in mortality (19 vs. 32%) in those whose operation was performed within 48 h of perforation [61]. More recently, a retrospective case series in Tanzania reported that delay in surgery over 24 h was associated with higher mortality (24 vs. 14%) [47].
With respect to melioidosis, in the Australian series of prostatic abscesses, it was noted that only small abscesses (<1 cm) resolved with antibiotic therapy alone and drainage (either ultrasound- or CT-guided) was required in larger abscesses. Pus drained from the majority of abscesses showed viable bacteria despite supervised adequate and prolonged antibiotic therapy [58].
8.5.1 Availability, Affordability, and Feasibility
Removing the focus of infection in the septic patient is equally important in resource-limited settings as in high-income settings. However, source control and identification are challenging in resource-limited settings; poor investigative facilities limit diagnostic capability, and less invasive measures for control often require expensive equipment and expertise. Some conditions such as mycotic aneurysms in non-typhoidal salmonellae infections are reported to be invariably lethal without surgical resection [62]. Current SSC guidelines recommend source control within 12 h except in the case of pancreatic necrosis when delay appears to be beneficial. We found weak evidence from resource-limited settings to support timely source control (<24 h) in typhoidal perforations, although no studies specifically examined control <12 h. In view of the lack of evidence for other situations, we felt unable to apply a graded recommendation. There was no evidence of situations where delay in source control seemed beneficial.
Ultrasound and X-ray are the most available and inexpensive investigations to aid the anatomical infection site, and we found low-grade evidence of both investigations showing reasonable sensitivity in abdominal perforation and melioidosis. Radiological examination was available in 86% of patients with severe sepsis and septic shock associated with S. aureus bacteremia in Thailand [49], and in 15 out of 46 cases where an anatomical site of infection was identified, appropriate source control procedures occurred, although in five further cases, the patient was deemed unfit for the appropriate surgical procedure.
Based on the presented evidence, we suggest the infection source control is carried out within 12 h of admission to hospital (ungraded) except in the specific case of pancreatic necrosis. Radiography and ultrasound are good first-line imaging techniques (ungraded).
8.6 Use of Combination Antibiotic Therapy in Specific Situations
Although some data exist supporting combination therapy in all patients with sepsis or septic shock, particularly those with most severe disease [63,64,65,66], there are few randomized controlled trials examining this. Lack of good evidence and concerns over antimicrobial resistance and toxicity has meant that monotherapy is recommended in most instances. Notable exceptions are neutropenia and sepsis with Gram-negative multidrug-resistant bacteria or S. pneumoniae bacteremia. If combination therapy is used empirically, it is recommended that it is used for less than 3–5 days. Although there are often biologically plausible mechanisms of additive or synergistic action, success of combination therapy also appears to be related to the increased likelihood of the causative bacteria being susceptible to at least one antibiotic [67, 68]. In addition to multidrug-resistant infections, the subgroup wanted to assess evidence for benefit or combination therapy in specific diseases common to resource-limited settings.
We identified a total of nine relevant studies examining combination antibiotic therapy in patients in resource-limited settings: one meta-analysis of two randomized controlled trials in melioidosis, five studies examining combination therapy in multidrug-resistant (MDR) or extensively drug-resistant (XDR) A. baumannii infections (only one of which specifically addressed infections in patients with severe sepsis or septic shock), and one study of febrile neutropenia.
In a meta-analysis of two randomized clinical trials of additional cotrimoxazole to ceftazidime in the early phase of acute severe melioidosis in Thailand involving a total of 449 patients, no difference in mortality or recurrent disease was noted between the two treatment groups [69, 70]. Similarly, no difference was noted with combination therapy in the later eradication phase of treatment [71].
A retrospective study in Turkey investigated single agent (colistin) versus combination therapy (colistin/sulbactam) in 89 ICU patients with MDR A. baumannii ventilator-associated pneumonia, 80% of whom had severe sepsis or septic shock. After adjustment for APACHE II score, there was no difference in the mortality rate between groups. Clinical and bacteriological responses were higher in the combination group although not statistically significant [72].
A retrospective analysis of 110 nosocomial infections due to A. baumannii associated with systemic inflammatory response syndrome in Thailand found that there was improved clinical cure rate and outcome in patients treated with combination therapy and that combination therapy increased the chance of appropriate antibiotics [7].
A multicenter retrospective study of 214 patients in Turkey with XDR A. baumannii bloodstream infections found improved mortality and clinical and microbiological cure when colistin was used in combination compared to colistin alone [73].
Two hospital-wide studies of resistant A. baumannii isolates were identified: one of colistin-only susceptible strains and the other of multidrug-resistant strains (49 and 51 patients, respectively) reported to have nonsignificant reductions in mortality with combination treatment [74, 75].
One study compared combination therapy in 151 cases of febrile neutropenia in Turkey, analyzing response rates between non-carbapenem monotherapy or combination therapy and combination carbapenem therapy in 88 adults [76]. Similar rates of response were seen in all patients.
8.6.1 Availability, Affordability, and Feasibility
In many resource-limited settings, community infections are more likely to be caused by resistant organisms than in resource-rich settings [77]. Prior antibiotic use is known to affect the gut microflora which is the main source of pathogens for ICU-acquired infection; thus widespread unregulated community use of antibiotics is likely to lead to increased resistance, and this is reflected in the resistance profiles of organisms causing healthcare-associated infection in resource-limited settings [30, 78,79,80]. Limitation of laboratory and diagnostic facilities prevents definitive diagnosis or de-escalation of antibiotic treatment, and empiric therapy may remain the only therapeutic option. As antibiotics are often the most significant expenditure for patients with sepsis and septic shock in resource-limited settings, prolonged courses of combination therapy significantly increases healthcare costs [81]. A consensus paper from resource-rich settings concluded that the evidence is insufficient to warrant a general recommendation for combination antibiotic treatment [8], and we did not find any studies examining the benefit of combination therapy in situations where currently only monotherapy is advised in the current SSC guidelines. In studies of MDR or XDR A. baumannii infection, combination therapy appeared to be beneficial. In cases of XDR bacterial infection, some authors have argued that monotherapy should be avoided due to the risk of developing resistance. In addition combination therapy may be more efficient at killing bacteria and thus enable shorter courses of antibiotic therapy [67].
In the case of melioidosis, no evidence was found that initial combination treatment was superior although some have argued that combination therapy should be used for patients with deep-seated abscesses and focuses of infection [82].
Based on this we suggest that where the possibility of multidrug resistance is high, combination antibiotics should be used (2D). Choice of combination therapy should be guided by local epidemiology and known effective combinations (ungraded). Antimicrobial therapy should be de-escalated whenever possible (ungraded). We recognize that without microbiological information, de-escalation is difficult.
8.7 Use of Procalcitonin (PCT), C-Reactive Protein (CRP), or Other Biomarkers for De-escalation of Antibiotics
Reducing global antibiotic use is a major part of antibiotic stewardship programs aiming to reduce global spread of antimicrobial resistance. De-escalating treatment to narrow-spectrum agents and reducing the duration of antibiotic treatment are key elements in this approach. Since facilities for blood culture are often absent, the clinician often lacks guidance to de-escalate empirical-started antibiotic treatment. Semiquantitative CRP or PCT point-of-care tests have become increasingly available and could be a potential tool to guide de-escalation.
There are limited randomized controlled trial data concerning outcome following de-escalation of empiric antibiotic therapy [83]. There is more evidence on the use of biomarkers to de-escalate or terminate antibiotic therapy in severe sepsis and septic shock, but this comes mainly from resource-rich settings in Europe. The most widely available biomarkers studied for this purpose are PCT and CRP. PCT is generally more specific for bacterial sepsis but costlier compared to CRP. Results of several meta-analyses involving up to seven randomized controlled trials (total 1075 patients) have shown PCT can be used safely to reduce length of antibiotic treatment and may be cost-effective [84,85,86,87,88,89].
In resource-limited countries with high levels of antimicrobial resistance, strategies to reduce use of broad-spectrum agents are important. While we specifically searched for evidence of biomarkers in resource-limited settings, we also included studies from resource-rich settings that covered other biomarkers that would be potentially useful in resource-limited settings.
We identified two studies from resource-limited countries and also included one recent study from a resource-rich country on procalcitonin and one on fever course and white blood cell counts to guide antibiotic therapy [90] [91].
Eighty-one patients with a proven bacterial infection and sepsis, severe sepsis, or septic shock admitted to an ICU in Brazil were randomized to PCT-guided treatment or normal treatment. In the 51 patients per protocol analysis, median duration of antibiotic therapy was significantly lower in the PCT group, which was not at the expense of a worse treatment outcome. However, intention-to-treat analysis showed no difference. Reduced antibiotic costs led to significant cost savings in the PCT group, offsetting the increased cost of testing [91]. CRP levels were also measured in the PCT group, but these remained elevated until the end of antibiotic treatment.
A randomized clinical trial in China studied the use of PCT-guided initiation and termination of antibiotic therapy in 35 patients with severe acute pancreatitis compared to 36 patients who received a standard 14-day course of prophylactic antibiotics [92]. Average duration of antibiotic use, length of hospitalization, and costs of hospitalization were shorter in the PCT-guided group.
A more recent large multicenter randomized clinical trial from the Netherlands in 1575 critically ill patients showed that an antibiotic-stopping rule based on a reduction in plasma procalcitonin concentrations of >80% from its peak value (or an absolute decrease below 0·5 μg/L) resulted in a reduction of duration of antibiotic treatment and was associated with a significant decrease in mortality [93].
In a multicenter randomized clinical trial of 518 patients with complicated abdominal sepsis and adequate source control in the USA, patients were randomized to a white blood count/fever-guided cessation of antibiotics or a fixed 4-day course. In the white blood count/fever-guided group, antibiotic duration was significantly longer. There were no differences in outcome [90].
8.7.1 Availability, Affordability, and Feasibility
We found evidence from resource-limited settings that PCT-guided antibiotic policies can be cost-effective as cost of tests is offset by antibiotic cost savings [91, 92]. Two studies from resource-limited settings have shown benefit of PCT guidance in antibiotic de-escalation in sepsis and septic shock [91, 94]. CRP could be used as a cheaper alternative, but this will need additional evaluation. We did not find evidence of low-cost alternatives, including fever or white blood cell counts, being beneficial when compared to short-fixed durations of therapy.
Based on this we conclude that the use of biomarkers, in particular PCT and CRP, for de-escalation of antimicrobial therapy needs further study in resource-limited settings before a recommendation can be made.
8.8 Outstanding Questions for Future Research
In addition to reviewing the literature concerning the above questions, we also discussed areas currently lacking in evidence in resource-limited settings and where resource-rich country evidence may not be applicable.
Reducing duration of antibiotic use can reduce side effects, treatment costs, and antimicrobial resistance. Studies in resource-rich settings have shown that in general shortened courses of antibiotics do not appear to be harmful and may be associated with reduced antimicrobial resistance [66, 95]. Others, however, have argued that longer durations of treatment may be required in cases of immune deficiency, inadequate source control, MDR and XDR infections, poor tissue penetration of drugs, the presence of foreign materials, or inadequate initial antibiotics [95, 96]. Although reduced duration of antibiotic treatment would be particularly attractive in resource-limited settings, it remains unclear whether this can be safely adopted in places where definitive microbiological diagnosis is challenging and when there are high-prevalence rates of non-fermenting Gram-negative bacteria.
The recommendations for prevention of nosocomial infections in the current SSC guideline include a Grade 2B recommendation in favor of chlorhexidine mouthwash and selective digestive decontamination. These measures have been used in resource-rich settings [97], and the subgroup initially intended to discuss their use in resource-limited settings. However, they are yet to be tested in resource-limited settings, and as there are important differences in epidemiology of nosocomial infection and capacity for infection control, the subgroup felt that applying evidence from resource-rich settings was not appropriate. The efficacy and safety of these interventions in resource-limited settings therefore require further study.
Finally, the advent of new technologies with the ability to type and characterize microorganisms without the need for conventional culture techniques may negate the requirement for highly specialized microbiology staff and facilities. There is currently one ongoing study of their use in a resource-limited setting. However, careful cost-benefit analysis is required. These methods could eventually contribute significantly to improved management of patients with sepsis and septic shock as well as antibiotic stewardship programs.
References
Dondorp AM, Iyer SS, Schultz MJ. Critical care in resource-restricted settings. JAMA. 2016;315:753–4.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard G, Chiche JD, Coppersmith CM, Hitchkiss RS, Rubenfeld GD, Poll TVD, J-l V, Angus DC. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315:801–10.
Campaign SS surviving sepsis campaign responds to sepsis-3. In: Book surviving sepsis campaign responds to sepsis-3. http://www.survivingsepsis.org/SiteCollectionDocuments/SSC-Statements-Sepsis-Definitions-3-2016.pdf.
Kwizera A, Festic E, Dünser MW. What’s new in sepsis recognition in resource-limited settings? Intensive Care Med. 2016;42(12):2030–3.
World B country and lending groups. In: Book country and lending groups. http://data.worldbank.org/about/country-and-lending-groups.
Yokota PK, Marra AR, Martino MD, Victor ES, Durao MS, Edmond MB, dos Santos OF. Impact of appropriate antimicrobial therapy for patients with severe sepsis and septic shock—a quality improvement study. PLoS One. 2014;9:e104475.
Santimaleeworagun W, Wongpoowarak P, Chayakul P, Pattharachayakul S, Tansakul P, Garey KW. Clinical outcomes of patients infected with carbapenem-resistant acinetobacter baumannii treated with single or combination antibiotic therapy. J Med Assoc Thail. 2011;94:863–70.
Bochud P-Y, Bonten M, Marchetti O, Calandra T. Antimicrobial therapy for patients with severe sepsis and septic shock: an evidence-based review. Crit Care Med. 2004;32:S495–510.
Tanriover MD, Guven GS, Sen D, Unal S, Uzun O. Epidemiology and outcome of sepsis in a tertiary-care hospital in a developing country. Epidemiol Infect. 2006;134:315–22.
Hranjec T, Rosenberger LH, Swenson B, Metzger R, Flohr TR, Politano AD, Riccio LM, Popovsky KA, Sawyer RG. Aggressive versus conservative initiation of antimicrobial treatment in critically ill surgical patients with suspected intensive-care-unit-acquired infection: a quasi-experimental, before and after observational cohort study. Lancet Infect Dis. 2012;12:774–80.
Fadare JO, Adeoti AO, Aina F, Solomon OA, Ijalana JO. The influence of health insurance scheme on the drug prescribing pattern in a Nigerian tertiary healthcare facility. Niger Med J. 2015;56:344–8.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R, Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637.
Cheng B, Xie G, Yao S, Wu X, Guo Q, Gu M, Fang Q, Xu Q, Wang D, Jin Y, Yuan S, Wang J, Du Z, Sun Y, Fang X. Epidemiology of severe sepsis in critically ill surgical patients in ten university hospitals in China. Crit Care Med. 2007;35:2538–46.
Khwannimit B, Bhurayanontachai R. The epidemiology of, and risk factors for, mortality from severe sepsis and septic shock in a tertiary-care university hospital setting. Epidemiol Infect. 2009;137:1333–41.
Reddy EA, Shaw AV, Crump JA. Community-acquired bloodstream infections in Africa : a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:417–32.
Murdoch DR. Microbiological patterns in sepsis: what happened in the last 20 years? Int J Antimicrob Agents. 2009;34(Suppl 4):S5–8.
Goyette-Desjardins G, Auger J-P, Xu J, Segura M, Gottschalk M. Streptococcus suis, an important pig pathogen and emerging zoonotic agent-an update on the worldwide distribution based on serotyping and sequence typing. Emerg Microbes Infect. 2014;3:e45.
Scott JAG, Berkley JA, Mwangi I, Ochola L, Uyoga S, MacHaria A, Ndila C, Lowe BS, Mwarumba S, Bauni E, Marsh K, Williams TN. Relation between falciparum malaria and bacteraemia in Kenyan children: a population-based, case-control study and a longitudinal study. Lancet. 2011;378:1316–23.
Endris M, Takele Y, Woldeyohannes D, Tiruneh M, Mohammed R, Moges F, Lynen L, Jacobs J, van Griensven J, Diro E. Bacterial sepsis in patients with visceral leishmaniasis in Northwest Ethiopia. Biomed Res Int. 2014;2014:361058.
McKay R, Bamford C. Community- versus healthcare-acquired bloodstream infections at Groote Schuur Hospital, Cape Town, South Africa. S Afr Med J. 2015;105:363.
Ashley EA, Lubell Y, White NJ, Turner P. Antimicrobial susceptibility of bacterial isolates from community acquired infections in Sub-Saharan Africa and Asian low and middle income countries. Trop Med Int Health. 2011;16:1167–79.
Nickerson EK, Hongsuwan M, Limmathurotsakul D, Wuthiekanun V, Shah KR, Srisomang P, Mahavanakul W, Wacharaprechasgul T, Fowler VG, West TE, Teerawatanasuk N, Becher H, White NJ, Chierakul W, Day NP, Peacock SJ. Staphylococcus aureus bacteraemia in a tropical setting: patient outcome and impact of antibiotic resistance. PLoS One. 2009;4:e4308.
Rosenthal VD, Maki DG, Salomao R, Moreno CA, Mehta Y, Higuera F, Cuellar LE, Arikan OA, Abouqal R, Leblebicioglu H. Device-associated nosocomial infections in 55 intensive care units of 8 developing countries. Ann Intern Med. 2006;145:582–91.
Chen CJ, Huang YC. New epidemiology of Staphylococcus aureus infection in Asia. Clin Microbiol Infect. 2014;20:605–23.
Hawkey PM. Multidrug-resistant Gram-negative bacteria: a product of globalization. J Hosp Infect. 2015;89:241–7.
Molton JS, Tambyah PA, Ang BSP, Ling ML, Fisher DA. The global spread of healthcare-associated multidrug-resistant bacteria: a perspective from Asia. Clin Infect Dis. 2013;56:1310–8.
Stoesser N, Crook DW, Moore CE, Phetsouvanh R, Chansamouth V, Newton PN, Jones N. Characteristics of CTX-M ESBL-producing Escherichia coli isolates from the lao people’s democratic republic, 2004-09. In: Book characteristics of CTX-M ESBL-producing Escherichia coli isolates from the lao people’s democratic republic, 2004-09. 2012.
Vlieghe ER, Huang TD, Phe T, Bogaerts P, Berhin C, De Smet B, Peetermans WE, Jacobs JA, Glupczynski Y. Prevalence and distribution of beta-lactamase coding genes in third-generation cephalosporin-resistant Enterobacteriaceae from bloodstream infections in Cambodia. Eur J Clin Microbiol Infect Dis. 2015;34:1223–9.
Livermore DM. Fourteen years in resistance. Int J Antimicrob Agents. 2012;39:283–94.
Bataar O, Khuderchuluun C, Lundeg G, Chimeddorj S, Brunauer A, Gradwohl-Matis I, Duenser MW. Rate and pattern of antibiotic resistance in microbiological cultures of sepsis patients in a low-middle-income country’s ICU. Middle East J Anesthesiol. 2013;22:293–300.
Deshpande P, Shetty A, Kapadia F, Hedge A, Somon R, Rodrigues C. New Delhi Metallo 1: have carbapenems met their doom? Clin Infect Dis. 2010;51:1222–3.
Saleem AF, Qamar FN, Shahzad H, Qadir M, Zaidi AKM. Trends in antibiotic susceptibility and incidence of late-onset Klebsiella pneumoniae neonatal sepsis over a six-year period in a neonatal intensive care unit in Karachi, Pakistan. Int J Infect Dis. 2013;17:e961–5.
Manenzhe RI, Zar HJ, Nicol MP, Kaba M. The spread of carbapenemase-producing bacteria in Africa: a systematic review. J Antimicrob Chemother. 2015;70:23–40.
Andriamanantena TS, Ratsima E, Rakotonirina HC, Randrianirina F, Ramparany L, Carod J-F, Richard V, Talarmin A. Dissemination of multidrug resistant Acinetobacter baumannii in various hospitals of Antananarivo Madagascar. Ann Clin Microbiol Antimicrob. 2010;9:17.
Nasa P, Juneja D, Singh O, Dang R, Singh A. An observational study on bloodstream extended-spectrum beta-lactamase infection in critical care unit: Incidence, risk factors and its impact on outcome. Eur J Intern Med. 2012;23:192–5.
Moghnieh R, Estaitieh N, Mugharbil A, Jisr T, Abdallah DI, Ziade F, Sinno L, Ibrahim A. Third generation cephalosporin resistant Enterobacteriaceae and multidrug resistant gram-negative bacteria causing bacteremia in febrile neutropenia adult cancer patients in Lebanon, broad spectrum antibiotics use as a major risk factor, and correlation with poor prognosis. Front Cell Infect Microbiol. 2015;5:1–9.
Tuon FF, Gortz LW, Rocha JL. Risk factors for pan-resistant Pseudomonas aeruginosa bacteremia and the adequacy of antibiotic therapy. Braz J Infect Dis. 2012;16:351–6.
Fahad A, Alghannam A, Aslanpour Z, Evans S, Schifano F. A systematic review of counterfeit and substandard medicines in field quality surveys. Integr Pharm Res Pract. 2014;3:71–88.
Seear M, Gandhi D, Carr R, Dayal A, Raghavan D, Sharma N. The need for better data about counterfeit drugs in developing countries: a proposed standard research methodology tested in Chennai, India. J Clin Pharm Ther. 2011;36:488–95.
Nayyar GML, Breman JG, Newton PN, Herrington J. Poor-quality antimalarial drugs in southeast Asia and sub-Saharan Africa. In: Book poor-quality antimalarial drugs in southeast Asia and sub-Saharan Africa. 2012. p. 488–496.
Sterling SA, Miller WR, Pryor J, Puskarich MA, Jones AE. The impact of timing of antibiotics on outcomes in severe sepsis and septic shock. Crit Care Med. 2015;43:1.
Garnacho-Montero J, Gutiérrez-Pizarraya A, Escoresca-Ortega A, Fernández-Delgado E, López-Sánchez JM. Adequate antibiotic therapy prior to ICU admission in patients with severe sepsis and septic shock reduces hospital mortality. Crit Care. 2015;19:302.
Cañas B, Jáuregui R, Ballesteros M, Leizaola O, González-Castro A, Castellanos-Ortega A. Effects of antibiotic administration delay and inadequacy upon the survival of septic shock patients. Med Intensiva. 2015;39(8):459–66.
Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP, Artigas A, Schorr C, Levy MM. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014;42:1749–55.
Phua J, Koh Y, Du B, Tang YQ, Divatia JV, Tan CC, Gomersall CD, Faruq MO, Shrestha BR, Gia Binh N, Arabi YM, Salahuddin N, Wahyuprajitno B, Tu ML, Wahab AY, Hameed AA, Nishimura M, Procyshyn M, Chan YH, MOSAICS Study Group. Management of severe sepsis in patients admitted to Asian intensive care units: prospective cohort study. BMJ. 2011;342:d3245.
Jalili M, Barzegari H, Pourtabatabaei N, Honarmand AR, Boreiri M, Mehrvarz A, Ahmadinejad Z. Effect of door-to-antibiotic time on mortality of patients with sepsis in emergency department: a prospective cohort study. Acta Med Iran. 2013;51:454–60.
Chalya PL, Mabula JB, Koy M, Kataraihya JB, Jaka H, Mshana SE, Mirambo M, McHembe MD, Giiti G, Gilyoma JM. Typhoid intestinal perforations at a University teaching hospital in Northwestern Tanzania: a surgical experience of 104 cases in a resource-limited setting. World J Emerg Surg. 2012;7:4–4.
Guo Q, Li HY, Li YM, Nong LB, Xu YD, He GQ, Liu XQ, Jiang M, Xiao ZI, Zhong NS. Compliance with severe sepsis bundles and its effect on patient outcomes of severe community-acquired pneumonia in a limited resources country. Arch Med Sci. 2014;10:970–8.
Mahavanakul W, Nickerson EK, Srisomang P, Teparrukkul P, Lorvinitnun P, Wongyingsinn M, Chierakul W, Hongsuwan M, West TE, Day NP, Limmathurotsakul D, Peacock SJ. Feasibility of modified surviving sepsis campaign guidelines in a resource-restricted setting based on a cohort study of severe S. aureus sepsis. PLoS One. 2012;7:e29858.
Marshall JC, Maier RV, Jimenez M, Dellinger EP. Source control in the management of severe sepsis and septic shock: an evidence-based review. Crit Care Med. 2004;32:S513–26.
Kollef M, Micek S, Hampton N, Doherty JA, Kumar A. Septic shock attributed to Candida infection: importance of empiric therapy and source control. Clin Infect Dis. 2012;54:1739–46.
Tellor B, Skrupky LP, Symons W, High E, Micek ST, Mazuski JE. Inadequate source control and inappropriate antibiotics are key determinants of mortality in patients with intra-abdominal sepsis and associated bacteremia. Surg Infect (Larchmt). 2015;16:1–9.
Bloos F, Thomas-Rüddel D, Rüddel H, Engel C, Schwarzkopf D, Marshall JC, Harbarth S, Simon P, Riessen R, Keh D, Dey K, Weiß M, Toussaint S, Schädler D, Weyland A, Ragaller M, Schwarzkopf K, Eiche J, Kuhnle G, Hoyer H, Hartog C, Kaisers U, Reinhart K. Impact of compliance with infection management guidelines on outcome in patients with severe sepsis: a prospective observational multi-center study. Crit Care. 2014;18:R42.
Marshall JC, Al Naqbi A. Principles of source control in the management of sepsis. Crit Care Nurs Clin North Am. 2011;23:99–114.
Ansari AG, Naqvi QS, Naqvi H, et al. Management of typhoid ilial perforation: a surgical experience of 44 cases. Gomal J Med Sci. 2009;7:27–8.
Patil V, Vijayakumar A, Ajitha MB, Kumar LS. Comparison between tube ileostomy and loop ileostomy as a diversion procedure. ISRN Surg. 2012;2012:547523.
Ugochukwu AI, Amu OC, Nzegwu MA. Ileal perforation due to typhoid fever—review of operative management and outcome in an urban centre in Nigeria. Int J Surg. 2013;11:218–22.
Morse LP, Moller CC, Harvey E, Ward L, Cheng AC, Carson PJ, Currie BJ. Prostatic abscess due to Burkholderia pseudomallei: 81 cases from a 19-year prospective melioidosis study. J Urol. 2009;182:542–7. discussion 547
Maude RR, Teerapon I, Ariyaprasert P, Maude R, Hongsuwan M, Yuentrakul P, Limmathurotsakul D, Koh G, Chaowagul W, Day NPJ, Peacocka SJ. Maude meliodosis thailand. Trans R Soc Trop Med Hyg. 2012;106:629–31.
Khanna A, Misra MK. Typhoid perforation of the gut. Postgrad Med J. 1984;60:523–5.
Sitaram V, Moses BV, Fenn AS, Khanduri P. Typhoid ileal perforations: a retrospective study. Ann R Coll Surg Engl. 1990;72:347–9.
Wang JH, Liu YC, Yen MY, Wang JH, Chen YS, Wann SR, Cheng DL. Mycotic aneurysm due to non-typhi salmonella : report of 16 cases. Clin Infect Dis. 1996;23:743–7.
Kumar A, Safdar N, Kethireddy S, Chateau D. A survival benefit of combination antibiotic therapy for serious infections associated with sepsis and septic shock is contingent only on the risk of death: a meta-analytic/meta-regression study. Crit Care Med. 2010;38:1651–64.
Díaz-Martín A, Martínez-González ML, Ferrer R, Ortiz-Leyba C, Piacentini E, Lopez-Pueyo MJ, Martín-Loeches I, Levy MM, Artigas A, Garnacho-Montero J. Antibiotic prescription patterns in the empiric therapy of severe sepsis: combination of antimicrobials with different mechanisms of action reduces mortality. Crit Care. 2012;16:R223.
Gattarello S. What is new in antibiotic therapy in community-acquired pneumonia? An evidence-based approach focusing on combined therapy. Curr Infect Dis Rep. 2015;17:45.
Barrett J, Edgeworth J, Wyncoll D. Shortening the course of antibiotic treatment in the intensive care unit. Expert Rev Anti-Infect Ther. 2015;13:463–71.
Baker S, Thieu Nga TV, Thi Loan H, Campbell JI, Le Minh V, Van Hao N, Trung Nghia HD, Vinh Phat V, Minh Yen L, Hien TT, Thi Khanh Nhu N, Thwaites L, Van Vinh Chau N, Huong Lan NP, Hoang Nhu TD, Thwaites G, Thanh Tam PT, Thompson C, Tuyen HT, Parry CM. In vitro activity of colistin in antimicrobial combination against carbapenem-resistant Acinetobacter baumannii isolated from patients with ventilator-associated pneumonia in Vietnam. J Med Microbiol. 2015;64:1162–9.
Dinc G, Demiraslan H, Elmali F, Ahmed SS, Alp E, Doganay M. Antimicrobial efficacy of doripenem and its combinations with sulbactam, amikacin, colistin, tigecycline in experimental sepsis of carbapenem-resistant Acinetobacter baumannii. New Microbiol. 2015;38:67–73.
Chierakul W, Anunnatsiri S, Short JM, Maharjan B, Mootsikapun P, Simpson AJH, Limmathurotsakul D, Cheng AC, Stepniewska K, Newton PN, Chaowagul W, White NJ, Peacock SJ, Day NP, Chetchotisakd P. Two randomized controlled trials of ceftazidime alone versus ceftazidime in combination with trimethoprim-sulfamethoxazole for the treatment of severe melioidosis. Clin Infect Dis. 2005;41:1105–13.
Chierakul WAS, Chaowagul W, Peacock SJ, Chetchotisakd P, Day NPJ. Addition of Trimethoprim-sulfamethoxazole to ceftazidime during parenteral treatment of meliodosis is not associated with a long-term outcome benefit. Clin Infect Dis. 2007;45:521–3.
Chetchotisakd P, Chierakul W, Chaowagul W, Anunnatsiri S, Phimda K, Mootsikapun P, Chaisuksant S, Pilaikul J, Thinkhamrop B, Phiphitaporn S, Susaengrat W, Toondee C, Wongrattanacheewin S, Wuthiekanun V, Chantratita N, Thaipadungpanit J, Day NP, Limmathurotsakul D, Peacock SJ. Trimethoprim-sulfamethoxazole versus trimethoprim-sulfamethoxazole plus doxycycline as oral eradicative treatment for melioidosis (MERTH): a multicentre, double-blind, non-inferiority, randomised controlled trial. Lancet. 2014;383:807–14.
Kalin G, Alp E, Akin A, Coskun R, Doganay M. Comparison of colistin and colistin/sulbactam for the treatment of multidrug resistant Acinetobacter baumannii ventilator-associated pneumonia. Infection. 2013;42:37–42.
Batirel A, Balkan II, Karabay O, Agalar C, Akalin S, Alici O, Alp E, Altay FA, Altin N, Arslan F, Aslan T, Bekiroglu N, Cesur S, Celik AD, Dogan M, Durdu B, Duygu F, Engin A, Engin DO, Gonen I, Guclu E, Guven T, Hatipoglu CA, Hosoglu S, Karahocagil MK, Kilic AU, Ormen B, Ozdemir D, Ozer S, Oztoprak N, Sezak N, Turhan V, Turker N, Yilmaz H. Comparison of colistin–carbapenem, colistin–sulbactam, and colistin plus other antibacterial agents for the treatment of extremely drug-resistant Acinetobacter baumannii bloodstream infections. Eur J Clin Microbiol Infect Dis. 2014;33:1311–22.
Zhou Q, Lee SK, Jiang SY, Chen C, Kamaluddeen M, Hu XJ, Wang CQ, Cao Y. Efficacy of an infection control program in reducing ventilator-associated pneumonia in a Chinese neonatal intensive care unit. Am J Infect Control. 2013;41:1059–64.
Simsek F, Gedik H, Yildirmak MT, Iris NT, Türkmen A, Ersoy A, Ersöz M, Gücüyener A. Colistin against colistin-only-susceptible Acinetobacter baumannii-related infections: monotherapy or combination therapy. Indian J Med Microbiol. 2012;30:448–52.
Gedik H, Yildirmak T, Simsek F, Kanturk A, Aydýn D, Anca D, Yokus O, Demirel N. The outcome of non-carbapenem-based empirical antibacterial therapy and VRE colonisation in patients with hematological malignancies. Afr Health Sci. 2013;13:363–8.
Kimang'a AN. A situational analysis of antimicrobial drug resistance in Africa: are we losing the battle? Ethiop J Health Sci. 2012;22:135–43.
Inchai J, Pothirat C, Liwsrisakun C, Deesomchok A, Kositsakulchai W, Chalermpanchai N. Ventilator-associated pneumonia: epidemiology and prognostic indicators of 30-day mortality. Jpn J Infect Dis. 2015;68:181–6.
Werarak P, Waiwarawut J, Tharavichitkul P, Pothirat C, Rungruanghiranya S, Geater SL, Chongthaleong A, Sittipunt C, Horsin P, Chalermskulrat W, Wiwatworapan T, Thummakul T, Mootsikapun P, Rungsrithong N, Supawita S, Chuchotthavorn C, Tongsai S, Thamlikitkul V. Acinetobacter baumannii nosocomial pneumonia in tertiary care hospitals in Thailand. J Med Assoc Thail. 2012;95(Suppl 2):S23–33.
Nhu NT, Lan NP, Campbell JI, Parry CM, Thompson C, Tuyen HT, Hoang NV, Tam PT, Le VM, Nga TV, Nhu Tdo H, Van Minh P, Nga NT, Thuy CT, Dung le T, Yen NT, Van Hao N, Loan HT, Yen LM, Nghia HD, Hien TT, Thwaites L, Thwaites G, Chau NV, Baker S. Emergence of carbapenem-resistant Acinetobacter baumannii as the major cause of ventilator-associated pneumonia in intensive care unit patients at an infectious disease hospital in southern Vietnam. J Med Microbiol. 2014;63:1386–94.
Hantrakun V, Chierakul W, Chetchotisakd P, Anunnatsiri S, Currie BJ, Peacock SJ, Day NPJ, Cheah P, Limmathurotsakul D, Lubell Y. Cost-effectiveness analysis of parenteral antimicrobials for acute melioidosis in Thailand. Trans R Soc Trop Med Hyg. 2015;109:416–8.
Dance D. Treatment and prophylaxis of melioidosis. Int J Antimicrob Agents. 2014;43:310–8.
Leone M, Bechis C, Baumstarck K, Lefrant JY, Albanèse J, Jaber S, Lepape A, Constantin JM, Papazian L, Bruder N, Allaouchiche B, Bézulier K, Antonini F, Textoris J, Martin C. De-escalation versus continuation of empirical antimicrobial treatment in severe sepsis: a multicenter non-blinded randomized noninferiority trial. Intensive Care Med. 2014;40:1399–408.
Nobre V, Harbarth S, Graf J-D, Rohner P, Pugin J. Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med. 2008;177:498–505.
Stolz D, Smyrnios N, Eggimann P, Pargger H, Thakkar N, Siegemund M, Marsch S, Azzola A, Rakic J, Mueller B, Tamm M. Procalcitonin for reduced antibiotic exposure in ventilator-associated pneumonia: a randomised study. Eur Respir J. 2009;34:1364–75.
Hochreiter M, Köhler T, Schweiger A, Keck F, Bein B, von Spiegel T, Schroeder S. Procalcitonin to guide duration of antibiotic therapy in intensive care patients: a randomized prospective controlled trial. Crit Care. 2009;13:R83.
Schroeder S, Hochreiter M, Koehler T, Schweiger AM, Bein B, Keck FS, Von Spiegel T. Procalcitonin (PCT)-guided algorithm reduces length of antibiotic treatment in surgical intensive care patients with severe sepsis: Results of a prospective randomized study. Langenbeck’s Arch Surg. 2009;394:221–6.
Bouadma L, Luyt C-E, Tubach F, Cracco C, Alvarez A, Schwebel C, Schortgen F, Lasocki S, Veber B, Dehoux M, Bernard M, Pasquet B, Régnier B, Brun-Buisson C, Chastre J, Wolff M. Use of procalcitonin to reduce patients' exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 2010;375:463–74.
Harrison M, Collins CD. Is procalcitonin-guided antimicrobial use cost-effective in adult patients with suspected bacterial infection and sepsis? Infect Control Hosp Epidemiol. 2015;36:265–72.
Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, Cook CH, O’Neill PJ, Mazuski JE, Askari R, Wilson MA, Napolitano LM, Namias N, Miller PR, Dellinger EP, Watson CM, Coimbra R, Dent DL, Lowry SF, Cocanour CS, West MA, Banton KL, Cheadle WG, Lipsett PA, Guidry CA, Popovsky K. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015;372:1996–2005.
Deliberato RO, Marra AR, Sanches PR, Martino MDV, Ferreira CEDS, Pasternak J, Paes AT, Pinto LM, dos Santos OFP, Edmond MB. Clinical and economic impact of procalcitonin to shorten antimicrobial therapy in septic patients with proven bacterial infection in an intensive care setting. Diagn Microbiol Infect Dis. 2013;76:266–71.
Qu R, Ji Y, Ling Y, Ye C-Y, Yang S-M, Liu Y-Y, Yang R-Y, Luo Y-F, Guo Z. Procalcitonin is a good tool to guide therapy in patients with severe acute pancreatitis. Saudi Med J. 2012;33:382–7.
de Jong E, van Oers JA, Beishuizen A, Vos P, Vermeijden WJ, Haas LE, Loef BG, Dormans T, van Melsen GC, Kluiters YC, Kemperman H, van den Elsen MJ, Schouten JA, Streefkerk JO, Krabbe HG, Kieft H, Kluge GH, van Dam VC, van Pelt J, Bormans L, Otten MB, Reidinga AC, Endeman H, Twisk JW, van de Garde EMW, de Smet A, Kesecioglu J, Girbes AR, Nijsten MW, de Lange DW. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis. 2016;16:819–27.
Nargis W, Ibrahim M, Ahamed BU. Procalcitonin versus C-reactive protein: usefulness as biomarker of sepsis in ICU patient. Int J Crit Illn Inj Sci. 2014;4:195–9.
Pugh R, Grant C, Cooke RP, Dempsey G. Short-course versus prolonged-course antibiotic therapy for hospital-acquired pneumonia in critically ill adults (Review). Summary of findings for the main comparison. 2011.
Timsit J-F, Soubirou J-F, Voiriot G, Chemam S, Neuville M, Mourvillier B, Sonneville R, Mariotte E, Bouadma L, Wolff M. Treatment of bloodstream infections in ICUs. BMC Infect Dis. 2014;14:1–11.
Klompas M, Speck K, Howell MD, Greene LR, Berenholtz SM. Reappraisal of routine oral care with chlorhexidine gluconate for patients receiving mechanical ventilation systematic review and meta-analysis. JAMA Intern Med. 2014;174(5):751–61.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2019 The Author(s)
About this chapter
Cite this chapter
Thwaites, C.L. et al. (2019). Infection Management in Patients with Sepsis and Septic Shock in Resource-Limited Settings. In: Dondorp, A., Dünser, M., Schultz, M. (eds) Sepsis Management in Resource-limited Settings. Springer, Cham. https://doi.org/10.1007/978-3-030-03143-5_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-03143-5_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-03142-8
Online ISBN: 978-3-030-03143-5
eBook Packages: MedicineMedicine (R0)