Abstract
Congenital infection with Trypanosoma cruzi is a global problem, occurring on average in 5% of children born from chronically infected mothers, with variations depending on the region. In endemic areas with inadequate vector control, Chagas disease, also known as American trypanosomiasis, is usually a vector-borne disease. In areas with effective vector control and in urban areas, the main route of new cases of CD is through mother-to-child transmission. The estimated number of new cases of congenital T. cruzi infection is 8668 cases/year [2]. This is also the case of non-endemic countries where, due to population migration, CD is increasingly becoming a public health problem in non-endemic settings. The majority of infected infants are asymptomatic, and the diagnosis is based on the microscopic observation of the parasite in the blood of newborns and by serology in infants older than 8 months of age when maternal transplacental antibodies have waned. Two drugs are available for treatment, benznidazole and nifurtimox. Treatment should be implemented immediately after diagnosis since the sooner the infection is treated, the better the prognosis. The treatment efficacy is around 95% in different cohorts with a good drug safety profile. Recent studies have shown that its transmission can be prevented through treatment of infected women before they become pregnant. Considering that etiological treatment of the child is highly effective if performed before 1 year of age, the diagnosis of infection in pregnant women and their newborns has to become the standard of care and integrated into the surveillance programs of syphilis and human immunodeficiency virus.
Similar content being viewed by others
Keywords
1 Introduction
Chagas disease or American trypanosomiasis is caused by the hemoflagellate parasite Trypanosoma cruzi. Infection most often occurs in Latin America, the endemic area of Chagas disease, via vector transmission. In the past few decades, a growing migratory current has brought large numbers of patients from rural to urban areas, changing the epidemiology of Chagas disease. Currently, the largest number of infected people in Latin America dwells in cities with no vector transmission, making the mother-to-child transmission the main route of infection of the disease in these areas and the main route of transmission overall. Also, migration of Latin Americans to non-endemic countries has brought the disease, and congenital cases, to areas where Chagas disease had never been present before, putting newborns at risk of misdiagnosis or no diagnosis at all in the case of asymptomatic patients [1].
T. cruzi infection initially presents with an acute phase of variable duration (2–8 weeks) characterized by high parasitemia and non-specific symptoms (e.g., fever, hepatosplenomegaly), followed by a phase known as the chronic indeterminate or latent asymptomatic phase that can last for decades before developing cardiac and/or digestive disorders in about 30% of the patients.
Endemic countries, with the support of the Pan American Health Organization (PAHO) , have established regional programs for the prevention and control of CD. These programs mostly focus on the elimination of the triatomine vector by insecticide spraying, prevention of transfusion of contaminated blood, and screening for maternal infection during pregnancy. In large part due to these programs, the current burden of CD in Latin America has been reduced from 2.8 million disability-adjusted life years to less than 500,000 in 2015 [2].
Unfortunately, strategies to prevent vector transmission have no impact on vertical transmission, which leads to a continuous stream of new congenital cases from mothers with the disease.
The PAHO has stressed the need to consider congenital Chagas disease as a public health problem and recommends that each country develops protocols for universal pregnancy screening and treatment of infected newborns. Most pregnant women with the disease are in the asymptomatic chronic phase and have vertical transmission rates of approximately 5% [3].
Universal screening of pregnant women for detection of Chagas disease is extremely important given the asymptomatic nature of the disease in the vast majority of these women and the high effectiveness and safety of pharmacological treatment in infected newborns. Implementation of universal screening has also led to the realization that most infected newborns are asymptomatic and would hardly be identified if screening is not performed.
2 Epidemiology
It is important to keep in mind that the epidemiology of Chagas disease should refer to the epidemiology of the patients with the disease and not to the areas where the vector can be found. This is a common confusion when discussing Chagas disease that may leave most of the patients (i.e., those who live in urban areas without exposure to the vector) out of the picture.
Chagas disease patients can be found in all of the Americas, including North America, and, due to migratory currents, also in most continents of the world. Cases have been reported in countries as far from the Americas as Japan and Australia and in virtually all of Europe. The surge in cases in non-endemic countries has prompted the implementation of diagnostic and treatment guides in these areas [4].
Recently the PAHO has estimated that there are 5,700,000 infected people in Latin America, with Argentina having the largest absolute number of patients and Bolivia the highest prevalence of the infection. Approximately 8700 babies are born with congenital Chagas disease each year in Latin America [2].
Chagas disease prevalence in pregnant women ranges from 3% to 40% depending on the region and increases significantly after 20 years of age, which suggests that vector and transfusion control programs have been highly effective in thwarting disease transmission [5]. However, certain areas of Argentina, Bolivia, and Paraguay still have high infection rates in children under 10 years old due to uncontrolled vector presence. The same is true for some areas in Central America, which has an important impact on the epidemiology of North American countries such as Mexico and the United States due to migration of Latin American patients to these areas.
Migration has also led to a prevalent urban picture of the disease, with most new cases occurring due to congenital transmission [6]. The highest incidence of congenital cases can be found in cities, where most infected patients live, in spite of being an area with no vector transmission [5, 7]. The explanation for this situation is that large migrations took place from rural areas to the cities, which brought a large proportion of infected patients from areas with vector presence to cities without the vector.
The number of infected women of childbearing age has been estimated [2] to be approximately 1,250,000 in Latin America, and the overall incidence of congenital Chagas disease infection has been estimated to be 0.9 per 1000 live newborns. This would lead to approximately 8700 infected newborns every year. However, the actual number of congenital transmissions diagnosed and treated is much lower than this estimate, most likely due to a lack in implementation of universal screening programs and to a reluctance to treat infected newborns.
In the United States, approximately 300,000 cases are believed to be present [8], and 40,000 pregnant women may be infected, resulting in 2000 congenital cases through mother-to-child transmission [9]. Clearly, there is a need for active surveillance data in order to better refine these prevalence data.
3 Infection in Pregnancy
Chagas disease does not seem to affect fertility [10, 11]. Reports from the 1970s suggested a high incidence of prematurity and high morbidity in infected newborns. However, these observations were based on populations of symptomatic women in the acute phase of the infection. Maternal chronic infection has no effect on the outcome of pregnancy or on the health of newborns as long as there is no maternal transmission of parasites to the unborn child [12]. Fetal infection in early gestation increases the risk of premature delivery, low birth weight, and premature rupture of amniotic membranes, effects that may be related to placental inflammation observed in these cases [13].
Most pregnant women are in the chronic phase of infection and lack any symptoms or signs related to the infection [14]. Absence of clinical and electrocardiogram findings in pregnant women may be explained by the fact that the peak of fertility in the areas with high prevalence of Chagas disease is approximately 20–30 years of age, whereas cardiac or gastrointestinal tract involvement does not appear in infected patients until well past 40 years of age.
Fetal infection requires the presence of circulating parasites in the pregnant mother’s bloodstream. T. cruzi persistently infects the host and can be found in the bloodstream in both acute and chronic phases, meaning that a woman can transmit the infection in any of her pregnancies [15, 16]. However, acute infection exacerbates the risk of transplacental transmission of the infection, possibly due to the high parasitemia observed in the acute phase. In the published case series, infection was observed in 71% of newborns of infected mothers in the acute phase, 57% of whom were born prematurely [17, 18].
Most women of fertile age are in the chronic asymptomatic phase, which implies a low level of circulating parasites. However, parasite replication and circulation have been shown to increase during pregnancy, particularly in the last trimester. In fact, a direct relationship between maternal parasitemia and risk of congenital infection has been identified [19,20,21]. This increased risk provides strong support for pharmacological treatment (i.e., with benznidazole or nifurtimox) of women before they become pregnant, as children or young adults, to abolish parasitemia and prevent congenital transmission [22, 23].
4 Factors Associated to Congenital Transmission of Chagas Disease
Reported rates of congenital transmission show significant geographic variability that ranges from 1% to 18.2% [3]. The reasons for this variability remain unexplained to date.
Congenital transmission of T. cruzi requires an interaction between the parasite, the maternal immune system, and the placenta.
-
1.
The parasite : T. cruzi circulates in the bloodstream as trypomastigotes, which can disseminate to tissues and invade the placenta. After accessing the placental cells, the parasite transforms into the intracellular form, the amastigote, and starts dividing. After bursting out of the host cell, amastigotes become trypomastigotes again, and, if the parasite manages to reach the fetal circulation, it can infect the fetus. T. cruzi has been classified into six groups (called discrete typing units (DTU)). However, no relationship has been observed between DTUs and the risk of congenital transmission of the infection [24]. Large gaps still exist in the understanding of the role of the genetic diversity of T. cruzi, in the infection, the risk of disease progression, and the risk of congenital transmission and of the reactivation in immunosuppressed subjects [25].
-
2.
Maternal immune system : Most pregnant women can be found with low-level parasitemia in the chronic stage. Maternal IgG antibodies are thought to control the infection and limit placental invasion, thus limiting placental transfer of the parasite to the fetus. In acute infections, where the immune response to the parasite is still immature and fails to control parasitemia, congenital transmission rates are significantly higher [21, 26].
-
3.
Placenta: The placenta plays a vital role as a barrier that protects the fetus from infectious agents. T. cruzi infection is believed to take place toward the end of the pregnancy since the majority of infected newborns are asymptomatic.
Histological examination of placentas from infected mothers shows necrotic areas with inflammation and high numbers of amastigote nests. These areas can be found mainly in the areas of placental membrane insertions, which lead to the suggestion that the main infection route of the organ is via the marginal sinus to the chorion, infecting macrophages and fibroblasts, eventually reaching the fetal vessels [27].
Placentas from women in the chronic stage commonly lack significant signs of inflammation and have low numbers or no amastigote nests. These observations suggest the existence of antiparasitic mechanisms protecting the placenta of women at this stage of the infection.
Transmission of the infection seems to be lower during early pregnancy possibly due to the intervillous space being close to the arterial spaces. Placental blood flow is continuous and diffuses starting on week 12 of gestation, which has been proposed as a reason for the observed infections at a higher gestational age [28].
5 Chagas Disease and Breastfeeding
Chagas disease can be acquired by ingestion of foods or juice contaminated with vector feces containing the parasite. This fact suggests the possibility that the disease can also be transmitted by breastmilk from an infected woman. However, oral infections due to contaminated food have been linked to a heavy load of parasites in the food, something that is unlikely in breastmilk.
There are very few epidemiological data suggesting infant exposure through breastmilk [29]. A few studies have observed trypomastigotes in breastmilk from women in the acute phase of the infection, but these observations have not been confirmed by other authors [30]. One case of possible human infection linked to contaminated breastmilk has been documented, in a breastfed infant who became infected and whose mother had bleeding nipples, which raises the possibility of an oral route of infection, most likely due to the ingestion of blood and not breastmilk [31].
Experimental mouse models have shown a low rate of infection via breastmilk in breastfeeding mice fed from mice in the acute infection stage [29].
Considering the data previously mentioned, and given that most infected women nowadays would be in the chronic stage (i.e., low parasitemia) at the time of breastfeeding, the risk of transmission of Chagas disease to their breastfed babies would be close to negligible. Therefore, maternal Chagas disease is not considered a contraindication to breastfeeding. The only possible exception is a woman in the acute phase of the infection who also has bleeding nipples.
6 Clinical Findings in the Newborn
Most infected newborns are asymptomatic. Clinical manifestations of Chagas disease in newborns vary widely, from premature babies with important multiorgan involvement and high risk of mortality to completely asymptomatic full-term babies [15, 32,33,34,35,36]. This wide range of clinical presentations has been observed in several geographical areas and may be explained to some extent by variations in parasite strains, maternal nutritional state, and variations in maternal immune response to the infection.
Symptomatic newborns can have varying degrees of morbidity. Clinical signs may be related to the timing of fetal infection. Infections in the first and/or second trimester of pregnancy lead to prematurity and significant clinical manifestations such as low birth weight, hepatosplenomegaly, anemia, thrombocytopenia, and, more rarely, meningoencephalitis, myocarditis, and pneumonitis [32, 35, 37, 38].
Widespread maternal screening for Chagas disease has brought about the diagnosis of a larger number of infected infants, most of whom turned out to be completely asymptomatic. This observation provides support for the idea that most of the infections take place during the third trimester or near the end of the pregnancy [15, 39].
Symptomatic cases show clinical manifestations that resemble those observed in other intrauterine infections such as toxoplasmosis and Cytomegalovirus infection. The most common clinical sign is hepatomegaly and anemia and thrombocytopenia. Much less commonly, eye and/or digestive tract involvement has been described [40, 41]. Mortality has been reported to be approximately 5%, mainly in patients with acute-disseminated infection with myocarditis and/or meningoencephalitis [12].
Several case series of congenital cases can be found in the literature. In Cordoba City, Argentina, 52 cases were described (62% term babies), with an incidence of 30% abnormal weight for gestational age [42]. Approximately 30% of cases were asymptomatic, 31% had hepatosplenomegaly and tachycardia, and the remaining 38% had delayed clinical signs, mostly hepatosplenomegaly. Only four infants had signs of heart failure and none had meningoencephalitis. No deaths were observed in this series, and no cardiovascular sequelae were found after 10 years of follow-up [43].
In a case series of 102 infants collected over 18 years in the Province of Salta, Argentina, 33.3% of patients were asymptomatic, 28% were premature babies, and 59% had hepatomegaly, 42% splenomegaly, 40% jaundice, 39% anemia, 5% hydrops fetalis, and 4% meningoencephalitis [44].
Another case series, from Bolivia, described infants with congenital Chagas infection; 54% were asymptomatic, but there was also a high rate of prematurity, and 25% had respiratory distress, 16% hepatomegaly, 14% splenomegaly, 13% cardiomegaly, 11% neurological involvement, 8% anasarca, and 8% petechia [12].
Finally, a case series from the Parasitology and Chagas Service of the Buenos Aires Children’s Hospital “Ricardo Gutierrez,” Argentina, described 168 patients, 76% of whom were asymptomatic, and 9% had hepatosplenomegaly, 1% sepsis, 2% myocarditis, and 2% hepatitis [35].
Some cases of coinfection of T. cruzi and HIV have been reported; most of them are severe with profound central nervous system involvement and marked parasitemia observed by microhematocrit (MH) method at the time of diagnosis [45].
7 Diagnosis
Diagnosis of Chagas disease in pregnant women is made by serological testing. In areas without vector transmission, a single serological test (with two different serological methods) should suffice to confirm or rule out maternal infection. The most commonly used tests are ELISA, indirect hemagglutination (IHA) , indirect immunofluorescence (IFI), and direct agglutination. No test is sensitive or specific enough to allow use of any single test for diagnosis. Current guidelines recommend the use of two serological tests based on a different set of antigens (e.g., whole-parasite lysate and recombinant antigens) to ensure high enough specificity and sensitivity in the diagnosis of Chagas disease [46]. In areas with active vector transmission, serological testing should be performed at the beginning and near the end of the pregnancy period and considered for any pregnant mother with a febrile illness without a clear explanation to rule out acute infection.
Diagnostic tests for Chagas disease have to be carried out for any newborn with an infected mother. Infected newborns are considered to be in the acute phase of the infection. Thus, initial diagnostic procedures involve searching for parasites in blood, commonly using direct parasitological methods with a concentration step. These methods are based on direct visualization of the parasite in the white blood cell phase after centrifugation of a very small volume of blood obtained in a heparinized capillary tube [15, 47]. Direct detection of the parasite in blood is facilitated by the fact that the trypanosome has a characteristic movement pattern and a relatively large size that allows its visualization by optical microscopy. In addition, the high numbers of parasites present in the blood of infected newborns make detection a relatively simple task for adequately trained laboratory personnel. The peak of parasitemia is observed at 1 month of age.
Diagnosis of congenital infection during the first weeks of life should be based on the examination of the infant’s blood using a direct parasitological method (i.e., microhematocrit) to look for the presence of T. cruzi.
Serological tests are not useful during the first months of life due to passive transfer of IgG from the mother during gestation. Serological tests for specific IgM would be potentially useful but have not been fully developed to date.
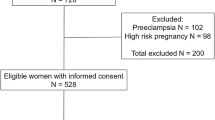
If the infant has a negative parasitemia during the first few weeks of life, a serological test at 8 months of age should be performed to rule out or confirm the infection. It is assumed that maternal antibodies disappear after 8 months of age, meaning that if the serological tests are positive at this time, the detected IgG reflects an immune response of the infant against the parasite, and therefore there is an active infection. If the patient has a negative serological test at 8 months, the congenital infection is ruled out [15, 47] (Fig. 1). In the few cases that have quantitative serological values close to the cutoff level at 8 months, the tests should be repeated after 1 month to confirm the diagnosis.
7.1 Diagnosis in Newborns
Direct parasitological detection methods such as the microhematocrit (MH) method are the diagnostic methods of choice for newborns. The MH method is based on the observation of parasites (trypomastigotes) in the white blood cell layer after centrifuging blood from the newborn in a heparinized capillary tube. The MH method has numerous advantages, including a low volume of blood requirement (0.3 ml), fast turnover (under 30 min), and high sensitivity in the hands of adequately trained personnel. The MH method is the suggested procedure by the Pan American Health Organization and public health Organization for diagnosis of newborns [47].
A drawback of this method is the requirement for a trained operator, which may lead to variability in diagnostic sensitivity across centers depending on the level of training and experience [32]. Another consideration is that the age of the newborn at the time of blood sampling is important as parasitemia increases during the first days of life, which has led to the suggestion that repeated blood sampling could increase sensitivity of the method. However, repeated sampling is difficult to implement in screening programs aimed at mostly asymptomatic newborns [32, 37]. Infants with clinical signs had higher parasite loads and were significantly more likely to be detected by direct parasitological test.
Indirect parasitological methods (i.e., xenodiagnosis, blood culture, and inoculation of lactating mice) have high sensitivity but require access to highly trained personnel and complex infrastructure and take weeks to months to yield results. None of these indirect methods are in routine use currently [15].
Histological examination of the placenta has limited sensitivity, and placental involvement does not closely correlate to fetal infection [48].
Modern PCR techniques are being developed and standardized for clinical use and have shown higher sensitivity than conventional parasitological diagnostic techniques in some series [49,50,51]. However, false positives have been reported, possibly due to the presence of free parasite DNA from the mother in fetal circulation [52, 53]. Currently, PCR methods should be considered experimental since the PCR sensitivity varies widely depending on the DNA extraction methods, primers and population tested.
The use of isothermal amplification molecular methods, such as loop-mediated isothermal amplification and nucleic acid sequence-based amplification, is becoming increasingly popular for the detection of trypanosomes as they offer simple, rapid, and cheap alternatives to traditional PCR-based methods [54, 55]. Isothermal tests involve a single reaction in a single tube incubated at a constant temperature; therefore, these techniques do not require the expensive thermocycling equipment that is necessary for PCR.
Widespread clinical use of these molecular tests still requires further testing in larger series to accurately evaluate sensitivity and specificity. Alternative serological methods, such as the detection of T. cruzi-specific IgM in the infant, have unfortunately never been adequately investigated, mainly due to the perception of low sensitivity of these methods and the consequent lack of interest in the laboratory diagnostics industry. Nontraditional antigens, such as SAPA [56,57,58], have been proposed as good markers of recent infection in newborns but have not been shown to be sufficiently sensitive in other studies [32].
Development of immune complexes (i.e., antibody-antigen complexes) due to high levels of parasitemia has been shown to produce false negatives in antibody-based tests due to T. cruzi-specific antibody sequestration in those complexes, particularly using hemagglutination test [15].
7.2 Diagnosis for Children Over 8 Months of Age
Infants have circulation antibodies which originated in the mother and which were transferred through the placenta during the last months of gestation. Due to this, identification of T. cruzi-specific IgG is not useful for diagnosis of infant infection as these antibodies may reflect maternal T. cruzi-specific IgG.
The age at which maternal antibodies disappear has been reported from 6 to 9 months. The more sensitive the test used, the longer the amount of time the transferred maternal antibodies will be detected. Using indirect hemagglutination and immunofluorescence, which are less sensitive tests, the maternal antibodies are not detected at 6 months. When a highly sensitive ELISA test is employed, maternal antibodies can be detected in a small number of infants at 8 months. Children over 8 months of age are expected to have eliminated these maternal antibodies that could have produced false-positive results in antibody-based tests for the diagnosis of Chagas disease. After this age, the methods of choice for the diagnosis of T. cruzi infection, or to rule out the infection, are serological tests. No single serological test has sufficient sensitivity and specificity to be relied on alone. Therefore, Chagas disease is diagnosed in children over 8 months of age if two distinct serological IgG tests, principally ELISA using whole-parasite lysates or recombinant antigens, are positive [47].
Diagnosis in children over 8 months of age is confirmed if two serological tests are positive.
8 Therapy
Only two drugs are available and have been shown to be efficacious in the treatment of congenital and pediatric Chagas disease: nifurtimox and benznidazole. Both drugs lead to a high response (close to 100% in children under 3 years of age), as measured by the decrease of antibody titers and conversion to negative serology at follow-up. Several clinical studies have shown that the earlier the treatment is administered, the higher the chance of complete response paired with a significantly lower risk of adverse events to the drugs. Successful treatment of infected infants will prevent the development of later cardiological and gastrointestinal complications in adulthood. These facts highlight the need for early diagnosis and treatment [35, 43, 59,60,61,62].
Benznidazole was developed in 1971. It was initially being developed as a chemotherapeutic agent, and hence this may explain the mg/kg dosing approach. Usual doses can vary between 5 and 10 mg/kg/day BID. Benznidazole is formulated in scored tablets of 50 and 100 mg. A pediatric formulation (a 12.5 mg dispersible tablet) is currently in development.
Nifurtimox was developed by Bayer in 1970; usual doses are 10–15 mg/kg/day TID. Only a 120 mg scored tablet is currently available. A pediatric 30 mg dispersible tablet is under development.
Both drugs are well absorbed with good tissue distribution.
Treatment duration with any of these two drugs has been empirically set at 60 days, based on studies performed on older children [60, 63].
Newborns and infants have high response rates (over 95%) [35, 50, 59], after 60 days of treatment. An excellent response was also observed in a cohort of newborns treated for 30 days with once-daily (OD) benznidazole dosing [61]. These results suggest that further clinical studies are urgently needed to define the optimal dosing schedule of these drugs in order to improve compliance and decrease adverse drug reaction rates, given that efficacy rates seem to be close to optimal.
Table 1 summarizes the published clinical trials of congenital cases treated with benznidazole or nifurtimox with sufficient therapeutic data to provide meaningful conclusions. In the summarized studies, a decrease in antibody titers until negative seroconversion was observed.
Clinical studies have consistently shown a better tolerance of benznidazole or nifurtimox in young children and infants compared to older children (i.e., above 7 years of age) and adults, with treatment dropout rates close to zero in newborns [35, 43, 65, 70] and around 10% in infants and young children [63]. These rates increase up to 20–40% in adults [71].
The main adverse drug reactions (ADRs) associated with benznidazole and nifurtimox are similar and include anorexia, headache, irritability, sleep disturbances, leukopenia, thrombocytopenia, rash, gastrointestinal upset, increased liver enzymes, and neuropathy. Most of these ADRs are rare, except for mild rashes (more common with benznidazole) and anorexia, irritability, and headache (more common with nifurtimox) [42]. Gastrointestinal upset is also common, but problems associated with the administration of formulations which are not specifically developed for children may play a role in this ADR since tablets need to be crushed for administration.
In a large cohort of infants and children followed at the Parasitology and Chagas Service, Buenos Aires Children’s Hospital “Ricardo Gutierrez,” 69% of patients had no ADRs [72]. Most of the ADRs observed in this cohort were mild and did not require treatment interruption. Children older than 7 years of age had a higher frequency of mild rash that in some cases temporary treatment interruption and administration of antihistamines before completing treatment are required.
Premature and low-weight newborns seem to have higher rates of leukopenia and thrombocytopenia associated with the treatment. This observation led to the development of a treatment protocol in our institution that starts treatment with half the dose (e.g., 2.5 mg/kg/day instead of 5 mg/kg/day) until there is a normal blood count at 1 week of treatment after checking for ADRs. If no hematological ADRs are observed, full dose is then instituted until the full 60 days of treatment are completed [15].
Recent pediatric pharmacokinetic studies of benznidazole have shown that children have lower drug levels in blood compared to older children and adults, possibly due to a higher clearance rate. However, the therapeutic response was excellent, and ADRs were rare in the study population, suggesting that adults and older children may be receiving higher-than-necessary benznidazole doses and possibly dose reduction in this older population may lead to decreased ADR rates without affecting response rates [68]. This hypothesis remains to be formally proven in a clinical study to date.
In our experience, in a series of 62 congenitally infected children treated with nifurtimox, adverse effects were common, but most were mild (24% poor feeding, 14.5% irritability, and 6.5% vomiting). Three newborns had reversible leukopenia and thrombocytopenia [15]. Pediatric pharmacokinetic studies of nifurtimox in children are scarce. Currently a large clinical trial of a nifurtimox pediatric formulation is underway, and it includes a pharmacokinetic arm to try to address this gap [Clinicaltrials.gov#NCT02625974].
8.1 Follow-Up of Treatment Response
Treatment protocols of children with Chagas disease should include evaluation of potential ADRs, including blood counts and liver function tests, at 7, 30, and 60 days of treatment. If a newborn has a positive parasitemia at the start of the treatment, a weekly evaluation of parasitemia by a direct parasitological test like the microhematocrit test is recommended until it becomes negative usually between the second and third weeks of treatment [15, 35, 61]. The main criterion for therapeutic failure is the identification of the presence of the parasite by direct parasitological methods. If parasitemia persists, inappropriate compliance with the treatment should be considered, as well as (less likely) medication intolerance (e.g., vomiting) and parasite resistance. However, it should be mentioned that parasite resistance to benznidazole or nifurtimox seems to be extremely rare and well-documented examples of this event are extremely scarce. In case of treatment failure or parasite resistance, change of medication (benznidazole to nifurtimox or vice versa) is advisable.
After treatment is completed, patients need to be monitored with quantitative serological tests every 3 months during the first year and then every 6 months until serology becomes negative. After two consecutive negative serological tests, the patient is considered cured (Fig. 2). Cure rates, as evaluated by conventional serology, are over 90% in infants treated before 1 year of age [15, 35, 50, 59, 61, 65]. Newborns with positive parasitemia are considered cured when their serological tests become negative, around 8–12 months of age.
The shorter the duration of the infection, the faster the serological tests become negative. Infants treated during the first year of life commonly become negative within 1 year of treatment. Older children show a slower rate of decrease in antibody titers that can take years to become negative [60, 63].
In patients with persistent high serological titers during posttreatment follow-up, a direct parasitological test such as PCR should be considered, and if positive, a new round of treatment should be evaluated. In such a case, evaluation should focus on compliance with the treatment, as the most common reason for treatment failure is, by far, non-compliance.
It is important to keep in mind that the longer the follow-up, the higher the probability of negative seroconversion.
9 Prevention of Congenital Infection
Primary prevention of congenital infection can be achieved by controlling vector transmission, which will avoid maternal infection. This strategy has been successful in many areas in Latin America. However several regions with high rates of vector transmission remain. These are linked to poor housing and house infestation with the vectors.
Secondary prevention by screening and treatment of pregnant women is currently not viable due to the lack of information on fetal safety for nifurtimox and benznidazole. An alternative way of secondary prevention, namely, pharmacological treatment of girls and women before pregnancy, has been shown to be effective in preventing vertical transmission of the disease [22, 23, 73].
Effective tertiary prevention by newborn screening, diagnosis, and treatment of infected infants requires universal screening strategies that identify infected pregnant women and allow evaluation of every newborn to these women. Unfortunately, these strategies are hampered by the high rate of migration of infected subjects and poor compliance with screening strategies in some areas by governments and health systems.
According to the recommendations of the Technical Group on “Prevention and Control of Congenital Transmission and Case Management of Congenital Infections,” [47] serological testing is recommended for pregnant women (1) who are living in disease-endemic areas, (2) who are living in disease non-endemic areas and have occasionally received blood transfusion in disease-endemic areas, and (3) who are living in disease non-endemic areas and are born or have lived previously in disease-endemic areas or whose mothers were born in such areas.
Since 2010, Pan American Health Organization (PAHO) member states have committed to the elimination of mother-to-child transmission (EMTCT) of HIV and syphilis in Latin America. In addition, the PAHO Strategy and Plan of Action for Chagas Disease Prevention, Control, and Care [74] includes the specific objective of supporting implementation of secondary prevention of congenital Chagas disease. It recognizes that reducing mother-to-child transmission of Chagas disease requires T. cruzi screening for pregnant women as part of universal prenatal care as well as monitoring, diagnosing, and treating all newborns of infected mothers.
These commitments were renewed and expanded in 2016 through the approved Plan of Action for the Prevention and Control of HIV and Sexually Transmitted Infections (2016–2021), contributing to the end of AIDS and sexually transmitted infections as a public health problem in the Americas. The plan of action expands the EMTCT initiative (labeled “EMTCT Plus”), leveraging the maternal and child health platform to include elimination of other preventable communicable diseases in the Americas, such as hepatitis B and Chagas disease. A PAHO document was published in 2017 [75] proposing several interventions at different levels of the health system listed below.
9.1 EMTCT Plus Interventions at Different Levels of the Health System
Adolescence and Pre-pregnancy
-
Diagnosis and treatment of T. cruzi-infected girls and women of childbearing age.
Pregnancy
-
Routine serological screening for HIV and syphilis as well as Chagas disease and hepatitis B (HBsAg) when part of national policy.
-
Follow-up of Chagas-seropositive pregnant women.
Childbirth
-
T. cruzi parasitological and serological screening of newborns with infected mothers.
Postnatal Period: Mothers
-
Treatment of T. cruzi-seropositive mothers after pregnancy (benznidazole or nifurtimox).
Postnatal Period: Newborns
-
T. cruzi serology of newborns with infected mothers (at 8 months).
-
Treatment of T. cruzi-seropositive children before 1 year of age (benznidazole or nifurtimox) and clinical and serological monitoring until negative.
-
Immediate treatment of all newborns with positive parasitology for T. cruzi.
Cross-Cutting Interventions
-
Chagas disease: accelerate actions to interrupt domiciliary transmission by the principal vectors.
-
Chagas disease: consider serological testing of siblings of infants infected with T. cruzi (cluster approach).
10 Conclusion
Patients with Chagas disease can be found throughout the Americas as well as in most countries in Europe. This is due to the migration of infected women who run the risk of giving birth to infected babies in non-endemic areas. There is a need for active surveillance data in order to better refine prevalence data. Also, reported rates of congenital transmission show significant geographic variability. The reasons for this variability remain unexplained to date and should be investigated. Large gaps still exist in the understanding of the role of the genetic diversity of T. cruzi, if any, on the infection, risk of disease progression, and risk of congenital transmission. The actual number of congenital cases diagnosed and treated is lower than estimated. A significant obstacle for the diagnosis and treatment of infected newborns is the lack of highly sensitive diagnostic tests applicable at an early age and the high failure rate in tracking and following up infected pregnant mothers and their offspring. The treatment with benznidazole or nifurtimox is highly effective if it is administered as early as possible. Further clinical studies are urgently needed to define the optimal dosing schedule of drugs for treatment in order to improve compliance and decrease rates of adverse events. Pharmacokinetic studies in infants have shown that lower concentrations of benznidazole have produced excellent therapeutic responses. These results suggest that older children and adults may be receiving higher doses than necessary. Dose reduction in this older population may lead to decreased ADR rates without affecting response rates, but this hypothesis still has to be formally proved in a clinical study.
It is imperative to establish strategies that will allow:
-
To systematically screen pregnant women for Chagas disease infection.
-
To systematically evaluate every child born to an infected mother.
-
To treat every infected child, as early as possible.
References
Verani JR, Montgomery SP, Schulkin J, Anderson B, Jones JL. Survey of obstetrician-gynecologists in the United States about Chagas disease. Am J Trop Med Hyg. 2010;83(4):891–5.
WHO. Chagas disease in Latin America: an epidemiological update based on 2010 estimates. Wkly Epidemiol Rec. 2015;90(6):11.
Howard EJ, Xiong X, Carlier Y, Sosa-Estani S, Buekens P. Frequency of the congenital transmission of Trypanosoma cruzi: a systematic review and meta-analysis. BJOG. 2014;121(1):22–33.
Soriano-Arandes A, Angheben A, Serre-Delcor N, Trevino-Maruri B, Gomez IPJ, Jackson Y. Control and management of congenital Chagas disease in Europe and other non-endemic countries: current policies and practices. Trop Med Int Health. 2016;21(5):590–6.
Moscatelli G, Garcia Bournissen F, Freilij H, Berenstein A, Tarlovsky A, Moroni S, et al. Impact of migration on the occurrence of new cases of Chagas disease in Buenos Aires city, Argentina. J Infect Dev Ctries. 2013;7(8):635–7.
Moscatelli G, Berenstein A, Tarlovsky A, Siniawski S, Biancardi M, Ballering G, et al. Urban Chagas disease in children and women in primary care centres in Buenos Aires, Argentina. Mem Inst Oswaldo Cruz. 2015;110(5):644–8.
Ministerio de salud A. Boletin epidemiologico anual. 2010;2010:63.
Hotez PJ. Neglected infections of poverty in the United States of America. PLoS Negl Trop Dis. 2008;2(6):e256.
Buekens P, Almendares O, Carlier Y, Dumonteil E, Eberhard M, Gamboa-Leon R, et al. Mother-to-child transmission of Chagas’ disease in North America: why don’t we do more? Matern Child Health J. 2008;12(3):283–6.
Cevallos AM, Hernandez R. Chagas’ disease: pregnancy and congenital transmission. Biomed Res Int. 2014;2014:401864.
Bittencourt AL, Barbosa HS, Rocha T, Sodre I, Sodre A. Incidence of congenital transmission of Chagas’ disease in premature births in the Maternidade Tsylla Balbino (Salvador, Bahia). Rev Inst Med Trop Sao Paulo. 1972;14(2):131–4.
Torrico F, Alonso-Vega C, Suarez E, Rodriguez P, Torrico MC, Dramaix M, et al. Maternal Trypanosoma cruzi infection, pregnancy outcome, morbidity, and mortality of congenitally infected and non-infected newborns in Bolivia. Am J Trop Med Hyg. 2004;70(2):201–9.
Duaso J, Rojo G, Cabrera G, Galanti N, Bosco C, Maya JD, et al. Trypanosoma cruzi induces tissue disorganization and destruction of chorionic villi in an ex vivo infection model of human placenta. Placenta. 2010;31(8):705–11.
Brutus L, Schneider D, Postigo J, Romero M, Santalla J, Chippaux JP. Congenital Chagas disease: diagnostic and clinical aspects in an area without vectorial transmission, Bermejo, Bolivia. Acta Trop. 2008;106(3):195–9.
Freilij H, Altcheh J. Congenital Chagas’ disease: diagnostic and clinical aspects. Clin Infect Dis. 1995;21(3):551–5.
Sanchez Negrette O, Mora MC, Basombrio MA. High prevalence of congenital Trypanosoma cruzi infection and family clustering in Salta, Argentina. Pediatrics. 2005;115(6):e668–72.
Moretti E, Basso B, Castro I, Carrizo Paez M, Chaul M, Barbieri G, et al. Chagas’ disease: study of congenital transmission in cases of acute maternal infection. Rev Soc Bras Med Trop. 2005;38(1):53–5.
Salas NA, Cot M, Schneider D, Mendoza B, Santalla JA, Postigo J, et al. Risk factors and consequences of congenital Chagas disease in Yacuiba, south Bolivia. Trop Med Int Health. 2007;12(12):1498–505.
Hermann E, Truyens C, Alonso-Vega C, Rodriguez P, Berthe A, Torrico F, et al. Congenital transmission of Trypanosoma cruzi is associated with maternal enhanced parasitemia and decreased production of interferon-gamma in response to parasite antigens. J Infect Dis. 2004;189(7):1274–81.
Kaplinski M, Jois M, Galdos-Cardenas G, Rendell VR, Shah V, Do RQ, et al. Sustained domestic vector exposure is associated with increased Chagas cardiomyopathy risk but decreased parasitemia and congenital transmission risk among young women in Bolivia. Clin Infect Dis. 2015;61(6):918–26.
Brutus L, Castillo H, Bernal C, Salas NA, Schneider D, Santalla JA, et al. Detectable Trypanosoma cruzi parasitemia during pregnancy and delivery as a risk factor for congenital Chagas disease. Am J Trop Med Hyg. 2010;83(5):1044–7.
Fabbro DL, Danesi E, Olivera V, Codebo MO, Denner S, Heredia C, et al. Trypanocide treatment of women infected with Trypanosoma cruzi and its effect on preventing congenital Chagas. PLoS Negl Trop Dis. 2014;8(11):e3312.
Moscatelli G, Moroni S, Garcia-Bournissen F, Ballering G, Bisio M, Freilij H, et al. Prevention of congenital Chagas through treatment of girls and women of childbearing age. Mem Inst Oswaldo Cruz. 2015;110(4):507–9.
Burgos JM, Altcheh J, Bisio M, Duffy T, Valadares HM, Seidenstein ME, et al. Direct molecular profiling of minicircle signatures and lineages of Trypanosoma cruzi bloodstream populations causing congenital Chagas disease. Int J Parasitol. 2007;37(12):1319–27.
Messenger LA, Miles MA, Bern C. Between a bug and a hard place: Trypanosoma cruzi genetic diversity and the clinical outcomes of Chagas disease. Expert Rev Anti-Infect Ther. 2015;13(8):995–1029.
Torrico MC, Solano M, Guzman JM, Parrado R, Suarez E, Alonzo-Vega C, et al. Estimation of the parasitemia in Trypanosoma cruzi human infection: high parasitemias are associated with severe and fatal congenital Chagas disease. Rev Soc Brasil Med Trop. 2005;38(Suppl 2):58–61.
Kemmerling U, Bosco C, Galanti N. Infection and invasion mechanisms of Trypanosoma cruzi in the congenital transmission of Chagas’ disease: a proposal. Biol Res. 2010;43(3):307–16.
Carlier Y, Truyens C. Congenital Chagas disease as an ecological model of interactions between Trypanosoma cruzi parasites, pregnant women, placenta and fetuses. Acta Trop. 2015;151:103–15.
Norman FF, Lopez-Velez R. Chagas disease and breast-feeding. Emerg Infect Dis. 2013;19(10):1561–6.
Amato Neto V, Matsubara L, Campos R, Moreira AA, Pinto PL, Faccioli R, et al. Trypanosoma cruzi in the milk of women with chronic Chagas disease. Rev Hosp Clin. 1992;47(1):10–1.
Bittencourt AL, Sadigursky M, Da Silva AA, Menezes CA, Marianetti MM, Guerra SC, et al. Evaluation of Chagas’ disease transmission through breast-feeding. Mem Inst Oswaldo Cruz. 1988;83(1):37–9.
Bern C, Martin DL, Gilman RH. Acute and congenital Chagas disease. Adv Parasitol. 2011;75:19–47.
Moya P, Moretti E, Paolasso R, Basso B, Blanco S, Sanmartino C, et al. Neonatal Chagas disease: laboratory diagnosis during the first year of life. Medicina. 1989;49(6):595–9.
Torrico F, Vega CA, Suarez E, Tellez T, Brutus L, Rodriguez P, et al. Are maternal re-infections with Trypanosoma cruzi associated with higher morbidity and mortality of congenital Chagas disease? Trop Med Int Health. 2006;11(5):628–35.
Altcheh J, Biancardi M, Lapena A, Ballering G, Freilij H. Congenital Chagas disease: experience in the Hospital de Ninos, Ricardo Gutierrez, Buenos Aires, Argentina. Rev Soc Brasil Med Trop. 2005;38(Suppl 2):41–5.
Bittencourt AL. Congenital Chagas disease. Am J Dis Child. 1976;130(1):97–103.
Azogue E, Darras C. Congenital Chagas in Bolivia: comparative study of the effectiveness and cost of diagnostic methods. Rev Soc Bras Med Trop. 1995;28(1):39–43.
Carlier Y, Sosa-Estani S, Luquetti AO, Buekens P. Congenital Chagas disease: an update. Mem Inst Oswaldo Cruz. 2015;110(3):363–8.
Bayer AM, Hunter GC, Gilman RH, Cornejo Del Carpio JG, Naquira C, Bern C, et al. Chagas disease, migration and community settlement patterns in Arequipa, Peru. PLoS Negl Trop Dis. 2009;3(12):e567.
Bittencourt AL, Mota E, Ribeiro Filho R, Fernandes LG, de Almeida PR, Sherlock I, et al. Incidence of congenital Chagas’ disease in Bahia, Brazil. J Trop Pediatr. 1985;31(5):242–8.
Bittencourt AL, Sadigursky M, Barbosa HS. Congenital Chagas’ disease. Study of 29 cases. Rev Inst Med Trop Sao Paulo. 1975;17(3):146–59.
Moya PR, Paolasso RD, Blanco S, Lapasset M, Sanmartino C, Basso B, et al. Treatment of Chagas’ disease with nifurtimox during the first months of life. Medicina. 1985;45(5):553–8.
Moya P, Basso B, Moretti E. Congenital Chagas disease in Cordoba, Argentina: epidemiological, clinical, diagnostic, and therapeutic aspects. Experience of 30 years of follow up. Rev Soc Brasil Med Trop. 2005;38(Suppl 2):33–40.
Zaidenberg M. Congenital Chagas’ disease in the province of Salta, Argentina, from 1980 to 1997. Rev Soc Bras Med Trop. 1999;32(6):689–95.
Freilij H, Altcheh J, Muchinik G. Perinatal human immunodeficiency virus infection and congenital Chagas’ disease. Pediatr Infect Dis J. 1995;14(2):161–2.
WHO EC. Control of Chagas disease. World Health Organization technical report series. Brussels: WHO EC; 2002. 905:i-vi, 1–109, back cover
Carlier Y, Torrico F, Sosa-Estani S, Russomando G, Luquetti A, Freilij H, et al. Congenital Chagas disease: recommendations for diagnosis, treatment and control of newborns, siblings and pregnant women. PLoS Negl Trop Dis. 2011;5(10):e1250.
Fernandez-Aguilar S, Lambot MA, Torrico F, Alonso-Vega C, Cordoba M, Suarez E, et al. Placental lesions in human Trypanosoma cruzi infection. Rev Soc Brasil Med Trop. 2005;38(Suppl 2):84–6.
Duffy T, Bisio M, Altcheh J, Burgos JM, Diez M, Levin MJ, et al. Accurate real-time PCR strategy for monitoring bloodstream parasitic loads in chagas disease patients. PLoS Negl Trop Dis. 2009;3(4):e419.
Schijman AG, Altcheh J, Burgos JM, Biancardi M, Bisio M, Levin MJ, et al. Aetiological treatment of congenital Chagas’ disease diagnosed and monitored by the polymerase chain reaction. J Antimicrob Chemother. 2003;52(3):441–9.
Messenger LA, Gilman RH, Verastegui M, Galdos-Cardenas G, Sanchez G, Valencia E, et al. Toward improving early diagnosis of congenital Chagas disease in an endemic setting. Clin Infect Dis. 2017;65(2):268–75.
Bern C, Verastegui M, Gilman RH, Lafuente C, Galdos-Cardenas G, Calderon M, et al. Congenital Trypanosoma cruzi transmission in Santa Cruz, Bolivia. Clin Infect Dis. 2009;49(11):1667–74.
Oliveira I, Torrico F, Munoz J, Gascon J. Congenital transmission of Chagas disease: a clinical approach. Expert Rev Anti-Infect Ther. 2010;8(8):945–56.
Besuschio SA, Llano Murcia M, Benatar AF, Monnerat S, Cruz I, Picado A, et al. Analytical sensitivity and specificity of a loop-mediated isothermal amplification (LAMP) kit prototype for detection of Trypanosoma cruzi DNA in human blood samples. PLoS Negl Trop Dis. 2017;11(7):e0005779.
Rivero R, Bisio M, Velazquez EB, Esteva MI, Scollo K, Gonzalez NL, et al. Rapid detection of Trypanosoma cruzi by colorimetric loop-mediated isothermal amplification (LAMP): a potential novel tool for the detection of congenital Chagas infection. Diagn Microbiol Infect Dis. 2017;89(1):26–8.
Leguizamon MS, Campetella OE, Reyes MB, Ibanez CF, Basombrio MA, Rincon J, et al. Bloodstream Trypanosoma cruzi parasites from mice simultaneously express antigens that are markers of acute and chronic human Chagas disease. Parasitology. 1991;102(Pt 3):379–85.
Reyes MB, Lorca M, Munoz P, Frasch AC. Fetal IgG specificities against Trypanosoma cruzi antigens in infected newborns. Proc Natl Acad Sci U S A. 1990;87(7):2846–50.
Mallimaci MC, Sosa-Estani S, Russomando G, Sanchez Z, Sijvarger C, Alvarez IM, et al. Early diagnosis of congenital Trypanosoma cruzi infection, using shed acute phase antigen, in Ushuaia, Tierra del Fuego, Argentina. Am J Trop Med Hyg. 2010;82(1):55–9.
Altcheh J, Corral R, Biancardi MA, Freilij H. Anti-F2/3 antibodies as cure marker in children with congenital Trypanosoma cruzi infection. Medicina. 2003;63(1):37–40.
de Andrade AL, Zicker F, de Oliveira RM, Almeida Silva S, Luquetti A, Travassos LR, et al. Randomised trial of efficacy of benznidazole in treatment of early Trypanosoma cruzi infection. Lancet. 1996;348(9039):1407–13.
Chippaux JP, Clavijo AN, Santalla JA, Postigo JR, Schneider D, Brutus L. Antibody drop in newborns congenitally infected by Trypanosoma cruzi treated with benznidazole. Trop Med Int Health. 2010;15(1):87–93.
Sosa-Estani S, Segura EL. Etiological treatment in patients infected by Trypanosoma cruzi: experiences in Argentina. Curr Opin Infect Dis. 2006;19(6):583–7.
Sosa Estani S, Segura EL, Ruiz AM, Velazquez E, Porcel BM, Yampotis C. Efficacy of chemotherapy with benznidazole in children in the indeterminate phase of Chagas’ disease. Am J Trop Med Hyg. 1998;59(4):526–9.
Rubio M, Donoso F. Enfermedad de Chagas en niños y tratamiento con Bay 2502. Bol Chile Parasitol. 1969;24:43–8.
Russomando G, de Tomassone MM, de Guillen I, Acosta N, Vera N, Almiron M, et al. Treatment of congenital Chagas’ disease diagnosed and followed up by the polymerase chain reaction. Am J Trop Med Hyg. 1998;59(3):487–91.
Blanco SB, Segura EL, Cura EN, Chuit R, Tulián L, et al. Congenital transmisión of Trypanosoma cruzi: and operational outline for detecting and treating infected infants in north-western Argentina. Trop Med Int Health. 2000;5:293–301.
Chippaux JP, Clavijo AN, Santalla JA, Postigo JR, Schneider D, Brutus L. Antibody drop in newborns congenitally infected by Trypanosoma cruzi treated with benznidazole. Trop Med Int Health. 2010;15:87–93.
Altcheh J, Moscatelli G, Mastrantonio G, Moroni S, Giglio N, Marson ME, et al. Population pharmacokinetic study of benznidazole in pediatric Chagas disease suggests efficacy despite lower plasma concentrations than in adults. PLoS Negl Trop Dis. 2014;8(5):e2907.
Balouz V, Melli LJ, Volcovich R, Moscatelli G, Moroni S, González N, Ballering G, Bisio M, Ciocchini AE, Buscaglia CA, Altcheh J. The trypomastigote small surface antigen from trypanosoma cruzi improves treatment evaluation and diagnosis in pediatric chagas disease. J Clin Microbiol. 2017;55:3444–53.
Chippaux JP, Salas-Clavijo AN, Postigo JR, Schneider D, Santalla JA, Brutus L. Evaluation of compliance to congenital Chagas disease treatment: results of a randomised trial in Bolivia. Trans R Soc Trop Med Hyg. 2013;107(1):1–7.
Lescure FX, Le Loup G, Freilij H, Develoux M, Paris L, Brutus L, et al. Chagas disease: changes in knowledge and management. Lancet Infect Dis. 2010;10(8):556–70.
Altcheh J, Moscatelli G, Moroni S, Garcia-Bournissen F, Freilij H. Adverse events after the use of benznidazole in infants and children with Chagas disease. Pediatrics. 2011;127(1):e212–8.
Murcia L, Simon M, Carrilero B, Roig M, Segovia M. Treatment of Infected Women of Childbearing Age Prevents Congenital Trypanosoma cruzi Infection by Eliminating the Parasitemia Detected by PCR. J Infect Dis. 2017;215(9):1452–8.
PAHO/WHO. Strategy and plan of action for Chagas disease prevention, control and care. Washington, DC: PAHO; 2010. p. CE146/14.
PAHO. EMTCT plus. Framework for elimination of mother-to-child transmission of HIV, syphilis, hepatitis B, and Chagas. Washington, DC: PAHO PAHO; 2017. p. 17–009.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Altcheh, J.M. (2019). Congenital Chagas Disease. In: Altcheh, J., Freilij, H. (eds) Chagas Disease. Birkhäuser Advances in Infectious Diseases. Springer, Cham. https://doi.org/10.1007/978-3-030-00054-7_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-00054-7_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-00053-0
Online ISBN: 978-3-030-00054-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)