Abstract
The lymphatic system has a critical role in the immune system’s recognition and response to disease, and it is an additional circulatory system throughout the entire body. Most solid cancers primarily spread from the main site via the tumour’s surrounding lymphatics before haematological dissemination. Targeting drugs to lymphatic system is quite complicated because of its intricate physiology. Therefore, it tends to be an important target for developing novel therapeutics. Currently, nanocarriers have encouraged the lymphatic targeting, but still there are challenges of locating drugs and bioactives to specific sites, maintaining desired action and crossing all the physiological barriers. Lymphatic therapy using drug-encapsulated colloidal carriers especially liposomes and solid lipid nanoparticles emerges as a new technology to provide better penetration into the lymphatics where residual disease exists. Optimising the proper procedure, selecting the proper delivery route and target area and making use of surface engineering tool, better carrier for lymphotropic system can be achieved. Thus, new methods of delivering drugs and other carriers to lymph nodes are currently under investigation.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Human Immunodeficiency Virus
- Sentinel Lymph Node
- Lymphatic Vessel
- Lymphatic System
- Solid Lipid Nanoparticles
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
1.1 Development of the Lymphatic Vascular System
The lymphatic system was first recognised by Gaspare Aselli in 1627, and the anatomy of the lymphatic system was almost completely characterised by the early nineteenth century. However, knowledge of the blood circulation continued to grow rapidly in the last century [1]. Two different theories are proposed which are in favour of origin of the lymphatic vessels. Firstly, centrifugal theory of embryologic origin of the lymphatics was described in the early twentieth century by Sabin and later by Lewis, postulating that lymphatic endothelial cells (LECs) are derived from the venous endothelium. Later the centripetal theory of lymphatic development was proposed by Huntington and McClure in 1910 which describes the development of the lymphatic system beginning with lymphangioblasts, mesenchymal progenitor cells, arising independently of veins. The venous connection to the lymphatic system then happens later in development [2].
The lymphatic vessels in the embryo are originated at mid-gestation and are developed after the cardiovascular system is fully established and functional [3]. A dual origin of lymphatic vessels from embryonic veins and mesenchymal lymphangioblasts is also proposed [4]. Recent studies provide strong support of the venous origin of lymphatic vessels [5–8]. The recent discovery of various molecular markers has allowed for more in-depth research of the lymphatic system and its role in health and disease. The lymphatic system has recently been elucidated as playing an active role in cancer metastasis. The knowledge of the active processes involved in lymphatic metastasis provides novel treatment targets for various malignancies.
1.2 Anatomy and Physiology of the Lymphatic System
The lymphatic system consists of the lymphatic vessels, lymph nodes, spleen, thymus, Peyer’s patches and tonsils, which play important roles in immune surveillance and response. The lymphatic system serves as the body’s second vascular system in vertebrates and functions co-dependently with the cardiovascular system [9, 10]. The lymphatic system comprises a single irreversible, open-ended transit network without a principal driving force [9]. It consists of five main types of conduits including the capillaries, collecting vessels, lymph nodes, trunks and ducts. The lymphatic system originates in the dermis with initial lymphatic vessels and blind-ended lymphatic capillaries that are nearly equivalent in size to but less abundant than regular capillaries [9, 11]. Lymphatic capillaries consist of a single layer of thin-walled, non-fenestrated lymphatic endothelial cells (LECs), alike to blood capillaries. The LECs, on the contrary to blood vessels, have poorly developed basement membrane and lack tight junctions and adherent junctions too. These very porous capillaries act as gateway for large particles, cells and interstitial fluid. Particles as large as 100 nm in diameter can extravasate into the interstitial space, get phagocytosed by macrophages and are ultimately passed on to lymph nodes [11–14]. Lymphatic capillary endothelial cells are affixed to the extracellular matrix by elastic anchoring filaments, which check vessel collapse under high interstitial pressure. These initial lymphatics, under a positive pressure gradient, distend and create an opening between loosely anchored endothelial cells letting for the entry of lymph, a protein-rich exudate from the blood capillaries [12, 15, 16]. In initial lymphatic vessels, overlying endothelial cell–cell contacts prevent fluid reflux back into the interstitial space [17, 18].
After the collection of lymph by the lymphatic capillaries, it is transported through a system of converging lymphatic vessels of progressively larger size, is filtered through lymph nodes where bacteria and particulate matter are removed and finally goes back to the blood circulation. Lymph is received from the initial capillary lymphatic by deeper collecting vessels that contain valves to maintain unidirectional flow of lymph. These collecting vessels have basement membranes and are surrounded by smooth muscle cells with intrinsic contractile activity that in combination with contraction of surrounding skeletal muscles and arterial pulsations propels the lymph to lymph nodes [19–21]. The collecting lymphatic vessels unite into lymphatic trunks, and the lymph is finally returned to the venous circulation via the thoracic duct into the left subclavian vein [22, 23]. The flow of lymph toward the circulatory system is supported by increases in interstitial pressure as well as contractions of the lymphatic vessels themselves. Roughly 25 l of lymphatic fluid enters the cardiovascular system each day [11].
1.3 Need for Lymphatic Targeting
The key functions of the lymphatic system are maintenance of normal tissue fluid balance, absorption of lipids and fat-soluble vitamins from the intestine and magnetism and transport of immune cells. Lymphatics transport the antigen-presenting cells as well as antigens from the interstitium of peripheral tissues to the draining lymph nodes where they initiate immune responses via B- and T-cells in the lymph nodes [9, 12, 24, 25]. Tissue fluid balance is maintained by restoring interstitial fluid to the cardiovascular system [9]. Although capillaries have very low permeability to proteins, these molecules as well as other macromolecules and bacteria accumulate in the interstitium. Due to the accumulation of these large molecules in the interstitium, significant tissue oedema would result. The lymphatic system offers the mechanism by which these large molecules re-enter the blood circulation [26]. The lymphatic system is the site of many diseases such as metastitial tuberculosis (TB), cancer and filariasis [27]. Due to the peculiar nature and anatomy of the lymphatic system, localisation of drugs in the lymphatics has been particularly difficult to achieve.
The lymphatic system has an active role in cancer metastasis. Although many cancers may be treated with surgical resection, microscopic disease may remain and lead to locoregional recurrence. Conventional systemic chemotherapy cannot prove effective for delivering drugs to the lymphatic system without dose-limiting toxicities [28]. Lymphatic system functions in the clearance of particulate matter from the interstitium following presentation to lymph nodes have created interest in developing microparticulate systems to target regional lymph nodes. Molecule’s composition is important in determining uptake into the lymphatics and retention within the lymph nodes. Colloidal materials, for example, liposomes, activated carbon particles, emulsions, lipids and polymeric particulates, are highly taken up by the lymphatics; that’s why nowadays these substances are emerging as potential carriers for lymphatic drug targeting [29]. The vast majority of drugs following oral administration are absorbed directly into portal blood, but a number of lipophilic molecules may get access to the systemic circulation via the lymphatic pathway [30, 31]. Intestinal lymphatic transport of lipophilic molecules is significant and presents benefits in a number of situations:
-
1.
The total systemic bioavailability of lipophilic molecules may be increased, and the hepatic first-pass metabolism may be reduced by the intestinal lymphatic absorption [30].
-
2.
Targeting immunomodulatory agents, cytotoxic agents and drugs used in the treatment of human immunodeficiency virus (HIV) to the lymphatic system has a potential to maximise therapeutic benefits and minimise systemic exposure [30, 32].
-
3.
Following association of the drug with chylomicrons, intestinal lymphatic transport may alter the pharmacokinetic and the pharmacodynamic properties of the drug [32–35].
The lymphatic system also acts as the primary systemic transport pathway for B- and T-lymphocytes as well as the main route of metastatic spread of a number of solid tumours [36, 37]. Therefore, lymphatic absorption of the immunomodulatory and anticancer compounds may be more effective [38, 39]. The presence of wide amounts of HIV-susceptible immune cells in the lymphoid organs makes antiretroviral drug targeting to these sites of tremendous interest in HIV therapy. This strategy comprises once again targeting nanosystems to immune cell populations, particularly macrophages. Also evidence further suggests that lymph and lymphoid tissue, and in particular gut-associated lymphoid tissue, play a major role in the development of HIV and antivirals which target acquired immunodeficiency syndrome (AIDS) may therefore be more effective when absorbed via the intestinal lymphatics [40, 41]. Other viruses like hepatitis B [42] and morbillivirus [43] (which also replicate in gut-associated lymphoid tissue) and the closely related canine distemper virus [44] including severe acute respiratory syndrome (SARS)-associated coronavirus [45] may also spread via the lymphatic network, and the chronic persistence of hepatitis C is believed to result from uptake into systemic lymphocytes and sequestration into the lymph [46].
Targeting drugs to lymphatic system is a tough and challenging task, and it totally depends upon the intricate physiology of the lymphatic system. Targeting facilitates direct contact of drug with the specific site, decreasing the dose of the drugs and minimising the side effects caused by them. Currently, nanocarriers have encouraged the lymphatic targeting, but still there are challenges of locating drugs and bioactives to specific sites, maintaining desired action and crossing all the physiological barriers. These hurdles could be overcome by the use of modified nanosystems achieved by the surface engineering phenomena.
2 Targets for Lymphatic Delivery
From the growing awareness of the importance of lymph nodes in cancer prognosis, their significance for vaccine immune stimulation and the comprehension that the lymph nodes harbour HIV as well as other infectious diseases stems the development of new methods of lymph node drug delivery [47–50]. New methods of delivering drugs and other carriers to lymph nodes are currently under investigation.
2.1 Cancer
Lymph node dissemination is the primary cause of the spread of majority of solid cancers [51]. In regard to cancer metastasis, the status of the lymph node is a major determinant of the patient’s diagnosis. The most important factor that determines the appropriate care of the patient is correct lymph node staging [52]. But patient survivals have been shown to improve by the therapeutic interventions that treat metastatic cancer in lymph nodes with either surgery or local radiation therapy [53].
2.2 Human Immunodeficiency Virus
Viraemia is an early indication of primary infection with HIV followed by a specific HIV immune response and a dramatic decline of virus in the plasma [54]. Long after the HIV virus can be found in the blood, HIV can be found in high levels in mononuclear cells located in lymph nodes. Viral replication in these lymph nodes has been reported to be about 10- to 100-fold higher than in the peripheral blood mononuclear cells [55]. Standard oral or intravenous drug delivery to these lymph node mononuclear cells is difficult [56]. Even if highly active antiretroviral therapy (HAART) can reduce plasma viral loads in HIV-infected patients by 90 %, active virus can still be isolated from lymph nodes even after 30 months of HAART therapy.
2.3 Filaria
Lymph nodes are the key element of the life cycle of several parasite organisms, including filaria. Lymphatic vessels and lymph nodes of infected patients can carry adult worms. This adult filaria obstructs the lymphatic drainage that results into swelling of extremities that are distal to the infected lymph node. These very symptoms of swollen limbs in patients with filarial disease have been termed elephantiasis. The eradication of adult worms in lymph nodes is not frequently possible, and commonly a much extended course of medical therapy is required for it to be successful [57].
2.4 Anthrax
New methods of curing anthrax have become a burning interest following the recent outburst of anthrax infections and deaths in the USA as a result of terrorism. In anthrax infection, endospores from Bacillus anthracis that gain access into the body are phagocytosed by macrophages and carried to regional lymph nodes where the endospores germinate inside the macrophages and become vegetative bacteria [58]. According to one literature, computed tomography of the chest was performed on eight patients infected with inhalational anthrax. Mediastinal lymphadenopathy was found in seven of the eight patients [59]. In another case report of a patient, the anthrax bacillus was shown to be rapidly sterilised within the blood stream after initiation of antibiotic therapy. However, viable anthrax bacteria were still present in postmortem mediastinal lymph node specimens [60]. Treatment and control of these diseases are hard to accomplish because of the limited access of drugs to mediastinal nodes using common pathways of drug delivery. Also, the anatomical location of mediastinal nodes represents a difficult target for external beam irradiation.
2.5 Tuberculosis
Newer methods to target antituberculosis drugs to these lymph nodes could possibly decrease the amount of time of drug therapy. TB requires lengthy treatment minimum of approximately 6 months probably because of its difficulty in delivering drugs into the tubercular lesions.
The TB infection is caused by mycobacteria that invade and grow chiefly in phagocytic cells. Lymph node TB is the most common form of extrapulmonary TB rating approximately as 38.3 %. This is frequently found to spread from the lungs to lymph nodes. In one study, total TB lymph node involvement was found as 71 % of the intrathoracic lymph nodes, 26 % of the cervical lymph nodes and 3 % of the axillary lymph nodes [61].
3 Approaches for Lymphatic Targeting
Targeted delivery of drugs can be achieved utilising carriers with a specified affinity to the target tissue. There are two approaches for the targeting, i.e. passive and active. In passive targeting, most of the carriers accumulate to the target site during continuous systemic circulation to deliver the drug substance, the behaviour of which depends highly upon the physicochemical characteristics of the carriers. Whereas much effort has been concentrated on active targeting, this involves delivering drugs more actively to the target site.
3.1 Passive Targeting
Passive targeting involves the transport of carriers through leaky tumour vasculature into the tumour interstitium and cells by convection or passive diffusion. Further, nanocarriers and drug then accumulate at the target site by the enhanced permeation and retention (EPR) effect [62]. The EPR effect is most prominent mainly in cancer targeting. Moreover, the EPR effect is pertinent for about all fast-growing solid tumours [63]. The EPR effect will be most positive if nanocarriers can escape immune surveillance and circulate for a long period. Very high local concentrations of drug-loaded nanocarriers can be attained at the target site, for example, about 10- to 50-fold higher than in normal tissue within 1–2 days [64].
However, there exist some limitations for passively targeting the tumour; first is the degree of tumour vascularisation and angiogenesis which is important for passive targeting of nanocarriers [65]. And, second, due to the poor lymphatic drainage in tumours, the interstitial fluid pressure increases which correlates nanocarrier size relationship with the EPR effect: larger and long-circulating nanocarriers (100 nm) are more retained in the tumour, whereas smaller molecules easily diffuse [66].
3.2 Active Targeting
Active targeting is based upon the attachment of targeting ligands on the surface of the nanocarrier for appropriate receptor binding that are expressed at the target site. The ligand particularly binds to a receptor overexpressed in particular diseased cells or tumour vasculature and not expressed by normal cells. In addition, targeted receptors should be present uniformly on all targeted cells. Targeting ligands are either monoclonal antibodies (mAbs) and antibody fragments or non-antibody ligands (peptidic or not). These can also be termed as ligand-targeted therapeutics [67, 68]. Targeting approaches for lymphatic targeting are shown in Fig. 20.1.
4 Carriers for Lymphatic Targeting
Current research is focussed on two types of carriers, namely, colloidal carriers and polymeric carriers. Targeting strategies for lymphatics are shown in Fig. 20.2.
4.1 Colloidal Carriers
Much effort has been concentrated to achieve lymphatic targeting of drugs using colloidal carriers. The physicochemical nature of the colloid itself has been shown to be of particular relevance, with the main considerations being size of colloid and hydrophobicity. The major purpose of lymphatic targeting is to provide an effective anticancer chemotherapy to prevent the metastasis of cancer cells by accumulating the drug in the regional lymph node.
4.1.1 Emulsifying Drug Delivery Systems
Emulsions are probably well-known particulate carriers with comparative histories of research and have been widely used as a carrier for lymph targeting. Hashida et al. demonstrated that injection of water-in-oil (W/O) or oil-in-water (O/W) emulsions favoured lymphatic transport of mitomycin C via the intraperitoneal and intramuscular routes and uptake into the regional lymphatics was reported in the order of O/W > W/O > aqueous solution. The nanoparticle-in-oil emulsion system, containing anti-filarial drug in gelatin nanoparticles, was studied for enhancing lymphatic targeting [69]. Pirarubicin and Lipiodol emulsion formulation was developed for treating gastric cancer and metastatic lymph nodes [70, 71]. After endoscopic injection of the pirarubicin–Lipiodol emulsion, the drug retained over 7 days at the injection site and in the regional lymph node.
Hauss et al. in their study have explored the lymphotropic potential of emulsions and self-emulsifying drug delivery systems (SEDDS). They investigated the effects of a range of lipid-based formulations on the bioavailability and lymphatic transport of ontazolast following oral administration to conscious rats and found that all the lipid formulations increased the bioavailability of ontazolast comparative to the control suspension, the SEDDS promoted more rapid absorption and maximum lymphatic transport is found with the emulsion [72, 73].
4.1.2 Liposomes
Lymphatic delivery of drug-encapsulated liposomal formulations has been investigated extensively in the past decade. Liposomes possess ideal features for delivering therapeutic agents to the lymph nodes which are based on their size, which prevents their direct absorption into the blood; the large amount of drugs and other therapeutic agents that liposomes can carry; and their biocompatibility. The utility of liposomes as a carrier for lymphatic delivery was first investigated by Segal et al. in 1975 [74].
Orally administered drug-incorporated liposomes enter the systemic circulation via the portal vein and intestinal lymphatics. Drugs entering the intestinal lymphatic through the intestinal lumen avoid liver and first-pass metabolism as they first migrate to lymphatic vessels and draining lymph nodes before entering systemic circulation. Lymphatic uptake of carriers via the intestinal route increases bioavailability of a number of drugs. For oral delivery of drug-encapsulated liposomal formulations, intestinal absorbability and stability are the primary formulation concerns. Ling et al. evaluated oral delivery of a poorly bioavailable hydrophilic drug, cefotaxime, in three different forms: liposomal formulation, aqueous-free drug and a physical mixture of the drug and empty liposomes [75]. The liposomal formulation of the drug turned out to exhibit a 2.7-fold increase in its oral bioavailability compared to the aqueous dosage and a 2.3-fold increase for the physical mixture. They also accounted that the liposomal formulation leads to a significant enhancement of the lymphatic localisation of the drug relative to the other two formulations. As a result, liposome systems emerged as useful carriers for poorly bioavailable hydrophilic drugs, promoting their lymphatic transport in the intestinal lymph as well as their systemic bioavailability.
Conventional liposomal formulations contain anticancer drugs incorporated in them for intravenous infusion in treating various types of cancers. Doxil, a chemotherapeutic formulation of PEGylated liposomes of doxorubicin, is widely used as first-line therapy of AIDS-related Kaposi’s sarcoma, breast cancer, ovarian cancer and other solid tumours [76–80]. Liposomal delivery of anticancer drug actinomycin D via intratesticular injection has shown greater concentration of the drug in the local lymph nodes. Furthermore, a study by Hirnle et al. found liposomes as a better carrier for intralymphatically delivered drugs contrasted with bleomycin emulsions [81]. Systemic liposomal chemotherapy is preferred mainly because of its reduced side effects compared to the standard therapy and improved inhibition of the anticancer drugs from enzymatic digestion in the systemic circulation. Effective chemotherapy by pulmonary route could overcome various lacunas associated with systemic chemotherapy like serious non-targeted toxicities, poor drug penetration into the lymphatic vessels and surrounding lymph node and first-pass clearance concentrating drugs in the lungs and draining lymphatics in the case of oral delivery.
Latimer et al. developed liposomes of paclitaxel and a vitamin E analogue α-tocopheryloxy acetic acid (α-TEA) in an aerosol formulation for treating murine mammary tumours and metastases [82]. Similarly, Lawson et al. performed a comparative study for the anti-proliferative efficacy of a 9-nitro-camptothecin (9-NC)-encapsulated dilauroylphosphatidylcholine liposomal delivery, α-TEA and a combination therapy of 9-NC and α-TEA, in a metastatic murine mammary tumour model. Liposome-encapsulated individual as well as combination treatment was delivered via an aerosol for curing metastases of lungs and of the surrounding lymph node. The animals treated with the combination therapy were found to have less proliferative cells compared to the animals treated with 9-NC alone when immunostained with Ki-67. The in vivo anticancer efficacy studies demonstrated that the combination treatment greatly hindered the tumour progression compared to each treatment alone, leading to the prolonged survival rate [83]. High levels of drugs could be targeted to lymph nodes containing TB using liposomal antituberculosis drug therapy [84].
Deep lung lymphatic drainage could also be visualised using 99mTc radioactive marker-incorporated liposomes. In addition, Botelho et al. delivered aerosolised nanoradioliposomal formulation to wild boars and observed their deep lung lymphatic network and surrounding lymph nodes [85]. Also, this technique has offered new information of the complicated structure of lymphatic network and has emerged as a new and non-invasive molecular imaging technique for the diagnosis of early dissemination of lung cancers as compared to the conventional computed tomography.
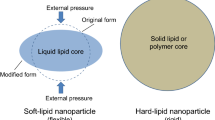
4.1.3 Solid Lipid Nanoparticles
Solid lipid nanoparticles (SLN) could be a good formulation strategy for incorporating drugs with poor oral bioavailability due to low solubility in GI tract or pre-systemic hepatic metabolism (first-pass effect) permitting transportation into the systemic circulation through the intestinal lymphatics. Bargoni et al. have performed various studies on absorption and distribution of SLN after duodenal administration [86–89]. In one study, 131I-17-iodoheptadecanoic acid-labelled drug-free SLN were delivered into the duodenal lumen of fed rats, and transmission electron microscopy and photon correlation spectroscopy results of the lymph and blood samples verified the transmucosal transport of SLN [86].
In a later study of tobramycin-loaded SLN after duodenal administration, the improvement of drug absorption and bioavailability was ascribed mostly to the favoured transmucosal transport of SLN to the lymph compared to the blood [88]. The same group conducted a study using idarubicin-loaded SLN, administered via the duodenal route rather than intravenous route, and observed enhancement in drug bioavailability [89].
Reddy et al. prepared etoposide-loaded tripalmitin (ETPL) SLN radiolabelled with 99mTc and administered the ETPL nanoparticles subcutaneously, intraperitoneally and intravenously, to mice bearing Dalton’s lymphoma tumours, and 24 h after subcutaneous administration, gamma scintigraphy and the radioactivity measurements showed that the ETPL SLN revealed a clearly higher degree of tumour uptake given via subcutaneous route (8- and 59-fold higher than that of the intraperitoneal and intravenous routes, respectively) and reduced accumulation in reticuloendothelial system organs [90].
Targeting therapies are of great potential in small cell lung cancer considering intrathoracic lymph node metastasis occurring in approximately 70 % of the limited stage patients and to nearly 80 % of the extensive stage patients [91]. Considering the case of non-small cell lung cancer, extensive rate of metastasis of lymphatics is seen in greater than 80 % of stage IV patients [92]. Videira et al. compared the biodistribution of inhaled 99mTc-d,l-hexamethylpropyleneamine oxime (HMPAO)-radiolabelled SLN with that of the free tracer administered through the same route, and gamma scintigraphic results specified that the radiolabelled SLN were primarily cleared from lungs via the lymphatics [93, 94].
4.1.4 Nanocapsules
Nanocapsules tend to be the most promising approach for lymphatic targeting because of their possibility of attaining distinct qualities with an easy manufacturing process. Nanocapsules coated with hydrophobic polymers could be easily captured by lymphatic cells in the body, when administered, because the hydrophobic particle is generally recognised as a foreign substance. The lymphatic targeting ability of poly(isobutylcyanoacrylate) nanocapsules encapsulating 12-(9-anthroxy) stearic acid upon intramuscular administration was evaluated and compared with three conventional colloidal carriers [69]. In vivo study in rats proved that poly(isobutylcyanoacrylate) nanocapsules retained in the right iliac regional lymph nodes in comparison with other colloidal carriers following intramuscular administration.
4.2 Polymeric Carriers
For effective targeted and sustained delivery of drugs to lymph, several polymeric particles have been designed and studied. The polymers are categorised in two types based on their origin either natural polymers like dextran, alginate, chitosan, gelatin, pullulan and hyaluronan or synthetic polymers like PLGA, PLA and PMMA.
4.2.1 Natural
Dextran a natural polysaccharide has been used as a carrier for a range of drug molecules due to its outstanding biocompatibility. Bhatnagar et al. synthesised cyclosporine A-loaded dextran acetate particles labelled with 99mTc. These particles gradually distributed cyclosporine A all through the lymph nodes following subcutaneous injection into the footpad of rats [95]. Dextran (average molecular weights of 10, 70 and 500 kDa)-conjugated lymphotropic delivery system of mitomycin C has been studied and it was reported that after intramuscular injection in mice, this mitomycin C–dextran conjugates retained for a longer period in regional lymph nodes for nearly 48 h while the free mitomycin was quickly cleared.
Hyaluronan, also called as hyaluronic acid, is a natural biocompatible polymer that follows lymphatic drainage from the interstitial spaces. Cai et al. demonstrated a novel intralymphatic drug delivery method synthesising a cisplatin–hyaluronic acid conjugate for breast cancer treatment. Following subcutaneous injection into the upper mammary fat pad of female rats, most of the carrier localised in the regional nodal tissue compared to the standard cisplatin formulation [96].
4.2.2 Synthetic
Poly(lactide-co-glycolide) as synthetic polymer that is used to prepare biodegradable nanospheres has been accounted to deliver drugs and diagnostic agents to the lymphatic system. Similarly, nanospheres coated with block copolymers of poloxamers and poloxamines with radiolabelled 111In-oxine are used to trace the nanoparticles in vivo. Upon s.c. injection, the regional lymph node showed a maximum uptake of 17 % of the administered dose [97].
Dunne et al. synthesised a conjugate of block copolymer cis-diamminedichloro-platinum(II) (CDDP) and poly(ethylene oxide)-block-poly(lysine) (PEO-b-PLys) for treating lymph node metastasis. One animal treatment with 10 wt.% CDDP–polymer resulted into limited tumour growth in the draining lymph nodes and prevention of systemic metastasis [98]. Johnston and coworkers designed a biodegradable intrapleural (ipl) implant of paclitaxel consisting gelatin sponge impregnated with poly(lactide-co-glycolide) (PLGA–PTX) for targeting thoracic lymphatics. In rat model, this system exhibited lymphatic targeting capability and showed sustained drug release properties [99].
Kumanohoso et al. designed a new drug delivery system for bleomycin by loading it into a small cylinder of biodegradable polylactic acid to target lesions. This system showed significantly higher antitumour effect compared to bleomycin solution and no treatment [100]. To treat lesions, a new biodegradable colloidal particulate-based nanocarrier system was designed to target thoracic lymphatics and lymph nodes. Various nano- and microparticles of charcoal, polystyrene and poly(lactide-co-glycolide) were studied for the lymphatic distribution after intrapleural implantation in rats, and after 3 h of intrapleural injection, the lymphatic uptake was observed [101].
4.3 Miscellaneous Carriers
4.3.1 Dendrimers
Kobayashi et al. utilised dendrimer-based contrast agents for dynamic magnetic resonance lymphangiography [102]. Gadolinium (Gd)-containing dendrimers of different sizes and molecular structures (PAMAM-G8, PAMAM-G4 and DAB-G5) (PAMAM, polyamidoamine; DAB, diaminobutyl) are used as contrast agents. Size and molecular structure play a great role in distribution and pharmacokinetics of dendrimers. For example, PAMAM-G8 when injected intravenously had a comparatively long life in the circulatory system with minimum leakage out of the vessels, whereas PAMAM-G4 cleared rapidly from the systemic circulation due to rapid renal clearance but had immediate survival in lymphatic circulation. The smaller-sized DAB-G5 showed greater accumulation and retention in lymph nodes useful for lymph node imaging using MR-LG. Gadomer-17 and Gd-DTPA–dimeglumine (Magnevist) were evaluated as controls. Imaging experiments revealed that all of the reagents are able to visualise the deep lymphatic system except Gd-DTPA–dimeglumine. To visualise the lymphatic vessels and lymph nodes, PAMAM-G8 and DAB-G5 were used, respectively. While PAMAM-G4 provided good contrast of both the nodes and connecting vessels, Gadomer-17 was able to visualise lymph nodes, but not as clear as Gd-based dendrimers. Kobayashi also delivered various Gd-PAMAM (PAMAM-G2, PAMAM-G4, PAMAM-G6, PAMAM-G8) and DAB-G5 dendrimers to the sentinel lymph nodes and evaluated its visualisation with other nodes. The G6 dendrimer provided excellent opacification of sentinel lymph nodes and was able to be absorbed and retained in the lymphatic system [103].
Using a combination of MRI and fluorescence with PAMAM-G6-Gd-Cy, the sentinel nodes were more clearly observed signifying the potential of the dendrimers as platform for dual imaging. Kobayashi et al. further overcame the sensitivity limitation and depth limitations of each individual method by the simultaneous use of two modalities (radionuclide and optical imaging). Making use of PAMAM-G6 dendrimers conjugated with near-infrared (NIR) dyes and an 111In radionuclide probe, multimodal nanoprobes were developed for radionuclide and multicolour optical lymphatic imaging [104, 105].
Later Kobayashi also proposed the use of quantum dots for labelling cancer cells and dendrimer-based optical agents for visualising lymphatic drainage and identifying sentinel lymph nodes [106]. Polylysine dendrimers have been best used for targeting the lymphatic system and lymph nodes.
4.3.2 Carbon Nanotubes
Carbon nanotubes (CNT) possess various mechanochemical properties like high surface area, mechanical strength and thermal and chemical stability which cause them to be versatile carriers for drugs, proteins, radiologicals and peptides to target tumour tissues. Hydrophilic multiwalled carbon nanotubes (MWNTs) coated with magnetic nanoparticles (MN-MWNTs) have emerged as an effective delivery system for lymphatic targeting following subcutaneous injection of these particles into the left footpad of Sprague Dawley rats; the left popliteal lymph nodes were dyed black. MN-MWNTs were favourably absorbed by lymphatic vessels following their transfer into lymph nodes and no uptake was seen in chief internal organs such as the liver, spleen, kidney, heart and lungs. Gemcitabine loaded in these particles was evaluated for its lymphatic delivery efficiency and MN-MWNTs–gemcitabine displayed the maximum concentration of gemcitabine in the lymph nodes [107]. McDevitt et al. synthesised tumour-targeting water-soluble CNT constructs by covalent attachment of monoclonal antibodies like rituximab and lintuzumab using 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid (DOTA) as a metal ion chelator while the fluorescent probe was fluorescein. CNT-([111In] DOTA) (rituximab) explicitly targeted a disseminated human lymphoma in vivo trials compared to the controls CNT-([111In] DOTA) (lintuzumab) and [111In]rituximab [108].
Tsuchida and coworkers evaluated the drug delivery efficiency of water-dispersed carbon nanohorns in a non-small cell lung cancer model. Polyethylene glycol (PEG)–doxorubicin conjugate bound oxidised single-wall carbon nanohorns (oxSWNHs) injected intratumourally into mice bearing human non-small cell lung cancer (NCI-H460) caused a significant retardation of tumour growth. Histological analyses showed (probably by means of interstitial lymphatic fluid transport), migration of oxSWNHs to the axillary lymph node occurred which is a major site of breast cancer metastasis near the tumour [109]. Shimada et al. described a silica particle-based lymphatic drug delivery system of bleomycin and compared its therapeutic efficacy to that of free bleomycin solution in a transplanted tumour model in animals. Silica particle-adsorbed bleomycin showed considerable inhibitory effect on tumour growth and lymph node metastasis compared to free bleomycin solution [110]. Activated carbon particles of aclarubicin are used for adsorption and sustained release into lymph nodes. Upon subcutaneous administration into the fore foot-pads of rats these particles showed significantly elevated distribution of aclarubicin to the auxiliary lymph nodes compared to aqueous solution of the drug [111]. Activated carbon particles of aclacinomycin A, adriamycin, mitomycin C and pepleomycin have also been used by another group for adsorption. Higher level of drug concentration was maintained in the new dosage form than in the solution form [112].
4.3.3 Antibody–Drug Conjugates
Antibody–drug conjugates enhance the cytotoxic activity of anticancer drugs by conjugating them with antibodies. Antibodies conjugated with cytostatic drugs such as calicheamicin have been used for the treatment of various lymphomas, including non-Hodgkin B-cell lymphoma (NHL), follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL) [113–116].
CD20 B-cell marker is expressed on the surface membrane of pre-B-lymphocytes and mature B-lymphocytes. The anti-CD20 mAb rituximab (Rituxan) is now the most potential antibody for the treatment of non-Hodgkin B-cell lymphomas (B-NHL) [117]. Rituximab-conjugated calicheamicin elevated the antitumour activity of rituximab against human B-cell lymphoma (BCL) xenografts in preclinical models [118].
CD22 is a B-lymphoid lineage-specific differentiation antigen expressed on the surface of both normal and malignant B-cells. Hence, the CD22-specific antibody could be effective in delivering chemotherapeutic drugs to malignant B-cells. Also, CD22 (Siglec-2) antibodies targeting to CD22 are suited for a Trojan horse strategy. Thus, antibody-conjugated therapeutic agents bind to the Siglec and are carried efficiently into the cell [119]. A lot of interest has been seen in clinical progress of the conjugated anti-CD22 antibodies, especially inotuzumab ozogamicin (CMC-544) [120].
CD30 is expressed in the malignant Hodgkin and Reed–Sternberg cells of classical Hodgkin lymphoma (HL) and anaplastic large-cell lymphoma. Younes and Bartlett reported an ongoing phase I dose-escalation trial in relapsed and refractory HL patients with Seattle Genetics (SGN-35), a novel anti-CD30-antibody–monomethylauristatin E conjugate. SGN-35 was stable in the blood and released the conjugate only upon internalisation into CD30-expressing tumour cells [121]. Huang et al. constructed (anti-HER2/neu–IgG3–IFNα), another antibody–drug conjugate, and examined its effect on a murine B-cell lymphoma, 38C13, expressing human HER2/neu, and this significantly inhibited 38C13/HER2 tumour growth in vivo [122].
4.3.4 Hybrid Nanosystems
Hybrid systems use combination of two or more delivery forms for effective targeting. Khatri et al. prepared and investigated the in vivo efficacy of plasmid DNA-loaded chitosan nanoparticles for nasal mucosal immunisation against hepatitis B. Chitosan–DNA nanoparticles prepared by the coacervation process adhered to the nasal or gastrointestinal epithelia and are easily transported to the nasal-associated lymphoid tissue (NALT) and Peyer’s patches of the gut-associated lymphoid tissue (GALT) both as IgA inductive site [123], in which chitosan–DNA might be taken in by M cell, and transported across the mucosal boundary and thereby transfect immune cells within NALT or GALT [124].
A work demonstrates targeting of three peptides containing sequences that bind to cell markers expressed in the tumour vasculature (p24-NRP-1 and p39-Flt-1) [125, 126] and tumour lymphatics (p47-LyP-1) [127] and were tested for their ability to target 3(nitrilotriacetic acid)-ditetradecylamine (NTA3-DTDA) containing liposomes to subcutaneous B16-F1 tumours. Significantly, a potential antitumour effect was seen after administration of doxorubicin-loaded PEG750 liposomes engrafted with p24-NRP-1.
Hybrid liposomes composed of l-α-dimyristoylphosphatidylcholine and polyoxyethylene (25) dodecyl ether prepared by sonication showed remarkable reduction of tumour volume in model mice of acute lymphatic leukaemia (ALL) treated intravenously with HL-25 without drugs after the subcutaneous inoculation of human ALL (MOLT-4) cells was verified in vivo. Prolonged survival (>400 %) was noted in model mice of ALL after the treatment with HL-25 without drugs [128].
In a report, LyP-1 peptide-conjugated PEGylated liposomes loaded with fluorescein or doxorubicin were prepared for targeting and treating lymphatic metastatic tumours. The in vitro cellular uptake and in vivo near-infrared fluorescence imaging results confirmed that LyP-1-modified liposome increased uptake by tumour cells and metastatic lymph nodes.
In another study, in vitro cellular uptake of PEG–PLGA nanoparticle (LyP-1-NPs) was about four times that of PEG–PLGA nanoparticles without LyP-1 (NPs). In vivo study, about eight times lymph node uptake of LyP-1-NPs was seen in metastasis than that of NPs, indicated LyP-1-NP as a promising carrier for target-specific drug delivery to lymphatic metastatic tumours [129].
4.3.5 Biotherapeutics
Currently, surgery, radiation therapy and chemotherapy are the principal methods for cancer treatment. Gene therapies may act synergistically or additively with them. For example, another case demonstrated that replacement of the p53 (protein 53) gene in p53-deficient cancer cell lines enhanced the sensitivity of these cells to Ad-p53 (adenovirus-expressed protein 53) and cisplatin (CDDP) and resulted into greater tumour cell death [130]. Later, Son and Huang [131] stated that treatment of CDDP-resistant tumour cells with CDDP increased the sensitivity of these cells to transduction by DNA-carrying liposomes. Also, Chen et al. [132] described that to improve tumour killing, herpes simplex virus thymidine kinase (HSV-TK) and interleukin (IL) expression can be combined. On the whole, greater therapeutic effect can be achieved by effectively combining conventional cancer treatments and gene therapy together.
5 Physicochemical Aspects of Lymphatic Targeting
Mainly colloidal carriers have emerged as potential targeting agents to lymphatic system. Physicochemical properties affect the efficiency of colloid uptake into the lymphatic system [28]. These properties include size, number of particles, surface charge, molecular weight and colloid lipophilicity. Physicochemical properties are altered by adsorption of group of hydrophilic polymers like poloxamers and poloxamines to the particle surface. These properties modified the biodistribution of particles in vivo, particularly the avoidance of the reticuloendothelial system (RES) upon intravenous administration [133, 134]. In one study, it was opined that opsonisation may cause alteration of the particle surface in vivo [135].
5.1 Size of the Carrier
Size could be important factor in defining the behaviour of particulates after subcutaneous injection. Small particles with diameter less than a few nanometres generally exchanged through the blood capillaries, whereas larger particles of diameters up to a few tens of nanometres absorbed into the lymph capillaries. But particles over a size of few hundred nanometres remain trapped in the interstitial space for a long time [136]. Christy et al. have shown a relationship between colloid size and ease of injection site drainage using model polystyrene nanospheres after subcutaneous administration to the rat [137]. Results showed distribution of polystyrene nanospheres in the size range 30–260 nm 24 h after administration and 74–99 % of the recovered dose retained at the administration site, and as particle diameter increased, drainage became slower. It has been proposed earlier that the optimum colloid size range for lymphoscintigraphic agents is l0–50 nm [138].
Size has less importance when colloids are administered intraperitoneally (i.p.) within the nanometre size range, as drainage is only from a cavity into the initial lymphatics; hence, no diffusion is required through the interstitial space [28]. The size limit of the open junctions of the initial lymphatic wall is the only barrier to uptake from the peritoneal cavity into the lymphatics [139].
5.2 Concentration and Volume
More number of particles at the injection site decreases their rate of drainage, owing to increased obstruction of their diffusion through the interstitial space [139, 140]. Scientists at Nottingham University investigated this effect using polystyrene nanospheres of 60 nm. Following administration to the rat, the concentration range of nanospheres was approximately 0.05–3.0 mg/ml. Lower lymphatic uptake was seen on increasing the concentration of nanospheres in the injection volume due to slower drainage from the injection site. Injecting oily vehicles intramuscularly to the rat, the effect of injection volume has been studied. Increasing volume of sesame oil accelerated oil transport into the lymphatic system. Upon s.c. administration, volumes of aqueous polystyrene particle suspensions have been investigated in the range 50–150 μl [39].
5.3 Surface Charge
Surface charge studies have been done utilising liposome as colloidal carrier. The surface charge of liposomes affected their lymphatic uptake from s.c. and i.p. injection sites. Negatively charged liposomes showed faster drainage than that for positive liposomes after i.p. administration [141]. Patel et al. also indicated that liposome localisation in the lymph nodes followed a particular order negative > positive > neutral [142].
5.4 Molecular Weight
Macromolecule having high molecular weight has a decreased ability for exchange across blood capillaries and lymphatic drainage becomes the route of drainage from the injection site which shows a linear relationship between the molecular weight of macromolecules and the proportion of the dose absorbed by the lymphatics. For a compound to be absorbed by the lymphatics, the molecular weight should range between 1,000 and 16,000 [141, 143]. The effect of molecular weight becomes negligible when targeting carriers to the lymphatic system as the molecular weight of a colloidal carrier is generally less than 1,000 Da.
5.5 Lipophilicity
The most important determinant of the phagocytic response and so lymphatic uptake is the lipophilicity of a colloid [144]. Opsonins generally unite with lipophilic rather than hydrophilic surfaces; hence, the hydrophilic particles show reduced phagocytosis [145]. Hydrophobic polystyrene nanospheres adsorbed with hydrophilic block copolymers showed drastic reduction in phagocytosis prior to i.v. administration [146].
In the case of polystyrene nanospheres of 60-nm diameter, PEO chains of the poloxamers and poloxamines adsorbed onto the surface of the particle described the relationship between interstitial injection site drainage and lymph node uptake in rat [144]. Uncoated nanospheres of this diameter showed reduced drainage from the injection site with 70 % of the administered dose remaining after 24 h. The adsorption of block copolymers can enhance the drainage from the injection site such that levels remaining at the injection site may be as little as 16 % after 24 h, with very hydrophilic polymers such as poloxamine 908. Uptake of nanospheres into the regional lymph nodes may also be improved by the adsorption of block copolymers with intermediate lengths of polyoxyethylene, such as poloxamine 904. This polymer may sequester up to 40 % of the given dose by the lymph nodes after 24 h [147].
6 Effect of Surface Modification on Carriers
Surface modification could prove as an effective strategy for potential targeting to lymphatic system. The influence can be quoted in following ways.
6.1 Surface Modification with Polyethylene Glycols
Coating of a carrier with hydrophilic and sterically stabilised PEG layer can successfully enhance lymphatic absorption, reducing specific interaction of particle with the interstitial surrounding, and inhibit the formation of too large particle structure [49]. Surface modification of liposomes with PEG also does not have a significant effect on lymph node uptake. Small liposomes coated with PEG showed greatest clearance from the s.c. injection site with small 86-nm PEG-coated liposomes having <40 % remaining at the injection site at 24 h. Larger neutral and negatively charged liposomes had a clearance >60 % remaining at the initial s.c. injection site. However, this smaller amount of large liposomes that were cleared from the injection site was compensated by better retention in the lymph node [148]. Oussoren et al. reported that the amount of liposomes cleared from the injection site was somewhat greater with the PEG-coated liposomes [149]. This improved clearance did not result in improved lymph node retention because the fraction of PEG liposomes retained by the lymph node is decreased. Phillips et al. also studied the slightly improved clearance of PEG-coated liposomes from the s.c. injection site [148].
Porter and coworkers demonstrated that PEGylation of poly-l-lysine dendrimers resulted into better absorption from s.c. injection sites and stated that the extent of lymphatic transport may be improved by increasing the size of the PEGylated dendrimer complex. They estimated the lymphatic uptake and lymph node retention properties of several generation four dendrimers coated with PEG or 4-benzene sulphonate after subcutaneous administration in rats. For this surface modification study, three types of PEGs with molecular weights of 200, 570 or 2,000 Da were taken. PEG200-derived dendrimers showed rapid and complete absorption into the blood when injected subcutaneously, and only 3 % of the total given dose was found in the pooled thoracic lymph over 30 h, whereas PEG570- and PEG2000-derived dendrimers showed lesser absorption, and a higher amount was recovered in lymphatics (29 %) over 30 h. However, the benzene sulphonate-capped dendrimer was not well absorbed either in the blood or in lymph following subcutaneous injection [150].
6.2 Surface Modification with Ligands
Carriers capped with nonspecific human antibodies as ligands showed greater lymphatic uptake and lymph node retention compared to uncoated one at the s.c. site. Liposomes coated with the antibody, IgG, have been shown to increase lymph node localisation of liposomes to 4.5 % of the injected dose at 1 h, but this level decreased to 3 % by 24 h [151]. In a study, the liposomes containing positively charged lipids had approximately 2–3 times the lymph node localisation (up to 3.6 % of the injected dose) than liposomes containing neutral or negatively charged lipids (1.2 % of the injected dose) [149]. Attachment of mannose to the surface of a liposome increased lymph node uptake by threefold compared to control liposomes [152].
Another study demonstrated HBsAg entrapped dried liposomes with their surfaces modified with galactose. Pharmacokinetic study in rats showed that galactosylated liposomes delivered higher amounts of HBsAg to the regional lymph nodes than other ungalactosylated formulations [153].
Lectin is another ligand that can be attached to the carriers for improved targeting to intestinal lymphatics. Bovine serum albumin containing acid phosphatase model protein and polystyrene microspheres conjugated with mouse M-cell-specific Ulex europaeus lectin. Ex vivo results showed that there was favoured binding of the lectin-conjugated microspheres to the follicle-associated epithelium. Final results indicated that coupling of ligands such as lectin specific to cells of the follicle-associated epithelium can improve the targeting of encapsulated candidate antigens for delivery to the Peyer’s patches of the intestine for better oral delivery [154].
6.3 Surface Modification with Biotin
To improve carrier retention in lymph nodes, a new method of increasing lymphatic uptake of subcutaneously injected liposome utilises the high-affinity ligands biotin and avidin. Biotin is a naturally occurring cofactor and avidin is a protein derived from eggs. Avidin and biotin are having extremely high affinity for each other. For instance, upon injection, the avidin and the biotin liposomes move into the lymphatic vessels. Biotin liposomes that migrate through the lymphatic vessels meet the avidin resulting in an aggregate that becomes trapped in the lymph nodes [155, 156]. The biotin liposome/avidin system has promising potential as therapeutic agent for delivery to lymph nodes. It can be applied not only to s.c. targeting of lymph nodes but also to intracavitary lymph node targeting [50].
Different ligands with their application in lymphatic targeting are represented in Table 20.1.
7 Future Trends and Conclusion
The lymphatics have the potential to play a major role in anticancer treatment as lymphatic spread is recognised to precede haematological spread in many cancers including melanoma, breast, colon, lung and prostate cancers. Currently, the focus is on the development of drug carriers that can localise chemotherapy to the lymphatic system, thus improving the treatment of localised disease while minimising the exposure of healthy organs to cytotoxic drugs. The delivery of novel carriers to lymph nodes for therapeutic purposes has much promise. Giving importance to the lymphatic route in metastasis, this delivery system may have great potential for targeted delivery of various therapeutic agents to tumours and their metastatic lymph nodes. Various delivery systems have been discussed here but colloidal carriers, especially, liposomes have been the carrier of choice to date. The purpose of this review is to provide an improved and effective lymphotropic system with a satisfactory quality for clinical use and to establish a preparation method applicable for industrial production. Surface-engineered lymphotropic systems may prove as an effective carrier for anti-HIV, anticancer and oral vaccine delivery in near future.
Abbreviations
- AIDS:
-
Acquired immunodeficiency syndrome
- CNT:
-
Carbon nanotube
- DAB:
-
Diaminobutyl
- EPR:
-
Enhanced permeation and retention
- GALT:
-
Gut-associated lymphoid tissue
- HA:
-
Hyaluronic acid
- HAART:
-
Highly active antiretroviral therapy
- HER:
-
Human epidermal growth factor receptor
- HIV:
-
Human immunodeficiency virus
- i.m.:
-
Intramuscular
- i.p.:
-
Intraperitoneal
- IFN:
-
Interferon
- IgG:
-
Immunoglobulin G
- ipl:
-
Intrapleural
- LECs:
-
Lymphatic endothelial cells
- mAbs:
-
Monoclonal antibodies
- MN-MWNTs:
-
Magnetic multiwalled nanotubes
- MWNTs:
-
Multiwalled nanotubes
- NALT:
-
Nasal-associated lymphoid tissue
- PAMAM:
-
Polyamidoamine
- PEG:
-
Polyethylene glycol
- PLA:
-
Polylactic acid
- PLGA:
-
Poly(lactic-co-glycolic acid)
- PMMA:
-
Poly(methyl methacrylate)
- RES:
-
Reticuloendothelial system
- s.c.:
-
Subcutaneous
- SARS:
-
Severe acute respiratory syndrome
- SEDDS:
-
Self-emulsifying drug delivery system
- SLN:
-
Solid lipid nanoparticles
- TB:
-
Tuberculosis
- TUNEL assay:
-
Terminal deoxynucleotidyl transferase dUTP nick end labelling assay
References
Swartz MA (2001) The physiology of the lymphatic system. Adv Drug Deliv Rev 50:3–20
Huntington GS, McClure CFW (2005) The anatomy and development of the jugular lymph sacs in the domestic cat (Felis domestica). Am J Anat 10:177–312
Fr S (1902) On the origin of the lymphatic system from the veins and the development of the lymph hearts and thoracic duct in the pig. Am J Anat 1:367–389
Wilting J, Aref Y, Huang R, Tomarev SI, Schweigerer L, Christ B et al (2006) Dual origin of avian lymphatics. Dev Biol 292:165–173
Srinivasan RS, Dillard ME, Lagutin OV, Lin FJ, Tsai S, Tsai MJ et al (2007) Lineage tracing demonstrates the venous origin of the mammalian lymphatic vasculature. Genes Dev 21:2422–2432
Wigle JT, Harvey N, Detmar M, Lagutina I, Grosveld G, Gunn MD et al (2002) An essential role for Prox1 in the induction of the lymphatic endothelial cell phenotype. EMBO J 21:1505–1513
Wigle JT, Oliver G (1999) Prox1 function is required for the development of the murine lymphatic system. Cell 98:769–778
Yaniv K, Isogai S, Castranova D, Dye L, Hitomi J, Weinstein BM (2006) Live imaging of lymphatic development in the zebrafish. Nat Med 12:711–716
Maby-El Hajjami H, Petrova TV (2008) Developmental and pathological lymphangiogenesis: from models to human disease. Histochem Cell Biol 130:1063–1078
Rinderknecht M, Detmar M (2008) Tumor lymphangiogenesis and melanoma metastasis. J Cell Physiol 216:347–354
Heller LJ, Mohrman DE (1981) Cardiovascular physiology. McGraw-Hill
Cueni LN, Detmar M (2006) New insights into the molecular control of the lymphatic vascular system and its role in disease. J Invest Dermatol 126:2167–2177
Givoli D, Doukhovni I, Moghimi S, Rajabi-Siahboomi A (1996) Advanced colloid-based systems for efficient delivery of drugs and diagnostic agents to the lymphatic tissues. Prog Biophys Mol Biol 65:221–249
Leak L (1976) The structure of lymphatic capillaries in lymph formation. In: Federation Proceedings. p 1863
Gerli R, Solito R, Weber E, Agliano M (2000) Specific adhesion molecules bind anchoring filaments and endothelial cells in human skin initial lymphatics. Lymphology 33:148
Weber E, Rossi A, Solito R, Sacchi G, Agliano M, Gerli R (2002) Focal adhesion molecules expression and fibrillin deposition by lymphatic and blood vessel endothelial cells in culture. Microvasc Res 64:47–55
Schmid-Schönbein GW (2003) The second valve system in lymphatics. Lymphat Res Biol 1:25–31
Trzewik J, Mallipattu S, Artmann GM, Delano F, Schmid-Schönbein GW (2001) Evidence for a second valve system in lymphatics: endothelial microvalves. FASEB J 15:1711–1717
Leak L, Burke J (1968) Ultrastructural studies on the lymphatic anchoring filaments. J Cell Biol 36:129–149
Sharma R, Wendt JA, Rasmussen JC, Adams KE, Marshall MV, Sevick‐Muraca EM (2008) New horizons for imaging lymphatic function. Ann NY Acad Sci 1131:13–36
von der Weid PY, Zawieja DC (2004) Lymphatic smooth muscle: the motor unit of lymph drainage. Int J Biochem Cell Biol 36:1147–1153
Casley-Smith J (1980) The fine structure and functioning of tissue channels and lymphatics. Lymphology 13:177
Moore KL, Dalley AF (1999) Clinically oriented anatomy. Lippincott Williams & Wilkins, Baltimore
Alitalo K, Tammela T, Petrova TV (2005) Lymphangiogenesis in development and human disease. Nature 438:946–953
Oliver G, Detmar M (2002) The rediscovery of the lymphatic system: old and new insights into the development and biological function of the lymphatic vasculature. Genes Dev 16:773–783
Mohrman ED, Heller LJ (2002) Cardiovascular Physiology. McGraw-Hill Companies Inc, USA
Morton DL, Eilber FR, Joseph WL, Wood WC, Trahan E, Ketcham AS (1970) Immunological factors in human sarcomas and melanomas: a rational basis for immunotherapy. Ann Surg 172:740
O’Hagan DT, Christy NM, Davis SS (1992) Particulates and lymphatic drug delivery. In: Charman WN, Stella VJ (eds) Lymphatic transport of drugs. CRC, Boca Raton, FL, pp 279–315
Charman WN, Stella VJ (1992) Lymphatic transport of drugs. CRC, Boca Raton, FL
Charman WN, Porter CJH (1996) Lipophilic prodrugs designed for intestinal lymphatic transport. Adv Drug Deliv Rev 19:149–169
Porter CJH, Charman WN (2001) Intestinal lymphatic drug transport: an update. Adv Drug Deliv Rev 50:61–80
Wasan KM (2002) The role of lymphatic transport in enhancing oral protein and peptide drug delivery. Drug Dev Indus Pharm 28:1047–1058
Humberstone AJ, Porter CJH, Edwards GA, Charman WN (1998) Association of halofantrine with postprandially derived plasma lipoproteins decreases its clearance relative to administration in the fasted state. J Pharm Sci 87:936–942
Shah AK, Sawchuk RJ (2006) Effect of co-administration of intralipidTM on the pharmacokinetics of cyclosporine in the rabbit. Biopharm Drug Dispos 12:457–466
Wasan KM, Cassidy SM (1998) Role of plasma lipoproteins in modifying the biological activity of hydrophobic drugs. J Pharm Sci 87:411–424
Arya M, Bott SR, Shergill IS, Ahmed HU, Williamson M, Patel HR (2006) The metastatic cascade in prostate cancer. Surg Oncol 15:117–128
Cense H, Van Eijck C, Tilanus H (2006) New insights in the lymphatic spread of oesophageal cancer and its implications for the extent of surgical resection. Best Pract Res Clin Gastroenterol 20:893
Garzon-Aburbeh A, Poupaert JH, Claesen M, Dumont P, Atassi G (1983) 1, 3-dipalmitoylglycerol ester of chlorambucil as a lymphotropic, orally administrable antineoplastic agent. J Med Chem 26:1200–1203
Muranishi S (1980) Lymphatic delivery of drugs and its application to cancer chemotherapy (author’s transl). Yakugaku zasshi: J Pharm Soc Jpn 100:687
Pantaleo G, Graziosi C, Demarest JF, Cohen OJ, Vaccarezza M, Gantt K et al (1994) Role of lymphoid organs in the pathogenesis of human immunodeficiency virus (HIV) infection. Immunol Rev 140:105–130
Pantaleo G, Graziosi C, Fauci AS (1993) The role of lymphoid organs in the immunopathogenesis of HIV infection. AIDS 7:S19
Umeda M, Marusawa H, Seno H, Katsurada A, Nabeshima M, Egawa H et al (2005) Hepatitis B virus infection in lymphatic tissues in inactive hepatitis B carriers. J Hepatol 42:806–812
Von Messling V, Svitek N, Cattaneo R (2006) Receptor (SLAM [CD150]) recognition and the V protein sustain swift lymphocyte-based invasion of mucosal tissue and lymphatic organs by a morbillivirus. J Virol 80:6084–6092
Lan N, Yamaguchi R, Inomata A, Furuya Y, Uchida K, Sugano S et al (2006) Comparative analyses of canine distemper viral isolates from clinical cases of canine distemper in vaccinated dogs. Vet Microbiol 115:32–42
Spiegel M, Schneider K, Weber F, Weidmann M, Hufert FT (2006) Interaction of severe acute respiratory syndrome-associated coronavirus with dendritic cells. J Gen Virol 87:1953–1960
Kessel A, Toubi E (2007) Chronic HCV-related autoimmunity: a consequence of viral persistence and lymphotropism. Curr Med Chem 14:547–554
Düzgünes N, Simoes S, Slepushkin V, Pretzer E, Rossi J, De Clercq E et al (2001) Enhanced inhibition of HIV-1 replication in macrophages by antisense oligonucleotides, ribozymes and acyclic nucleoside phosphonate analogs delivered in pH-sensitive liposomes. Nucleosides Nucleotides Nucleic Acids 20:515–523
Hirnle P (1997) Liposomes for drug targeting in the lymphatic system. Hybridoma 16:127–132
Oussoren C, Storm G (2001) Liposomes to target the lymphatics by subcutaneous administration. Adv Drug Deliv Rev 50:143–156
Phillips WT, Klipper R, Goins B (2000) Novel method of greatly enhanced delivery of liposomes to lymph nodes. J Pharmacol Exp Ther 295:309–313
Hanahan D, Weinberg RA (2000) The hallmarks of cancer. Cell 100:57–70
Torabi M, Aquino SL, Harisinghani MG (2004) Current concepts in lymph node imaging. J Nucl Med 45:1509–1518
Busby JE, Evans CP (2004) Old friends, new ways: revisiting extended lymphadenectomy and neoadjuvant chemotherapy to improve outcomes. Curr Opin Urol 14:251–257
Gagné JF, Désormeaux A, Perron S, Tremblay MJ, Bergeron MG (2002) Targeted delivery of indinavir to HIV-1 primary reservoirs with immunoliposomes. Biochim Biophys Acta (BBA)-Biomembranes 1558:198–210
Cohen OJ, Pantaleo G, Lam GK, Fauci AS (1997) Studies on lymphoid tissue from HIV-infected individuals: implications for the design of therapeutic strategies. In: Springer seminars in immunopathology. Springer, pp 305–322
Désormeaux A, Bergeron MG (2005) Lymphoid tissue targeting of anti-HIV drugs using liposomes. Methods Enzymol 391:330–351
El Setouhy M, Ramzy RMR, Ahmed ES, Kandil AM, Hussain O, Farid HA et al (2004) A randomized clinical trial comparing single-and multi-dose combination therapy with diethylcarbamazine and albendazole for treatment of bancroftian filariasis. Am J Trop Med Hyg 70:191–196
Dixon D, Terry C, Meselson M, Guillemin J, Hanna PC, Clínicas M (1999) Infección bacteriana por ántrax. N Engl J Med 341:815–826
Jernigan JA, Stephens DS, Ashford DA, Omenaca C, Topiel MS, Galbraith M et al (2001) Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Emerg Infect Dis 7:933
Barakat LA, Quentzel HL, Jernigan JA, Kirschke DL, Griffith K, Spear SM et al (2002) Fatal inhalational anthrax in a 94-year-old Connecticut woman. JAMA 287:863–868
Ilgazli A, Boyaci H, Basyigit İ, Yildiz F (2004) Extrapulmonary tuberculosis: clinical and epidemiologic spectrum of 636 cases. Arch Med Res 35:435–441
Haley B, Frenkel E (2008) Nanoparticles for drug delivery in cancer treatment. In: Urologic oncology: seminars and original investigations. Elsevier, pp 57–64
Maeda H, Bharate G, Daruwalla J (2009) Polymeric drugs for efficient tumor-targeted drug delivery based on EPR-effect. Eur J Pharm Biopharm 71:409
Iyer AK, Khaled G, Fang J, Maeda H (2006) Exploiting the enhanced permeability and retention effect for tumor targeting. Drug Discov Today 11:812–818
Bae YH (2009) Drug targeting and tumor heterogeneity. J Control Release 133:2
Pirollo KF, Chang EH (2008) Does a targeting ligand influence nanoparticle tumor localization or uptake? Trends Biotechnol 26:552–558
Adams GP, Schier R, McCall AM, Simmons HH, Horak EM, Alpaugh RK et al (2001) High affinity restricts the localization and tumor penetration of single-chain fv antibody molecules. Cancer Res 61:4750–4755
Gosk S, Moos T, Gottstein C, Bendas G (2008) VCAM-1 directed immunoliposomes selectively target tumor vasculature in vivo. Biochim Biophys Acta (BBA)-Biomembranes 1778:854–863
Nishioka Y, Yoshino H (2001) Lymphatic targeting with nanoparticulate system. Adv Drug Deliv Rev 47:55–64
Karajgi J, Vyas S (1994) A lymphotropic colloidal carrier system for diethylcarbamazine: preparation and performance evaluation. J Microencapsul 11:539–545
Yoshimura K, Nunomura M, Takiguchi N, Oda K, Suzuki H, Furukawa R et al (1996) Evaluation of endoscopic pirarubicin-Lipiodol emulsion injection therapy for gastric cancer. Jpn J Canc Chemother 23:1519–1522
Hauss DJ, Mehta SC, Radebaugh GW (1994) Targeted lymphatic transport and modified systemic distribution of CI-976, a lipophilic lipid-regulator drug, via a formulation approach. Int J Pharm 108:85–93
Kommuru T, Gurley B, Khan M, Reddy I (2001) Self-emulsifying drug delivery systems (SEDDS) of coenzyme Q 10: formulation development and bioavailability assessment. Int J Pharm 212:233–246
Segal A, Gregoriadis G, Black C (1975) Liposomes as vehicles for the local release of drugs. Clin Sci Mol Med 49:99
Sheue Nee Ling S, Magosso E, Abdul Karim Khan N, Hay Yuen K, Anne Barker S (2006) Enhanced oral bioavailability and intestinal lymphatic transport of a hydrophilic drug using liposomes. Drug Dev Ind Pharm 32:335–345
Frenkel V, Etherington A, Greene M, Quijano J, Xie J, Hunter F et al (2006) Delivery of liposomal doxorubicin (Doxil) in a breast cancer tumor model: investigation of potential enhancement by pulsed-high intensity focused ultrasound exposure. Acad Radiol 13:469–479
O’brien M, Wigler N, Inbar M, Rosso R, Grischke E, Santoro A et al (2004) Reduced cardiotoxicity and comparable efficacy in a phase III trial of pegylated liposomal doxorubicin HCl (CAELYX™/Doxil®) versus conventional doxorubicin for first-line treatment of metastatic breast cancer. Ann Oncol 15:440–449
Prescott L (1995) Doxil offers hope to KS sufferers. J Int Assoc Physicians AIDS Care 1:43
Soundararajan A, Bao A, Phillips WT, Perez R, Goins BA (2009) Liposomal doxorubicin (Doxil): in vitro stability, pharmacokinetics, imaging and biodistribution in a head and neck squamous cell carcinoma xenograft model. Nucl Med Biol 36:515–524
Tejada-Berges T, Granai C, Gordinier M, Gajewski W (2002) Caelyx/Doxil for the treatment of metastatic ovarian and breast cancer. Expert Rev Anticancer Ther 2:143–150
Hirnle P, Harzmann R, Wright J (1988) Patent blue V encapsulation in liposomes: potential applicability to endolympatic therapy and preoperative chromolymphography. Lymphology 21:187
Latimer P, Menchaca M, Snyder RM, Yu W, Gilbert BE, Sanders BG et al (2009) Aerosol delivery of liposomal formulated paclitaxel and vitamin E analog reduces murine mammary tumor burden and metastases. Exp Biol Med 234:1244–1252
Lawson KA, Anderson K, Snyder RM, Simmons-Menchaca M, Atkinson J, Sun LZ et al (2004) Novel vitamin E analogue and 9-nitro-camptothecin administered as liposome aerosols decrease syngeneic mouse mammary tumor burden and inhibit metastasis. Cancer Chemother Pharmacol 54:421–431
Bermudez LE (1994) Use of liposome preparation to treat mycobacterial infections. Immunobiology 191:578–583
Rabaça Roque Botelho MF, Marques T, Gomes F, Andrade Figueiredo Bairos VA, de Matos Santos Rosa M, Pedroso de Lima J (2009) Nanoradioliposomes molecularly modulated to study the lung deep lymphatic drainage. Rev Port Pneumol 15:261–293
Bargoni A, Cavalli R, Caputo O, Fundarò A, Gasco MR, Zara GP (1998) Solid lipid nanoparticles in lymph and plasma after duodenal administration to rats. Pharm Res 15:745–750
Cavalli R, Bargoni A, Podio V, Muntoni E, Zara GP, Gasco MR (2003) Duodenal administration of solid lipid nanoparticles loaded with different percentages of tobramycin. J Pharm Sci 92:1085–1094
Cavalli R, Zara GP, Caputo O, Bargoni A, Fundarò A, Gasco MR (2000) Transmucosal transport of tobramycin incorporated in SLN after duodenal administration to rats. Part I—a pharmacokinetic study. Pharmacol Res 42:541–545
Zara GP, Bargoni A, Cavalli R, Fundarò A, Vighetto D, Gasco MR (2002) Pharmacokinetics and tissue distribution of idarubicin‐loaded solid lipid nanoparticles after duodenal administration to rats. J Pharm Sci 91:1324–1333
Harivardhan Reddy L, Sharma R, Chuttani K, Mishra A, Murthy R (2005) Influence of administration route on tumor uptake and biodistribution of etoposide loaded solid lipid nanoparticles in Dalton’s lymphoma tumor bearing mice. J Control Release 105:185–198
Elliott JA, Osterlind K, Hirsch FR, Hansen HH (1987) Metastatic patterns in small-cell lung cancer: correlation of autopsy findings with clinical parameters in 537 patients. J Clin Oncol 5:246–254
Stenbygaard LE, Sørensen JB, Larsen H, Dombernowsky P (1999) Metastatic pattern in non-resectable non-small cell lung cancer. Acta Oncol 38:993–998
Müller RH, Mäder K, Gohla S (2000) Solid lipid nanoparticles (SLN) for controlled drug delivery–a review of the state of the art. Eur J Pharm Biopharm 50:161–177
Videira MA, Botelho M, Santos AC, Gouveia LF, Pedroso de Lima J, Almeida AJ (2002) Lymphatic uptake of pulmonary delivered radiolabelled solid lipid nanoparticles. J Drug Target 10:607–613
Bhatnagar A, Singh AK, Singh T, Sethi RS, Soni NL (1998) Inflammation imaging using Tc-99m dextran. Clin Nucl Med 23:123–124
Cai S, Xie Y, Bagby TR, Cohen MS, Forrest ML (2008) Intralymphatic chemotherapy using a hyaluronan–cisplatin conjugate. J Surg Res 147:247–252
Hawley AE, Illum L, Davis SS (1997) Lymph node localisation of biodegradable nanospheres surface modified with poloxamer and poloxamine block co-polymers. FEBS Lett 400:319–323
Dünne AA, Boerner HG, Kukula H, Schlaad H, Wiegand S, Werner JA et al (2007) Block copolymer carrier systems for translymphatic chemotherapy of lymph node metastases. Anticancer Res 27:3935–3940
Liu J, Meisner D, Kwong E, Wu XY, Johnston MR (2009) Translymphatic chemotherapy by intrapleural placement of gelatin sponge containing biodegradable Paclitaxel colloids controls lymphatic metastasis in lung cancer. Cancer Res 69:1174–1181
Kumanohoso T, Natsugoe S, Shimada M, Aikou T (1997) Enhancement of therapeutic efficacy of bleomycin by incorporation into biodegradable poly-d, l-lactic acid. Cancer Chemother Pharmacol 40:112–116
Liu J, Wong HL, Moselhy J, Bowen B, Wu XY, Johnston MR (2006) Targeting colloidal particulates to thoracic lymph nodes. Lung Cancer 51:377–386
Kobayashi H, Kawamoto S, Choyke PL, Sato N, Knopp MV, Star RA et al (2003) Comparison of dendrimer‐based macromolecular contrast agents for dynamic micro‐magnetic resonance lymphangiography. Magn Reson Med 50:758–766
Kobayashi H, Kawamoto S, Bernardo M, Brechbiel MW, Knopp MV, Choyke PL (2006) Delivery of gadolinium-labeled nanoparticles to the sentinel lymph node: comparison of the sentinel node visualization and estimations of intra-nodal gadolinium concentration by the magnetic resonance imaging. J Control Release 111:343–351
Kobayashi H, Koyama Y, Barrett T, Hama Y, Regino CAS, Shin IS et al (2007) Multimodal nanoprobes for radionuclide and five-color near-infrared optical lymphatic imaging. ACS Nano 1:258–264
Koyama Y, Talanov VS, Bernardo M, Hama Y, Regino CAS, Brechbiel MW et al (2007) A dendrimer‐based nanosized contrast agent dual‐labeled for magnetic resonance and optical fluorescence imaging to localize the sentinel lymph node in mice. J Magn Reson Imag 25:866–871
Kobayashi H, Ogawa M, Kosaka N, Choyke PL, Urano Y (2009) Multicolor imaging of lymphatic function with two nanomaterials: quantum dot-labeled cancer cells and dendrimer-based optical agents. Nanomedicine 4:411–419
Yang D, Yang F, Hu J, Long J, Wang C, Fu D et al (2009) Hydrophilic multi-walled carbon nanotubes decorated with magnetite nanoparticles as lymphatic targeted drug delivery vehicles. Chem Commun 29:4447–4449
McDevitt MR, Chattopadhyay D, Kappel BJ, Jaggi JS, Schiffman SR, Antczak C et al (2007) Tumor targeting with antibody-functionalized, radiolabeled carbon nanotubes. J Nucl Med 48:1180–1189
Murakami T, Sawada H, Tamura G, Yudasaka M, Iijima S, Tsuchida K (2008) Water-dispersed single-wall carbon nanohorns as drug carriers for local cancer chemotherapy. Nanomedicine 3:453–463
Shimada M, Natsugoe S, Aikou T (1995) Enhanced efficacy of Bleomycin adsorbed on silica particles against lymph node metastasis derived from a transplanted tumor. Anticancer Res 15:109
Hagiwara A, Takahashi T, Iwamoto A, Yoneyama C, Matsumoto S, Muranishi S (1991) Selective distribution of aclarubicin to regional lymph nodes with a new dosage form: aclarubicin adsorbed on activated carbon particles. Anticancer Drugs 2:261
Lucci A, Turner RR, Morton DL (1999) Carbon dye as an adjunct to isosulfan blue dye for sentinel lymph node dissection. Surgery 126:48–53
Advani A, Coiffier B, Czuczman MS, Dreyling M, Foran J, Gine E et al (2010) Safety, pharmacokinetics, and preliminary clinical activity of inotuzumab ozogamicin, a novel immunoconjugate for the treatment of B-cell non-Hodgkin’s lymphoma: results of a phase I study. J Clin Oncol 28:2085–2093
Dijoseph J, Dougher M, Armellino D, Evans D, Damle N (2007) Therapeutic potential of CD22-specific antibody-targeted chemotherapy using inotuzumab ozogamicin (CMC-544) for the treatment of acute lymphoblastic leukemia. Leukemia 21:2240–2245
DiJoseph JF, Armellino DC, Boghaert ER, Khandke K, Dougher MM, Sridharan L et al (2004) Antibody-targeted chemotherapy with CMC-544: a CD22-targeted immunoconjugate of calicheamicin for the treatment of B-lymphoid malignancies. Blood 103:1807–1814
DiJoseph JF, Dougher MM, Evans DY, Zhou BB, Damle NK (2011) Preclinical anti-tumor activity of antibody-targeted chemotherapy with CMC-544 (inotuzumab ozogamicin), a CD22-specific immunoconjugate of calicheamicin, compared with non-targeted combination chemotherapy with CVP or CHOP. Cancer Chemother Pharmacol 67:741–749
Grillo-López AJ (2003) Rituximab (Rituxan®/MabThera®): the first decade (1993–2003). Expert Rev Anticancer Ther 3:767–779
DiJoseph JF, Dougher MM, Armellino DC, Kalyandrug L, Kunz A, Boghaert ER et al (2007) CD20-specific antibody-targeted chemotherapy of non-Hodgkin’s B-cell lymphoma using calicheamicin-conjugated rituximab. Cancer Immunol Immunother 56:1107–1117
O’Reilly MK, Paulson JC (2009) Siglecs as targets for therapy in immune-cell-mediated disease. Trends Pharmacol Sci 30:240–248
Fayad L, Patel H, Verhoef G, Czuczman M, Foran J, Gine E et al (2006) Clinical activity of the immunoconjugate CMC-544 in B-cell malignancies: preliminary report of the expanded maximum tolerated dose (MTD) cohort of a phase 1 study. Blood 108:766a
Younes A, Forero-Torres A, Bartlett N, Leonard J, Rege B, Kennedy D et al (2008) Objective responses in a phase I dose-escalation study of SGN-35, a novel antibody-drug conjugate (ADC) targeting CD30, in patients with relapsed or refractory Hodgkin lymphoma. J Clin Oncol 26:8526
Xuan C, Steward KK, Timmerman JM, Morrison SL (2010) Targeted delivery of interferon-alpha via fusion to anti-CD20 results in potent antitumor activity against B-cell lymphoma. Blood 115:2864–2871
Van der Lubben I, Verhoef J, Borchard G, Junginger H (2001) Chitosan for mucosal vaccination. Adv Drug Deliv Rev 52:139–144
Janes K, Calvo P, Alonso M (2001) Polysaccharide colloidal particles as delivery systems for macromolecules. Adv Drug Deliv Rev 47:83–97
An P, Lei H, Zhang J, Song S, He L, Jin G et al (2004) Suppression of tumor growth and metastasis by a VEGFR‐1 antagonizing peptide identified from a phage display library. Int J Cancer 111:165–173
Starzec A, Vassy R, Martin A, Lecouvey M, Di Benedetto M, Crépin M et al (2006) Antiangiogenic and antitumor activities of peptide inhibiting the vascular endothelial growth factor binding to neuropilin-1. Life Sci 79:2370
Laakkonen P, Porkka K, Hoffman JA, Ruoslahti E (2002) A tumor-homing peptide with a targeting specificity related to lymphatic vessels. Nat Med 8:751–755
Ichihara H, Ueno J, Umebayashi M, Matsumoto Y, Ueoka R (2011) Chemotherapy with hybrid liposomes for acute lymphatic leukemia leading to apoptosis in vivo. Int J Pharm 406:173–178
Luo G, Yu X, Jin C, Yang F, Fu D, Long J et al (2010) LyP-1-conjugated nanoparticles for targeting drug delivery to lymphatic metastatic tumors. Int J Pharm 385:150–156
Ramesh R, Saeki T, Templeton NS, Ji L, Stephens LC, Ito I et al (2001) Successful treatment of primary and disseminated human lung cancers by systemic delivery of tumor suppressor genes using an improved liposome vector. Mol Ther 3:337–350
Son K, Huang L (1994) Exposure of human ovarian carcinoma to cisplatin transiently sensitizes the tumor cells for liposome-mediated gene transfer. Proc Natl Acad Sci USA 91:12669–12672
Chen SH, Chen X, Wang Y, Kosai K, Finegold MJ, Rich SS et al (1995) Combination gene therapy for liver metastasis of colon carcinoma in vivo. Proc Natl Acad Sci USA 92:2577–2581
Davis SS, Illum L (1988) Polymeric microspheres as drug carriers. Biomaterials 9:111–115
Illum L, Davis S, Müller R, Mak E, West P (1987) The organ distribution and circulation time of intravenously injected colloidal carriers sterically stabilized with a blockcopolymer-poloxamine 908. Life Sci 40:367–374
Papahadjopoulos D (1996) Fate of liposomes in vivo: a brief introductory review. J Liposome Res 6:3–17
Bergqvist L, Strand S, Haftstrom L, Jonsson P (1984) The characterisation of radio colloids used for administration to the lymphatic system. In: Davis SS, Ilium L, McVic JG, Tomlinson E (eds) Microspheres and drug therapy: pharmaceutical immunological and medical aspects. Elsevier, Amsterdam, pp 263–267
Christy N, Moghimi S, Illum L, Davis S (1992) Effect of size on the lymphatic uptake of a model colloid system. In: Proceedings of the international symposium on controlled release of bioactive materials. pp 355–356
Strand S, Bergqvist L (1989) Radiolabeled colloids and macromolecules in the lymphatic system. Crit Rev Ther Drug Carrier Syst 6:211
Bettendorf U (1979) Electron microscopic studies on the peritoneal resorption of intraperitoneally injected latex particles via the diaphragmatic lymphatics. Lymphology 12:66
Winkel Kz (1972) Lymphologie mit Radionukliden. H. Hoffmann
Hirano K, Hunt CA, Strubbe A, MacGregor RD (1985) Lymphatic transport of liposome-encapsulated drugs following intraperitoneal administration–effect of lipid composition. Pharm Res 2:271–278
Patel HM, Katherine MB, Vaughan-Jones R (1984) Assessment of the potential uses of liposomes for lymphoscintigraphy and lymphatic drug delivery failure of 99-technetium marker to represent intact liposomes in lymph nodes. Biochim Biophys Acta (BBA)-General Subjects 801:76–86
Supersaxo A, Hein WR, Steffen H (1990) Effect of molecular weight on the lymphatic absorption of water-soluble compounds following subcutaneous administration. Pharm Res 7:167–169
Moghimi S, Hawley A, Christy N, Gray T, Illum L, Davis S (1994) Surface engineered nanospheres with enhanced drainage into lymphatics and uptake by macrophages of the regional lymph nodes. FEBS Lett 344:25–30
Patel H (1992) Serum opsonins and liposomes: their interaction and opsonophagocytosis. Crit Rev Ther Drug Carrier Syst 9:39–90
Florence AT, Attwood D (2011) Physicochemical principles of pharmacy. Pharmaceutical Press, London
Hawley A, Davis S, Illum L (1995) Targeting of colloids to lymph nodes: influence of lymphatic physiology and colloidal characteristics. Adv Drug Deliv Rev 17:129–148
Phillips WT, Andrews T, Liu H, Klipper R, Landry AJ, Blumhardt R et al (2001) Evaluation of [(99m) Tc] liposomes as lymphoscintigraphic agents: comparison with [(99m) Tc] sulfur colloid and [(99m) Tc] human serum albumin. Nucl Med Biol 28:435
Oussoren C, Storm G (1997) Lymphatic uptake and biodistribution of liposomes after subcutaneous injection: III. Influence of surface modification with poly(ethyleneglycol). Pharm Res 14:1479–1484
Kaminskas LM, Kota J, McLeod VM, Kelly BD, Karellas P, Porter CJH (2009) PEGylation of polylysine dendrimers improves absorption and lymphatic targeting following SC administration in rats. J Control Release 140:108–116
Mangat S, Patel HM (1985) Lymph node localization of non-specific antibody-coated liposomes. Life Sci 36:1917–1925
Wu MS, Robbins JC, Bugianesi RL, Ponpipom MM, Shen T (1981) Modified in vivo behavior of liposomes containing synthetic glycolipids. Biochim Biophys Acta (BBA)-General Subjects 674:19–29
Kim CK, Jeong EJ (1997) Enhanced lymph node delivery and immunogenicity of hepatitis B surface antigen entrapped in galactosylated liposomes. Int J Pharm 147:143–151
Akande J, Yeboah KG, Addo RT, Siddig A, Oettinger CW, D’Souza MJ (2010) Targeted delivery of antigens to the gut-associated lymphoid tissues: 2. Ex vivo evaluation of lectin-labelled albumin microspheres for targeted delivery of antigens to the M-cells of the Peyer’s patches. J Microencapsul 27:325–336
Medina LA, Calixto SM, Klipper R, Phillips WT, Goins B (2004) Avidin/biotin‐liposome system injected in the pleural space for drug delivery to mediastinal lymph nodes. J Pharm Sci 93:2595–2608
Medina LA, Klipper R, Phillips WT, Goins B (2004) Pharmacokinetics and biodistribution of 111In avidin and 99 Tc biotin-liposomes injected in the pleural space for the targeting of mediastinal nodes. Nucl Med Biol 31:41–51
Gu B, Xie C, Zhu J, He W, Lu W (2010) Folate-PEG-CKK 2-DTPA, A potential carrier for lymph-metastasized tumor targeting. Pharm Res 27:933–942
Sinha R, Kim GJ, Nie S, Shin DM (2006) Nanotechnology in cancer therapeutics: bioconjugated nanoparticles for drug delivery. Mol Cancer Ther 5:1909–1917
Hauff P, Reinhardt M, Briel A, Debus N, Schirner M (2004) Molecular targeting of lymph nodes with l-selectin ligand-specific US contrast agent: a feasibility study in mice and dogs. Radiology 231:667–673
Drobnik J (1991) Hyaluronan in drug delivery. Adv Drug Deliv Rev 7:295–308
Kaur CD, Nahar M, Jain NK (2008) Lymphatic targeting of zidovudine using surface-engineered liposomes. J Drug Target 16:798–805
Coppi G, Iannuccelli V (2009) Alginate/chitosan microparticles for tamoxifen delivery to the lymphatic system. Int J Pharm 367:127–132
Swart PJ, Beljaars L, Kuipers ME, Smit C, Nieuwenhuis P, Meijer DKF (1999) Homing of negatively charged albumins to the lymphatic system: general implications for drug targeting to peripheral tissues and viral reservoirs. Biochem Pharmacol 58:1425–1435
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Controlled Release Society
About this chapter
Cite this chapter
Singh, I., Swami, R., Khan, W., Sistla, R. (2014). Delivery Systems for Lymphatic Targeting. In: Domb, A., Khan, W. (eds) Focal Controlled Drug Delivery. Advances in Delivery Science and Technology. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-9434-8_20
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9434-8_20
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4614-9433-1
Online ISBN: 978-1-4614-9434-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)