Abstract
It does not matter what type of autopsy-based pathology you practice, be it foetal, neonatal and paediatric, adult, neuropathological or forensic, you will come across many cases where the patient has suffered localised or systemic organ failure and “shock” as part of their terminal illness. This maybe suggested within the clinical history or documented within the hospital notes but needs to be confirmed during the autopsy examination. However, if there is a delay between death and the autopsy examination then post-mortem autolysis will occur which may, especially if the time period goes beyond a day, confuse the picture presented to the pathologist. It is with this in mind that this chapter does not discuss the physiology of shock but rather concentrates on the macroscopic and microscopic pathology of shock and how, when possible, to differentiate the changes from that of post-mortem autolysis. Although the pathological descriptions of shock have been documented previously within the medical literature, these texts have, at times, been poorly illustrated. This chapter brings these texts together and concentrates on illustrating the macroscopic and microscopic changes of shock to provide a comprehensive reference source on this subject.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Preview
Unable to display preview. Download preview PDF.
Similar content being viewed by others
References
Thompson D, editor. The concise Oxford dictionary. 9th ed. Oxford: Claredon Press, 1995.
May C. Lord Moran’s memoir: Shell-shock and the pathology of fear. J R Soc Med 1998;91:95–100.
Reide U, Sandritter W, Mittermayer C. Circulatory shock: a review. Pathology 1981;13:299–311.
Post-mortem Changes. In: Janssen W, editor. Forensic histopathology. Berlin: Springer-Verlag, 1984;13–46.
Pietra G. The lung in shock. Hum Pathol 1974;5:121–2.
Katzenstein AA, Bloor CM, Leibow AA. Diffuse alveolar damage - the role of oxygen, shock and related factors. Am J Pathol 1976;85:210–28.
Addis BJ. Diffuse alveolar damage. In: Corrin B, editor. Systemic pathology, vol. 10. The respiratory system. London: Churchill Livingston, 1995;55–68.
Corrin B. Lung pathology in septic shock. J Clin Pathol 1980;33:891–4.
Schlag G, Redl H. Morphology of the microvascular system in shock: lung, liver and skeletal muscles. Crit Care Med l985;13:1045–9.
Orell SR. Lung pathology in respiratory distress following shock in the adult. APMIS Sect A 1971;79:65–76.
Moon VH. The pathology of secondary shock. Am J Pathol 1948;24:235–73.
Aabo K, Hansen KB. Megakaryocytes in pulmonary blood vessels. 1. Incidence at autopsy, clinicopathological relations especially to disseminated intravascular coagulation. APMIS. Sect A. 1978;86:285–91.
Pumphrey RSH, Roberts ISD. Investigating possible anaphylactic deaths. In: Burton J, Rutty G, editors. The Hospital Autopsy, 2nd ed. London: Arnold, 2001;147–58.
McGovern VJ. Shock. Pathol Ann. 1971;6:279–98.
McGovern VJ. Shock revisited. Pathol Ann 1984;19:15–36
McGovern VJ, Tiller DJ. Shock. A clinicopathological correlation. New York: Masson, 1980.
Krausz T, Cohen J. Shock. In: McGee J O’D, Isaacson PG, Wright NA, editors. Oxford textbook of pathology. Oxford: Oxford University Press, 1992;550–51.
Shock. In: Janssen W, editor. Forensic histopathology. Berlin: Springer-Verlag, 1984; 156–78
Evans TJ, Krausz T. Pathogenesis and pathology of shock. In: Anthony PP, MacSween RNM, editors. Recent advances in histopathology 16. London: Churchill Livingston, 1994;21–48.
Wiggers CJ. Physiology of shock. New York: Commonwealth Fund. 1950.
Hackle DB, Goodale WT. Effects of haemorrhagic shock on the heart and circulation of intact dogs. Circulation 1955;11:628–34.
Martin AM, Hackle DB. The myocardium of the dog in haemorrhagic shock. A histochemical study. Lab Invest 1963;12:77–91.
Lisagor P, Cohen D, McDonnell B, Lawlor D, Moore C. Irreversible shock revisited: mechanical support of the cardiovascular system: a case report and review. J Trauma 1997;42:1182–6.
McGovern VJ. Hypovolaemic shock with particular reference to the myocardial and pulmonary lesions. Pathology 1980;12:63–73.
Page DL, Caulfield JB, Kastor JA, DeSanctis RW, Sanders CA. Myocardial changes associated with cardiogenic shock. New Eng J Med 1971;285:133–7.
Todd GL, Baroldi G, Pieper GM, et al. Experimental catecholamine-induced myocardial necrosis. I. Morphology, quantification and regional distribution of acute contraction bands lesions. J Mol Cell Cardiol 1985a;17:317–38.
Davies MJ, Mann JM, editors. Systemic pathology, vol. 10. The cardiovascular system. Part B: Acquired diseases of the heart. London: Churchill Livingston, 1995;44–6
Dalgaad OZ. An electron microscopic study of glomeruli in renal biopsies taken from human shock kidney. Lab Invest 1960;9:364–6.
Waugh D, Schlieter W, James AW. Intraglomerular epithelial reflux: an early lesion of acute renal failure. Arch Pathol 1964;77:93.
Jennette JC, Olson JL, Schwartz MM, Silva FB, Heptinstall RH, editors. Acute renal failure. In: Heptinstal’s pathology of the kidney, 5th ed. London: Lippincott William and Wilkins,1998.
Martines G. Autolisi postmortale del tubulo nefronico sperimentalmente provocata. Riv Patol Clin Sper 1964;5:263.
Osvaldo I, Jakson JD, Cook ML, Latta H. Reactions of kidney cells during autolysis. Light microscopic observations. Lab Invest 1965;14:603.
Birgens HS, Henriksen J, Matzen P, Poulsen H. The shock liver. Acta Med Scand 1978;204:417–21.
Lefkowitch JH, Mendez L. Morphologic features of hepatic injury in cardiac disease and shock. J Hepatol 1986;2:313–27.
Ishak KG, Rogers WA. Cryptogenic acute cholangitis - assiociation with toxic shock syndrome. Am J Clin Pathol 1981;76:619–26.
Banks JG, Foulis AK, Ledingham IM, MacSween RNM. Liver function in septic shock. J Clin Pathol 1982;35:1249–52.
Cowley RA, Hawkins JR, Jones RT, Trump BF. Pathology and pathophysiology of the liver. In: Cowley RA, Trump BF, editors. Pathophysiology of shock, anoxia and ischaemia. Baltimore: Williams and Wilkins, 1982;285–300.
Muller PH, Willot M, Oliveira de SAFM, Debarge A. Aspects histologiques de l’autolyse hepatique. Acta Med Leg Soc (Leige) 1965;18:243.
Itoh M, Paulsen G, Guth PH. Hemorrhagic shock and acid gastric injury in the rat. Gastroenterology 1986;90:1103–10.
Bailey RW, Hamilton SR, Morris JB, Bulkley GB, Smith GW. Pathogenesis of non-occlusive ischaemic colitis. Ann Surg 1986;203:590–99.
Marston A, Pheils MT, Thomas ML, Morson BC. Ischaemic colitis. Gut 1966;7:1.
Bailey RW, Hamilton SR, Morris JB, Bulkley GB, Smith GW. Pathogenesis of non-occlusive ischaemic colitis. Ann Surg 1986;203:590–99.
McGovern VJ, Goulston SJM. Ischaemic enterocolitis. Gut 1965;6:213–20.
Kliegman RM, Fanaroff AA. Necrotising enterocolitis. New Eng J Med 1984;310:1093–103.
Whithead R, editor. Necrotising enterocolitis of the newborn. In: Gastrointestinal and oesophageal pathology. London: Churchill Livingstone, 1995;699–701.
Gilbert-Barness E, editor. Neonatal necrotising enterocolitis. In: Potter’s pathology of the fetus and infant, vol 2. London: Mosby, 1997;803–05.
Wigglesworth JS, editor. Intestinal infarction and necrotising enterocolitis. In: Perinatal pathology. London: WB Saunders, 1984;266–70.
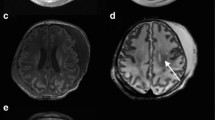
Auer RN, Sutherland GR. Hypoxia and related conditions. In: Graham DI, Lantos PL editors, Greenfield’s neuropathology, 7th ed. London: Arnold, 2002;233–80.
Kaur B, Rutty G, Timperley W. The possible role of hypoxia in the formation of axonal bulbs. J Clin Pathol 1999;52;203–09.
Harrington D, Rutty GN, Timperley WR. ß amyloid precursor protein axonal bulbs may form in non-head-injured patients. J Clin Forensic Med 2000;7:19–25.
Councilman WT, Mallory FB, Pearce RM. A study of the bacteriology and pathology of 220 fatal cases of diptheria. J Boston Soc Med Sci 1900;5:139–319.
Greendyke RM. Adrenal haemorrhage. Amer J Clin Pathol 1965;43:210–15.
Warshaw AL, O’Hara PJ. Susceptibility of the pancreas to ischaemic injury in shock. Ann Surg 1978;188:197–201.
Pfeffer RB, Lazzarini-Robertson A, Safadi D, Mixter G, Secoy CF, Hinton JW. Gradations of pancreatitis, edematous, through hemorrhagic, experimentally produced by controlled injection of microspheres into blood vessels in dogs. Surgery 1962;51:764–9.
Feiner H. Pancreatitis after cardiac surgery. Am J Surg 1976;131:684–8.
Seemayer TA, Osbourne C, De Chadarevian J-P. Shock-related injury of pancreatic Islets of Langerhans in newborn and young infants. Hum Pathol 1985;16:1231–4.
Bernstein J. Renal tubular and pancreatic islet necrosis in newly born infants. Am J Dis Child 1958;96:705–10.
Gmaz-Nikulin E, Plamenac P, Hegewald G, Gaon D. Pancreatic lesions in shock and their significance. J Pathol 1981;135:223–36.
Barzilai A, Ryback BJ, Medina JA, Toth L, Dreiling DA. The morphological changes of the pancreas in hypovolemic shock and the effect of pretreatment with steroids. Int J Pancreatol 1987;2:23–32.
Jones RT, Garcia JH, Mergner WJ, Pendergrass RE, Valigorsky JM, Trump BF. Effects of shock on the pancreatic acinar cell. Cellular and subcellular effects in humans. Arch Pathol 1975;99:634–44.
Emery JL, Bury HPR. Involutionary changes in the Islets of Langerhans in the foetus and newborn. Biol Neonat 1964;6:16–25.
Jaffe R. Pancreatitic Islets in Shock. In: Stocker JT, Dehner LP, editors. Pediatric pathology, 2nd ed, vol 2. London: Lippincott William and Wilkins, 2001;824.
Betz EH. Les modifications des glandes endocrines au cours des etats de shock. Acta Anaesthesiol Belg 1968;3:224–33.
Mukai S. Determination of post-mortem interval by histological examination of pancreas. Jap Z Leg Med 1955;9:19.
Kovacs K. Necrosis of anterior pituitary in humans. Part 1. Neuroendocrinology 1969;4:170–99.
Kovacs K. Necrosis of anterior pituitary in humans. Part 2. Neuroendocrinology 1969;4:200–41.
Kovacs K. Adenohypophysial necrosis in routine autopsies. Endocrinologie 1972;60:309–16.
Plaut A. pituitary necrosis in routine autopsies. Am J Pathol 1952;28:883–99.
Saeger W, Hanke D. Nekrosen der Hypophyse und ihre Beziehung zum Schock. Verh Dtsch Ges Pathol 1978;62:301.
Sheehan HL, Murdoch R. Post-partum necrosis of the anterior pituitary; pathological and clinical aspects. J Obst Gynaec Brit Emp 1938;45:456–90.
Sheehan HL The repair of post-partum necrosis of the anterior lobe of the pituitary gland. Acta Endocrinol 1965;48:40–60.
Sheehan HL, Davis JC. Pituitary necrosis. Br Med Bull 1968;24:59–70.
Horvath E, Scheithaver BW, Kovacs K, Lloyd RV. Hypothalamus and pituitary. In: Graham D, Lantos P, editors. Greenfields neuropathology. 7th ed, vol. 1. London: Arnold, 2002; 1024.
Latka H, AdamW. Hyaluronidase als Ursache fruher postmortaler Verandererunggen der Hypophyse. Dtsch Z Ges Gerichtl Med 1953;42:32.
Kojima M, Takahashi K. Pathological study on the changes of lymphatic tissues in shock with special reference to the secondary nodule lesion. Acta Pathol Jpn 1971;21:387–403.
Kojima M, Takahashi K, Yamaguchi A, Sue A, Terashima K. Experimental analysis on pathogenesis of the secondary nodule lesion in lymph nodes induced in shock. Acta Pathol Jpn. 1971;21:405–14.
Howat AJ, Variend S. Nuclear fragmentation and epitheliod change of germinal centres in the lymphoid tissue of child deaths. Pediatr Dev Pathol 1986;5:125–34.
Tappero P. Contributo allo studio tanatologico della milza. Minerva Med Leg (Torino) 1969;89:12.
Coen R, McAdams AJ Visceral manifestations of shock in congenital heart disease. Am J Ds Child 1970;199:383–9.
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2004 Springer-Verlag London Limited
About this chapter
Cite this chapter
Rutty, G.N. (2004). The Pathology of Shock Versus Post-mortem Change. In: Rutty, G.N. (eds) Essentials of Autopsy Practice. Springer, London. https://doi.org/10.1007/978-1-4471-0637-1_5
Download citation
DOI: https://doi.org/10.1007/978-1-4471-0637-1_5
Publisher Name: Springer, London
Print ISBN: 978-1-4471-1168-9
Online ISBN: 978-1-4471-0637-1
eBook Packages: Springer Book Archive