Abstract
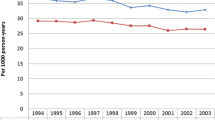
Heart failure (HF) is an epidemic disorder that currently affects more than 5 million people in the United States, with an estimated 550,000 new diagnoses each year. Given the increasing age of the population and the improved survival of patients from acute myocardial infarctions and other diseases, the incidence of heart failure will undoubtedly continue to grow. Current data from the NHLBI’s Framingham Heart Study suggests that at age 40, the lifetime risk of developing heart failure for both men and women is approximately one in five (or 20%), and 1- and 5-year mortality is about 30% and 50%, respectively. The Framingham study suggests that patients with heart failure have mortality rates four to eight times higher compared to the general population of the same age. Hospital discharges for HF rose from 877,000 in 1996 to 1,106,000 in 2006. Furthermore, the estimated cost of HF in the United States for 2010 is $39.2 billion. However, appropriate recognition and early treatment of heart failure, risk factors, and use of evidence-based therapies in patients already diagnosed with heart failure can help to prevent this expected increase in HF incidence and reduce the mortality, number of hospitalizations, and health care costs associated with this disorder.
Similar content being viewed by others
Keywords
- Heart Failure
- Chronic Heart Failure
- Cardiac Resynchronization Therapy
- Leave Ventricular Assist Device
- Heart Failure With Preserve Ejection Fraction
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Heart failure (HF) is an epidemic disorder that currently affects more than 5 million people in the United States, with an estimated 550,000 new diagnoses each year. Given the increasing age of the population and the improved survival of patients from acute myocardial infarctions and other diseases, the incidence of heart failure will undoubtedly continue to grow. Current data from the NHLBI’s Framingham Heart Study suggests that at age 40, the lifetime risk of developing heart failure for both men and women is approximately one in five (or 20%), and 1- and 5-year mortality is about 30% and 50%, respectively. The Framingham study suggests that patients with heart failure have mortality rates four to eight times higher compared to the general population of the same age. Hospital discharges for HF rose from 877,000 in 1996 to 1,106,000 in 2006. Furthermore, the estimated cost of HF in the United States for 2010 is $39.2 billion. However, appropriate recognition and early treatment of heart failure, risk factors, and use of evidence-based therapies in patients already diagnosed with heart failure can help to prevent this expected increase in HF incidence and reduce the mortality, number of hospitalizations, and health care costs associated with this disorder.
Etiology
Although the most common cause of heart failure is ischemic cardiomyopathy (up to two-thirds of all cases), the remaining heart failure conditions do not fit into this category. Appropriate identification of the etiology of heart failure is important to help with therapy.
The causes of heart failure can be further categorized by primary dysfunction (systolic or diastolic). There is considerable overlap with several factors that can independently result in heart failure with systolic dysfunction or heart failure with preserved left ventricular ejection fraction (HFpEF) or a combination of both.
Heart Failure with Systolic Dysfunction
Most simply, heart failure with systolic dysfunction can be defined as a reduction in ejection fraction from impaired contractility of the left ventricle. However, the pathophysiology behind heart failure is complex involving not just impaired myocardial contractility but activation of the neuroendocrine system leading to unfavorable cardiac remodeling that causes chamber enlargement and reduction in ejection fraction.
Chief Complaint/Symptoms
Oftentimes, there is no correlation between the severity of symptoms and the extent of ejection fraction reduction; therefore, a patient with a significantly reduced EF may be asymptomatic. In fact, up to one-half of all patients with left ventricular systolic dysfunction are without symptoms. However, in patients with symptoms, the most common and earliest presenting symptom is shortness of breath that manifests itself with progressively increasing severity as (1) exertional dyspnea, (2) orthopnea, (3) paroxysmal nocturnal dyspnea, and (4) dyspnea at rest.
-
1.
Exertional dyspnea: As heart failure progresses, the degree of activity needed to induce dyspnea declines. However, as mentioned earlier, there is not always a correlation between exercise capacity and LV function.
-
2.
Orthopnea: This symptom of heart failure presents itself as the heart failure becomes more advanced or in decompensated states. It is defined as shortness of breath that develops when lying down and is relieved with elevation of the head with pillows. Typically, orthopnea is characterized by the number of pillows required for sleeping. The change in the number of pillows needed is important in quantifying the heart failure. In advanced heart failure, orthopnea may be so severe that the patient cannot lie down and must sleep sitting upright in a chair to avoid pulmonary congestion.
-
3.
Paroxysmal nocturnal dyspnea: This symptom occurs as LV failure worsens and is often described as a sudden awakening by the patient after several hours of sleep causing the patient to immediately sit upright, gasping for air, with the associated feelings of severe anxiety/panic and suffocation. Bronchospasm may be present, as well.
-
4.
Dyspnea at rest: This symptom signals failure of compensatory mechanisms and end-stage heart failure. Dyspnea at rest results from decreased pulmonary compliance with increased airway resistance, as well as hypoxemia associated with increased pulmonary capillary wedge pressure, and decreased respiratory muscle function.
Other cardiac symptoms of heart failure include fatigue, weakness, low exercise tolerance, chest pain/pressure, palpitations, dizziness, syncope, anorexia, weight loss, abdominal pain, bloating, cough, insomnia, oliguria, and cerebral symptoms ranging from anxiety to depressed mood to memory impairment and confusion.
Signs/Physical Examination
The physical signs associated with heart failure are dependent upon the degree of compensation, the acuity, and chamber involvement (right-sided versus left-sided heart failure).
-
1.
Volume overload can cause a multitude of physical signs.
-
(a)
Pulmonary rales occur over the lung bases from the accumulation of fluid in the pulmonary interstitium and alveloli caused by elevated pulmonary capillary wedge pressures/left atrial pressures. Acute cardiogenic pulmonary edema is commonly characterized by rales with wheezing and frothy, blood-tinged sputum. However, the presence of pulmonary congestion is not accompanied by rales in 80% of patients with systolic heart failure because of chronic perivascular compensation and increased lymphatic drainage.
-
(b)
Dullness over the lung bases can also be a common sign of volume overload from extravasation of fluid into the pleural space.
-
(c)
Jugular venous pulse (JVP), measured at a 45° angle, can also be a marker of volume overload. The JVP remains the most accurate and commonly used clinical assessment tool to determine increased left-sided filling pressures with a sensitivity of 70% and specificity of 79%.
-
(d)
Third heart sound (S3 gallop) is an early sign of decompensated heart failure and signifies increased left-sided filling pressures in the setting of diminished LV function.
-
(e)
Mitral and tricuspid regurgitation murmurs often accompany decompensated heart failure with ventricular dilatation. However, there is little correlation between intensity of the murmur to the severity of heart failure as severe mitral regurgitation may have a soft murmur.
-
(f)
Edema, although a hallmark sign of heart failure with volume overload, can also be observed in other conditions, such as nephrotic syndrome, hypoproteinemia, or chronic venous insufficiency. It should be noted that for peripheral edema to occur requires a gain of at least 5 L of extracellular fluid volume in adults.
-
(g)
Ascites occurs in the setting of elevated right-sided filling pressures that causes increased pressures in the portal vein circulation.
-
(h)
Hepatomegaly is a common finding in patients with chronic right-sided heart failure; however, with acute heart failure, rapid congestion can cause hepatomegaly with a pulsatile liver that is palpable.
These last three physical findings, edema, ascites, and congestive hepatomegaly, are hallmark signs of right-sided heart failure when elevated right-sided heart pressures are transmitted to the hepatic and gastrointestinal venous circulation that results in previously mentioned symptoms of abdominal pain, bloating, anorexia, and nausea.
-
(a)
-
2.
Pulsus alternans is another sign commonly found with heart failure. It is defined as an alteration of one strong and one weak beat without a change in the cycle length during pulse palpation.
-
3.
Signs of peripheral perfusion (i.e. color, warm or cool extremities, capillary refill) can help gauge the stage of heart failure.
-
4.
Vitals signs can also help monitor the progression of heart failure. Low blood pressure, tachycardia, tachypnea, and narrow pulse pressure often signify an advanced stage of heart failure.
-
5.
Cardiac cachexia is often a sign of chronic heart failure because of anorexia and/or increased total metabolism.
Etiology (Table 11.1)
-
1.
Ischemic cardiomyopathy: As mentioned earlier, it is the most common cause of heart failure caused by coronary artery disease with subsequent wall-motion abnormalities and left ventricular systolic dysfunction. It is important to stress that stenosis of the coronary arteries does not automatically lead to ischemic cardiomyopathy. However, patients with ischemic cardiomyopathy who have viable myocardium do benefit from percutaneous and surgical revascularization, which can halt or even reverse the progression of heart failure.
-
2.
Dilated cardiomyopathy: Among young people, dilated cardiomyopathy is the most common cardiomyopathy accounting for about 25% of cases. More than 50% of all causes of dilated cardiomyopathy are idiopathic, with the remaining causes being infectious, inflammatory, toxic, high-output states, endocrine, nutritional disorders, autoimmune, congenital/inherited heart conditions, peripartum cardiomyopathy, hypertension, arrhythmia, stress-induced, and electrolyte deficiency. Dilated cardiomyopathy occurs with adverse cardiac remodeling which then leads to cardiac hypertrophy, dilation, and systolic dysfunction. Some nonischemic causes of dilated cardiomyopathy are reversible, and it is important to identify them early to establish appropriate treatment.
-
3.
Infectious cardiomyopathy: Most commonly, viral infections, such as HIV, CMV, coxsackievirus A and B, influenza, adenovirus, herpes viruses, poliovirus, enteroviruses, rubella, rubeola, hepatitis B or C virus, EBV, mumps, parvovirus B19, or echovirus are associated with infectious cardiomyopathy. Other causes can be the tick-borne illness, Rocky Mountain spotted fever, by the bacterial organism, Rickettsia rickettsii. In addition, fungi, such as aspergillosis, cryptococosis, coccidioidomycosis, and histoplasmosis, can also lead to a cardiomyopathy. The protozoa, Trypanosoma cruzi, leads to Chagas’ disease, which causes severe ventricular enlargement, often with apical aneurysm, seen with the cardiomyopathy. It is also associated with arrhythmias, thromboembolic stroke, and sudden death. Chagas disease is most commonly seen in Central and South America. Another protozoa that can cause a cardiomyopathy is Toxoplasmosis gondii. Helminths, such as trichinosis and schistosomiasis, can also result in a cardiomyopathy. Infectious cardiomyopathies can also be a result of bacterial illnesses by Legionella, Clostridium, streptococci, staphylococci, salmonella, and Shigella. Another reported cause of infectious cardiomyopathies is Lyme disease by the spirochete, Borelia burgdorferi.
-
4.
Inflammatory cardiomyopathy: This disease is characterized by the inflammatory infiltration of the myocardium, and therefore, is also known as myocarditis with cardiac dysfunction. Common causes of an inflammatory cardiomyopathy can be from an infectious etiology or from hypereosinophilia, cardiotoxic agents, systemic autoimmune diseases, or collagen vascular diseases. Unfortunately, an inflammatory cardiomyopathy caused by a systemic process has a poor prognosis as it often responds unfavorably to medical therapy and cardiac transplantation. Giant cell myocarditis is a rare, but lethal type of inflammatory cardiomyopathy with a 1-year mortality rate of up to 80%, median survival of 3–5 months from onset of symptoms that are consistent with progressive heart failure.
-
5.
Autoimmune: Systemic lupus erythematosus is one of the common autoimmune disorders that can cause heart failure with systolic dysfunction. It is often associated with myocarditis and an inflammatory cardiomyopathy. Another autoimmune disorder, Celiac disease, can also cause an idiopathic dilated cardiomyopathy. Following a gluten-free diet can reverse the cardiomyopathy and improve cardiac function in these patients.
-
6.
Cardiotoxic agents: Common toxins affecting the heart are chemotherapeutic agents, particularly anthracyclines, alcohol, cocaine, and catecholamines. Chemotherapeutic agents cause myocyte destruction that lead to a dilated cardiomyopathy. It is recommended that prior to chemotherapy, patients have a baseline echocardiogram. Radionuclide ventriculography (MUGA scan) provides very accurate measurements of systolic function. It is often considered the preferred imaging modality in circumstances where precise measurements of systolic function are needed, such as the case with patients undergoing chemotherapy that undergo periodic cardiac evaluation. Alcohol is another common cause of toxin-mediated cardiomyopathy and accounts for approximately 33% of all cases of dilated cardiomyopathy. In early stages, complete abstinence from alcohol may entirely reverse the cardiomyopathy; however, continued use of alcohol can lead to a 5-year mortality of 50%.
-
7.
Valvular disorders: Valve-related systolic heart failure is associated most commonly with mitral regurgitation, aortic regurgitation, and/or severe aortic stenosis and outflow tract obstruction. Mitral and aortic regurgitation lead to heart failure from a constant state of volume overload, whereas severe aortic stenosis and outflow tract obstruction eventually cause LV dysfunction and heart failure.
-
8.
Endocrine disorders: Because thyroid conditions (i.e. hypo- or hyperthyroidism) can commonly occur, patients with new-onset heart failure should have thyroid function testing as heart failure caused by thyroid disorders is potentially reversible. With hypothyroidism, a decreased cardiac output with bradycardia, and in some cases, a pericardial effusion can occur. In contrast, hyperthyroidism often presents with tachycardia or atrial fibrillation and can be accompanied by fatigue and weight loss. Patients on amiodarone are at an increased risk for developing hyperthyroidism. In Cushing’s syndrome, the excess cortisol causes a dilated cardiomyopathy, which can also occur in the presence of excess growth hormone, as seen in patients with acromegaly. In patients with pheochromocytoma, the excess adrenergic stimulants cause direct injury to cardiac myocytes that can lead to systolic dysfunction.
-
9.
Stress-induced cardiomyopathy (Takotsubo cardiomyopathy): Also known as “broken heart syndrome,” this cardiomyopathy occurs after an acute stress and is also thought to be a result of the excess sympathomimetic amines following an acutely stressful event. Subsequent echocardiogram shows a reversible apical ballooning.
-
10.
Hypertensive cardiomyopathy: Also known as “burnt-out hypertensive heart,” it is the final outcome that initially begins with LV hypertrophy until progression to LV dysfunction thought to be from microvascular ischemia. Hypertensive cardiomyopathy can present in conjunction with ischemic cardiomyopathy as hypertension contributes significantly to coronary artery disease development. With appropriate medical treatment, the negative effects of hypertensive cardiomyopathy can be slowed or reversed.
-
11.
Congenital/inherited cardiomyopathy: Familial dilated cardiomyopathy account for approximately 20–30% of all cases of dilated cardiomyopathy. It carries an unfavorable prognosis and is associated with gene mutations. Arrhythmogenic right ventricular dysplasia (ARVD) is defined by fatty infiltration of the right ventricle that can be difficult to diagnose by endomyocardial biopsy given the patchiness of the disease. However, MRI can be helpful in making the diagnosis. ARVD often occurs in young people, predominantly men, and presents with syncope or ventricular arrhythmias. Although, infrequently, it can occur with right-sided heart failure. Another inherited disorder that affects the right ventricle is Uhl’s anomaly. Unlike ARVD, however, Uhl’s anomaly is often associated with right-sided heart failure. It is caused by death of cardiac myocytes throughout the right ventricle and is characterized by a paper-thin right ventricular wall. It presents in early childhood and often, the only cure is cardiac transplantation. Left ventricular noncompaction is the abnormal interference of normal ventricular development leading to systolic dysfunction, ventricular arrhythmias, and thromboembolism. Muscular dystrophies, such as Duchenne’s and Becker’s, arise from genetic mutations and are more commonly associated with a dilated cardiomyopathy. In addition, Fabry’s disease, an alpha-galactosidase A deficiency, is a rare occurrence that can lead to LV hypertrophy and dysfunction.
Treatment
The treatment goals for acute decompensated heart failure and chronic heart failure differ. We will discuss the precipitants and management of acute decompensated heart failure later. In chronic heart failure management, the main objectives are to improve symptoms, reduce hospitalizations, and prolong survival. The diagram below illustrates the pathophysiology behind chronic systolic heart failure. Our understanding of this model is the basis behind the main medical therapies used in the treatment of chronic heart failure. These agents target different points of the diagram to interfere with this deleterious cycle to reduce symptoms and adverse effects that ultimately lead to death. Table 11.2 summarizes the main clinical trials for each class of agents critical to the management of chronic heart failure. Table 11.3 summarizes the drug dosing of the primary medical therapies in chronic heart failure treatment.

-
1.
Angiotensin-converting enzyme inhibitors (ACE-I)
The long-term benefits of this class of drugs can be attributed to their effects on the renin-angiotensin-aldosterone system (RAAS). ACE-I function by inhibiting the enzyme that converts angiotensin I to angiotensin II, thereby preventing the negative downstream effects of the neurohormonal RAAS pathway caused by excess angiotensin II, aldosterone, and catecholamines. ACE-I have been shown to reverse the pathologic cardiac remodeling caused by progressive myocardial fibrosis, inflammation, and apoptosis associated with overstimulation of the RAAS pathway. Several randomized trials have established the benefit of ACE-I in patients with chronic LV dysfunction (Table 11.2). Consistently, ACE-I were shown to decrease mortality by approximately 20–25% at 1–5 years. Although low doses of an ACE-I should be used at first, over time, however, the dose should be gradually uptitrated to the optimal dosage used in the management of heart failure (Table 11.3). Because hyperkalemia and acute renal insufficiency can occur with ACE-I, close monitoring with labwork is advised after initiation or increase of an ACE-I. Small increases in creatinine levels (up to 30%) should be tolerated and expected, and the ACE-I should not be discontinued. If the creatinine increases by more than 30%, the ACE-I dose can be halved. However, if the creatinine level increases by more than 100%, the ACE-I should be held at that time. If hyperkalemia occurs, first discontinue any potassium supplementation, and if hyperkalemia continues to persist, then the ACE-I dose can be reduced. Other side effects of ACE-I are hypotension, cough, teratogenicity, and angioedema. For patients that develop a true ACE-inhibitor cough, angiotensin-II receptor blockers (ARBs) are an acceptable alternative. However, for patients who develop angioedema from an ACE-I, it is an absolute contraindication to use any type of ACE-I or ARB. Angioedema can occur within 2 weeks of initiation of an ACE-I or can present months to years after starting the medication.
-
2.
Angiotensin-II receptor blockers (ARBs)
ARBs also work by targeting the RAAS pathway and function by inhibiting the angiotensin II type 1 receptors. ARBs act downstream of angiotensin-converting enzyme inhibitors and weaken the effects of angiotensin II. Clinical trials have shown ARBs to be equivalent to ACE-I in the management of heart failure. They remain acceptable alternatives in patients who are ACE-I intolerant, usually to the associated cough. Despite ARBs being better tolerated, they have the same side effect profile as ACE-inhibitors, with the exception of cough, and therefore, should be used and monitored in the same way as ACE-I. Although a logical hypothesis might be that combination therapy with an ACE-inhibitor and an ARB would provide greater inhibition of the RAAS pathway and increased benefit in heart failure patients, data to support this theory have been inconclusive. The CHARM-ADDED trial showed that the addition of an ARB to an ACE-inhibitor reduced heart failure hospitalizations and cardiac mortality by 15% compared to monotherapy with an ACE-I alone. However, in contrast, the VALIANT trial revealed no additional benefit in the use of combination therapy, and in fact, showed increased hypotension and hyperkalemia.
-
3.
Aldosterone antagonists
The third class of therapeutic agents that target the RAAS pathway and provide a significant mortality reduction in patients with heart failure is aldosterone receptor antagonists, such as spironolactone and eplerenone. The benefit of these drugs is derived from the inhibition of aldosterone, an adrenal hormone produced through angiotensin II-dependent and -independent pathways. Aldosterone has been shown to cause fibrosis and adverse remodeling of the myocardium. The most common side effect of aldosterone antagonists is hyperkalemia, which can be exacerbated in patients with renal insufficiency or in those already taking an ACE-inhibitor or ARB. As a result, regular monitoring is required. In patients with creatinine 2.0–2.5 mg/dL or potassium 4.5–5 mg/day, the aldosterone antagonist should be started at a lower dose (12.5 mg/day or 25 mg every other day), and the potassium supplement should be discontinued or held. Aldosterone antagonists should be avoided in patients with a baseline creatinine >2.5 mg/dL or potassium ≥ 5.0 mEq/L. In addition, although spironolactone may also cause gynecomastia and galactorrhea, these side effects are rarely associated with eplerenone.
-
4.
Beta-blockers
In addition to the RAAS inhibitors, beta-blockers are also essential to the management of chronic heart failure with LV systolic dysfunction through their actions on the neurohormonal axis. In heart failure, the sympathetic nervous system is chronically activated causing sustained stimulation of beta-receptors that eventually leads to a downregulation and desensitization of these beta-receptors to beta-adrenergic agonists. As a result, there is a reduced inotropic and chronotropic response of the myocardium to normal adrenergic stimulation. These effects are reversed with the initiation of beta-blockers as they help to upregulate beta 1-receptors and enhance cardiac contractility. Only carvedilol (Coreg), metoprolol succinate (Toprol XL), and bisoprolol have been approved for the treatment of chronic heart failure. Beta-blockers have consistently been shown to reduce mortality by approximately 25–45%. In general, beta-blockers should not be started in the setting of decompensated heart failure. It is recommended that patients be stable, clinically euvolemic, and already on an ACE-I or ARB prior to starting a beta-blocker. Beta-blockers should be initiated at low doses and slowly up-titrated every 2–4 weeks until goal dosages in the optimal management of heart failure are reached. Beta-blockers have a myriad of side effects, most commonly fatigue and dizziness/lightheadedness related to hypotension. Fatigue typically improves after 1–2 weeks of treatment, and in circumstances of recurrent hypotension, beta-1-selective agents, such as metoprolol succinate, may have lesser blood pressure-lowering effects than carvedilol, which has nonselective, alpha-1-receptor inhibition, as well. Beta-1-selective agents may also be better tolerated in patients with bronchospasm. Other adverse effects are bradycardia and worsening heart failure (i.e. increased fluid retention and congestion), which can occur given the negative inotropic effects of beta-blockers. Dose reduction and slower up-titration of beta-blockers, as well as more aggressive diuresis and salt restriction may be necessary to minimize these effects. Beta-blockers should be avoided in patients with advanced conduction system disease, unless a permanent pacemaker is present.
-
5.
Hydralazine and nitrates
For patients intolerant to ACE-inhibitors or ARBs, combination therapy with hydralazine and nitrates is an acceptable alternative in the management of chronic heart failure as it improves symptoms and reduces mortality (V-HEFT I trial). Furthermore, this vasodilator combination therapy was shown to confer a 43% decrease in mortality in African Americans with advanced heart failure already on optimal medical therapy with an ACE-I/ARB and beta-blocker (A-HEFT trial). Based on these significant results, the combination of hydralazine and nitrates is recommended for the management of chronic heart failure in this population of patients. Side effects of hydralazine are reflex tachycardia and a lupus-like syndrome, whereas nitrates can causes headaches, hypotension, and tolerance after continuous use.
-
6.
Diuretics
Diuretic therapy helps with symptomatic management in chronic heart failure by maintaining euvolemia in patients. Because overuse of diuretics is associated with electrolyte abnormalities and organ dysfunction (i.e. acute renal failure), only the lowest dose of diuretic needed to maintain euvolemia should be used. The loop diuretics furosemide (Lasix), torsemide (Demadex), and bumetanide (Bumex) are the most commonly used. Torsemide and bumetanide are more expensive loop diuretics but have better bioavailability and are more effective in diuretic-resistant patients. The conversion from oral furosemide to torsemide to bumetanide is about 40:20:1. In the case of intravenous-to-oral dose conversions, the intravenous and oral doses for both torsemide and bumetanide are equivalent, whereas the conversion from intravenous-to-oral furosemide is 1:2. If loop diuretics do not adequately prevent volume overload, a thiazide diuretic, such as metolazone (Zaroxolyn) or hydrochlorothiazide, can be added to assist with further diuresis. Thiazide diuretics work by inhibiting the reabsorption of Na+/Cl− in the distal convoluted tubule, thereby allowing for increased diuresis. The effective combination of a loop diuretic with a thiazide can produce substantial volume depletion. As a result, it is recommended to use a thiazide with a loop diuretic for only short-term with close monitoring of electrolytes and renal function.
-
7.
Digoxin
The use of digoxin in the management of chronic heart failure is controversial given its narrow therapeutic index and adverse reactions. As a result, it is often reserved for patients that have heart failure with concomitant atrial fibrillation, or for patients on optimal medical therapy who continue to be frequently hospitalized. The DIG trial showed that although digoxin did not improve mortality, it did decrease heart failure hospitalizations. Digoxin is a cardiac glycoside derived from the foxglove plant that functions as both a positive inotrope and a negative chronotropic agent. It increases intracellular calcium by blocking the Na-K-exchange ion channel, thereby increasing contractility. Digoxin levels < 1 ng/mL are desirable with toxicity occurring at levels greater than 2 ng/mL. As a result, digoxin should be used with caution in patients with renal insufficiency and in the elderly. Adverse events associated with digoxin have included cardiac arrhythmias (bidirectional VT, atrial tachycardia with AV block, atrial fibrillation with regular ventricular response), gastrointestinal symptoms, and neurological manifestations (i.e. visual changes/blurriness, dizziness, confusion, hallucinations). Hypokalemia and hypomagnesemia can exacerbate these negative effects, as well as lower the threshold for digoxin toxicity.
-
8.
Other therapies in chronic heart failure with systolic dysfunction
-
(a)
Cardiac resynchronization therapy (CRT): Up to one-third of patients with heart failure develop ventricular dyssynchrony (defined electrically as a QRS duration >120 ms, particularly those with a left bundle branch block morphology), which is associated with reduced cardiac efficiency. The benefits of biventricular pacemakers on mortality and morbidity in this subgroup of patients were evaluated in the COMPANION and CARE-HF trials. In these large, randomized studies, CRT was associated with a definitive mortality benefit, as well as a reduction in hospitalizations in comparison to patients receiving optimal medical therapy alone. The more recent MADIT-CRT trial also demonstrated a reduction in mortality and/or heart failure events in patients with heart failure. Biventricular pacemakers can consist of a right atrial lead with a right ventricular lead +/− ICD and epicardial left ventricular lead (placed through the coronary sinus). This allows biventricular pacemakers to resynchronize LV contraction and improve cardiac function. Based on data from the COMPANION and CARE-HF trials, CRT can be considered in chronic heart failure patients with dyssynchrony (QRS ≥ 120 ms), LVEF ≤ 35%, and NYHA functional class III-IV symptoms despite being on optimal medical management. MADIT-CRT trial showed benefit of CRT in patients with LVEF ≤ 30%, QRS ≥ 130 ms, NYHA functional class I-II HF symptoms, and were in sinus rhythm.
-
(b)
Implantable Cardiac Defibrillators (ICD): ICD implantation is frequently used in patients with chronic heart failure with systolic dysfunction for the primary prevention of sudden cardiac death from ventricular arrhythmias. The MADIT and MADIT-II trials demonstrated a survival benefit of ICD implantation in patients with ischemic cardiomyopathy with LVEF ≤ 30%. Results from the subsequent SCD-HEFT trial further showed a survival benefit of ICD in patients with nonischemic cardiomyopathy with LVEF ≤ 35%, as well. However, because patients with nonischemic cardiomyopathy often respond favorably to optimal medical therapy with LVEF improvement, at least a 3-month trial of optimal medical therapy (at least an ACE-I/ARB and beta blocker) in these patients must be attempted with LVEF remaining depressed despite medical management before ICD can be implanted. In addition, because the DINAMIT trial showed no mortality benefit for ICDs implanted within 40 days after an acute myocardial infarction, these patients with ischemic cardiomyopathy must wait at least 40 days before ICD implantation. Although the mortality benefit associated with ICD implantation has been established, in certain patients, ICD therapy may not be ideal given its huge cost and multiple risks. For example, in patients that are of an advanced age or have significant, life-shortening comorbidities, the survival benefit that ICD implantation can confer on these patients is reduced. Also, the risks associated with ICD implantation include inappropriate shocks, device infection, generator-site hematoma, cardiac rupture, and pneumothorax.
-
(a)
Heart Failure with Preserved Left Ventricular Ejection Fraction (Diastolic Heart Failure)
Heart failure with preserved ejection fraction (HFpEF) represents the other category of chronic heart failure. In fact, studies have shown that approximately one-half of patients with heart failure have a preserved ejection fraction. More commonly, HFpEF occurs in women and patients >65 years of age. Although it was initially thought that patients with HFpEF had improved survival outcomes, the mortality rates are actually similar in both types of heart failure.
HFpEF can be characterized by (1) normal or mildly abnormal systolic LV function (2) signs or symptoms of congestive heart failure and (3) evidence of diastolic dysfunction. HFpEF arises when myocardial relaxation or distensibility is disturbed leading to high cardiac filling pressures that are needed to maintain appropriate cardiac output. Common disorders that affect the viscoelastic properties or compliance of the LV are hypertension, LV hypertrophy, diabetes, obesity, and coronary artery disease. Other causes may be infiltrative processes (amyloid, sarcoid, hemochromatosis), hypertrophic cardiomyopathy, high output cardiac disorders (arteriovenous malformation, arteriovenous fistula, hyperthyroidism, anemia), and constrictive disease processes. Conditions such as atrial fibrillation and chronic renal insufficiency often can exacerbate diastolic heart failure.
Chief Complaint/Symptoms
The symptoms associated with HFpEF are identical to those of systolic heart failure that were previously mentioned. Oftentimes, a patient with preserved systolic function who is compensated will remain asymptomatic. However, dyspnea is typically the earliest symptom to occur.
Signs/Physical Examination
There are no specific clinical signs to distinguish systolic from diastolic heart failure. However, in general, heart failure patients with preserved systolic function more commonly present with acute or “flash” pulmonary edema with hypertension. On the contrary, patients with HFpEF can also have a slow and steady fluid accumulation presentation. In addition, when HFpEF occurs in the setting of constriction or restriction, these patients may present mainly with signs of right-sided heart failure, such as edema, ascites, abdominal distension, congestive hepatomegaly, and a positive hepatojugular reflex. Other signs that can be associated with pericardial constriction are Kussmaul’s sign, which is paradoxical elevation of jugular venous pressure on inspiration, and Friedrich’s sign, which is a “flickering” noted in the jugular venous pressure that represents a rapid “y” descent/short “y” duration.
Etiology
-
1.
LV Hypertrophy (LVH): Systemic hypertension, hypertrophic cardiomyopathy, or LV outflow obstruction can cause LV hypertrophy. The increased wall thickness associated with LVH reduces passive filling. Subendocardial ischemia can also be found with LVH and can interfere with active myocyte relaxation.
-
2.
Coronary Artery Disease (CAD): As just mentioned, active myocyte relaxation can be diminished by ischemia, either acute or chronic. Chronic ischemia, scar tissue from a prior myocardial infarction, or pathologic remodeling of the myocardium lead to reduced LV compliance and impaired passive filling. In addition, ischemia can cause tachyarrhythmias, such as atrial fibrillation, that decrease diastolic filling time.
-
3.
Restrictive cardiomyopathy: Myocardial and endomyocardial restrictive diseases can be categorized as being either infiltrative or noninfiltrative or can be classified as primary or secondary. Most myocardial infiltrative diseases are considered secondary restrictive cardiomyopathies, whereas myocardial noninfiltrative and endomyocardial diseases are primary restrictive cardiomyopathies. These diseases cause the heart to become rigid and resistant to ventricular filling during diastole.
-
(a)
Myocardial infiltrative diseases/Secondary restrictive cardiomyopathies
-
(i)
Amyloidosis: In amyloid heart disease, interstitial deposits (amyloid deposits/insoluble amyloid fibrils) replace normal cardiac myofilaments, thereby affecting myocardial contractility. The major types of amyloidosis are primary, secondary, familial, or senile. Primary amyloid is associated with multiple myeloma and is caused by overproduction of light-chain immunoglobulins from a monoclonal population of plasma cells. Secondary amyloid is typically associated with inflammatory conditions, such as rheumatoid arthritis, Crohn’s disease, and tuberculosis. Lastly, familial and senile amyloidosis leads to overproduction of transthyretin. Endomyocardial biopsy is the gold standard for diagnosing amyloid heart disease (Congo red stain of amyloid deposits on histology). However, cardiac MRI has become an increasingly popular imaging modality used to detect cardiac amyloidosis. On cardiac MRI, a distinct pattern of late gadolinium enhancement along the subendocardium and myocardium is noted in cases of cardiac amyloid disease. Cardiac MRI for the diagnosis of cardiac amyloidosis yields a sensitivity of 80%, specificity of 94%, positive predictive value of 92%, and negative predictive value of 85%. Echocardiography can also be used in the diagnosis of cardiac amyloid. Typical echocardiographic findings associated with cardiac amyloidosis include a granular, sparkling appearance of thickened ventricular walls and significant biatrial enlargement. Patients with amyloid may have no evidence of LVH on EKG despite the presence of LVH on echocardiogram. The extent of wall thickness determines survival; in patients with increased wall thickness, the average survival is <6 months. Overall, however, cardiac amyloidosis has a poor prognosis as patients with a normal wall thickness have only an average survival of 2.4 years. Cardiac transplantation is contraindicated in patients with systemic amyloidosis.
-
(ii)
Sarcoidosis: Infiltration of noncaseating graulomas with patchy scar formation in the heart characterizes sarcoidosis with cardiac involvement. In all patients with cardiac sarcoidosis, while it is clinically recognized in only 5% of patients, at autopsy, cardiac involvement is seen in 25% of patients. Myocardial restriction occurs as a result of the patchy scar formation, and the sarcoid granulomas cause conduction system disease that can result in sudden cardiac death from ventricular tachyarrhythmias or high-degree heart block. As a result, pacemaker placement is recommended in patients with cardiac sarcoidosis and conduction system disease, and ICD placement is recommended in the subset of patients with a history of VT. Because of the patchy nature of the disease, endomyocardial biopsy has a sensitivity of only 20–30% in the diagnosis of cardiac sarcoidosis. The presence of giant cells and noncaseating granulomas on biopsy confirms cardiac sarcoidosis. Echocardiography is not sensitive in the detection of cardiac sarcoid. In contrast, cardiac MRI is a highly sensitive method that can detect early cardiac sarcoid and can be used serially to monitor treatment response. Cardiac transplantation as a treatment for cardiac sarcoidosis is a possibility in certain patients.
-
(iii)
Hemochromatosis: Primary hemochromatosis occurs from an autosomal recessive genetic abnormality that causes increased absorption of iron from the gastrointestinal tract, whereas secondary hemochromatosis is a result of iron overload from repeated blood transfusions. In both instances, the presence of excessive iron leads to iron deposition in the myocardium causing a restrictive cardiomyopathy. Treatment of hemochromatosis often is phlebotomy and chelation therapy.
-
(iv)
Glycogen storage diseases: Gaucher’s, Hurler’s, and Fabry’s diseases are the most common of these genetically transmitted diseases. Cardiac involvement is often characterized by LV wall thickness.
-
(i)
-
(b)
Myocardial Noninfiltrative Disease/Primary Restrictive Cardiomyopathy
-
(i)
Idiopathic restrictive cardiomyopathy: This condition can be inherited in an autosomal dominant pattern or can occur sporadically. It is associated with patchy endocardial fibrosis that is difficult to diagnose with endomyocardial biopsy. This interstitial fibrosis can result in variable hypertrophy that can be seen, along with biatrial enlargement and near-normal LV dimensions, on echocardiography. Mean survival time is 9 years. Cardiac transplantation is a treatment option for some patients.
-
(i)
-
(c)
Endomyocardial Diseases/Primary Restrictive Cardiomyopathies
-
(i)
Hypereosinophilic syndrome (Loeffler’s endocarditis): As the name suggests, this restrictive cardiac disease occurs in the setting of eosinophilia where activated eosinophils release their cytoplasmic granular content that causes toxic damage and destruction to the endomyocardium. Subsequent endocardial thickening and obliteration of the cardiac apex occurs as a result. Another associated complication that can occur is a mural thrombus. As a result, anticoagulation, as well as corticosteroids, cytotoxic drugs, and typical heart failure medications are commonly used in treatment.
-
(ii)
Carcinoid heart disease: The elevated concentration of serotonin and 5-hydroxyindoleacetic acid associated with untreated carcinoid syndrome leads to formation of lesions, typically in the right ventricular endocardium. These vasoactive substances can also affect the right-sided heart valves (carcinoid valvular disease).
-
(i)
-
(a)
-
4.
Pericardial constriction (constrictive pericarditis): Constrictive pericarditis is a result of chronic inflammation that causes the pericardium to become thickened by fibrosis, scarring, and/or calcification. Consequently, the pericardial space is obliterated in the process and diastolic function is adversely affected, as a result. The loss of pericardial compliance interferes with normal cardiac filling by placing a constraint on the heart. As the ventricles begin filling at the start of diastole, this external volume constraint causes pressures to rapidly increase causing ventricular filling to prematurely stop. An equalization of pressures in all four cardiac chambers is typically seen with pericardial constriction. Common causes are mantle chest radiation, open-heart surgery, idiopathic or viral pericarditis, collagen vascular disease, end-stage renal disease/hemodialysis, malignancy, and tuberculosis. It is important to note that postcardiotomy and chest irradiation can result in pericardial constriction or restrictive cardiomyopathy. To help distinguish between constriction and restriction, echocardiography and right- and left- heart catheterizations are used. Findings on two-dimensional echocardiography with Doppler suggestive of constriction are septal bounce (rapid early diastolic filling); thickened, echogenic pericardium; and adherent pericardium to the myocardium
Treatment
Unlike in patients with systolic dysfunction, to date, there have been no large, randomized clinical trials of therapies that demonstrate a mortality benefit in patients with HFpEF. For example, the CHARM-preserved trial suggested candesartan therapy had a 15% relative risk reduction in hospitalizations; however, there was not a mortality benefit. As a result, there are no clear guidelines to direct optimal medical management in this group of heart failure patients. Therapy, therefore, is instead geared towards relief of symptoms, such as volume overload, and treatment of causative factors, such as hypertension, atrial fibrillation, and coronary artery disease.
For instance, diuretics should be used to control signs and symptoms of volume overload, such as pulmonary congestion and peripheral edema. Simultaneously, strict restriction on fluid and sodium intake should be implemented to further prevent volume overload.
In addition, in those patients with atrial fibrillation, rapid ventricular rates are poorly tolerated by further impedance of diastolic filling. Medications such as beta-blockers and calcium channel blockers are helpful in reducing the heart rate, thereby allowing improved diastolic filling. Interestingly, there is little data to support the hypothesis that the conversion of atrial fibrillation to sinus rhythm improves outcomes in patients with HFpEF even though atrial fibrillation often leads to decompensation in patients with diastolic dysfunction.
In the large subset of patients with HFpEF and coexisting hypertension, systolic and diastolic blood pressures should be treated aggressively according to the Joint National Committee (JNC) 7 guidelines. Treatment of hypertension has been shown to diminish cardiac hypertrophy, improve ventricular relaxation and distensibility, and subsequently improve diastolic filling.
In those patients with coronary artery disease causing chronic ischemia and associated diastolic dysfunction, coronary revascularization can be considered, along with lipid-lowering agents, antiplatelet therapy, and beta-blockade.
Contrary to most patients with diastolic dysfunction who face a dismal prognosis, patients with diastolic dysfunction caused by constrictive pericarditis can be treated with pericardiectomy. Unfortunately, despite similarities in presentation, patients with restrictive cardiomyopathies do not have a curative treatment and fall into the general category of patients with HFpEF where medical therapies provide only symptomatic relief and can only slow down the progression of disease.
Acute Decompensated Heart Failure
There are several precipitants that can exacerbate chronic heart failure, either with systolic dysfunction or preserved ejection fraction, and cause an acute decompensated state (Table 11.4).
Treatment should first be geared towards identifying and potentially reversing any underlying cause. The medical therapies used in the acute setting are with the goal of improving symptoms associated with respiratory and circulatory compromise. Hemodynamic monitoring should be considered as treatments are optimized for organ perfusion and normalization of cardiac filling pressures and function.
Treatment
-
1.
Oxygenation
In acute decompensated heart failure, oxygen saturation should be maintained at least ≥90%. Positive airway ventilation and/or intubation may be necessary to achieve this goal.
-
2.
Vasodilators
Acute decompensated heart failure in the setting of elevated blood pressures often presents with acute or “flash” pulmonary edema caused by increased vascular resistance and poor diastolic filling from diminished left ventricular relaxation. Vasodilators, such as nitroglycerin, are first-line drug therapy in these instances but should not be used in patients in cardiogenic shock.
-
3.
Diuretics
Diuretics provide not only a vasodilatory effect but can reduce intravascular volume, which oftentimes helps to relieve the acute presentation of pulmonary edema in decompensated states. With diuretic therapy, 66% of patients have improved symptoms by 24 h and 80% of patients by 3 days or at time of discharge. Diuretics are commonly administered intravenously with close monitoring of electrolytes, net fluid balance, and daily weights. In cases with associated renal insufficiency, ultrafiltration can be used as an alternative to pharmacologic diuresis to assist with fluid removal in volume overloaded states.
-
4.
Inotropes
Acute decompensated heart failure with hemodynamic compromise may warrant the need for inotropic therapy to improve tissue perfusion. Both intravenous dobutamine and milrinone can accomplish this through their ability to increase cardiac output. However, results from trials, such as the OPTIME-CHF and ADHERE trials, do not support the routine use of inotropes because mortality and morbidity are not reduced and there is actually an increase in adverse events. Persistent hypotension, myocardial ischemia, and cardiac arrhythmias have been noted. In some cases, vasopressors, such as norepinephrine, dopamine, and vasopressin are temporarily used to treat the associated hypotension with inotropic use.
-
5.
Mechanical Support
Intra-aortic balloon pumps (IABP) can be used in patients with cardiogenic shock to provide temporary hemodynamic stability. An IABP helps to reduce afterload, augment cardiac output, and decease myocardial oxygen requirement. Other devices that can be used in the setting of acute cardiogenic shock are percutaneous ventricular assist devices and left ventricular assist devices (LVAD), which will be addressed later in this chapter.
Classification of Heart Failure
There are three main classification systems in the assessment of heart failure: New York Heart Association (NYHA) functional classification, American College of Cardiology and American Heart Association (ACC/AHA) staging system, and the Killip classification. The NYHA functional classification system is the most commonly used method to describe signs and symptoms of heart failure (Table 11.5).
The ACC/AHA staging system describes heart failure as a progression of disease (Table 11.6).
The Killip classification system is often employed in patients after acute coronary syndromes or can be helpful in describing patients with heart failure who require placement of a pulmonary artery catheter (Table 11.7).
These three classification models provide an accurate assessment of patients with heart failure and are another standard used by health care providers to reliably estimate prognosis and mortality rate. For example, a patient classified as NYHA functional class IV has a 1-year survival rate of between 30% and 50%.
Prognosis
There are several predictors that can be utilized to accurately assess survival in patients with heart failure. The Seattle Heart Failure Model is a risk-prediction tool that incorporates these factors, some of which are NYHA class, age, LV ejection fraction, and cardiac dyssynchrony, and provides the ability to calculate survival probability in a patient with heart failure.
Diagnostic Testing
We have discussed the clinical presentations and etiologies of both chronic and acute heart failure. This section will focus on accurately establishing the diagnosis of heart failure upon initial evaluation of a patient with presenting symptoms (as described earlier in this chapter) suggestive of heart failure. The algorithm below is a reasonable, stepwise approach towards making the diagnosis of new-onset heart failure.

The initial evaluation should begin with obtaining basic laboratory values, that includes complete blood count, comprehensive metabolic profile, thyroid function tests, fasting lipid profile, troponin level, and in some instances, a B-type natriuretic peptide level. A BNP or NT-proBNP level can be helpful in making the diagnosis of heart failure, however, keeping in mind multiple variables (i.e. age, gender, BMI, renal function, medical therapy) can influence and confound the interpretation. Regardless, BNP or NT-proBNP levels are useful in ruling out heart failure as it has a negative predictive value of up to 90% when the level is <300 pg/mL.
An electrocardiogram and chest x-ray should also be attained to evaluate for ischemia, infarct, or arrhythmias, as well as for pulmonary edema, cardiomegaly, or other factors that could be causing dyspnea. Afterwards, if necessary, a transthoracic echocardiogram can be considered to assess LV systolic and diastolic function, chamber enlargement, wall thickness, valvular abnormalities, or pericardial effusion/tamponade. From this point, focus can then be directed towards determining the etiology of the heart failure to look for reversible causes.
Special Topics in Heart Failure
Advanced treatment with mechanical assist devices and/or cardiac transplantation can be considered in patients with end-stage heart failure. We will briefly focus on left ventricular assist devices (LVADs) and cardiac transplantation.
Left Ventricular Assist Devices (LVADs)
LVADs are circulatory support devices that extract oxygenated blood from either the left atrium or left ventricle and directs flow of the blood through a pulsatile or continuous-flow generator that then directs flow of blood out of the aorta. LVADs can be short-term or used as long-term devices as bridge to transplant, bridge to recovery, or destination therapy. For LVADs being used for destination therapy, the REMATCH trial showed a 48% relative risk reduction of mortality in patients with end-stage heart failure not eligible for cardiac transplant that received LVAD (pulsatile HeartMate XVE) compared to the group treated medically. When LVADs are used as a bridge to transplant, 70–80% of patients with an LVAD are successfully bridged to transplantation, compared to only 36% of patients on inotropic therapy. Currently, based on results from the HeartMate II trial, the smaller and more efficient, continuous-flow LVADs are being used more commonly than the pulsatile devices as they were shown to have a 2-year survival of 58% compared to 24% in the pulsatile flow group.
Cardiac Transplantation
Heart transplantation remains the gold standard for treatment of end-stage heart failure; however, the number of available organs is limited. Survival rates after heart transplantation are 85% at 1 year, 70% at 5 years, and 50% at 10 years, respectively. Malignancy and coronary artery vasculopathy are some of the complications associated with transplant that limit survival.
The United Network for Organ Sharing (UNOS), a national, nonprofit organization, along with local organ procurement organizations (OPO), allocate organs for transplantation in the United States, maintain organ transplantation waiting lists, and evaluate potential organ donors. Screening and evaluation for transplant consideration is extensive. Some absolute contraindications to transplant are irreversible pulmonary hypertension and systemic illness that will limit survival. Once a patient is accepted as a potential candidate for cardiac transplantation by a UNOS-certified transplant program, the potential recipient is given a status level on the UNOS list based on specified criteria. Status 1A is given the highest priority.
Suggested Reading
Abraham WT, Adams KF, Fonarow GC, et al. In-hospital mortality in patients with acute decompensated heart failure requiring intravenous vasoactive medications: an analysis from the Acute Decompensated Heart Failure National Registry (ADHERE). J Am Coll Cardiol. 2005;46:57–64.
Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–37.
Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350(21):2140–50.
CIBIS-II Investigators. The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomized trial. Lancet. 1999;353:9–13.
Cleland JGF, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539–49.
Cohn JN, Archibald DG, Ziesche S, et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure. Results of a veterans administration cooperative study. N Engl J Med. 1986;314(24):1547–52.
Cohn JN, Tognoni G. Valsartan heart failure trial investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–75.
CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl J Med. 1987;316(23):1429–35.
Crow S, John R, Boyle A, et al. Gastrointestinal bleeding rates in recipients of nonpulsatile and pulsatile left ventricular assist devices. J Thorac Cardiovasc Surg. 2009;137:208–15.
Cuculich PS, Kates AM, editors. Cardiology subspecialty consult, vol. 2. Philadelphia: Wolters Kluwer/Lippincott Williams and Wilkins; 2009. p. 19–23, 112–161.
Cuff MS, Califf RM, Adams KF, et al. Short-term intravenous milrinone for acute exacerbation of chronic heart failure. JAMA. 2002;287(12):1541–7.
Dargie HJ et al. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomized trial. Lancet. 2001;357:1385–90.
Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336(8):525–33.
Felker GM, Benza RL, Chandler AB, et al. Heart failure etiology and response to milrinone in decompensated heart failure: results from the OPTIME-CHF study. J Am Coll Cardiol. 2003;41:997–1003.
Goldhaber JI, Hamilton MA. Role of inotropic agents in the treatment of heart failure. Circulation. 2010;121:1655–60.
Granger CB, McMurray JJ, Yusuf S, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM-Alternative trial. Lancet. 2003;362:772–6.
Griffin BP, Topol EJ, editors. Manual of cardiovascular medicine. 3rd ed. Philadelphia: Wolters Kluwer/Lippincott Williams and Wilkins; 2009. p. 105–90.
He J, Ogden LG, Bazzano LA, et al. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001;161(7):996–1002.
Ho KK, Anderson KM, Kannel WB, et al. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993;88(1):107–15.
Hohnloser S, Kuck KH, Dorian P, et al. Prophylactic use of an implantable cardioverter-defibrillator after acute myocardial infarction. N Engl J Med. 2004;351:2481–8.
Hunt S, Abraham WT, Chin MH, et al. ACC/AHA 2005 Guideline Update for the diagnosis and management of chronic heart failure in the adult: a Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2005;112:154–235.
Januzzi Jr JL, Camargo CA, Anwaruddin S, et al. The N-terminal pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am J Cardiol. 2005;95(8):948–54.
Levy WC, Mozaffarian D, Linker DT, et al. The seattle heart failure model: prediction of survival in heart failure. Circulation. 2006;113:1424–33.
Libby P, Bonow RO, editors. Braunwald’s heart disease: a textbook of cardiovascular medicine. 8th ed. Philadelphia: WB Saunders; 2008. p. 509–727.
Lindenfeld J, Mann DL, et al. Executive summary: HFSA 2010 comprehensive heart failure practice guideline. J Card Fail. 2010;16(6):475–539.
McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285(26):1441–5.
McMurray JJ, Ostergren J, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-Added Trial. Lancet. 2003;362:767–71.
MERIT-HF Study Group. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999;353:2001–7.
Moss AJ, Hall WJ, Cannom DS, et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009;361(14):1329–38.
Moss AJ, Hall WJ, Cannom DS, For the Multicenter Automatic Defibrillator Implantation Trial Investigators. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. N Engl J Med. 1996;335(26):1933–40.
Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346(12):877–83.
Nohria A, Mielniczuk LD, Stevenson LW. Evaluation and monitoring of patients with acute heart failure syndromes. Am J Cardiol. 2005;96(6):32–40.
Packer M, Coats AJ, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344:1651–8.
Pfeffer MA, Braunwald E, Moye LA, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 1992;327(10):669–77.
Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348(14):1309–21.
Pitt B, Zannad F, Remme WJ. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341(10):709–17.
Rose EA, Gelijns AC, et al. Long-term mechanical left ventricular assistance for end-stage heart failure. N Engl J Med. 2001;345(20):1435–43.
Ryden L, Armstrong PW, Cleland JGF, et al. Efficacy and safety of high-dose lisinopril in chronic heart failure patients at high cardiovascular risk, including those with diabetes mellitus. Eur Heart J. 2000;21(23):1967–78.
Slaughter MS. Hematologic effects of continuous flow left ventricular assist devices. J Cardiovasc Transl Res. 2010;3(6):618–24. Epub 2010 Sep 11.
Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009;361:1–11.
SOLVD Investigators. Effect if enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325(5):293–302.
Steinhart B, Thorpe KE, Ahmed BM, et al. Improving the diagnosis of acute heart failure using a validated prediction model. J Am Coll Cardiol. 2009;54(16):1515–21.
Taylor AL, Ziesche S, Yancy C, et al. African-American heart failure trial investigators. Combination of isosorbide dinitrate and hydralazine in blacks with heart failure. N Engl J Med. 2004;351(20):2049–57.
Young JB, Abraham WT, Stevenson LW, For the VMAC Study Group. Results of the VMAC trial: vasodilation in the management of acute congestive heart failure. Circulation. 2000;102:2794.
Yusuf S, Pfeffer MA, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003;362:777–81.
Zannad F, McMuray JV, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364:11–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag London Limited
About this chapter
Cite this chapter
Lien, S.F., Alexis, J.D. (2012). Congestive Heart Failure. In: Bisognano, J., Beck, R., Connell, R. (eds) Manual of Outpatient Cardiology. Springer, London. https://doi.org/10.1007/978-0-85729-944-4_11
Download citation
DOI: https://doi.org/10.1007/978-0-85729-944-4_11
Published:
Publisher Name: Springer, London
Print ISBN: 978-0-85729-943-7
Online ISBN: 978-0-85729-944-4
eBook Packages: MedicineMedicine (R0)