Abstract
Clinical data available on coinfections are contradictory concerning both the number of viruses involved and the severity of the condition. A total of 114 patients aged 0–59 months with symptoms of respiratory tract infection were enrolled into the study. Nasal and pharyngeal swabs were tested using the PCR method for the following 12 viruses: influenza A, influenza B, respiratory syncytial virus A (RSV A), respiratory syncytial virus B (RSV B), adenovirus, metapneumovirus, coronavirus 229E/NL63 (hCoV229), coronavirus OC43 (hCoVOC43), parainfluenza virus 1 (PIV-1), parainfluenza virus 2 (PIV-2), parainfluenza virus 3 (PIV-3), and rhinovirus A/B. Coinfections were detected in nine (8 %) patients. Five of the coinfections were related to influenza A (H3N2) virus associated with the following other, single or combined, respiratory viruses: influenza B in one case, hCoV229 in two cases, hCoV229, RSV A, and PIV-2 in one case, and PIV-1, PIV-2, RSV A, RSV B, and adenovirus in one case. The other four coinfections were caused by: adenovirus and hCoVOC43, adenovirus, and rhinovirus, RSV A and PIV-1, influenza B, and RSV B. We did not observe any significant differences in the clinical course of infections caused either by a single or multiple viral factors.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Respiratory viral infections are a major source of morbidity and mortality in childhood. Children with respiratory infections are generally treated as outpatients and the etiology of their disease is usually not investigated. In case of hospitalization, the diagnostic techniques employed are often not sensitive enough (Jin et al. 2007). It is estimated that 50–85 % of pediatric acute respiratory tract infections are of viral origin. Experience and understanding of the role of viral coinfections in respiratory tract infections have grown in recent years due to the introduction of molecular techniques (Brunstein et al. 2008; Mahony et al. 2007). At present, clinical data available on confection are variable, sometimes contradictory, in terms of both the number of viruses involved and the severity of the condition. These discrepancies may be due to such factors as geographical region and detection methods (Kumar 2009). The detection of respiratory viruses in children using molecular methods can be challenging. The reason for this is that virus-virus coinfections and mixed viral-bacterial infections occur in 15–30 % of cases and viruses can be detected in 25–45 % of children in the absence of respiratory symptoms (Frobert et al. 2011; Peng et al. 2009; Raymond et al. 2009). Although, the effects of viral coinfections have been described and analyzed in the literature, the number of such studies is limited, especially in Central Eastern Europe, including Poland. The aim of this study was to analyze the incidence and clinical course of respiratory tract infections caused by more than one viral etiological factor among children aged 0–59 months.
2 Material and Methods
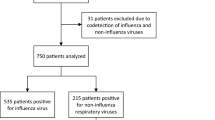
Ethical approval was obtained from the Medical University of Warsaw, Poland. Data and specimens were obtained from patients aged 0–59 months with respiratory tract infection symptoms: fever > 38°C, sore throat or cough lasting less than 96 h. The exclusion criteria were the following: symptoms lasting longer than 96 h, age > 59 months, ongoing antibiotic therapy, and the child’s guardian refusal to take swabs. A total of 114 patients were enrolled into the study: 52 children hospitalized in the General Pediatric Ward and 62 children requiring ambulatory care; all with acute respiratory tract infections. Guardians of all the children enrolled were provided with written information regarding the study’s aims and methods, and written consent was obtained from all the guardians. Two swabs were taken from the patients: one nasal and one pharyngeal. Viscose swabs were used to collect specimens that were stored for less than 24 h at a temperature of 2–8 °C and then transported to the National Influenza Center at the National Institute of Public Health – National Institute of Hygiene in Warsaw, Poland, where specimens from patients, stored at -80 °C, were tested by RT-PCR using a RV12 ACE Detection Kit (Seegene, Seoul, South Korea) for the detection of the following respiratory viruses: influenza A virus, influenza B virus, human respiratory syncytial virus A (RSV A), human respiratory syncytial virus B (RSV B), human adenovirus, human metapneumovirus, human coronavirus 229E/NL63 (hCoV229), human coronavirus OC43 (hCoVOC43), human parainfluenza virus 1 (PIV-1), human parainfluenza virus 2 (PIV-2), human parainfluenza virus 3 (PIV-3), and human rhinovirus A/B. A random hexamer primer for cDNA synthesis was used with the First Strand cDNA Synthesis Kit (Fermentas, York, UK). Each cDNA preparation was subject to the RV12 PCR procedure according to the manufacturer’s instructions (Seegene, Seoul, South Korea). Afterwards, amplicons were detected using gel electrophoresis. The subtyping of influenza viruses was carried out using conventional multiplex RT-PCR (Influenza A/B OneStep Typing Set; Seegene, Seoul, South Korea). A panel of Seeplex RT-PCR assays was used to detect influenza A, influenza B, and the three subtypes of influenza A (H1, H3, and H1N1 2009).
A descriptive analysis of patients with coinfections was carried out, including age, gender and symptoms. A comparison of symptoms of infections caused by a single viral agent and those caused by more than one agent was performed. The statistical analysis was conducted with a medical statistical calculator available at www.medcalc3000.com
3 Results
Nine patients (8 %) were infected by more than one viral agent; 64 (56 %) patients were infected by a single virus; 41 (36 %) samples were negative. Single etiological agents were as follows: influenza A (29 cases, 25 %), RSV B (18 cases, 16 %), RSV A (5 cases, 4 %), adenovirus (4 cases, 4 %), HCoVOC43 (3 cases, 3 %), hCoV229 (2 cases, 2 %), PIV-1 (1 case, 1 %) and PIV-2 (1 case, 1 %). Five cases caused by influenza A (H3N2) virus were associated with coinfections with other respiratory viruses, such as influenza B (1 case), hCoV229 (2 cases), hCoV229, RSV A, and PIV-2 combined (1 case), and PIV-1, PIV-2, RSV A, RSV B, and adenovirus combined (1 case). Figure 1 presents an image of PCR test results for a multiple coinfection with six respiratory viruses.
The remaining four were double infections caused by adenovirus and hCoVOC43, adenovirus and rhinovirus, RSV A and PIV-1, and influenza B and RSV B. The demographical and clinical characteristics of patients with coinfections are presented in Table 1. The incidence of viral coinfections was similar among hospitalized and non-hospitalized children with symptoms of respiratory tract infection (7.6 % vs. 8 %, respectively). Symptoms and clinical course of the disease caused by either single or multiple agents were similar; no significant differences were observed (Table 2).
4 Discussion
In the present study, the prevalence of viral coinfections among young children with acute respiratory tract infection was on the low side of 8 %. In the literature, coinfection rates appreciably vary depending on the study. Peng et al. (2009) found multiple etiological agents in 36 % of hospitalized children; coinfections occurred predominantly among children aged 3–6 years and the most common pathogens were influenza A, influenza B, and PIV-1. Renois et al. (2010) detected 17 % of multiple infections among patients with acute respiratory tract infections; they were combinations of influenza A/H1N1v virus with CoV, human bocavirus (HBoV), RSV or human rhinoviruses (HRVs). Bonzel et al. (2008) diagnosed viral coinfections in 16 % of samples, with RSV and hBoV being the most common combination. In that study, viral coinfection was found in 17 % of children with bronchitis and in 23 % of those with bronchiolitis, while in patients with pneumonia 33 % were positive for 2 or more viral pathogens. In the present study, the majority of coinfections were associated with influenza A infection and all of them occurred in children younger than 24 months.
We failed to not observe any significant differences in the clinical course of infections caused by either a single or multiple viral factors. Our data are in agreement with other studies that have reported no clinical differences between patients with respiratory infections caused by a single or multiple agents detected in nasopharyngeal aspirates from children (Martin et al. 2012; Nascimiento et al. 2010). Camargo et al. (2012) found coinfections with influenza A H1N1 in 22 % of patients with no greater morbidity or mortality. Suryadevara et al. (2011) diagnosed 28 % of multipathogen viral infections among febrile children younger than 24 months with acute respiratory infections. The most common viruses detected were RSV and rhinovirus/enterovirus. There were no differences in the severity of disease when comparing patients infected with one or multiple pathogens. However, there are some studies that show that coinfection may be a risk factor for poor evolution. Aberle et al. (2005) reported that airway obstruction was more severe when RSV contributed to coinfection and the hospital stay was lengthened when rhinovirus was involved. In another study, Greensill et al. 2003 showed that when coinfection consisted of RSV and metapneumovirus, evolution was worse. Further, Richard et al. (2008), who studied the relationship of coinfection with the need for admission to the pediatric intensive care unit (PICU), concluded that the presence of two or more viruses increased the likelihood of admission. However, in another study conducted among patients admitted to the PICU, Ghani et al. (2012) found that bacterial coinfection was only associated with a longer hospital stay, with no increase in mortality. Calvo et al. (2008) reported multiple viral infections in hospitalized infants with respiratory tract disease in about 17 % cases and these coinfections were linked to higher fever, longer hospital stays, and a more frequent use of antibiotics compared with the cases of single RSV infections. It is worth noting that the detection of more than one virus may be due to the presence of viral fragments persisting for up to 5–6 weeks after the onset of symptoms, which may actually be irrelevant for the current clinical course. Further studies are required to confirm or exclude associations between co-detected respiratory viruses and to demonstrate the underlying mechanisms of such associations which may lead to cooperation or competition between viruses. Another important issue that remains unclear is the long-term effect that such coinfections may have on the development of chronic lung disease.
A limitation of the present study was a relatively small number of cases evaluated compared with the usually high numbers seen in pediatric practice. Another limitation was the lack of inclusion of bacterial coinfections. Predisposing factors for synchronous coinfection were not detected in our study, although there are some other data pointing to such a possibility. For instance, a high rate of codetection of HBoV with HAdV was reported and a prolonged shedding of the HBoV may potentially contribute to this phenomenon (Jartii et al. 2011). On the other hand, an advantage of the present study was that we described viral coinfections among young immunocompetent children, while other authors often report multiple infections among immunosupressed patients (Stefanska et al. 2013).
To conclude, viral respiratory coinfections do occur in young immunocompetent young children, but such infections do not seem to play an important role in the clinical presentation of acute respiratory infections in this age group. Studies involving larger numbers of patients and using improved quantitative detection techniques are needed to define the exact role of viral coinfections in the course of respiratory disease.
References
Aberle JH, Aberle SW, Pracher E, Hutter HP, Kundi M, Popow-Kraupp T (2005) Single versus dual respiratory virus infections in hospitalized infants: impact on clinical course of disease and interferon-gamma response. Pediatr Infect Dis J 24:605–610
Bonzel L, Tenenbaum T, Schroten H, Schildgen O, Schweitzer-Krantz S, Adams O (2008) Frequent detection of viral coinfection in children hospitalized with acute respiratory tract infection using a real-time polymerase chain reaction. Pediatr Infect Dis J 27:589–594
Brunstein JD, Cline CL, McKinney S, Thomas E (2008) Evidence from multiplex molecular assays for complex multipathogen interactions in acute respiratory infections. J Clin Microbiol 46:97–102
Calvo C, García-García ML, Blanco C, Vázquez MC, Frías ME, Pérez-Breña P (2008) Multiple simultaneous viral infections in infants with acute respiratory tract infections in Spain. J Clin Virol 42:268–272
Camargo C, Guatura SB, Bellei N (2012) Respiratory viral coinfection among hospitalized patients with H1N1 2009 during the first pandemic wave in Brazil. Braz J Infect Dis 16:180–183
Frobert E, Escuret V, Javouhey E, Casalegno JS, Bouscambert-Duchamp M, Moulinier C (2011) Respiratory viruses in children admitted to hospital intensive care units: evaluating the CLARTR pneumovir DNA array. J Med Virol 83:150–155
Ghani AS, Morrow BM, Hardie DR, Argent AC (2012) An investigation into the prevalence and outcome of patients admitted to a pediatric intensive care unit with viral respiratory tract infections in Cape Town, South Africa. Pediatr Crit Care Med 13:e275–e281
Greensill J, McNamara PS, Dove W, Flanagan B, Smyth RL, Hart CA (2003) Human metapneumovirus in severe respiratory syncytial virus bronchiolitis. Emerg Infect Dis 9:372–375
Jartii T, Hedman K, Jartii L, Ruuskanen O, Allander T, Soderlund-Venermo M (2011) Human bocavirus- the first 5 years. Rev Med Virol 22:46–64
Jin YS, Kuak EY, Shin BM (2007) Detection of 12 respiratory viruses with two-set multiplex reverse transcriptase-PCR assay using a dual priming oligonucleotide system. Korean J Lab Med 27:420–427
Kumar RM (2009) The widely used diagnostics DNA microarrays – a review. Am J Infect Dis 5:207–218
Mahony J, Chong S, Merante F, Yaghoubian S, Shina T, Lisle C (2007) Development of respiratory virus panel test for the detection of twenty human respiratory viruses by using multiplex PCR and a fluid microbead-based assay. J Clin Microbiol 45:3056–3062
Martin ET, Kuypers J, Wald A, Englund JA (2012) Multiple versus single virus respiratory infections: viral load and clinical disease severity in hospitalized children. Influenza Other Respir Viruses 6:71–77
Nascimiento MS, Souza AV, Ferreira AV, Rodrigues JC, Abramovici S, Silva Filho LV (2010) High rate of viral identification and coinfections in infants with acute bronchiolitis. Clinics (Sao Paulo) 65:1133–1137
Peng D, Zhao D, Liu J, Wang X, Yang K, Xicheng H (2009) Multipathogen infections in hospitalized children with acute respiratory infections. Virol J 6:155. doi:10.1186/1743-422X-6-155
Raymond F, Carbonneau J, Boucher N, Robitaille L, Boisvert S, Wu WK (2009) Comparison of automated microarray detection with real-time PCR assays for detection of respiratory viruses in specimens obtained from children. J Clin Microbiol 47:743–750
Renois F, Talmud D, Huguenin A, Moutte L, Strady C, Cousson J (2010) Rapid detection of respiratory tract viral infections and coinfections in patients with influenza-like illnesses by use of reverse transcription-PCR DNA microarray systems. J Clin Microbiol 48:3836–3842
Richard N, Komurian-Pradel F, Javouhey E, Perret M, Rajoharison A, Bagnaud A (2008) The impact of dual viral infection in infants admitted to a pediatric intensive care unit associated with severe bronchiolitis. Pediatr Infect Dis J 27:213–217
Stefanska I, Romanowska M, Donevski S, Gawryluk D, Brydak B (2013) Coinfections with influenza and other respiratory viruses. Adv Exp Med Biol 756:291–301
Suryadevara M, Cummings E, Bonville CA, Bartholoma N, Riddell S, Kiska D (2011) Viral etiology of acute febrile respiratory illnesses in hospitalized children younger than 24 months. Clin Pediatr (Phila) 50:513–517
Conflicts of Interests
The authors declare no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Nitsch-Osuch, A., Kuchar, E., Topczewska-Cabanek, A., Wardyn, K., Życińska, K., Brydak, L. (2015). Incidence and Clinical Course of Respiratory Viral Coinfections in Children Aged 0–59 Months. In: Pokorski, M. (eds) Respiratory Contagion. Advances in Experimental Medicine and Biology(), vol 905. Springer, Cham. https://doi.org/10.1007/5584_2015_185
Download citation
DOI: https://doi.org/10.1007/5584_2015_185
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-30603-2
Online ISBN: 978-3-319-30604-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)