Abstract
Given the prevalence of myopia has been increasing significantly across the world, especially in East Asia, great challenges have been raised for myopia correction and the management of pathological myopia. Delaying the onset of myopia will likely reduce the prevalence of myopia as well as high myopia in school-aged children. Prevention of the onset of myopia is therefore an important priority. This chapter focuses on the clinical strategy to prevent or delay the onset of myopia among school-aged children, summarizing the interventions currently available, including increased time outdoors, reduced near work, latest optical interventions, eye exercises of acupoints, and takes a glance at future perspectives.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Time spent outdoors is well recognized as a factor preventing the development of myopia onset, and measures including adding an outdoor class, locking classroom doors during class recess, or glassed roof and walls incorporated in a classroom have been developed. But promotion to increase time spent outdoors as a school-based intervention program remains challenging especially in East Asia.
-
Near work activity has been suggested as a risk factor for myopia although the evidence is not entirely consistent. The total duration of near work activity may not be as important as the type of near work activity. Core techniques to implementing interventions of near work activities include effective measures of near work-related parameters, real-time data analyses, and alert systems.
-
School children growing up in myopigenic environments are likely to benefit from optical interventions designed to induce myopic defocus. The lens with multiple segments of defocus showed promising effect on slowing progression of myopia.
-
The Chinese eye exercises of acupoints advocated in mainland China and Taiwan were designed to relieve ocular fatigue and reduce the development and progression of myopia. But clinical significance of its efficacy has not been established according to available data.
-
Maximizing the utility of time outdoors is still the priority in the prevention of myopia onset. The role of screen time in myopia development is still ambiguous, the restriction may enable more time for children to go outdoors. Other approaches to prevent myopia onset still require further investigations, such as imposed myopic defocus, low-dose atropine, or some novel pharmacological agents for non-myopes.
7.1 Introduction
Over recent decades, the prevalence of myopia in school-aged children has been increasing significantly in East Asia. Up to 80% of junior high school students have myopia, of which 20% have high myopia in mainland China [1, 2], Hong Kong [3], Taiwan [4], South Korea [5], Japan [6], and Singapore [7]. Longitudinal data suggests that the incidence of myopia is around 10–20% per year among school-aged children [8,9,10,11]. If the onset of myopia can be delayed, the prevalence of myopia as well as high myopia in school-aged children will likely reduce. This chapter focuses on the clinical strategy to prevent or delay the onset of myopia among school-aged children, summarizing the interventions currently available, and takes a glance at future perspectives.
7.2 Onset of Myopia
The vast majority of literature suggests that most cases of myopia develop during the school-going age in children. The prevalence of myopia among preschool children is relatively low [12,13,14,15]; furthermore, a longitudinal study in Shunyi Beijing demonstrates that the annual incidence of myopia among 5-year-old children is below 5% [16]. After the age of 6 years, the prevalence of myopia starts to rise [6, 16,17,18,19]. The highest annual incidence of myopia is reported among school children from urban mainland China [18] and Taiwan [20], ranging from 20% to 30% through ages 7–14 years with earlier onset of myopia also being identified [6]. A study in Japan showed that while the prevalence of myopia has been increasing from 1984 to 1996, the prevalence among children aged 6 or younger has remained unchanged. This suggests that the majority of increased myopia onset is secondary to increased educational intensity and develops when children reach school age (Fig. 7.1) [6].
Age-specific prevalence of myopia in Japan in 1984 and 1996. © Matsumura et al. [6]
A long-term longitudinal study has demonstrated that there is a steady shift in refraction toward myopia, before the actual onset of myopia. Rates of progression increase dramatically the year of onset and this has been suggested by spherical equivalent refraction and axial length (Fig. 7.2) [21]. After the first detection of myopia, this acceleration is reduced (Fig. 7.2) [21, 22]. Myopic refractions tend to stabilize in late adolescent but can remain progressive until adulthood. The mean age at myopia stabilization is 15.6 years but this can vary among children of different ethnicities [23].
Changes in spherical equivalent refractions (a) and axial lengths (b) before and after myopia onset. © Xiang et al. [21]
Several factors have been found to be associated with the development of incident myopia in school. Asian ethnicity [19, 24], parental history of myopia [25, 26], reduced time outdoors [26], and level of near work activity [27, 28] are risk factors for incident myopia, although the evidence can be seen as controversial in some instances. Some studies have also suggested that non-myopic children with less hyperopic refractions and greater axial length/corneal radius of curvature ratios are more predisposed to develop myopia [18, 19]. The impact of gender to the development of myopia varies among populations. In Chinese school children, females have a greater chance of progressing to myopia [18]; while in multiethnic populations, gender seems to be less impactful [19, 24, 27].
Attempts have been made to establish tools to identify children at risk of developing myopia or high myopia. Among numerous associated factors, spherical equivalent refraction is the most promising predictor. By using a single measurement of refraction alone, future myopia onset of non-myopic children can be accurately predicted [29]. Moreover, children at risk of developing high myopia in adulthood can also be identified, with reasonably good sensitivity and specificity, when using an age-specific 5th percentile curve of refraction of the population (Fig. 7.3) as a cutoff [30]. Other promising tools for the prediction of future high myopia include the age of myopia onset [31] and age-specific annual refraction progression of children with myopia (Fig. 7.4) [32]. Information on age of myopia onset alone can predict high myopia with 85% accuracy using a receiver operating curve (ROC) [31].
Percentile curves of refractions for urban Chinese boys (a) and girls (b). © Chen et al. [30]
Age-specific annual progression of refraction in children with myopia. © Sankaridurg et al. [32]
7.3 Increased Time Outdoors as an Intervention
Time spent outdoors is well recognized as a factor preventing the development of myopia onset. Evidence of this was first presented in a three-year follow-up study of myopia in school children, showing that those who spent more time outdoors were less likely to progress [33]. Consistent results were reported in various studies, such as the Sydney Myopia Study, Orinda study as well as the Singapore Cohort Study of Risk Factors for Myopia [34,35,36]. This led to the commencement of several clinical trials, which confirmed the protective effect against myopia and indicated a dose-dependent effect, among them is the randomized clinical trial in Guangzhou which reported that an additional 40 min of outdoor activity can reduce the incidence of myopia by 23%. Additionally, the trial in Taiwan suggested that an extra 80 min may further reduce incidence by 50% [10, 37].
The mechanism of increased outdoor time as an intervention is not completely clear. Spending time outdoors itself, instead of physical activities outdoors, has been suggested to be the major protective factor [38]. Results from animal experiments indicated that protection due to bright light may be mediated by dopamine [39]. Some believe that ultraviolet light also plays an important role [40], with evidence suggesting that there is an association between vitamin D level and myopia [41,42,43], but data from a population-based cohort did not support this idea [44]. Alternatively, patterns of defocus on the retina by three-dimensional structures of the environment have also been proposed as a possible mechanism of protection from outdoor activities [45].
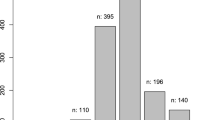
As an economically feasible intervention, getting children outside the classroom has been promoted in many public health programs such as Taiwan’s “Daily 120.” However, promotion to increase time spent outdoors as a school-based intervention program remains challenging. First, what is an effective amount of time outdoors? Population-based data suggest that 2–3 h a day would be beneficial [26, 35], however, this is difficult to achieve in some East Asian countries where the education system is very intensive. Some programs recommend adding an outdoor class into the curriculum, while others recommend prohibiting being inside during recess by locking classroom doors. Another group of researchers proposed a classroom design that incorporates a glassed roof and walls that enable maximize light intensity while students study indoors (Fig. 7.5) [46]. The protective effect of this bright classroom is now under investigation. Second, what is the appropriate location for outdoor activities? The ideal location appears to be in an area with bright light more than 10,000 lux, suggested by evidence from animal experiments [47, 48]. But the most recent results from Wu et al.’s study indicated that less bright light exposure, 1000-lux or 3000-lux for instance, is sufficient enough to generate a protective effect (Fig. 7.6) [49]. These findings seem to suggest that an environment such as the shade of a tree or building, the hallway, or playground could still work with an advantage to avoid sunburn or other side effects from UV exposure.
Classroom constructed with glass in China. ©Zhou et al. [46]
Light intensity of different locations in the school. ©Wu et al. [49]
Another concern is how do we measure outdoor activities? Traditionally, questionnaires have been commonly used to measure time outdoors but are less accurate due to recall bias. Objective measures can provide more precise real-time data. Wearable detectors have been developed to record light intensity and time outdoors, and even track the patterns of outdoor activities, including HOBO light meters, Nike+ Fuel Band, and others. Other measures have been used to estimate exposure to natural light such as conjunctival ultraviolet autofluorescence and skin photodamage, but these are more appropriate when measuring the cumulative light dosage or UV exposure [50, 51].
If increased time spent outdoors can prevent or delay the onset of myopia, it would ultimately reduce the prevalence of myopia or even high myopia among school-aged children. Documentation on the impact of time spent outdoors on the prevalence of myopia is of public health importance.
7.4 Reduced Near Work Intensity as an Intervention
Near work activity as a risk factor for myopia has been documented in some studies, although the evidence is not entirely consistent. A recent meta-analysis has reported a modest, but statistically significant, association between time spent performing near work and myopia (odds ratio, 1.14) [28].
It has been argued that the total duration of near work activity may not be as important as the type of near work activity. Studies have found that continuous reading of more than 30–45 min is associated with the presence of myopia and greater myopic refractive errors [52, 53]. Interestingly, after prolonged continuous reading, children are more likely to take up their preferred relaxed postures [54], such as close reading distance [53] and head tilt [52], both of which have been reported to be associated with the presence of myopia. Other factors that have been proposed to potentially contribute to the development of myopia include close nib-to-finger distance [52], downward angle of gaze [55, 56] and inadequate desk [52], or classroom lighting [56].
Efforts have been dedicated to developing novel devices to detect and correct inadequate near work behaviors. In mainland China, pens for myopia prevention has been invented. The pens are capable of detecting close reading distances (China Invention Patent, 200620010200.6) or nib-to-finger distances (China Invention Patent, 201020640746.6). Real-time retraction of the nib will occur when the eyes are too close to the reading materials or the nib-to-finger distance is inadequate, compelling children to adopt correct postures. The effect of the pens on preventing myopia onset is to be examined by future clinical trials.
Core techniques to implementing interventions of near work activities include effective measures of near work-related parameters, real-time data analyses, and alert systems. Wearable devices that possess these techniques have emerged in the last decade. A head-mounted instrument (Fig. 7.7) was built in Hong Kong for continuous logging of near work distance [57]. Measurements have proved to be accurate and repeatable over a range of distances and angles [57]. The Clouclip (Fig. 7.8) is another novel device developed in mainland China, primarily for the use of myopic children [58]. The device can measure reading distances and ambient illuminance, perform real-time data analyses, and feedback to children and parents (www.clouclip.com). This group of researchers used Clouclip to track reading distance and eye-level illuminance of children over a representative period of time [59]. Based on these data, they developed a summative index and found that a change in the index toward a more myopic behavior was significantly associated with increased myopic refractive errors in a preliminary longitudinal study [59]. The attempt to generate a simplified, summative index for risk estimation will help provide comprehensive information on near work-related behaviors and may help improve the efficacy of interventions.
Front view (a) and side view (b) of the near work analyzer for logging near work distance and its alignment in a straight-ahead position (c) and reading position (d). © Leung et al. [57]
Clouclip to monitor near work time. © Wen et al. [58]
7.5 Optical Interventions
The use of noninvasive optical interventions to prevent myopia is based on findings of the powerful STOP signals reported in numerous animal studies. By briefly exposing chickens to myopic defocus (the STOP signals), eye growth induced by presenting minus lenses can be slowed dramatically (Fig. 7.9) [60, 61]. It is therefore suggested that school children growing up in myopigenic environments are likely to benefit from routine optical interventions designed to induce myopic defocus [62]. The intervention regimen should combine variables including age, lens power, and duration of exposure to achieve an adequate effect on delaying the development of myopia [62].
Changes in refractions and ocular biometric parameters over 3 days of binocular negative lens wear interrupted by brief periods of positive lens wear on one eye and plano lens wear on the other eye. **P < 0.01; ***P < 0.001. © Zhu et al. [61]
While these optical interventions are an attractive idea, they have not been fully explored in human subjects—this will be elaborated further in Chap. 13 (Optical interventions for Prevention of Myopia Progression). A recent study has prescribed plus lenses to non-myopic children aged 5–8 years who are at risk of developing myopia [63]. The plus lenses imposed a 1.0 D myopic defocus and the children wore the correction the entire day. No cases of myopia onset have been observed in this group of children during the follow-up period (ranging from 3 to 9 years) [63]. The robustness of these study findings needs to be examined by future investigations.
The Defocus Incorporated Multiple Segments Lens (DIMS Lens) is a novel spectacle lens primarily designed for use in myopic children. The lens is composed of a central zone for optical correction of refractive error and an annular peripheral zone to induce myopic defocus. Interestingly, the lens peripheral zone contains numerous well-arranged small plus lenses, separated by small non-defocus areas. By using this design, myopic defocus is induced and visual quality is well reserved at the same time (presentation at the 16th International Myopia Conference [IMC]). In a pilot study conducted among school children, the DIMS lens slowed progression of myopia by 59% (presentation at the 16th IMC). The lens may also be promising for preventing myopia onset if adaptation can be successfully made for non-myopic children.
7.6 Eye Exercises of Acupoints
The eye exercises of acupoints are a set of bilateral acupoint self-massages designed to relieve ocular fatigue and reduce the development and progression of myopia. These eye exercises were introduced by the Chinese National Education Commission and have been advocated since the 1960s in mainland China and Taiwan. Children in primary and junior middle schools are required to perform the eye exercises twice a day. The 5-min exercises include: (1) knead Tianying (Ashi); (2) press and squeeze Jingming (BL1); (3) press and knead Sibai (ST2); and (4) press Taiyang (EX-HN5) and scrape Cuanzhu (BL2), Yuyao (EX-HN4), Sizhukong (TE23), Tongziliao (GB1), Chengqi (ST1) (Fig. 7.10).
Schematic diagram demonstrating the positions of acupoints used in Chinese eye exercises. © Lin et al. [67]
The efficacy of the Chinese eye exercises is believed to be from the theory of Traditional Chinese Medicine. By massaging the acupoints, Chi can be achieved and help relieve eye strain and recover ocular functions. Peak systolic velocity in the central retinal and ophthalmic arteries is observed after the eye exercises [64], which might provide some evidences to support this theory. Accommodative lag decreases significantly by 0.1 D after 5 min of performing the eye exercises [65].
Clinical significance has never been established in the published literature thus far. Cross-sectional studies have assessed the association between Chinese eye exercises and myopia with varied results [66,67,68,69]. The inconsistency can be explained by the different settings studied (rural vs. urban), failure to adjust for potential confounders (including parental myopia, time outdoors, and near work) and the lack of representative populations in some studies. In a recent study, the impact of Chinese eye exercises on the development of myopia has been examined using a longitudinal design [70]. No association between eye exercises and myopia onset has been found [70]. However, due to the limited sample size, low level of intervention time, and performance qualities of the exercises in the study, the actual impact is still not conclusive and needs to be justified by further studies.
7.7 Future Prospects
It has been estimated that without any effective controls or interventions the proportion of myopes in the population will reach up to 50% and 10% for high myopes by 2050 [71]. Approaches that have produced a reduction of at least 50% in incidence, such as time outdoors, have the potential to make a significant difference on the impending myopia epidemic. But the level of impact of the full utility of available interventions needs to be evaluated by further studies.
Another critical issue is how to implement both education intensity and outdoor time interventions in East Asia. There needs to be a balance between educational achievement and interventions delivered, which don’t exacerbate the prevalence of myopia in East Asia. This balance can be seen in Australia [72], with some of the highest educational ranks in the world (PISA, https://www.oecd.org/pisa/data/) but also high levels of outdoor activity and light intensity. Preventing the onset of myopia is certainly challenging in the East Asian population and requires a collaborative effort among clinics, schools, parents, and the entire society.
Nonetheless, maximizing the utility of time outdoors is still the priority in the prevention of myopia onset. The implementation of outdoor activities in school programs and daily life necessitates further propagation and feedback from parents and children. Novel devices combined with the internet and even social networks are a potential direction. An example is FitSight, which was developed by Saw et al. (Fig. 7.11) and comprises of a smartwatch with a light sensor and smartphone app that records time outdoors and sends feedback to parents and children [73]. This kind of devices needs to be proven to be useful by undertaking field study and determining wearability. Additionally, the price of the device should be considered in the design.
FitSight fitness tracker to record time outdoors. ©Verkicharla et al. [73]
Another behavior control method focuses on limiting the screen time on computers, tablets, and smart phones. Though the role of screen time in myopia development is still ambiguous, the restriction may enable more time for children to go outdoors. Applications to provide screen distance and time monitoring, alerts to rest eyes, blue light filters, and remote locking capability for parents are available in some countries (plano, https://www.plano.co/). The effect of this technology on myopia prevention remains to be seen.
Other approaches to prevent myopia onset still require further investigations, such as imposed myopic defocus, low-dose atropine, or some novel pharmacological agents for non-myopes. They may help to prevent myopia in those who are rapidly progressing or have high-risk genetic forms. Thus, a question is raised: how do we identify children that have an increased risk of becoming myopic or highly myopic? Risk estimation is therefore critical to achieve personalized treatment for individuals. For children who are non-myopic but at an increased risk of developing high myopia in the future, additional outdoor activities and aggressive approaches should be introduced with frequent follow-up visits. Tools of myopia prediction have been developed as mentioned before, and we expect to see the outcomes of the integration of risk prediction and clinical practice in the near future.
References
Wu LJ, et al. Prevalence and associated factors of myopia in high-school students in Beijing. PLoS One. 2015;10:e0120764. https://doi.org/10.1371/journal.pone.0120764.
Wu JF, et al. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS One. 2013;8:e82763. https://doi.org/10.1371/journal.pone.0082763.
Goh WS, Lam CS. Changes in refractive trends and optical components of Hong Kong Chinese aged 19-39 years. Ophthalmic Physiol Opt. 1994;14:378–82.
Lin LL, et al. Epidemiologic study of the prevalence and severity of myopia among schoolchildren in Taiwan in 2000. J Formos Med Assoc. 2001;100:684–91.
Jung SK, Lee JH, Kakizaki H, Jee D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in Seoul, South Korea. Invest Ophthalmol Vis Sci. 2012;53:5579–83. https://doi.org/10.1167/iovs.12-10106.
Matsumura H, Hirai H. Prevalence of myopia and refractive changes in students from 3 to 17 years of age. Surv Ophthalmol. 1999;44(Suppl 1):S109–15.
Wu HM, et al. Does education explain ethnic differences in myopia prevalence? A population-based study of young adult males in Singapore. Optom Vis Sci. 2001;78:234–9.
Shah RL, Huang Y, Guggenheim JA, Williams C. Time outdoors at specific ages during early childhood and the risk of incident myopia. Invest Ophthalmol Vis Sci. 2017;58:1158–66. https://doi.org/10.1167/iovs.16-20894.
Ku P.-W. et al. The associations between near visual activity and incident myopia in children. Ophthalmology. https://doi.org/10.1016/j.ophtha.2018.05.010.
He M, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314:1142–8. https://doi.org/10.1001/jama.2015.10803.
Lin LL, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singap. 2004;33:27–33.
Guo X, et al. Significant axial elongation with minimal change in refraction in 3- to 6-year-old Chinese preschoolers: The Shenzhen Kindergarten Eye Study. Ophthalmology. 2017;124:1826–38. https://doi.org/10.1016/j.ophtha.2017.05.030.
Giordano L, et al. Prevalence of refractive error among preschool children in an urban population: the Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116:739–46. https://doi.org/10.1016/j.ophtha.2008.12.030.
Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence of myopia and hyperopia in 6- to 72-month-old african american and Hispanic children: the multi-ethnic pediatric eye disease study. Ophthalmology. 2010;117:140–147.e143. https://doi.org/10.1016/j.ophtha.2009.06.009.
Dirani M, et al. Prevalence of refractive error in Singaporean Chinese children: the strabismus, amblyopia, and refractive error in young Singaporean Children (STARS) study. Invest Ophthalmol Vis Sci. 2010;51:1348–55. https://doi.org/10.1167/iovs.09-3587.
Zhao J, et al. The progression of refractive error in school-age children: Shunyi district, China. Am J Ophthalmol. 2002;134:735–43.
Xiang F, et al. Increases in the prevalence of reduced visual acuity and myopia in Chinese children in Guangzhou over the past 20 years. Eye. 2013;27:1353–8. https://doi.org/10.1038/eye.2013.194.
Wang SK, et al. Incidence of and factors associated with myopia and high myopia in Chinese children, based on refraction without cycloplegia. JAMA Ophthalmol. 2018;136:1017–24. https://doi.org/10.1001/jamaophthalmol.2018.2658.
Saw SM, et al. Incidence and progression of myopia in Singaporean school children. Invest Ophthalmol Vis Sci. 2005;46:51–7. https://doi.org/10.1167/iovs.04-0565.
Tsai DC, et al. Myopia development among young schoolchildren: The Myopia Investigation Study in Taipei. Invest Ophthalmol Vis Sci. 2016;57:6852–60. https://doi.org/10.1167/iovs.16-20288.
Xiang F, He M, Morgan IG. Annual changes in refractive errors and ocular components before and after the onset of myopia in Chinese children. Ophthalmology. 2012;119:1478–84. https://doi.org/10.1016/j.ophtha.2012.01.017.
Mutti DO, et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48:2510–9. https://doi.org/10.1167/iovs.06-0562.
COMET Group. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013;54:7871–84. https://doi.org/10.1167/iovs.13-12403.
French AN, Morgan IG, Burlutsky G, Mitchell P, Rose KA. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology. 2013;120:1482–91. https://doi.org/10.1016/j.ophtha.2012.12.018.
Jones-Jordan LA, et al. Early childhood refractive error and parental history of myopia as predictors of myopia. Invest Ophthalmol Vis Sci. 2010;51:115–21. https://doi.org/10.1167/iovs.08-3210.
Jones LA, et al. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48:3524–32. https://doi.org/10.1167/iovs.06-1118.
Williams C, Miller LL, Gazzard G, Saw SM. A comparison of measures of reading and intelligence as risk factors for the development of myopia in a UK cohort of children. Br J Ophthalmol. 2008;92:1117–21. https://doi.org/10.1136/bjo.2007.128256.
Huang HM, Chang DS, Wu PC. The association between near work activities and myopia in children-a systematic review and meta-analysis. PLoS One. 2015;10:e0140419. https://doi.org/10.1371/journal.pone.0140419.
Zadnik K, et al. Prediction of juvenile-onset myopia. JAMA Ophthalmol. 2015;133:683–9. https://doi.org/10.1001/jamaophthalmol.2015.0471.
Chen Y, Zhang J, Morgan IG, He M. Identifying children at risk of high myopia using population centile curves of refraction. PLoS One. 2016;11:e0167642. https://doi.org/10.1371/journal.pone.0167642.
Chua SY, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016;36:388–94. https://doi.org/10.1111/opo.12305.
Sankaridurg PR, Holden BA. Practical applications to modify and control the development of ametropia. Eye. 2014;28:134–41. https://doi.org/10.1038/eye.2013.255.
Parssinen O, Lyyra AL. Myopia and myopic progression among school children: a three-year follow-up study. Invest Ophthalmol Vis Sci. 1993;34:2794–802.
Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci. 2002;43:3633–40.
Rose KA, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–85. https://doi.org/10.1016/j.ophtha.2007.12.019.
Dirani M, et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009;93:997.
Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120:1080–5. https://doi.org/10.1016/j.ophtha.2012.11.009.
Nina J, Hanne J, Ernst G. Does the level of physical activity in university students influence development and progression of myopia?--a 2-year prospective cohort study. Invest Ophthalmol Vis Sci. 2008;49:1322.
Feldkaemper M, Schaeffel F. An updated view on the role of dopamine in myopia. Exp Eye Res. 2013;114:106–19.
Prepas SB. Light, literacy and the absence of ultraviolet radiation in the development of myopia. Med Hypotheses. 2008;70:635–7.
Jeremy AG, et al. Does vitamin D mediate the protective effects of time outdoors on myopia? Findings from a prospective birth cohort. Invest Ophthalmol Vis Sci. 2015;55:8550–8.
Mutti DO, Marks AR. Blood levels of vitamin D in teens and young adults with myopia. Optom Vis Sci. 2011;88:377–82.
Tideman JWL, et al. Low serum vitamin D is associated with axial length and risk of myopia in young children. Eur J Epidemiol. 2016;31:491–9.
Hammond DS, Josh W, Wildsoet CF. Dynamics of active emmetropisation in young chicks--influence of sign and magnitude of imposed defocus. Ophthalmic Physiol Opt. 2013;33:215–26.
Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31:622–60.
Zhou Z, et al. Pilot study of a novel classroom designed to prevent myopia by increasing children’s exposure to outdoor light. PLoS One. 2017;12:e0181772. https://doi.org/10.1371/journal.pone.0181772.
Cindy K, Regan Scott A. Correlation between light levels and the development of deprivation myopia. Invest Ophthalmol Vis Sci. 2015;56:299–309.
Lan W, Yang Z, Feldkaemper M, Schaeffel F. Changes in dopamine and ZENK during suppression of myopia in chicks by intense illuminance. Exp Eye Res. 2016;145:118–24.
Wu PC, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. 2018;125(8):1239–50.
Mcknight CM, et al. Myopia in young adults is inversely related to an objective marker of ocular sun exposure: The Western Australian Raine Cohort Study. Am J Ophthalmol. 2014;158:1079–1085.e1072.
Lingham G, et al. Investigating the long-term impact of a childhood sun-exposure intervention, with a focus on eye health: protocol for the Kidskin-Young Adult Myopia Study. BMJ Open. 2018;8:e020868. https://doi.org/10.1136/bmjopen-2017-020868.
Li SM, et al. Near work related parameters and myopia in chinese children: the Anyang Childhood Eye Study. PLoS One. 2015;10:e0134514. https://doi.org/10.1371/journal.pone.0134514.
Ip JM, et al. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci. 2008;49:2903–10. https://doi.org/10.1167/iovs.07-0804.
Charman WN. Myopia, posture and the visual environment. Ophthalmic Physiol Opt. 2011;31:494–501. https://doi.org/10.1111/j.1475-1313.2011.00825.x.
Vincent SJ, Collins MJ, Read SA, Carney LG, Yap MK. Corneal changes following near work in myopic anisometropia. Ophthalmic Physiol Opt. 2013;33:15–25. https://doi.org/10.1111/opo.12003.
Hua WJ, et al. Elevated light levels in schools have a protective effect on myopia. Ophthalmic Physiol Opt. 2015;35:252–62. https://doi.org/10.1111/opo.12207.
Leung TW, et al. A novel instrument for logging nearwork distance. Ophthalmic Physiol Opt. 2011;31:137–44. https://doi.org/10.1111/j.1475-1313.2010.00814.x.
Wen L, et al. A novel device to record the behavior related to myopia development— preliminary results in the lab. Invest Ophthalmol Vis Sci. 2016;57:2491.
Lan WZ, et al. The correlation between an objective index summarizing individual environmental risk factors and the change of refractive error. Invest Ophthalmol Vis Sci. 2018;41:59.
Winawer J, Wallman J. Temporal constraints on lens compensation in chicks. Vis Res. 2002;42:2651–68.
Zhu X, Winawer JA, Wallman J. Potency of myopic defocus in spectacle lens compensation. Invest Ophthalmol Vis Sci. 2003;44:2818–27.
Morgan I, Megaw P. Using natural STOP growth signals to prevent excessive axial elongation and the development of myopia. Ann Acad Med. 2004;33:16–20.
Tarutta E, Khodzhabekyan N, Filinova O, Milash S, Kruzhkova G. Long -term effects of optical defocus on eye growth and refractogenesis. Pomeranian J Life Sci. 2016;62:25–30.
Lin J. Observation of ocular haemodynamic change pre and post doing the eye exercises using color Doppler flood image. Chin J Ultrasound Diagn. 2004;5:446–7.
Li SM, et al. Efficacy of Chinese eye exercises on reducing accommodative lag in school-aged children: a randomized controlled trial. PLoS One. 2015;10:e0117552. https://doi.org/10.1371/journal.pone.0117552.
Changjun L, Wang J, Gou H, Jianzhou W. A survey on prevalence of myopia and its influential factors in middle school students. Mod Prev Med. 2010;37:3047–51.
Lin Z, et al. Eye exercises of acupoints: their impact on refractive error and visual symptoms in Chinese urban children. BMC Complement Altern Med. 2013;13:306. https://doi.org/10.1186/1472-6882-13-306.
Lin Z, et al. Eye exercises of acupoints: their impact on myopia and visual symptoms in Chinese rural children. BMC Complement Altern Med. 2016;16:349. https://doi.org/10.1186/s12906-016-1289-4.
Ping Z, Wang K, Chunhua Z, Bin Z. The epidemiological investigation of myopia in junior students. Prac J Med Pharm. 2004;21:543–5.
Kang MT, et al. Chinese eye exercises and myopia development in school age children: a Nested Case-Control Study. Sci Rep. 2016;6:28531. https://doi.org/10.1038/srep28531.
Holden BA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42. https://doi.org/10.1016/j.ophtha.2016.01.006.
Morgan IG. New perspectives on the prevention of myopia. Eye Sci. 2011;26:3.
Verkicharla PK, et al. Development of the fitsight fitness tracker to increase time outdoors to prevent myopia. Transl Vis Sci Technol. 2017;6:20.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
He, M., Chen, Y., Hu, Y. (2020). Prevention of Myopia Onset. In: Ang, M., Wong, T. (eds) Updates on Myopia. Springer, Singapore. https://doi.org/10.1007/978-981-13-8491-2_7
Download citation
DOI: https://doi.org/10.1007/978-981-13-8491-2_7
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-8490-5
Online ISBN: 978-981-13-8491-2
eBook Packages: MedicineMedicine (R0)