Abstract
Early attempts at percutaneous coronary intervention (PCI) using balloon angioplasty were largely hampered by technical limitations. Although balloon angioplasty was moderately successful at relieving an obstruction, the procedure frequently resulted in dissections which, if uncontrolled, often led to abrupt vessel closure. Furthermore, while acute luminal gain could be impressive, a combination of elastic recoil and smooth muscle hyper-proliferation often negated the benefits of an acceptable immediate angiographic result. Elastic recoil could occur minutes to hours post-procedure resulting in acute myocardial infarction (AMI) and need for emergent coronary artery bypass grafting (CABG). This led to a pivotal development in the history of PCI with introduction of the metallic stent, which drove rapid improvements in short- and long-term procedural safety and efficacy. Stent design has been a remarkable area of technological advances with pivotal milestones including evolution of metallic architecture and introduction of the drug-eluting stent (DES). Although DES is now considered the default option for most PCI, bare-metal stents (BMS) still represent a sizeable proportion of stent procedures in some countries and in some settings may have arguable advantage. In this chapter we aim to review contemporary evidence for the use of BMS in modern interventional practice.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
11.1 Introduction
Early attempts at percutaneous coronary intervention (PCI) using balloon angioplasty were largely hampered by technical limitations. Although balloon angioplasty was moderately successful at relieving an obstruction, the procedure frequently resulted in dissections which, if uncontrolled, often led to abrupt vessel closure. Furthermore, while acute luminal gain could be impressive, a combination of elastic recoil and smooth muscle hyper-proliferation often negated the benefits of an acceptable immediate angiographic result. Elastic recoil could occur minutes to hours post-procedure resulting in acute myocardial infarction (AMI) and need for emergent coronary artery bypass grafting (CABG). This led to a pivotal development in the history of PCI with introduction of the metallic stent, which drove rapid improvements in short- and long-term procedural safety and efficacy. Stent design has been a remarkable area of technological advances with pivotal milestones including evolution of metallic architecture and introduction of the drug-eluting stent (DES). Although DES is now considered the default option for most PCI, bare-metal stents (BMS) still represent a sizeable proportion of stent procedures in some countries and in some settings may have arguable advantage. In this chapter we aim to review contemporary evidence for the use of BMS in modern interventional practice.
11.2 Bare-Metal Stents
The introduction of BMS in the mid-1980s allowed PCI procedures to rapidly enter mainstream clinical practice. Early BMS were crude, being largely constructed of relatively thick 316 L stainless steel and needed to be cut to length, and then crimped onto the delivery balloon catheter. However, once successfully in situ, these devices were able to effectively maintain vessel patency and thereby largely prevent the abrupt vessel closure and elastic recoil which had hampered balloon only procedures. Consequently, PCI was to become safer and more efficacious. As technology improved further, particularly with pre-cut and pre-crimped stents delivered using a monorail system, PCI was to rapidly evolve into the preferred mode of revascularization for selected patients due to the minimal invasive nature of the procedure coupled with rapid recovery.
Early BMS had important limitations, related to both device design and to biocompatibility. This led to the emergence of neo-intimal hyperplasia and neo-atherosclerosis as factors which could preclude optimal long-term outcomes and result in in-stent restenosis (ISR). With time, it was learned that reduced strut thickness lessened the localized inflammatory responses that may both hinder endothelialization and drive ISR. This led to improved stent architecture and a shift from 316 L stainless steel to cobalt chromium, thereby permitting a marked reduction in strut thickness without loss of radial strength, while also facilitating improved delivery and conformability. Clinical studies demonstrated that the reduction in stent strut thickness resulted in improved delivery, conformability and reduced incidence of ISR.
11.3 Drug-Eluting Stents
One the most important milestones in interventional cardiology in recent decades was development of the DES. Initially these were developed by coating standard BMS with an anti-proliferative agent (e.g. sirolimus) which was bonded to the stent using a polymer which also served to regulate drug release. The anti-proliferative agent effectively led to localized arrest of the smooth muscle cell proliferation cycle around the implanted device and thereby limited propensity to ISR. With cardiologists eager to avoid ISR, DES technology rapidly entered mainstream practice and quickly became the default stent choice, with device implants both on and off label.
However an important downside to first-generation DES rapidly emerged related to delayed and incomplete neo-endothelialization around the stent struts. In early-generation DES, this led to observations of increased rates of stent thrombosis as compared to BMS. This resulted in the Food and Drug Administration (FDA) issuing an advisory warning regarding the risk of late stent thrombosis after DES. Consequently, this led to an immediate decline in DES usage. Progress to tackle these deficiencies was rapidly developed. Pharmacologically, more potent antiplatelet agents were brought to market with increased duration of dual antiplatelet therapy (DAPT). Meanwhile stent technological advances included thinner struts, improvements in anti-proliferative drugs, use of new polymers with increased biocompatibility or biodegradability and more recently polymer-free stents and the concept of a bioresorbable vascular scaffold (BVS) which over time is completely reabsorbed. Although in theory BVS offer advantage over both BMS and DES due to lack of permanent metallic structure, initial results have not met expectations with higher stent thrombosis and target-vessel MI rates resulting in some early platforms being withdrawn from clinical use. Research and development is ongoing, but currently BVS cannot be recommended for use during primary PCI and will not be discussed further in this chapter.
11.3.1 Anti-proliferative Drugs
Once the issues of ISR and stent thrombosis associated with use of stents were identified, several agents including gold, carbon and heparin were coated onto stents to try and improve biocompatibility, reduce inflammation and prevent thrombosis. None of these agents were shown to have any significant beneficial effects, and thus other solutions were clearly required.
The use of the anti-proliferative agents sirolimus and paclitaxel showed significant reductions in ISR compared to BMS and was utilized in first-generation DES. Sirolimus is an immunosuppressive compound that acts by receptor inhibition of the mammalian target of rapamycin (mTOR) resulting in the cell-cycle progression and consequently inhibits cell proliferation. Paclitaxel is an oncological agent that inhibits cell proliferation by disturbing cellular microtubule organization. The use of the ‘limus’ drugs has been shown to be superior to other anti-proliferative agents, and newer agents such as zotarolimus, everolimus and the more lipophilic biolimus are used in most current-generation DES with similar efficacy.
11.3.2 Polymers
Initial DES technology required the incorporation of anti-proliferative drugs into permanent synthetic polymers. These polymers however increase local inflammatory response and reduced endothelialization and were thought to be a key flaw in early designs driving propensity to stent thrombosis and mandating longer duration of DAPT. More biocompatible and even biodegradable polymers have now been developed. These cause less inflammation and hence permit more rapid and complete endothelial coverage. More recently, polymer-free DES have also been developed. These use the concept of drug storage ‘wells’ or surface etching to load the drug but allow rapid dissolution of the anti-proliferative agent without use of a polymer giving the benefits of the pharmacology with the early endothelialization offered by BMS.
Current-generation DES have reduced ISR rates to incredibly low levels while improving the safety profile of the devices and thus have become the ‘gold standard’ for definitive PCI in the majority of patients. This is supported by numerous randomized controlled trials, meta-analyses and real-world data showing improved safety and efficacy with new-generation DES. Nonetheless, some still argue that there remains a role for BMS in contemporary clinical practice. A number of important issues remain and in the context of primary PCI for STEMI.
Potential Advantages of BMS
-
More rapid endothelialization allowing abbreviated DAPT
-
Safety in high bleeding risk patients
-
Safety in elderly patients
-
Safe with concomitant need for anticoagulation (e.g. atrial fibrillation)
-
-
Reduced cost
-
Price sensitive healthcare models
-
11.4 DES vs. BMS for Primary PCI
Primary PCI is established as the optimal treatment strategy for STEMI patients with the use of coronary stenting achieving far superior reperfusion at lower risk compared to fibrinolysis. The use of BMS has been shown to be superior to balloon angioplasty alone, and several studies have subsequently shown advantage of DES over BMS. However, the supposed advantage of DES is predominantly driven by reduced need for long-term revascularization rather than immediate post-infarct survival. Newer-generation DES have largely been shown to be superior to first-generation stents for a broad range of indications with similar outcomes between most contemporary devices.
The EXAMINATION (everolimus-eluting stents versus bare-metal stents in ST-segment elevation myocardial infarction) trial investigated the use of everolimus-eluting stents (Xience V, Abbott Vascular) versus BMS (Multi-Link Vision, Abbott Vascular) in an all-comer STEMI population. 1498 patients were randomized in a 1:1 fashion, and 2-year analysis found that EES had a trend towards a reduction in the primary endpoint, namely, the combined endpoint of all-cause death, recurrent MI and any revascularization from 17.3% in BMS to 14.4% (p = 0.11). Rate of target lesion revascularization (TLR) was significantly lower in the EES group at 2.9% vs. 5.6% (p = 0.009) as was definite or probable stent thrombosis (0.8% vs. 2.1%; p = 0.03 and 1.35 vs. 2.8%; p = 0.04, respectively). Recently published 5-year follow-up results showed a significant reduction in the primary endpoint (21% vs. 26%; p = 0.033) with use of EES, mainly driven by the reduction of all-cause mortality by EES as compared to BMS (9% vs. 12%; p = 0.047). TLR was also significantly reduced although there was no difference in rates of stent thrombosis at 5 years.
COMFORTABLE AMI (the effect of biolimus-eluting stents with biodegradable polymer vs. bare-metal stents on cardiovascular events among patients with AMI) compared a biolimus DES (BioMatrix, Biosensors) with a biodegradable polymer (BES) with BMS in 1161 patients presenting with STEMI. Major adverse cardiac events (MACE) were reduced in BES (4.3%) vs. BMS (8.7%) at 1 year (p = 0.004). This reduction was driven by a reduction in target-vessel-related re-infarction (0.5% vs. 2.7%, p = 0.01) and ischaemia-driven TLR (1.6% vs. 5.7%, p < 0.001) in BES as compared to BMS. At 2-year follow-up, TLR continued to be reduced in the BES group (3.1% vs. 8.2%; p < 0.001) and cardiac death or target-vessel MI was also reduced (4.2% vs. 7.2%, p = 0.036). A combined analysis of EXAMINATION and COMFORTABLE AMI demonstrated a reduction in both stent thrombosis and target-vessel MI with the use of DES over BMS.
The Norwegian coronary stent trial (NORSTENT) examined the use of DES versus BMS in 9013 patients undergoing PCI (26.3% with STEMI) over a 3-year period. Patients were randomized in a 1:1 fashion to BMS or DES (82.9% everolimus-eluting stents and 13.1% zotarolimus-eluting stents). The primary outcome was a composite of death from any cause and nonfatal MI. After 6 years of follow-up, there was no difference found in the primary outcome between the groups (16.6% in the DES group vs. 17.1% in the BMS group; p = 0.66), which is reassuring given the ongoing use of BMS. There was however, in line with previous studies, a reduction in repeat revascularization (16.5% in DES vs. 19.8% in BMS; p < 0.001). There was also a reduction in the rate of definite stent thrombosis with DES (0.8% vs. 1.2%; p = 0.0498).
In light of these and other studies, it can be said that in the general STEMI population, the use of current-generation DES is preferable to BMS. This is driven by the reduction in target-vessel revascularization and myocardial infarction. There are some special specific issues however, which require review.
11.4.1 Stent Thrombosis
Although an infrequent occurrence, stent thrombosis (ST) is the most feared complication of stent implantation. ST can present immediately after stent implant or sometimes even many years later. Mode of presentation is highly variable but can include sudden (cardiac) death and STEMI. Worryingly ST has an extremely high mortality rate of up to 50% in some series—far in excess of that seen with STEMI due to de novo lesions. The explanation for the disparate mortality rate remains unclear. Nonetheless, avoidance of ST is of paramount importance, and the interventional cardiologist must always be mindful of the various factors that may predispose to this malignant process during any PCI procedure.
Purported mechanisms for ST are predominantly considered either mechanical, related to platelet activity, or a combination of both. The former includes stent mal-apposition, stent under-expansion, stent edge dissection, longer stent length and small stent calibre. In contrast, factors related to platelet function are represented by failure to adequately inhibit platelet adhesion/aggregation. This may include aspirin or thienopyridine ‘non-responders’ and, when these drugs have been erroneously omitted or withheld due to prescribing error, poor compliance, bleeding complications or need for emergent surgical interventions. Acute coronary syndrome (ACS) as a clinical entity at the time of the index procedure is also frequently cited as an independent predictor of stent thrombosis.
The timing of stent thrombosis differs between the types of stents. During the first months, it may occur after both BMS and DES implantation. However, beyond 1 year, it is more frequently observed after first-generation DES implantation. It was long assumed that this related to suboptimal endothelialization due to presence of the antimitotic agent or localized inflammation from ongoing presence of non-biocompatible polymers. Although autopsy and experimental studies have shown delayed healing to be more common with DES, new-generation DES have consistently shown a reduction in ST as compared to BMS, both short and long term. Therefore the risk of stent thrombosis is no longer a reason to advocate the use of BMS over DES.
11.4.2 DAPT Duration
The most common convincing reason for the use of BMS is to allow shorter durations of DAPT. This may be because of concerns of a high bleeding risk, poor compliance or the need for urgent/semi-urgent surgery. In a recent survey looking at the reasons for the decision to use BMS over DES at 31 European centres, concerns with patient DAPT compliance were the main reason for using BMS (39%). Concerns regarding compliance should be dealt with in a multidisciplinary fashion with assessment of a patient’s psychosocial status and patient education being of utmost importance. In high-risk anatomy, despite likely technical success of PCI, plain balloon angioplasty as a temporary reperfusion measure followed by coronary artery bypass may need to be considered.
The addition of more potent antiplatelet agents (e.g. prasugrel, ticagrelor) and studies demonstrating cardiovascular benefits of longer DAPT duration have resulted in the need for individualized DAPT decision-making with bleeding risk having to be balanced against the risk of further cardiovascular events. Tools such as the DAPT and PRECISE-DAPT scores can be used to guide the decision-making process. One study has shown safety of a <15 days of DAPT post PCI with BMS. However, in general, a minimum of 1-month DAPT is advised post BMS and 6 months post DES (for elective PCI).
Current guidelines advise the use of DAPT for 12 months post PCI for acute coronary syndromes, independent of the type of stent used. These guidelines however are largely based on the results of old studies with use of first-generation stents, and a number of recent studies have challenged these guidelines. The recent DAPT-STEMI trial assessed the efficacy of 6 vs. 12 months of DAPT in STEMI with the use of a zotarolimus-eluting stent in 1496 patients with the 6-month strategy reaching non-inferiority. Shorter DAPT regimes have also been investigated with several trials demonstrating safety of DES use with a 3-month DAPT regimen. Two studies have specifically examined very short DAPT strategies.
The ZEUS trial investigated the use of a zotarolimus-eluting stent (Endeavor, Medtronic) versus BMS with a short DAPT duration strategy in 1606 patients who were deemed uncertain for DES use on the basis of bleeding, thrombotic or restenosis risk criteria. 19% of the patients in the study were treated for STEMI and the median DAPT duration was 32 days. There was a reduction in the primary endpoint of MACE in the ZES group (17.5% vs. 22.1%; HR 0.76; 95% CI 0.61–0.95; p = 0.011) with lower MI (2.9% vs. 8.1% p < 0.001) and target-vessel revascularization (TVR) rates (5.9% vs. 10.7%; p = 0.001). Definite or probable stent thrombosis was also significantly reduced (2.0% vs. 4.1%; p = 0.019). The Endeavor stent has now been replaced by the newer-generation Resolute stent which has thinner struts and a more biocompatible polymer which theoretically should offer additional protection, although this has not been demonstrated in a randomized controlled trial.
A polymer-free and carrier-free drug-coated stent (DCS) that transfers umirolimus (biolimus A9) (BioFreedom, Biosensors) was compared to BMS (Gazelle, Biosensors) with a 1-month DAPT strategy in the LEADERS-FREE trial in 2466 high bleeding risk patients. 22.8% of the study population was treated for STEMI. 2-year follow-up demonstrated superiority of DCS over BMS with a reduction of a combined endpoint of cardiac death, MI or stent thrombosis (12.6% vs. 15.3%; HR 0.80; CI 0.64–0.99; p = 0.039). Clinically driven TLR was also significantly lower in the DCS (5.6% vs. 10.3%; p < 0.001). Recently published 2-year outcomes showed sustained benefits of DCS vs. BMS with a lower rates of the primary endpoint (13% vs. 21.5%, HR 0.57; 95% CI 0.39–0.85; p = 0.005) and TLR (7.4% vs. 10.4%; HR 0.45; 95% CI 0.24–0.83; p = 0.009). Stent thrombosis rates also tended to be lower with DCS (1.2% vs. 3.2%, HR 0.39; 95% CI 0.12–1.25; p = 0.1).
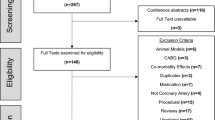
In summary, the requirement for a shortened duration of DAPT is no longer a robust reason to justify the use of BMS over DES with growing evidence that the use of DES is in fact superior (Fig. 11.1). Future trials are likely to add to the current evidence base.
11.4.3 Atrial Fibrillation
Atrial fibrillation (AF) is a common comorbidity in the setting of STEMI, estimated to occur in up to 20% of patients, and it is associated with a significant increase in mortality. The most important management issue in AF is the prevention of embolic events with anticoagulation. Traditionally this was achieved by the use of warfarin; however, the use of non-vitamin K antagonist oral anticoagulants (NOACs) is now recommended as first-line treatment for anticoagulation for AF. The addition of antiplatelet agents for the treatment of STEMI in patients with AF, or conversely the addition of anticoagulation for the treatment of AF in patients post-STEMI, significantly increases the risk of major bleeding. As part of a strategy to reduce duration of triple therapy with DAPT and an anticoagulant, the use of BMS for PCI in the setting of AF has been advocated; however this is no longer the accepted strategy due to evidence of the safety of shorter or indeed absence of the so-called triple therapy.
The WOEST (what is the optimal antiplatelet and anticoagulant therapy in patients with oral anticoagulation and coronary stenting) trial investigated the use of triple therapy (aspirin, clopidogrel and warfarin) versus double therapy (plavix and warfarin) in 573 patients undergoing PCI. Among the patient population, 28% had PCI for ACS and 31% of patients received BMS. The rate of bleeding episodes was significantly reduced in patients who received double therapy without any increase in thrombotic or cerebrovascular complications. In fact a composite endpoint of death, MI, stroke, TVR and stent thrombosis was lower in the double-therapy group (11.1% vs. 17.6%; HR 0.6; 95% CI 0.38–0.94; p = 0.025).
The use of NOACs in post-PCI regimens was examined in depth in the PIONEER-AF trial. Patients undergoing PCI with AF (either BMS or DES) were randomized to one of three pharmacological strategies; rivaroxaban 15 mg o.d. plus single P2Y12 inhibitor, low-dose rivaroxaban (2.5 mg b.d.) plus DAPT or warfarin and DAPT. 12% of the population included presented with STEMI and 31.8% received BMS. Both of the rivaroxaban regimens were associated with lower risk of clinically significant bleeding than the warfarin arm with no increase in cardiovascular or thromboembolic events. The use of other NOACs with similar shortened or less aggressive regimens is currently under investigation with results expected soon.
The evidence supporting the safety of shortened, or absence of, triple therapy in post-PCI patients with AF means that there is no compelling reason to use BMS in patients with AF and with broader indications for anticoagulation (paired with development of safer agents), combination of NOAC with a P2Y12 inhibitor is likely to be the favoured strategy.
11.4.4 Elderly Patients
For many of the reasons previously outlined (high bleeding risk, concerns regarding compliance, AF and other comorbidities), elderly patients have been traditionally seen as a population more suited to BMS use. In addition, they are often excluded from clinical trials. Elderly patients were not excluded in EXAMINATION or COMFORTABLE AMI, but the average age in both studies was approximately 60 years old.
The XIMA (Xience or vision stents for the management of angina in the elderly) trial compared the use of EES and BMS in 800 patients ≥80 years of age undergoing PCI for angina or ACS, and patients with STEMI were excluded. Results demonstrated that for the primary composite endpoint of death, MI, stroke, TVR or major haemorrhage, DES was non-inferior to BMS. Rates of haemorrhage were not increased in the DES group despite the longer use of DAPT (94% on DAPT at 1 year in DES group vs. 32.2% in BMS group). MI (8.7% vs. 4.3%; p = 0.01) and TVR (7.0% vs. 2.0%; p = 0.001) occurred more often in the BMS group. Although a STEMI population was not included, the data is reassuring in regard to similar advantages gained by the use of DES in elderly patients as seen in trials with a younger cohort.
The SENIOR (drug-eluting stents in elderly patients with coronary artery disease) trial investigated the use of DES vs. BMS in 1200 patients over the age of 75 undergoing PCI; 10.6% were treated for STEMI and DAPT duration was shortened—1 month in stable patients and 6 months in those presenting with ACS. The use of a bioabsorbable polymer DES (Synergy, Boston Scientific) was associated with a 29% reduction in the composite primary endpoint of all-cause mortality, MI stroke and revascularization at 1 year. Consistent with other studies, the benefit was driven by a 71% reduction in ischaemia-driven TLR. Bleeding and stent thrombosis rates in both groups were low.
As demonstrated there is growing evidence that the use of BMS in elderly patients, including in the setting of STEMI, is no longer a recommended strategy.
11.4.5 Cost
Reduced cost is a common reason cited for the use of BMS over DES in PCI. Although upfront costs may be reduced, the increase in use of DES has reduced this gap. A number of studies on the cost-effectiveness of using DES as opposed to BMS have shown that although periprocedural costs are higher, long-term cost-effectiveness is achieved due to the lower rates of future cardiovascular events with the use of new-generation DES. However cost-benefit analyses are not universally applicable to every healthcare environment, but we believe that in general stent cost cannot be used to justify use of BMS in STEMI.
11.5 Summary and Recommendations
In the present era, given generally excellent clinical outcomes, it is widely accepted that current-generation DES should be the default consideration for all patients undergoing PCI including primary PCI. Although theoretical advantages of BMS are often cited, current-generation DES not only appear to be more efficacious but also safer than BMS in a broad range of patients and clinical presentations. This likely now includes patients at high bleeding risk or where DAPT may need to be prematurely discontinued. However BMS use is likely to be continued in certain healthcare systems predominantly due to cost analyses. Recent data has shown that modern BMS have good long-term outcomes in regard to mortality and nonfatal MI but at the expense of increased revascularization.
Recommendations
-
New-generation DES should be the stent of choice for PCI including in STEMI presentations.
-
If a shortened DAPT regime is required, the use of DES is still preferable with safety of a 3-month strategy established.
-
If very short DAPT duration is required (1 month), then the use of a polymer-free biolimus A9-coated stent, if available, is preferable to BMS, although other contemporary platforms are currently under investigation in this setting.
-
BMS should not be used for complex anatomical subsets with higher rates of ISR.
11.6 Case Report: Primary PCI with Direct Stenting in Patient with Inferior Myocardial Infarction
11.6.1 Introduction
A 66-year-old male came to the hospital with continuing central chest pain of 3-h duration, accompanied by diaphoresis and dyspnoea. His risk factors were hypertension and dyslipidaemia. The ECG showed an inferior ST-elevation myocardial infarction (STEMI) with complete heart block (Fig. 11.2). His blood pressure was 80/60 mmHg. He was loaded with Aspirin 300 mg and clopidogrel 300 mg, given fluid boluses to support his BP and brought to the catheter laboratory for primary PCI (PPCI).
A temporary pacemaker wire was delivered to the right ventricle through the right femoral vein. Primary PCI was performed through right radial approach. A diagnostic TIG catheter was engaged to left coronary artery, and images were taken demonstrating that this was unobstructed (Fig. 11.3).
A JR 3.5 guide catheter was then delivered to right coronary artery but failed to engage adequately. The patient had VF requiring defibrillation two times at 200 joules with successful restoration of circulation. The guide was switched to an AL 0.75 which engaged well. Angiography revealed a 99% stenosis in the mid-right coronary artery (RCA), which was somewhat ectatic (Fig. 11.4). A Sion Blue was used to cross the lesion. Direct stenting was then done with a Promus Element Plus 3.5 × 20 mm, inflated at 14 ATM for 13 s (Fig. 11.5). Post dilatation was performed with a non-compliant 4 mm balloon up to 16 ATM. The final angiogram showed no dissection, TIMI flow III, residual stenosis 0% (Fig. 11.6).
Our patient was transferred to the coronary care unit for observation and discharged after 4 days. He remains well at subsequent outpatient review.
This case illustrates the utility of contemporary DES platforms. Coronary artery calibre can easily be misjudged, particularly in primary PCI; however many contemporary platforms allow for significant oversizing without disruption of stent architecture, polymer or drug release kinetics. Moreover, even in a large-calibre vessel, the benefit of a DES in terms of reduction of ISR and improving long-term outcomes particularly among diabetic patients cannot be disregarded.
Further Readings
Bonaa KH, Mannsverk J, Wiseth R, Aaberge L, Myreng Y, Nygard O, et al. Drug-eluting or bare-metal stents for coronary artery disease. N Engl J Med. 2016;375(13):1242–52.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Raber L, Kelbaek H, Ostojic M, Baumbach A, Heg D, Tuller D, et al. Effect of biolimus-eluting stents with biodegradable polymer vs bare-metal stents on cardiovascular events among patients with acute myocardial infarction: the COMFORTABLE AMI randomized trial. JAMA. 2012;308(8):777–87.
Sabate M, Brugaletta S, Cequier A, Iniguez A, Serra A, Hernadez-Antolin R, et al. The EXAMINATION trial (Everolimus-eluting stents versus bare-metal stents in ST-segment elevation myocardial infarction): 2-year results from a multicenter randomized controlled trial. JACC Cardiovasc Interv. 2014;7(1):64–71.
Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the task force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018;39(3):213–60.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
This chapter is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
Copyright information
© 2018 The Author(s)
About this chapter
Cite this chapter
Hensey, M., Sathananthan, J., Teguh, W.P., Mulvihill, N. (2018). Is There a Role for Bare-Metal Stents in Current STEMI Care?. In: Watson, T., Ong, P., Tcheng, J. (eds) Primary Angioplasty. Springer, Singapore. https://doi.org/10.1007/978-981-13-1114-7_11
Download citation
DOI: https://doi.org/10.1007/978-981-13-1114-7_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1113-0
Online ISBN: 978-981-13-1114-7
eBook Packages: MedicineMedicine (R0)