Abstract
Bispecific monoclonal antibodies (BsMAb) are unique engineered macromolecules that have two different pre-determined binding specificities. Their ability to simultaneously bind to a specific antigen and a given detection moiety enables them to function as excellent bifunctional immunoprobes in diagnostic assays. BsMAb are being exploited for the development of simple, rapid, and highly sensitive immunoassays for diagnosis of bacterial and viral infectious diseases. This chapter describes the use of BsMAb for the detection of Mycobacterium tuberculosis, Escherichia coli O157:H7, Bordetella pertussis, Severe Acute Respiratory Syndrome coronavirus, and Dengue virus. Further, BsMAb have been utilized for diagnosis of various types of cancers. The use of BsMAb in detection of prostate cancer and in cancer diagnostic imaging is also discussed.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Severe Acute Respiratory Syndrome
- Dengue Virus
- Tumor Uptake
- Severe Acute Respiratory Syndrome
- Bordetella Pertussis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
19.1 Introduction
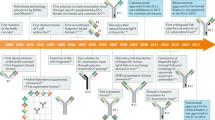
Bispecific monoclonal antibodies (BsMAb) are uniquely engineered hetero-bifunctional macromolecules with two distinct binding specificities within a single molecule (Cao and Suresh 1998; Suresh et al. 1986b). They represent the second generation of monoclonal antibodies, and although structurally bivalent, they are functionally univalent for binding each molecule. Typically, BsMAb have one paratope specific for a particular protein or an antigen and another paratope specific for a detection moiety such as an enzyme (Fig. 19.1). BsMAb can therefore function as versatile hetero-bifunctional cross-linkers. The binding of BsMAb to both molecules is dependent on the affinity of epitope–paratope interaction and is highly specific. BsMAb can be produced by three methods: (a) chemical conjugation involving chemical cross-linking (the original method for BsMAb production); (b) somatic hybridization involving hybridoma technology; and (c) genetic engineering involving recombinant DNA technology (Das and Suresh 2005). Production of BsMAb by hybridoma technology involving bifunctional fusion (Fig. 19.2) of two different hybridomas that produce distinct monoclonal antibodies is more common compared to the other BsMAb production methods (Kohler and Milstein 1975). BsMAb have been exploited for a variety of in vivo and in vitro applications ranging from diagnostics to therapeutics (Cao and Suresh 1998). The use of BsMAb for different therapeutic applications and gene therapy is described in detail in earlier chapters. This chapter focuses only on the diagnostic applications of BsMAb.
Diagrammatic representation of a bispecific antibody. One paratope of the Bispecific antibody is directed against a specific target antigen of a tumor, virus, bacteria, or a parasite. The second paratope of the Bispecific antibody is directed against an effector molecule, which may be a detection moiety (such as an enzyme), toxin, drug, liposome, radioisotope, cytokines or immune cells. The diagram is adapted from Cao and Suresh, Bioconjugate Chemistry, 1998
BsMAb function as excellent diagnostic immunoprobes due to their intrinsic binding sites to any two molecules in a pre-determined order. They offer distinct advantages over other conventional probes used in diagnostic assays due to their monovalency for one antigen and simultaneous binding to a marker enzyme. One epitope of BsMAb is usually directed against a marker enzyme such as horse radish peroxidase (HRPO), alkaline phosphatase, or β-galactosidase, which enables signal generation in immunodiagnostic assays. BsMAb have been used in a number of diagnostic applications such as immunoassays, immunohistochemistry, and radio-immunodiagnosis (Kreutz and Suresh 1997; Suresh 1991; Suresh et al. 1986a). Their use in diagnostic assays has revolutionized the field of immunodiagnostics due to the higher sensitivity and reproducibility that can be achieved in the assays.
19.2 Advantages of Using BsMAb in Diagnostics
The main advantage of using BsMAb in immunodiagnostics is that maximum specific activity and functional efficiency can be achieved since every antibody molecule is associated with a signal generating molecule (Kreutz and Suresh 1997). In addition to making the diagnostic assays rapid, BsMAb enhance sensitivity and specificity of detection. They significantly reduce or even eliminate false positive reactions especially in assays such as ELISA. In the case of immunohistochemistry, the use of BsMAb leads to decreased background, fine and sharp morphological information, clear and distinct identification of immune reactive sides, and good resolution of ultrastructural details (Milstein and Cuello 1983; Suresh et al. 1986a). Other advantages of using BsMAb in immunodiagnostic assays include improvement in signal to noise ratio and simplification of the assay procedure. They can easily be used as nanoprobes making ultrasensitive detection possible especially in the case of competitive immunoassays. In contrast to BsMAb, chemically conjugated monoclonal and polyclonal antibodies often exhibit higher background (Liu et al. 2003).
Traditionally monoclonal antibodies have been employed in many immunodiagnostic assays. Typically, the use of monoclonal antibodies in diagnostic applications requires chemical manipulation of the antibody such as chemical cross-linking in order to conjugate the detection moiety (such as an enzyme or biotin) onto the antibody. Chemical cross-linking of detection moieties to antibodies has many disadvantages as outlined below (Kricka 1994; Milstein and Cuello 1983). (a) It is a random process where the combination ratio of the antibody and the conjugating chemical is not fixed, generally resulting in batch to batch variations in the detection reagent produced. (b) The size of the resultant conjugated antibodies is not uniform influencing their ability to penetrate, which is especially critical for immunohistochemical applications. (c) Inactivation of active site or binding site of the detection moiety or the antibody and/or aggregation may occur during chemical conjugation. (d) Covalent linkages occur between the detection moiety and the antibody, which is not very preferable for in vivo diagnostic applications. (e) The antibodies produced often have low specific activity and decreased shelf life. The above factors have a significant impact on the performance of the conjugated monoclonal antibodies and therefore the reproducibility of the immunodiagnostic assay method. In contrast, the use of BsMAb completely eliminates the need for chemical conjugation of the antibody with the detection moiety. The bispecific nature of BsMAb ensures that the combination ratio of the antibody and the detection moiety is always 1:1. Further, since BsMAb are generally already tagged with the detection enzyme during the purification step, extra steps of enzyme addition and subsequent washing can be avoided during the immunoassay. BsMAb function as uniform, homogenous immunoconjugates with reproducible high specific activity and therefore serve as an excellent alternative to chemically conjugated monoclonal antibodies.
BsMAb are extremely versatile and function as robust immunoconjugates in the assay. They can be used in a variety of immunodiagnostic assays that are designed in multiple formats including the conventional format such as the microtitre plate assay and as well newer formats such as swab, strip, or filter disk assays. In the newer formats the end point of the assay can be read out visually without the need of any instrument, which makes the immunoassay extremely convenient for use as a point of care detection test in diverse health care settings.
19.3 BsMAb for Diagnosis of Infectious Diseases
One of the major challenges for the global health care system is to control the spread of infectious diseases, which cause 9.5 million deaths annually (WHO (2010), World Health Organization report). Diagnosis of a disease at its early stage is of paramount importance in combating both its progression and spread in the community. In order to develop effective diagnostic immunoassays for various infectious diseases, the high specificity of antigen–antibody interaction can be exploited. Due to their unique characteristics, BsMAb are extremely useful for developing simple, rapid, and point of care immunodiagnostic assays for detection of infective particles (specific antigen of the infective agent). The following sections describe some examples for the use of BsMAb in the diagnosis of infectious diseases caused by both bacteria and viruses.
19.3.1 Diagnosis of Bacterial Infections
19.3.1.1 Mycobacterium tuberculosis
According to the World Health Organization (WHO) about 1.3 million deaths were due to tuberculosis (TB) alone in the year 2008 (WHO-TB (2010), World health organization report on TB). Lack of early detection of infected individuals has resulted in the rapid spread of this disease to different parts of the world. The problem is further compounded due to co-infection with human immunodeficiency virus (HIV) that has led to a steep increase in morbidity and mortality. In fact, TB has now become the leading cause of death for HIV-infected patients (WHO-TB (2010), World Health Organisation report on TB). TB is caused by the bacterium Mycobacterium tuberculosis, which is highly resilient and rampant worldwide. The current diagnosis for M. tuberculosis mainly relies on the result of sputum smear microscopy (SSM) and bacterial culture method, both of which are not useful for early stage detection. SSM is not very sensitive and can only detect if the bacterial load is above 104/ml of sputum. Moreover, it is often difficult to collect sputum samples from elderly and pediatric populations who are especially vulnerable to M. tuberculosis infection due to their weak immune system. Bacterial culture method, which is still regarded as the gold standard for detecting M. tuberculosis takes about 7–10 days to provide results and also requires dedicated culture facilities. In the majority of TB cases, due to the above problems, detection is often performed based on clinical symptoms and results of chest radiograms. However, none of the above methods are specific because many other pulmonary diseases also show similar symptoms and chest radiograms. As a result of this delayed and faulty diagnosis system, patients are often treated incorrectly and in most cases this partly contributes to bacterial evolution towards multi-drug resistant (MDR) and extremely drug resistant (XDR) strains of M. tuberculosis.
Recently, sophisticated molecular assays such as interferon gamma release assay (IGRA) and nucleic acid amplification (NAA) assay have become available; however, their performance is also questionable (Campos et al. 2008; Lalvani and Millington 2008; Madariaga et al. 2007). These molecular assays are moreover difficult to perform in resource-constrained countries due to their high cost and requirement of technical sophistication. Currently there is no simple, rapid, and inexpensive point of care immunodiagnostic assay available for the detection of M. tuberculosis. Our laboratory therefore has developed a novel and highly sensitive immunodiagnostic assay for the detection of M. tuberculosis using BsMAb (Sarkar and Suresh 2010, University of Alberta, Unpublished data). Only a general outline of the developed BsMAb-based immunodiagnostic assay is described here. To design the immunoassay in either strip or swab format, any specific M. tuberculosis antigen can be used to generate BsMAb. The unraveling of the complete genome sequence of M. tuberculosis (Cole et al. 1998) has made it easier to identify antigens that are highly specific to the bacteria and not other related members of mycobacteria. Some of the important M. tuberculosis antigens (Palma-Nicolas and Bocanegra-Garcia 2007) that could be possible candidates for BsMAb generation are mentioned in Table 19.1.
The chosen M. tuberculosis antigen is used to first generate a monoclonal antibody and in the subsequent step the hybridoma secreting the monoclonal antibody is fused with another hybridoma secreting monoclonal antibody against any of the detection enzymes like HRPO or alkaline phosphatase to obtain a hybrid-hybridoma or quadroma producing the desirable BsMAb (Kreutz et al. 1998; Suresh et al. 1986b). After isolating a stable clone expressing the BsMAb, it is expanded in a bioreactor and subsequently the BsMAb is purified using affinity chromatography. Our laboratory has designed a novel purification process to isolate BsMAb in which one of the fusion monoclonal antibody partners is directed against HRPO (Bhatnagar et al. 2008). The process allows high efficiency purification of the BsMAb using m-aminophenylboronic acid agarose column along with HRPO tagging. The general format of the immunoassay involves coating a solid phase (swab or strip) with the M. tuberculosis antigen-specific monoclonal antibody and then blocking any unbound sites using a suitable buffer. The coated and blocked swab/strip is incubated with the clinical specimen collected from the patient. The M. tuberculosis antigen present in the sample would then specifically bind to the monoclonal antibody and other non-specific unbound materials are washed off, after which, the purified BsMAb is used as the detection antibody. As one arm of BsMAb can recognize the antigen, it would bind to the antigen forming a sandwich. Given that BsMAb is already tagged with HRPO, addition of the enzyme substrate 3, 3′, 5, 5′-tetramethylbenzidine (TMB) results in the formation of blue color that can easily be identified. A schematic of the general assay format is shown in Fig. 19.3.
General assay format for BsMAb-based immunoassay. The capture monoclonal antibody (MAb) is first immobilized onto a solid phase. This antibody binds to the respective specific antigen present in the test sample. Upon addition of the corresponding Bispecific monoclonal antibody (bsMAb), one arm of the bsMAb binds to the specific antigen while the other arm bound to HRPO converts the subsequently added TMB substrate to a blue colored product that can be easily detected
The BsMAb-based immunodiagnostic assay for the detection of M. tuberculosis infection has several distinct advantages. The assay is highly specific, sensitive and at the same time easy to perform since it does not require any technical expertise. In addition, results of the assay can be obtained within few hours of sample collection and also the end point can be read out visually. Furthermore, the design of the assay makes it inexpensive so that the test can easily be performed in resource-constrained settings.
19.3.1.2 Escherichia coli O157:H7
E. coli O157:H7 belongs to the group of Verocytotoxin or Shiga toxin producing E. coli that has surfaced as an important food- and water-borne pathogen worldwide (Fraser et al. 2004; Law 2000). It causes non-bloody or bloody diarrhea (hemorrhagic colitis) and hemolytic uremic syndrome characterized by hemolytic anemia, thrombocytopenia, and acute renal failure (Griffin and Tauxe 1991). E. coli O157:H7 is therefore classified as enterohemorrhagic E. coli (EHEC); it is reported to cause about 73,000 cases of infections per year in the United States alone (Mead et al. 1999). Several outbreaks of E. coli O157:H7 infection have been associated with recreational and municipal drinking water in North America, United Kingdom, and Japan (Bopp et al. 2003; Hrudey et al. 2003). Current methods to detect E. coli O157:H7 in water and food are traditional enrichment and plating on Sorbitol MacConkey agar and Rainbow agar selective media, Polymerase chain reaction (PCR), and other immunological methods (Bennett et al. 1996; Manafi and Kremsmaier 2001). The main drawbacks of these methods include time requirement (24–48 h for culture), difficulty in isolating DNA from sample (for PCR) and low sensitivity. It is important to note that low colony forming units (CFU) of E. coli O157:H7 present in contaminated food and water is generally sufficient to cause a severe infection, therefore having a sensitive method for detection during investigations of outbreaks is vital.
A highly sensitive BsMAb-based immunodetection assay was developed by our laboratory for the detection of E. coli O157:H7 in water samples (Guttikonda et al. 2007). E. coli O157:H7 whole bacteria and E. coli O157:H7 lipopolysaccharide (LPS) were used to first generate a monoclonal antibody, the hybridoma of which, was fused with anti-HRPO secreting monoclonal antibody hybridoma (Kreutz et al. 1998; Suresh et al. 1986b) to generate a quadroma producing BsMAb specific for both E. coli O157 and HRPO. The BsMAb was subsequently purified using benzhydroxamicacid agarose column (Husereau and Suresh 2001) and used in sandwich ELISA immunoassay. The anti-E. coli O157:H7 monoclonal antibody was used as the capture antibody to bind the bacteria from samples and the BsMAb was used as the detection antibody (Guttikonda et al. 2007). Refer to Fig. 19.3 for the general assay format. The detection limits of the assay were found to be 100 and 750 CFU/ml of sample for tap water and lake water, respectively. The immunoassay was further adapted to an immunofilter assay format to suit public health applications such as in water testing laboratories (Guttikonda et al. 2007). As low as 50 CFU of E. coli O157:H7/100 ml water were detected indicating that the assay is highly sensitive. Moreover the assay is highly specific since it did not detect a 500-fold excess of other bacterial strains such as Salmonella, Pseudomonas, and as well non-O157:H7 and non-pathogenic E. coli. A higher signal to noise ratio and a clean background was achieved in the assay since BsMAb served as a high specific activity probe. The BsMAb-based immunodetection assay therefore functions as a robust, ultrasensitive, and quick method for the detection of E. coli O157:H7. It has distinct advantages as it eliminates the amplification step required by other current assays and could easily be developed as a routine screening assay for detection of E. coli O157:H7 in water bodies especially in developing countries.
19.3.1.3 Bordetella pertussis
Whooping cough or pertussis caused by the bacterium Bordetella pertussis has become a major health concern in recent years especially among the adolescent age group (CDCP 2002, Centers for Disease Control and Prevention). Early and accurate diagnosis is critical in order to prevent the spread of infection and also ensure proper treatment of the affected individual. Conventional diagnosis of B. pertussis infection involves identification of the bacterium from culture of clinical nasopharyngeal aspirate samples, which generally takes about 3–7 days (Josephs 2000). Moreover, successful isolation and characterization is in turn dependent on several other factors such as proper specimen collection from the respiratory tract, storage, and culture conditions (Gustafsson et al. 1988). Another method for detection of B. pertussis involves the use of direct fluorescent-antibody assay that employs a fluorescence-labeled monoclonal antibody directed against a predominant antigenic LPS molecule present on the outer membrane of the bacterium (McNicol et al. 1995; Peppler 1984). Although detection of LPS is a good strategy, the assay is not sensitive and is also not easy to perform (Tilley et al. 2000).
Our laboratory therefore developed a highly sensitive and simple BsMAb-based immunodiagnostic assay for the detection of whole B. pertussis and soluble B. pertussis LPS (Tang et al. 2004). The assay is useful not only for analyzing clinical samples but also for immunochemical structural studies and serological characterization of B. pertussis LPS. The anti-B. pertussis LPS monoclonal antibody secreting hybridoma and the anti-HRPO monoclonal antibody secreting hybridoma were fused to generate a quadroma that produces BsMAb specific to both B. pertussis LPS and HRPO. BsMAb was subsequently purified by affinity chromatography using benzhydroxamicacid agarose column (Husereau and Suresh 2001) and used in a homosandwich ELISA immunoassay. Heat-killed B. pertussis BP347 by itself or spiked into nasopharyngeal aspirates was first bound by the anti-LPS specific monoclonal antibody, and then the BsMAb was added as the detection antibody (Tang et al. 2004). Refer to Fig. 19.3 for the general assay format. The assay showed high sensitivity with a practical lower limit of detection of ~5 CFU; the extrapolated theoretical lower limit of detection was found to be one bacterium by using the mean + 2 standard deviations of 20 control assays without B. pertussis. Interestingly, binding of B. pertussis to the anti-B. pertussis LPS monoclonal antibody-coated solid phase was found to be irreversible despite extensive washing suggesting a unique molecular velcro effect (Tang et al. 2004). The use of BsMAb in the immunoassay allowed ultrasensitive detection of B. pertussis since it avidly captured multiple exposed LPS molecules on the bacterial surface.
The BsMAb-based immunodiagnostic assay was adapted to an immunoswab format to facilitate easy, rapid, and point of care detection of B. pertussis in a primary health care setting. The sensitivity of detection was high since as few as ten bacteria could be detected compared to the controls (Tang et al. 2004). The BsMAb-based assay has unique advantages in being highly sensitive and easy to perform. It therefore facilitates early detection of B. pertussis infection and accurate monitoring of outbreaks of whooping cough.
19.3.2 Diagnosis of Viral Infections
19.3.2.1 Severe Acute Respiratory Syndrome Coronavirus
Severe acute respiratory syndrome (SARS) epidemic affected more than 8,000 people worldwide spreading over 30 countries across 5 continents in the 2002–2003 outbreak (Drosten et al. 2003; Peiris et al. 2003; Poon et al. 2004b). This highly contagious infection claimed over 900 lives in a short period of time with a fatality rate of 9.6%, emerging as a huge global threat to human health. SARS Coronavirus (SARS-CoV) is the etiological agent of SARS, which is believed to have transmitted from wild animals to the human population (Guan et al. 2003; Wang et al. 2006). According to WHO, the absence of a rapid screening test delayed the diagnosis of suspected cases of SARS and resulted in the spread of the disease worldwide. Current methods for the confirmation of SARS infection include detection of viral RNA by reverse transcription-PCR (Jiang et al. 2004; Poon et al. 2004a; Yam et al. 2003), detection of SARS-CoV antibodies in body fluids using indirect fluorescence assay (Chan et al. 2004), and isolation of SARS-CoV from clinical samples (Keyaerts et al. 2005; Yamashita et al. 2005). Since viral culture is a time consuming, tedious, and insensitive method, PCR and antibody detection methods are widely used; however, these two methods are expensive, laborious, and require technical expertise (Wu et al. 2004). A simple, rapid and inexpensive diagnostic test for the specific and early detection of SARS-CoV is therefore extremely important to limit the spread of infection and for proper risk management in the case of a future global outbreak especially since SARS has high rates of transmission and mortality.
Our laboratory has developed a highly sensitive, rapid, and simple BsMAb-based immunoswab assay for early detection of SARS-CoV (Kammila et al. 2008). The assay is designed to detect the most abundant and conserved viral antigen nucleocapsid protein NP (Di et al. 2005; Hiscox et al. 1995; Lau et al. 2004; Rota et al. 2003; Suresh et al. 2008) because its presence in different body fluids (serum, urine, nasopharyngeal aspirate, throat wash samples, and saliva) is suggestive of current infection. Three different monoclonal antibodies that recognize different epitopes on NP antigen and the anti-HRPO monoclonal antibody were employed to generate the BsMAb using hybrid-hybridoma technology. The obtained anti-SARS-CoV × anti-HRPO BsMAb was then purified by a novel, dual sequential affinity chromatography method (Protein-G column followed by m-aminophenyleboronic acid agarose column), which was developed by our laboratory (Bhatnagar et al. 2008). In the immunoswab assay, easy-to-use swabs were first coated with anti-SARS-CoV monoclonal antibody to capture NP in the test sample followed by detection with BsMAb (Kammila et al. 2008). Refer to Fig. 19.3 for the general assay format. The assay successfully detected SARS-CoV NP antigen spiked in different matrices such as saline, serum, and pig nasopharyngeal aspirate with high sensitivity. Pig nasopharyngeal aspirate was used as surrogate to human samples to test the ability of the immunoswab assay to detect low concentrations of NP antigen. The immunoswab assay showed NP detection limits of 10 pg/mL (1 pg/swab) in saline, 20–200 pg/mL (1–10 pg/swab) in pig nasopharyngeal aspirate and 500 pg/mL (25 pg/swab) in rabbit serum. Further, the sensitivity of NP detection was high in BsMAb-based assay compared to a parallel MAb-based assay (20 pg/mL vs. 200 pg/mL in saline; 20–200 pg/mL vs. 200 pg/mL in pig nasopharyngeal aspirate) indicating that the BsMAb-based immunoassay works better than its MAb-based counterpart. Furthermore to determine the robustness of the assay, swabs pre-coated with capture antibody were tested after storage for 2-, 6-, 10-, and 14-week time periods under different conditions (Kammila et al. 2008). The BsMAb-based immunoswabs showed good sensitivity for NP detection even on week 14 at 200 pg/mL (4°C storage) and 500 pg/mL (RT and −20°C storage) indicating a good shelf-life for the immunoswabs.
The immunoswab format has potential advantages particularly in clinical, rural, and primary healthcare settings such as ease of use, early phase detection, and in limiting the spread of infection. It is also extremely useful for SARS screening at all ports of mass human entry (airports, seaports, bus, train, and border stations). Interestingly, the time required to perform the assay was approximately 45 min, which make it a rapid test for SARS diagnosis (Kammila et al. 2008). The assay can easily be used to screen numerous suspected individuals within a short period of time during a future SARS outbreak given the relative ease of accessing nasopharyngeal aspirate with no invasive procedures. The BsMAb-based immunoswab detection of SARS-CoV NP antigen therefore serves as a simple point of care diagnostic test compared to other current methods (Di et al. 2005) and is also highly sensitive, inexpensive, and requires minimally trained personnel.
19.3.2.2 Dengue Virus
Dengue fever caused by Dengue virus is the most prevalent mosquito-borne viral infection in the world as more than 100 million cases are reported each year predominantly in the tropical and sub-tropical regions (Hemungkorn et al. 2007). Dengue virus belongs to the Flaviviridae family and four different serotypes (DENV1, DENV2, DENV3, and DENV4) have been identified so far. In humans, dengue viral infection causes a spectrum of diseases ranging from asymptomatic infection to severe hemorrhagic fever ultimately resulting in death (Hemungkorn et al. 2007). Diagnosis of dengue infection based on clinical symptoms cannot be deemed reliable, and therefore detection of the specific virus, viral antigen, genomic sequence, and/or antibodies is absolutely essential to confirm infection. Current methods to diagnose dengue infection include virus isolation, and other serological and molecular techniques that employ monoclonal or polyclonal antibodies labeled with an enzymatic or fluorometric marker (Shu and Huang 2004). These methods are less reliable, and moreover those that identify the virus or the viral genome are expensive and require specialized laboratories. It is important to diagnose an on-going or recent infection during the acute or early convalescent stages in order to facilitate better treatment, and ensure effective etiological investigation and disease control (Halstead 2007). Currently there is no sensitive, simple, and inexpensive diagnostic assay available for the detection of dengue virus infection at the acute or early stages.
Our laboratory has developed a novel, highly sensitive immunodiagnostic assay for the detection of Dengue virus using BsMAb (Ganguly and Suresh 2010, University of Alberta, Unpublished data). Only a general outline of the developed BsMAb-based immunodiagnostic assay is described here. To design the immunoassay, any specific Dengue virus antigen can be used to generate BsMAb that could be employed in a simple strip or swab assay format. The selected Dengue virus antigen is used to first generate a monoclonal antibody and in the subsequent step, the hybridoma secreting the monoclonal antibody is fused with another hybridoma secreting monoclonal antibody specific for HRPO to produce a quadroma producing the desired BsMAb. The BsMAb is subsequently purified by affinity chromatography using m-aminophenylboronic acid agarose column (Bhatnagar et al. 2008). The general format of the immunodiagnostic assay involves coating Dengue virus antigen-specific monoclonal antibody as the capture antibody on calcium alginate tipped swabs with aluminum/or plastic shafts as per previously published protocol (Tang et al. 2004). The swab is then blocked and later incubated with the specific antigen spiked in serum, after which, the purified BsMAb is used as the detection antibody. Addition of the HRPO substrate, TMB, results in the formation of blue color that can be identified visually (Refer to Fig. 19.3 for the general assay format).
The BsMAb-based immunodiagnostic assay for Dengue virus detection has several advantages. The assay is highly specific and easy to perform since it does not require any technical expertise or sophisticated instruments. In addition, the design of the assay makes it rapid and convenient as a point of care detection tool apt for use in primary health care settings and remote villages. These features make the assay very suitable for early detection of dengue infection and thereby control its spread in the community.
19.4 BsMAb for Diagnosis of Cancer
In addition to their un-controlled growth and aberrant cellular physiology, cancerous cells are often characterized by the presence of over-expressed biochemical molecules such as glycoproteins that are present on the cell surface and later shed into body fluids. Such over-expressed tumor-specific antigens have been exploited as markers to enable diagnosis, and in conjunction with a battery of clinical methods can also be of prognostic relevance. Based on specific tumor-associated antigens (TAA), BsMAb can be generated for use in cancer diagnostics (Songsivilai and Lachmann 1990; Souriau and Hudson 2003). Such BsMAb would bind to the corresponding cancer-specific antigen in the test sample and provide an easy read-out regarding the presence of a specific type of cancer. It is becoming more and more apparent that early and confirmative diagnosis of cancer is critical for the control and cure of the disease. Due to their distinct characteristics of being powerful immunoprobes, BsMAb are extremely valuable in developing simple, rapid, and highly sensitive immunodiagnostic assays that can be used for the detection of various types of cancer. The following sections describe the use of BsMAb in detection and diagnostic imaging of cancer.
19.4.1 Prostate Cancer
Prostate cancer is most common in men and is responsible for more deaths than any other cancer, except for lung cancer (NCI 2010, National Cancer Institute Statistics). About 218,890 new cases of prostate cancer were diagnosed in the United States alone during 2007. It is expected that 1 out of 6 men will be diagnosed with prostate cancer during their lifetime; a little over 1.8 million men in the United States are survivors of prostate cancer (NCI 2010, National Cancer Institute Statistics). Prostate-specific antigen (PSA) is a useful tumor-associated marker present in the serum that is widely used for screening and monitoring progression of prostate cancer (Caplan and Kratz 2002). There are several different assays currently available for the measurement of PSA, most of which involve the use of labeled monoclonal or polyclonal antibodies (Armbruster 1993; Cattini et al. 1993; Khosravi et al. 1995; Klee et al. 1994; Leinonen et al. 1993; Oesterling et al. 1995; Vihko et al. 1990; Yu and Diamandis 1993). These assays are technically complex, time consuming, and have lower sensitivity.
Our laboratory therefore developed a novel, highly sensitive, and rapid BsMAb-based immunoassay for the measurement of PSA (Kreutz and Suresh 1997). The anti-PSA monoclonal antibody secreting hybridoma was fused with anti-HRPO secreting hybridoma using the hybrid-hybridoma technology to generate a quadroma producing the anti-PSA × anti-HRPO BsMAb. The BsMAb was then purified by ammonium sulfate precipitation, anion exchange, and affinity chromatography, after which, it was used in the PSA immunoassay. The anti-PSA monoclonal antibody was used as the capture antibody and the BsMAb was used as the detection antibody to measure PSA levels in the test samples in a 20-min single-step assay (Fig. 19.4). The assay had high analytical sensitivity even with a short substrate incubation time; the detection limit was comparable to most commercially available assays requiring longer incubation times (Kreutz and Suresh 1997). With TMB as the enzyme substrate, a sensitivity of 0.028 mg/L was achieved for 5-min substrate incubation in comparison to the commercially available Hybritech Tandem-EIAR PSA assay that had a detection limit of 0.1 mg/L for 30-min substrate incubation. The developed assay was further evaluated using 138 clinical samples and results were found to correlate with those obtained by an automated Hybritech enzyme PSA immunoassay (Kreutz and Suresh 1997). Overall, the BsMAb-based immunoassay for PSA measurement has rapid kinetics and an excellent detection limit, which makes it a good candidate for use in the development of next-generation automated immunoassays and for rapid screening in health clinics.
Schematic representation of antibody complex formed during BsMAb-based immunoassay for PSA detection. PSA in the test sample is bound first by the capture monoclonal antibody and then by BsMAb detection antibody tagged to peroxidase (HRPO) to form an antibody sandwich complex. The diagram is adapted from Kreutz and Suresh, Clinical Chemistry, 1997
19.4.2 Cancer Diagnostic Imaging
Molecular imaging has transformed the field of cancer diagnosis with its superior ability to identify and localize cancer based on distinct molecular and functional characteristics of cancerous tissue. 18F-flurodeoxyglucose (18F-FDG)-based imaging using positron emission tomography (PET) or computed tomography (CT) has become popular for the detection and assessment of different types of tumors. Various specific monoclonal antibodies directed against different cancer antigens have also been employed; however, the sensitivity of these techniques is low compared to 18F-FDG-PET/CT. In theory, monoclonal antibodies should have been more ideal imaging candidates owing to their higher degree of specificity for tumor antigens and their ability to discriminate between tumor and inflammation. However, the high molecular weight of the radiolabeled monoclonal antibodies limits tumor uptake and causes insufficient clearance from surrounding tissues resulting in low contrast during imaging. The size also interferes with the ability of these molecules to extravasate from the vascular channels into the extravascular space thus leading to slow accretion of radiolabeled antibodies in tumors (typically 1–3 days to achieve maximum tumor uptake). While tumor uptake of radiolabeled monoclonal antibodies may reach between 10 and 30% of injected dose per gram of tumor in mouse xenograft models, there may only be an accretion of <0.1% injected dose per gram of tumor in humans owing to a larger vascular and extravascular volume of distribution. Although several antibody modifications have been made along with changes to the radionuclide moiety in order to obtain better signal to noise ratios and avoid non-specific tissue uptake by liver, kidneys, and bone marrow, none of them have yielded expected results.
In recent times, BsMAb have proven to be more useful in cancer diagnostic imaging especially using the “pre-targeting” strategy (Cardillo et al. 2004; Gold et al. 2008; Goldenberg et al. 2006, 2007; Rearden et al. 1983, 1985; Sharkey et al. 2007). This strategy aims to deliver high tumor accretion, eliminate background noise due to untargeted radioactivity from blood and normal tissues, and reduce unintended toxicity. It relies on BsMAb’s ability to effect tumor localization of the subsequently administered radiolabeled effector molecule. Targeting is achieved with BsMAb that binds to a target antigen with one arm and to a radiometal-chelate or hapten peptide complex (effector molecule) with the other arm. Animal model experiments have revealed an equivalent tumor uptake of BsMAb compared to radiolabeled antibodies and maximum accretion within minutes rather than several hours or days. Even the radionuclide was cleared very rapidly from the body, with more than 80% of the product eliminated in the urine within a few hours, allowing tumor/blood and tissue ratios to often be ≥10:1 within 1 h of the radionuclide administration. Tissue retention of the radiolabeled effector molecule was also found to be very low, even in the kidneys and liver that very often show elevated uptake of directly radiolabeled antibodies unless radioiodine is used. The use of BsMAb has significantly enhanced the imaging utility of pre-targeting procedures as compared to using directly radiolabeled antibodies. The de-coupling of the effector molecule from the pre-targeting agent is central to all the variations on this theme that has resulted in enhanced imaging of tumors.
BsMAb can be used in a simple two-step pre-targeting approach without the need for any clearing step or additional agents. Two-step procedures generally involve injection of the pre-targeting agent such as BsMAb and waiting for a day or two before all of the unbound fractions are drained off from the body’s circulation by excretion through liver or kidneys (BsMAb are easily cleared from the blood within a day). This is followed by administration of the radiolabeled effector molecule, which would only bind to a specific arm on the pre-targeted BsMAb at the tumor site. Patients would therefore be able to receive BsMAb injection by their oncologist, return a few days later and receive the radiolabeled product in a nuclear medicine facility such that imaging can be accomplished on the same day. Although it may take a few days before an image can be achieved using a pre-targeting approach, experienced investigators and preclinical data have suggested that the images would be superior in terms of specificity, sensitivity, signal intensity, and have minimal background compared to those obtained using radiolabeled monoclonal antibodies. In many cases, BsMAb-based pre-targeting approach has out-performed the results generated by clinically approved radiolabeled monoclonal antibodies, especially in imaging small tumors in colorectal and colonic cancer (Sharkey et al. 2005). In addition to giving better tumor/blood ratios, superior tumor uptake, enhanced tumor/non tumor ratios, the pre-targeted strategy retained tumor-specific signal intensity even 1 day post-injection of the radioactive effector molecule thus providing a 15-fold increase in signal strength at the tumor site. BsMAb are currently being exploited for imaging many CEA-expressing tumors, MUC-1-expressing pancreatic cancer, and CD20-expressing non-Hodgkin’s lymphoma (Peltier et al. 1993; Schuhmacher et al. 2001a, b).
BsMAb-based pre-targeting techniques for diagnostic imaging of cancers have taken nuclear imaging to a whole new level and are beginning to complement the present-day gold standard of 18F-FDG-PET. BsMAb are being further engineered to achieve optimal molecular weight and charge for better tumor uptake, rapid blood clearance, higher valency, improved affinity to TAA, enhanced signal intensity, and greater flexibility for binding to a variety of hapten-peptides carrying different radio-isotopes. Improvements in the methods used for the production of BsMAb by “Dock and Lock” molecular engineering strategies and their application in furthering pre-targeting applications in tumor imaging and therapy is described in Chap. 12. Given that highly specific and sensitive images are possible with BsMAb pre-targeting in both the experimental and clinical set up, it is evident that BsMAb-based cancer diagnostic imaging is very promising.
19.5 Conclusion
The use of BsMAb in immunodiagnostic assays has resulted in the development of next generation immunoassays that are highly sensitive, rapid, simple, and cost-effective. The specificity of the assays approaches the theoretical limit of immunodetection making them ultrasensitive. Importantly, these assays are invaluable as a point of care diagnostic tool. Such assays are of immense value especially in some resource-constrained countries to combat the spread of diseases. Rapid detection of communicable diseases has huge impact on the current global health scenario where an infectious disease can make quick transition from an epidemic to a pandemic like the recent outbreak of swine flu. Most of the current diagnostic assays measure specific antibodies to bacterial or viral antigens and therefore may report a previous infection since antibodies circulate in the blood 6 months post-infection. Such assays rarely detect infection at initial stages making early intervention almost impossible. In contrast, BsMAb-based diagnostics measure specific bacterial or viral antigens rather than the antibodies and therefore accurately reflect active diseased state and make early-stage detection possible.
In the coming years, BsMAb will prove valuable for use in diagnosis of different types of cancer. Since BsMAb-based cancer diagnosis has many advantages and is highly sensitive it will be useful not only for early detection of cancer but also convenient for monitoring the progression of the diseased state and assessing response to treatment. Given the immense potential of BsMAb as excellent immunoprobes, there are efforts to engineer newer forms of these antibodies with significantly improved binding specificity and avidity. BsMAb await a plethora of novel applications in the field of diagnostics.
References
Armbruster DA (1993) Prostate-specific antigen: biochemistry, analytical methods, and clinical application. Clin Chem 39(2):181–195
Bennett AR, MacPhee S, Betts RP (1996) The isolation and detection of Escherichia coli O157 by use of immunomagnetic separation and immunoassay procedures. Lett Appl Microbiol 22(3):237–243
Bhatnagar PK, Das D, Suresh MR (2008) Sequential affinity purification of peroxidase tagged bispecific anti-SARS-CoV antibodies on phenylboronic acid agarose. J Chromatogr B Analyt Technol Biomed Life Sci 863(2):235–241
Bopp DJ, Sauders BD, Waring AL, Ackelsberg J, Dumas N, Braun-Howland E, Dziewulski D, Wallace BJ, Kelly M, Halse T, Musser KA, Smith PF, Morse DL, Limberger RJ (2003) Detection, isolation, and molecular subtyping of Escherichia coli O157:H7 and Campylobacter jejuni associated with a large waterborne outbreak. J Clin Microbiol 41(1):174–180
Campos M, Quartin A, Mendes E, Abreu A, Gurevich S, Echarte L, Ferreira T, Cleary T, Hollender E, Ashkin D (2008) Feasibility of shortening respiratory isolation with a single sputum nucleic acid amplification test. Am J Respir Crit Care Med 178(3):300–305
Cao Y, Suresh MR (1998) Bispecific antibodies as novel bioconjugates. Bioconjug Chem 9(6):635–644
Caplan A, Kratz A (2002) Prostate-specific antigen and the early diagnosis of prostate cancer. Am J Clin Pathol 117(Suppl):S104–S108
Cardillo TM, Karacay H, Goldenberg DM, Yeldell D, Chang CH, Modrak DE, Sharkey RM, Gold DV (2004) Improved targeting of pancreatic cancer: experimental studies of a new bispecific antibody, pretargeting enhancement system for immunoscintigraphy. Clin Cancer Res 10(10):3552–3561
Cattini R, Cooksey M, Robinson D, Brett G, Bacarese-Hamilton T, Jolley N (1993) Measurement of alpha-fetoprotein, carcinoembryonic antigen and prostate-specific antigen in serum and heparinised plasma by enzyme immunoassay on the fully automated serono SR1 analyzer. Eur J Clin Chem Clin Biochem 31(8):517–524
CDCP (2002) Centers for Disease Control and Prevention. Pertussis 1997–2000. Morb Mortal Wkly Rep Surveill Summ 51:73–76
Chan PK, Ng KC, Chan RC, Lam RK, Chow VC, Hui M, Wu A, Lee N, Yap FH, Cheng FW, Sung JJ, Tam JS (2004) Immunofluorescence assay for serologic diagnosis of SARS. Emerg Infect Dis 10(3):530–532
Cole ST, Brosch R, Parkhill J, Garnier T, Churcher C, Harris D, Gordon SV, Eiglmeier K, Gas S, Barry CE 3rd, Tekaia F, Badcock K, Basham D, Brown D, Chillingworth T, Connor R, Davies R, Devlin K, Feltwell T, Gentles S, Hamlin N, Holroyd S, Hornsby T, Jagels K, Krogh A, McLean J, Moule S, Murphy L, Oliver K, Osborne J, Quail MA, Rajandream MA, Rogers J, Rutter S, Seeger K, Skelton J, Squares R, Squares S, Sulston JE, Taylor K, Whitehead S, Barrell BG (1998) Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 393(6685):537–544
Das D, Suresh MR (2005) Producing bispecific and bifunctional antibodies. Methods Mol Med 109:329–346
Di B, Hao W, Gao Y, Wang M, Wang YD, Qiu LW, Wen K, Zhou DH, Wu XW, Lu EJ, Liao ZY, Mei YB, Zheng BJ, Che XY (2005) Monoclonal antibody-based antigen capture enzyme-linked immunosorbent assay reveals high sensitivity of the nucleocapsid protein in acute-phase sera of severe acute respiratory syndrome patients. Clin Diagn Lab Immunol 12(1):135–140
Drosten C, Gunther S, Preiser W, van der Werf S, Brodt HR, Becker S, Rabenau H, Panning M, Kolesnikova L, Fouchier RA, Berger A, Burguiere AM, Cinatl J, Eickmann M, Escriou N, Grywna K, Kramme S, Manuguerra JC, Muller S, Rickerts V, Sturmer M, Vieth S, Klenk HD, Osterhaus AD, Schmitz H, Doerr HW (2003) Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med 348(20):1967–1976
Fraser ME, Fujinaga M, Cherney MM, Melton-Celsa AR, Twiddy EM, O’Brien AD, James MN (2004) Structure of shiga toxin type 2 (Stx2) from Escherichia coli O157:H7. J Biol Chem 279(26):27511–27517
Gold DV, Goldenberg DM, Karacay H, Rossi EA, Chang CH, Cardillo TM, McBride WJ, Sharkey RM (2008) A novel bispecific, trivalent antibody construct for targeting pancreatic carcinoma. Cancer Res 68(12):4819–4826
Goldenberg DM, Sharkey RM, Paganelli G, Barbet J, Chatal JF (2006) Antibody pretargeting advances cancer radioimmunodetection and radioimmunotherapy. J Clin Oncol 24(5):823–834
Goldenberg DM, Chatal JF, Barbet J, Boerman O, Sharkey RM (2007) Cancer imaging and therapy with bispecific antibody pretargeting. Update Cancer Ther 2(1):19–31
Griffin PM, Tauxe RV (1991) The epidemiology of infections caused by Escherichia coli O157:H7, other enterohemorrhagic E. coli, and the associated hemolytic uremic syndrome. Epidemiol Rev 13:60–98
Guan Y, Zheng BJ, He YQ, Liu XL, Zhuang ZX, Cheung CL, Luo SW, Li PH, Zhang LJ, Guan YJ, Butt KM, Wong KL, Chan KW, Lim W, Shortridge KF, Yuen KY, Peiris JS, Poon LL (2003) Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science 302(5643):276–278
Gustafsson B, Lindquist U, Andersson M (1988) Production and characterization of monoclonal antibodies directed against Bordetella pertussis lipopolysaccharide. J Clin Microbiol 26(2):188–193
Guttikonda S, Tang XL, Yang BM, Armstrong GD, Suresh MR (2007) Monospecific and bispecific antibodies against E. coli O157 for diagnostics. J Immunol Methods 327(1–2):1–9
Halstead SB (2007) Dengue. Lancet 370(9599):1644–1652
Hemungkorn M, Thisyakorn U, Thisyakorn C (2007) Dengue infection: a growing global health threat. Biosci Trends 1(2):90–96
Hiscox JA, Cavanagh D, Britton P (1995) Quantification of individual subgenomic mRNA species during replication of the coronavirus transmissible gastroenteritis virus. Virus Res 36(2–3):119–130
Hrudey SE, Payment P, Huck PM, Gillham RW, Hrudey EJ (2003) A fatal waterborne disease epidemic in Walkerton, Ontario: comparison with other waterborne outbreaks in the developed world. Water Sci Technol 47(3):7–14
Husereau DR, Suresh MR (2001) A general affinity method to purify peroxidase-tagged antibodies. J Immunol Methods 249(1–2):33–41
Jiang SS, Chen TC, Yang JY, Hsiung CA, Su IJ, Liu YL, Chen PC, Juang JL (2004) Sensitive and quantitative detection of severe acute respiratory syndrome coronavirus infection by real-time nested polymerase chain reaction. Clin Infect Dis 38(2):293–296
Josephs JE (2000) Pertussis in the adolescent and adult: a primary care concern. Clin Excell Nurse Pract 4(6):361–365
Kammila S, Das D, Bhatnagar PK, Sunwoo HH, Zayas-Zamora G, King M, Suresh MR (2008) A rapid point of care immunoswab assay for SARS-CoV detection. J Virol Methods 152(1–2):77–84
Keyaerts E, Vijgen L, Maes P, Neyts J, Van Ranst M (2005) Growth kinetics of SARS-coronavirus in Vero E6 cells. Biochem Biophys Res Commun 329(3):1147–1151
Khosravi MJ, Papanastasiou-Diamandi A, Mistry J (1995) An ultrasensitive immunoassay for prostate-specific antigen based on conventional colorimetric detection. Clin Biochem 28(4):407–414
Klee GG, Preissner CM, Oesterling JE (1994) Development of a highly sensitive immunochemiluminometric assay for prostate-specific antigen. Urology 44(1):76–82
Kohler G, Milstein C (1975) Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 256(5517):495–497
Kreutz FT, Suresh MR (1997) Novel bispecific immunoprobe for rapid and sensitive detection of prostate-specific antigen. Clin Chem 43(4):649–656
Kreutz FT, Xu DZ, Suresh MR (1998) A new method to generate quadromas by electrofusion and FACS sorting. Hybridoma 17(3):267–273
Kricka LJ (1994) Selected strategies for improving sensitivity and reliability of immunoassays. Clin Chem 40(3):347–357
Lalvani A, Millington KA (2008) Screening for tuberculosis infection prior to initiation of anti-TNF therapy. Autoimmun Rev 8(2):147–152
Lau SK, Woo PC, Wong BH, Tsoi HW, Woo GK, Poon RW, Chan KH, Wei WI, Peiris JS, Yuen KY (2004) Detection of severe acute respiratory syndrome (SARS) coronavirus nucleocapsid protein in sars patients by enzyme-linked immunosorbent assay. J Clin Microbiol 42(7):2884–2889
Law D (2000) Virulence factors of Escherichia coli O157 and other Shiga toxin-producing E. coli. J Appl Microbiol 88(5):729–745
Leinonen J, Lovgren T, Vornanen T, Stenman UH (1993) Double-label time-resolved immunofluorometric assay of prostate-specific antigen and of its complex with alpha 1-antichymotrypsin. Clin Chem 39(10):2098–2103
Liu F, Guttikonda S, Suresh MR (2003) Bispecific monoclonal antibodies against a viral and an enzyme: utilities in ultrasensitive virus ELISA and phage display technology. J Immunol Methods 274(1–2):115–127
Madariaga MG, Jalali Z, Swindells S (2007) Clinical utility of interferon gamma assay in the diagnosis of tuberculosis. J Am Board Fam Med 20(6):540–547
Manafi M, Kremsmaier B (2001) Comparative evaluation of different chromogenic/fluorogenic media for detecting Escherichia coli O157:H7 in food. Int J Food Microbiol 71(2–3):257–262
McNicol P, Giercke SM, Gray M, Martin D, Brodeur B, Peppler MS, Williams T, Hammond G (1995) Evaluation and validation of a monoclonal immunofluorescent reagent for direct detection of Bordetella pertussis. J Clin Microbiol 33(11):2868–2871
Mead PS, Slutsker L, Griffin PM, Tauxe RV (1999) Food-related illness and death in the United States reply to Dr. Hedberg. Emerg Infect Dis 5(6):841–842
Milstein C, Cuello AC (1983) Hybrid hybridomas and their use in immunohistochemistry. Nature 305(5934):537–540
NCI (2010) Key statistics about prostate cancer. http://www.cancer.org/Cancer/ProstateCancer/DetailedGuide/prostate-cancer-key-statistics. Cited on 23 July 2010
Oesterling JE, Moyad MA, Wright GL Jr, Beck GR (1995) An analytical comparison of the three most commonly used prostate-specific antigen assays: Tandem-R, Tandem-E, and IMx. Urology 46(4):524–532
Palma-Nicolas JP, Bocanegra-Garcia V (2007) Innovative strategies to diagnose and monitor tuberculosis patients. Arch Bronconeumol 43(4):225–232
Peiris JS, Lai ST, Poon LL, Guan Y, Yam LY, Lim W, Nicholls J, Yee WK, Yan WW, Cheung MT, Cheng VC, Chan KH, Tsang DN, Yung RW, Ng TK, Yuen KY (2003) Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 361(9366):1319–1325
Peltier P, Curtet C, Chatal JF, Le Doussal JM, Daniel G, Aillet G, Gruaz-Guyon A, Barbet J, Delaage M (1993) Radioimmunodetection of medullary thyroid cancer using a bispecific anti-CEA/anti-indium-DTPA antibody and an indium-111-labeled DTPA dimer. J Nucl Med 34(8):1267–1273
Peppler MS (1984) Two physically and serologically distinct lipopolysaccharide profiles in strains of Bordetella pertussis and their phenotype variants. Infect Immun 43(1):224–232
Poon LL, Chan KH, Wong OK, Cheung TK, Ng I, Zheng B, Seto WH, Yuen KY, Guan Y, Peiris JS (2004a) Detection of SARS coronavirus in patients with severe acute respiratory syndrome by conventional and real-time quantitative reverse transcription-PCR assays. Clin Chem 50(1):67–72
Poon LL, Guan Y, Nicholls JM, Yuen KY, Peiris JS (2004b) The aetiology, origins, and diagnosis of severe acute respiratory syndrome. Lancet Infect Dis 4(11):663–671
Rearden A, Nachtsheim DA, Frisman DM, Chiu P, Elmajian DA, Baird SM (1983) Altered cell surface antigen expression in bladder carcinoma detected by a new hemagglutinating monoclonal antibody. J Immunol 131(6):3073–3077
Rearden A, Taetle R, Elmajian DA, Majda JA, Baird SM (1985) Glycophorin A on normal and leukemia cells detected by monoclonal antibodies, including a new monoclonal antibody reactive with glycophorins A and B. Mol Immunol 22(4):369–378
Rota PA, Oberste MS, Monroe SS, Nix WA, Campagnoli R, Icenogle JP, Penaranda S, Bankamp B, Maher K, Chen MH, Tong S, Tamin A, Lowe L, Frace M, DeRisi JL, Chen Q, Wang D, Erdman DD, Peret TC, Burns C, Ksiazek TG, Rollin PE, Sanchez A, Liffick S, Holloway B, Limor J, McCaustland K, Olsen-Rasmussen M, Fouchier R, Gunther S, Osterhaus AD, Drosten C, Pallansch MA, Anderson LJ, Bellini WJ (2003) Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science 300(5624):1394–1399
Schuhmacher J, Kaul S, Klivenyi G, Junkermann H, Magener A, Henze M, Doll J, Haberkorn U, Amelung F, Bastert G (2001a) Immunoscintigraphy with positron emission tomography: gallium-68 chelate imaging of breast cancer pretargeted with bispecific anti-MUC1/anti-Ga chelate antibodies. Cancer Res 61(9):3712–3717
Schuhmacher J, Klivenyi G, Kaul S, Henze M, Matys R, Hauser H, Clorius J (2001b) Pretargeting of human mammary carcinoma xenografts with bispecific anti-MUC1/anti-Ga chelate antibodies and immunoscintigraphy with PET. Nucl Med Biol 28(7):821–828
Sharkey RM, Cardillo TM, Rossi EA, Chang CH, Karacay H, McBride WJ, Hansen HJ, Horak ID, Goldenberg DM (2005) Signal amplification in molecular imaging by pretargeting a multivalent, bispecific antibody. Nat Med 11(11):1250–1255
Sharkey RM, Karacay H, McBride WJ, Rossi EA, Chang CH, Goldenberg DM (2007) Bispecific antibody pretargeting of radionuclides for immuno single-photon emission computed tomography and immuno positron emission tomography molecular imaging: an update. Clin Cancer Res 13(18 Pt 2):5577s–5585s
Shu PY, Huang JH (2004) Current advances in dengue diagnosis. Clin Diagn Lab Immunol 11(4):642–650
Songsivilai S, Lachmann PJ (1990) Bispecific antibody: a tool for diagnosis and treatment of disease. Clin Exp Immunol 79(3):315–321
Souriau C, Hudson PJ (2003) Recombinant antibodies for cancer diagnosis and therapy. Expert Opin Biol Ther 3(2):305–318
Suresh MR (1991) Immunoassays for cancer-associated carbohydrate antigens. Semin Cancer Biol 2(6):367–377
Suresh MR, Cuello AC, Milstein C (1986a) Advantages of bispecific hybridomas in one-step immunocytochemistry and immunoassays. Proc Natl Acad Sci USA 83(20):7989–7993
Suresh MR, Cuello AC, Milstein C (1986b) Bispecific monoclonal antibodies from hybrid hybridomas. Methods Enzymol 121:210–228
Suresh MR, Bhatnagar PK, Das D (2008) Molecular targets for diagnostics and therapeutics of severe acute respiratory syndrome (SARS-CoV). J Pharm Pharm Sci 11(2):1s–13s
Tang XL, Peppler MS, Irvin RT, Suresh MR (2004) Use of bispecific antibodies in molecular velcro assays whose specificity approaches the theoretical limit of immunodetection for Bordetella pertussis. Clin Diagn Lab Immunol 11(4):752–757
Tilley PA, Kanchana MV, Knight I, Blondeau J, Antonishyn N, Deneer H (2000) Detection of Bordetella pertussis in a clinical laboratory by culture, polymerase chain reaction, and direct fluorescent antibody staining; accuracy, and cost. Diagn Microbiol Infect Dis 37(1):17–23
Vihko P, Kurkela R, Ramberg J, Pelkonen I, Vihko R (1990) Time-resolved immunofluorometric assay of human prostate-specific antigen. Clin Chem 36(1):92–95
Wang LF, Shi Z, Zhang S, Field H, Daszak P, Eaton BT (2006) Review of bats and SARS. Emerg Infect Dis 12(12):1834–1840
WHO (2010) World Health Organisation online report on infectious disease. http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_AnnexA.pdf. Cited on 22 June 2010
WHO-TB (2010) World Health Organisation online report on tuberculosis. http://www.who.int/mediacentre/factsheets/fs104/en/ Cited on 30 June 2010
Wu HS, Chiu SC, Tseng TC, Lin SF, Lin JH, Hsu YH, Wang MC, Lin TL, Yang WZ, Ferng TL, Huang KH, Hsu LC, Lee LL, Yang JY, Chen HY, Su SP, Yang SY, Lin SY, Lin TH, Su IS (2004) Serologic and molecular biologic methods for SARS-associated coronavirus infection, Taiwan. Emerg Infect Dis 10(2):304–310
Yam WC, Chan KH, Poon LL, Guan Y, Yuen KY, Seto WH, Peiris JS (2003) Evaluation of reverse transcription-PCR assays for rapid diagnosis of severe acute respiratory syndrome associated with a novel coronavirus. J Clin Microbiol 41(10):4521–4524
Yamashita M, Yamate M, Li GM, Ikuta K (2005) Susceptibility of human and rat neural cell lines to infection by SARS-coronavirus. Biochem Biophys Res Commun 334(1):79–85
Yu H, Diamandis EP (1993) Ultrasensitive time-resolved immunofluorometric assay of prostate-specific antigen in serum and preliminary clinical studies. Clin Chem 39(10):2108–2114
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Parashar, A., Sarkar, S., Ganguly, A., Sharma, S.K., Suresh, M.R. (2011). Bispecific Antibodies for Diagnostic Applications. In: Kontermann, R. (eds) Bispecific Antibodies. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-20910-9_19
Download citation
DOI: https://doi.org/10.1007/978-3-642-20910-9_19
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-20909-3
Online ISBN: 978-3-642-20910-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)