Abstract
Coral reef aorta is an uncommon syndrome caused by a distribution of rock-hard calcifications in the visceral part of the aorta. These heavily calcified plaques grow into the lumen and can cause significant stenoses, which may develop into visceral ischemia, renovascular hypertension, and malperfusion of the lower limbs. We report here our surgical experience in treating 138 patients.
The main symptoms were renovascular hypertension (69.5%), limb claudication (55%), and chronic visceral ischemia (31.1%).
One hundred thirty-five (97.8%) of the 138 patients were treated through vascular operations, including open thromboendarterectomy (TEA) of the aorta in an isolated suprarenal segment in 12 cases (8.8%) and the supra- and infrarenal aorta in 123 cases (91.1%). Aortic repair was performed with aortoaortic (n = 27), aortoiliac (n = 31), or aortofemoral (n = 35) bypass; 42 cases were treated instead with aortic patch repair. Visceral and renal arteries with atherosclerotic involvement were treated with TEA in 59 cases, and bypass reconstructions were performed in 20 cases.
Postoperative complications requiring corrective surgery occurred in 12 patients (8.8%). The overall rate of relevant complications was 25.9% (n = 35).
Coral reef aorta is a rare, unique disease of the juxta- and infrarenal aorta that is often associated with severe atherosclerotic disease in other domains. Surgical treatment offers good results, and a timely operation is advocated to avoid loss of kidney function, complications of long-standing hypertensive disease, and wasting from intestinal malperfusion.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
1 Introduction
Atherosclerotic occlusive disease of the aorta usually affects its distal portions, and calcifications and obstructions involving the suprarenal aorta are rare and mostly described in case reports [1, 2]. Coral reef aorta (CRA) is an uncommon syndrome caused by a distribution of rock-hard calcifications in the visceral part of the aorta [3]. These heavily calcified plaques that grow into the lumen can cause significant stenoses, which may develop into visceral ischemia, renovascular hypertension, and malperfusion of the lower limbs. Transaortic endarterectomy is accepted as the standard repair, and it is often performed through an extensive thoracoabdominal approach [4]. In the last decade, alternative management of CRA, such as endovascular and laparoscopic approach, has been proposed in order to reduce surgical invasiveness.
Our experience with the operative management of CRA was discussed earlier [5]. In this chapter, we describe the findings, operative procedure, and follow-up of 138 patients treated between 1993 and 2017. We focused on the early outcomes, long-term results, and the frequency of recurrent disease, with special emphasis on the visceral and renal arteries.
2 Materials and Methods
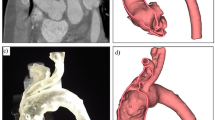
From January 1993 to June 2017, 138 patients (52 men, 86 women, mean age 62.5 years, range 45–86 years) underwent treatment for CRA. Data of patients were recorded and prospectively collected in a database. All patients who presented with the typical signs of CRA in the preoperative ultrasound examination were enrolled. According to our standard practice, patients with severe preoperative renal failure (serum creatinine >2.5 mg/dL) underwent noncontrast computed tomography (NCCT); all the others were studied with contrast computed tomography (CCT) and intra-arterial digital subtraction angiography (DSA). CRA is visualized in the NCCT and in the CCT as white intraluminal blocks in the visceral aorta, with a density comparable with the structure of the bone (Fig. 4.1).
A cloudy formation that narrows the visceral aorta to a very small lumen or total occlusion is the typical morphology of CRA during DSA (Fig. 4.2).
These characteristic signs on preoperative imaging were present in all cases.
Most patients presented with the typical risk factors for arteriosclerosis. Diabetes was found in 23.2% of the patients; heavy smoking (up to 40 cigarettes per day) was found in 70.2% and hypertension with more than two medications in 68.1%. Comorbidities such as tuberculosis, syphilis, or aortitis [6, 7] could not be detected in the study population. All patients underwent a thorough cardiological and neurological examination, including an electrocardiogram, transthoracic echocardiogram, chest X-ray, and Doppler and duplex ultrasound scans of the supra-aortic branches, arms, and limbs. In our experience, CRA is frequently associated with coronary artery disease (CAD) (44 pts., 31.8%); and for this reason, since 2010, all patients with CRA, without severe preoperative renal failure, have been subjected to ECG-gated angio-CT. When significant coronary artery lesions were present, angioplasty of the coronary arteries or coronary bypass surgery was performed before the aortic surgery. After discharge, all surviving patients were introduced in a follow-up protocol with regular clinical and ultrasound evaluation at 1 month, 6 months, and yearly thereafter.
2.1 Symptomatology and Findings
Depending on the extent of the disease and the aortic branches involved, three leading symptoms were found, of which the most frequent finding was renovascular arterial hypertension causing headache and vertigo. Ninety-six patients (69.5%) were found to take one (ten patients), two (21 patients), three (40 patients), or more than three (25 patients) medications to control arterial blood pressure. All the patients had developed either severe renal artery stenoses or stenosis of the suprarenal aorta due to protrusion of the coral reef-like calcifications. Intermittent claudication due to peripheral arterial occlusive disease was found in 76 patients (55.0%). The pain-free walking distance was less than 200 m (peripheral arterial occlusive disease Fontaine stage IIb) in 47 patients (34.0%). Forty-three patients (31.1%) presented with chronic visceral ischemia causing diarrhea, weight loss, and abdominal pain. Abdominal angina occurred in 32 of 43 patients (74.4%), and weight loss occurred in 38 of 43 patients (88.3%).
Preoperative examinations showed total occlusion of branches (n = 38; celiac trunk n = 8, superior mesenteric artery [SMA] n = 5, inferior mesenteric artery [IMA] n = 15, right renal artery [RRA] n = 7, left renal artery [LRA] n = 3) and heavily stenotic branches (n = 94; celiac trunk n = 21, SMA n = 17, IMA n = 27, RRA n = 17, LRA n = 12).
2.2 Surgical Procedure
One hundred thirty-five (97.8%) of the 138 patients underwent open surgery. Three patients with CRA noneligible for open surgery for severe comorbidities were treated endovascularly. All surgical procedures were performed under general anesthesia. The operative approach was a median laparotomy in 63 patients (46.6%), a bilateral subcostal laparotomy with medial visceral rotation in 29 patients (21.4%), and a left-sided thoracoabdominal approach in 43 patients (31.8%).
After an extensive exposure of the aorta and the visceral and renal vessels (Fig. 4.3), a thromboendarterectomy (TEA) of the aorta was performed in an isolated suprarenal segment in 12 cases (8.8%) and the supra- and infrarenal aorta in 123 cases (91.1%) (Fig. 4.4).
Due to the extension of the plaques into the distal aorta, a TEA of the aortic bifurcation was necessary in 34 patients (25.1%). Distal to the aortic bifurcation, a TEA of the iliac artery (unilateral n = 4, bilateral n = 8) was performed in 12 cases (8.8%). Blood flow was restored by TEA to the celiac trunk in 25 cases (21 stenosis, 4 total occlusion) (18.5%) and to the SMA in 17 cases (all stenosis) (12.5%).
Whenever possible, visceral vessels were selectively cannulated with occlusion/perfusion Pruitt catheter and perfused with cold crystalloid (Ringer 4 °C).
In three cases of total occlusion, CT was reimplanted with bypass; in one patient with long occlusion of the CT, with a valid collateral network from the SMA, the CT was ligated.
SMA was reimplanted with aortovisceral bypass in five cases of total occlusion.
TEA was performed in 17 cases (12.5%) of stenotic renal artery disease.
In 12 cases (8.8%) with heavily calcified stenosis, the origin of the renal artery was transversely cut and the renal artery reimplanted with a bypass. Renal artery revascularization was not performed in case of occlusion with contract kidney (n = 10).
Whenever possible, renal arteries were selectively cannulated with occlusion/perfusion Pruitt catheter and perfused. From 1993 to 2010, renal arteries were perfused with cold crystalloid (Ringer 4 °C), but since 2010, following initial encouraging results during thoracoabdominal open repair [8], histidine-tryptophan-ketoglutarate (Custodiol; Dr. Franz-Kohler Chemie GmbH, Bensheim, Germany) was used for renal protection during the procedure (Fig. 4.5).
Aortorenal and aortovisceral bypass were performed using Dacron grafts (n = 9) and polytetrafluoroethylene (PTFE) (n = 7), and after an initial experience during thoracoabdominal open surgery, since 2013 also the Gore Hybrid Vascular Graft (GHVG; W. L. Gore and Associates, Flagstaff, Ariz) has been used for vessel reimplantation (n = 4) [9].
Aortic repair was performed with aortoaortic (n = 27), aortoiliac (n = 31), or aortofemoral (n = 35) bypass with proximal beveled anastomosis on the visceral and renal vessels in the majority of cases (Fig. 4.6); 42 cases were treated instead with aortic patch repair (Fig. 4.7).
Intraoperative angiography at the end of the surgical procedure was performed in 43 cases (31.8%) in order to assess vessel patency in case of extensive TEA or bypass repair of heavily calcified stenosis. In 17 cases, additional simultaneous stenting was performed for persistent stenosis or intraluminal flap (n = 14) or in case of acute angulation of the aortovisceral and aortorenal distal anastomosis (n = 3).
3 Results
3.1 30-Day Results
Three patients (2.2%) died during or soon after surgery. One patient died from acute cardiac arrest during surgery. One patient died from cardiac arrest (postoperative day 4), and one patient died from multiorgan failure after a prolonged stay in the intensive care unit (postoperative day 22). Postoperative complications that required corrective surgery or additional endovascular procedure occurred in 12 patients (8.8%). The most significant problem was acute ischemia of the lower extremities, which required thrombectomy or femoropopliteal revascularization in five patients. One patient with thoraco-phreno-laparotomy was treated in the intensive care unit with pleural drainage due to prolonged pleural effusion. One patient undergone surgical revision for postoperative bleeding during postoperative day 2. One patient suffered from colon ischemia, which resulted in subtotal colectomy. In one case, acute occlusion after TEA of the aortic bifurcation was treated with aortobifemoral bypass. Three patients required additional endovascular procedures for postoperative complications. Two patients with acute renal failure during postoperative day 2 and 4 with acute renal artery occlusion documented by ultrasound were treated with endovascular recanalization and stenting. In one case, an angiography with additional stenting of CT was performed during postoperative day 2 for acute occlusion.
The overall rate of relevant complications was 25.9% (n = 35). Ten patients (7.4%) developed a major adverse cardiac event after surgery requiring coronary artery angioplasty in nine cases and medical treatment in one.
Other relevant complications were temporary renal failure requiring temporary continuous veno-venous hemofiltration in six patients (4.4%), renal failure requiring permanent dialysis in two patients (1.4%), and respiratory failure with necessity of orotracheal reintubation in five patients (3.7%).
3.2 Follow-Up
The follow-up examination included medical history, physical examination, and duplex ultrasound scan and was performed after the index procedure at 1 month, 6 months, 1 year, and yearly thereafter. At a mean follow-up of 63 ± 15 months, 18 (13.3%) of the 135 patients died, including the 3 patients who died during the hospital stay post-surgery. One patient died from renal failure, and five patients died from vascular complications (myocardial (n = 2) and brain infarction (n = 3)).Three patients died from a malignant disease (metastatic lung, pancreatic, and gastric cancer, respectively). In six cases, the cause of death could not be identified.
Late complications leading to secondary surgical or endovascular procedure during follow-up occurred in 12 patients (9.0%) within a time interval of 3–55 months after the first procedure. One patient suffered a thrombotic occlusion of the aortobifemoral prosthesis in one limb, 55 months after surgery, treated with thrombectomy and femoral TEA. Two patients were treated endovascularly with stenting for new-onset limb claudication due to iliac artery stenosis 3 and 21 months after surgery, respectively. One patient was treated endovascularly for iliac anastomotic false aneurysm 32 months after index procedure.
Eight patients with visceral and renal vessel stenosis were treated endovascularly; data regarding visceral and renal vessel patency at follow-up are reported in Table 4.1.
The level of creatinine was comparable with the preoperative period in 122 patients (92.4%), slightly elevated in 6 patients, and elevated in 4 patients.
Among 96 patients suffering from arterial hypertension, 59 patients (61.4%) were still on antihypertensive medication but with reduced medication. In 37 patients with preoperative arterial hypertension, the number of medications was the same as the preoperative period.
All the 43 patients with preoperative chronic visceral ischemia experienced a slow but steady return to normal status after surgical treatment.
Compared with the patients’ conditions before surgery, there was significant clinical and diagnostic improvement after surgery in 126 of the 132 follow-up patients (95.4%), and 4 patients remained stable (3.0%). The two patients with renal failure requiring permanent dialysis presented clinical signs of impairment.
4 Discussion
Reports on calcification and obstruction of the abdominal aorta were rare before 1984 [10,11,12,13,14], when Qvarfordt et al. described a series of nine patients with a unique disease consisting of isolated stenosis of the suprarenal aorta due to a rock-hard, calcified mass [3]. Since then, many authors have been reporting case series of patients diagnosed with similar lesions.
Schulte et al. reported a series of 21 patients, and the most common symptoms were hypertension, intermittent claudication, abdominal pain, impaired renal function, lower extremity pain at rest, and end-stage renal disease. All patients underwent vascular surgical procedures, including open thromboendarterectomy of suprarenal, infrarenal, or supra- and infrarenal aorta and also thromboendarterectomy of visceral and renal vessels in a high percentage of cases or bypass reconstructions in about one-third of cases [15].
In a series of 70 patients with CRA reported by Grotemeyer et al., the most frequent finding was renovascular hypertension, which caused vertigo, headaches, and visual symptoms in about half of the patients. All patients had developed severe stenosis of the renal artery or suprarenal aorta due to protrusion of the coral reef-like calcifications. Intermittent claudication due to peripheral arterial occlusive disease, with pain-free walking distance less than 200 m, was the second most common symptom. Other symptoms were chronic visceral ischemia that caused diarrhea, weight loss, and abdominal angina. Sixty-nine patients underwent surgery with thromboendarterectomy performed on an isolated suprarenal, infrarenal, or both supra- and infrarenal aorta [4].
CRA is not strictly confined to the suprarenal aortic segment; Sako [10] and Harbison [16] had already described infrarenal disease of the same type. In our experience, 91.1% of patients showed a concomitant supra- and infrarenal presence of typical coral reef atherosclerosis. Additionally, a high percentage of patients also suffered from manifest atherosclerotic disease in other vascular areas, in particular coronary arteries (31.8%). Therefore, CRA cannot be regarded as a disease completely separate from the frequent process of general atherosclerosis but rather denotes one with its own particular manifestations and unusual consequences.
Risk factor analysis in our patients underscored the presence of general risk factors for atherosclerosis but the absence of recognized specific, underlying causes.
The clinical picture in our group is consistent with previous reports and is dominated by the hemodynamic compromise of bowel and kidney and lower limb malperfusion with intermittent claudication.
During preoperative evaluation, duplex scan was used to identify hemodynamic aberrations but was not useful for defining the upper limit of the extent of disease because of the heavy calcification and its position. For this reason, NCCT represents an additional value since it helps in identifying the cranial border of the process and thus in defining the best operative approach, whether abdominal or thoracoabdominal. Moreover, in patients without severe preoperative renal failure, CCT and DSA offer important information about vessel patency and collateral networks.
Additional preoperative work-up includes the coronary and supra-aortic vessels because of the very high incidence of concomitant disease and the perioperative risk of mortality and morbidity from this disease. Due to a not negligible incidence of cardiac postoperative complications in our experience, nowadays all patients with CRA and without a preoperative severe renal function impairment (creatinine serum level <2.5 mg/dL) underwent ECG-gated angio-CT and are preoperatively treated in case of significant coronary artery disease.
During preoperative evaluation, chest X-rays and an assessment of pulmonary function are useful in view of the pulmonary morbidity of this operative approach in a patient group composed of heavy smokers.
In literature, several surgical accesses have been proposed: from more invasive laparotomy or thoracotomy [3, 4] to lesser invasive lumbotomy [17] and laparoscopy [18]. In our experience, a median laparotomy, a bilateral subcostal laparotomy with medial visceral rotation, and a left-sided thoracoabdominal incision were tailored to any single patient according to disease extension and patient characteristics.
Open TEA of the occluded parts of the aorta and transaortic TEA of the aortic branches are the most widely used surgical procedures for CRA. Flynn [19] was the first to publish results on aortic TEA in 1959. He removed a calcified aortic plug extending from the descending aorta into the renal arteries in a 27-year-old woman suffering from renovascular hypertension. Thromboendarterectomy represents the surgical procedure of choice for this pattern of sclerotic disease [3, 10, 20, 21]. Aortic repair could be performed with prosthetic patch in case of TEA alone. Prosthetic reconstructions can be amended wherever the thickness of the remaining aortic wall after dissection in the adventitial layer or complicated iliac disease renders it inevitable. In case of severe heavily calcified stenosis or occlusion, visceral and renal vessels could be reimplanted using bypass.
Intraoperative angiography offers the possibility to visualize possible residual stenosis or morphological aberrancies after TEA or after bypass reimplantation that could be treated immediately preventing future occlusion of the vessels. In our experience, 43 angiographies were performed after the procedure with 17 additional simultaneous stenting with good angiographic results.
The kidney is one of the major targets of coral reef aortic disease, and a high percentage of patients presented with renal artery stenosis in this series. A large subgroup of these patients suffered from renovascular hypertension, and surgical treatment was effective in ameliorating this symptom with a general reduction of number of medications needed.
If present, abdominal angina produced a severe malnutrition syndrome in our patients. Their deteriorated status should not defer but encourage timely operation, since patients in our group experienced a slow but steady return to normal status after surgical treatment.
Because of the variable extension of aortic plaque, open surgery for CRA is burdened by high mortality and morbidity rates [22]; despite this, transaortic endarterectomy still represents the treatment of choice in such patients in our experience. To reduce surgical invasivity, some authors have reported a successful endovascular treatment by placement of a stent graft [23, 24]. However, the risk for distal embolization and the technical difficulty in the deployment of the stent graft remain important concerns [15], and then this strategy could be addressed only to less severe forms of CRA [17] or in case of patients with severe comorbidities that could not be treated with surgical approach.
5 Conclusion
Coral reef aorta is a rare, unique disease of the juxta- and infrarenal aorta that is often associated with severe atherosclerotic disease in other domains. The main symptoms are lower limb claudication, hypertension, deterioration of renal function, and angina abdominalis. Surgical treatment offers good results, and a timely operation is advocated to avoid loss of kidney function, complications of long-standing hypertensive disease, and wasting from intestinal malperfusion.
References
Charnsangavej C. Intraluminal calcification and occlusion of the abdominal aorta above the renal arteries. Cardiovasc Intervent Radiol. 1981;4:242–4.
Lipchik EO, Rob CG, Schwartzberg S. Obstruction of the abdominal aorta above the level of the renal arteries. Radiology. 1964;82:443–6.
Qvarford PG, Reilly LM, Sedwitz MM, Ehrenfeld WK, Stoney RJ. “Coral reef” atherosclerosis of the suprarenal aorta: a unique clinical entity. J Vasc Surg. 1984;1:903–8.
Grotemeyer D, Pourhassan S, Rehbein H, Voiculescu A, Reinecke P, Sandmann W. The coral reef aorta–a single centre experience in 70 patients. Int J Angiol. 2007;16:98–105.
Chiesa R, Melissano G, Tshombay Y, Moura MRL. Endoarterectomia dell’aorta toraco-addominale nell’ischemia intestinale acuta e cronica. G Ital Chir Vasc. 2000;7:279–90.
Axilrod HD. Obstruction of the aortic isthmus by a calcified thrombus. Arch Pathol. 1946;41:63–5.
Bialkowski J, Szkutnik M, Bermúdez-Cañete R, Kusa J, Regiec S, Mullins CE. Síndrome de la aorta media causado por enfermedad de Takayasu: Tratamiento con stents y seguimiento a medio plazo. Rev Esp Cardiol. 2002;55:682–5.
Tshomba Y, Kahlberg A, Melissano G, Coppi G, Marone E, Ferrari D, et al. Comparison of renal perfusion solutions during thoracoabdominal aortic aneurysm repair. J Vasc Surg. 2014;59(3):623–33.
Chiesa R, Kahlberg A, Mascia D, Tshomba Y, Civilini E, Melissano G. Use of a novel hybrid vascular graft for sutureless revascularization of the renal arteries during open thoracoabdominal aortic aneurysm repair. J Vasc Surg. 2014;60(3):622–30.
Sako Y. Arteriosclerotic occlusion of the midabdominal aorta. Surgery. 1966;59:709–12.
Bercot M, Idatte JM, Piwnica A. Hypertension arterielle sèvère par stènose de l’aorte sous-diaphragmatiqne. Nouv Press Med. 1972;1:2539–42.
Borromée L, Frija G, Baglin A, Domart M, Lacombe P, Prinseau J, et al. Pseudo-coarctation due a une masse intra-aortique calcifike. Sem Hop Paris. 1983;59:2827–30.
Lipchick E, Rob C, Schwartzberg B. Obstruction of the abdominal aorta above the level of the renal arteries. Radiology. 1964;82:443–5.
Cooley D, De Bakey M. Resection of the thoracic aorta with replacement by homograft for aneurysms and constrictive lesions. J Thorac Surg. 1955;29:66–104.
Schulte KM, Reiher L, Grabitz L, Sandmann W. Coral reef aorta: a long-term study of 21 patients. Ann Vasc Surg. 2000;14(6):626–33.
Harbison S. Arteriosclerotic occlusion of the aorta: a case presenting an unusual location. Surgery. 1957;41:488–90.
DeRubertis BG, Jabori SO, Quinones-Baldrich W, Lawrence PF. Retroperitoneal trapdoor endarterectomy for paravisceral “coral reef” aortic plaque. J Vasc Endovasc. 2012;46:487–91.
Di Centa I, Coggia M, Javerliat I, Alfonsi P, Maury JM, Kitzis M, et al. Total laparoscopic suprarenal aortic coral reef removal. J Vasc Surg. 2006;44:194–7.
Flynn PJ, Kattus AA. Coarctation of the aorta with proximal aortic dilatation and calcific atheromatous degeneration corrected by endarterectomy. J Thorac Cardiovasc Surg. 1959;38:369.
Peillon C, Morlet C, Laissy JP, et al. Endoaortic calcific proliferation of the upper abdominal aorta. Ann Vasc Surg. 1989;3:181–6.
Patra P, Despins P, Duveau D, et al. Obstructive calcification of the descending thoracic aorta and suprarenal abdominal aorta. Two cases (in French). Presse Med. 1985;14:209–11.
Belczak SQ, Sincos IR, Aun R, Costa KV, Araujo EA. Coral reef aorta, emergency surgical: case report and literature review. Einstein (Sao Paulo). 2014;12:237–41.
Verma H, Baliga K, George RK, Tripathi RK. Surgical and endovascular treatment of occlusive aortic syndromes. J Cardiovasc Surg. 2013;54:55–69.
Holfeld J, Gottardi R, Zimpfer D, Dorfmeister M, Dumfarth J, Funovics M, et al. Treatment of symptomatic coral reef aorta by endovascular stent-graft placement. Ann Thorac Surg. 2008;85:1817–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rinaldi, E., Kahlberg, A., Mascia, D., Melissano, G., Chiesa, R. (2019). Aortic “Coral Reef” with Visceral Artery Involvement: Treatment Options. In: Tshomba, Y., Baccellieri, D., Chiesa, R. (eds) Visceral Vessels and Aortic Repair. Springer, Cham. https://doi.org/10.1007/978-3-319-94761-7_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-94761-7_4
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-94760-0
Online ISBN: 978-3-319-94761-7
eBook Packages: MedicineMedicine (R0)