Abstract
Sensor technologies have gained attention as an effective means to monitor physical and mental wellbeing of elderly. In this study, we examined the possibility of using passive in-home sensors to detect frailty in older adults based on their day-to-day in-home living pattern. The sensor-based elderly monitoring system consists of PIR motion sensors and a door contact sensor attached to the main door. A set of pre-defined features associated with elderly’s day-to-day living patterns were derived based on sensor data of 46 elderly gathered over two different time periods. A series of feature vectors depicting different behavioral aspects were derived to train and test three machine learning algorithms; Logistic Regression, Linear Discriminant Analysis and Naïve Bayes. The best prediction scores yielded by seven features, namely, daytime napping, time in the bedroom, night-time sleep, kitchen activity level, kitchen use duration, in-home transitions and away duration. These features produced an area under the ROC curve of 98%, 79% and 93%, for Logistic Regression, Linear Discriminant Analysis and Naïve Bayes algorithms respectively. The findings of this study provide implications on how a non-intrusive sensor-based monitoring system comprised of a minimum set of sensors coupled with predictive analytics can be used to detect frail elderly.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Many countries around the world are undergoing a profound and rapid change in population demographics. In 2016, 12.4% of the population in the Asia-Pacific region was 60 years or older, but this is projected to increase to more than 25% by 2050 [1]. Along with this trend, we have also witnessed a proliferation in cost-effective home and community health care models to support changing population dynamics. Such models assist elderly to age independently in their own homes and to maintain their quality of life for as long as possible. The success of community and home healthcare models depends on a range of services provided by social workers, caregivers and health professionals; such services include regular health assessments, home nursing and allied health aimed at prevention, diagnosis and treatment of health care issues. However, community health caregivers and social workers often face challenges when providing care for people with complex health care needs.
In this regard, technological advancements are transforming traditional health and service models. Specifically, predictive analytics in health and medical care has enabled preventive medicine which entails predicting the probability of a disease and instituting preventive measures to either prevent the disease or significantly decrease its impact on the patient [2]. However, research on technology-based innovations for predictive health and medicine is still in its infancy and are mostly based on clinical settings. In this study, we present an initial research effort to enable community caregivers and social workers to predict elderly’s frailty level based on their day-to-day in-home living pattern.
Frailty is a state of preclinical disability, which embodies an elevated susceptibility to functional declines and adverse health outcomes [3]. It has been often linked to physical as well as mental health wellbeing in older adults [4, 5], as the state of being frail could affect the functional performance and independency in performing activities of daily living. Moreover, past studies have shown the relationship between functional performance declines and adverse health events which lead to hospital admissions or institutionalization or even mortality [6]. Therefore, prevention and early diagnosis of frailty and functional declines is important to ensure that the elderly not only live longer, but also live healthily and independently.
In this study, we examine the possibility of using passive in-home sensors to predict frailty level of older adults. We present a novel approach to unobtrusively identify frail elderly based on their day-to-day living patterns. The findings of this research have many practical implications for health and community care.
2 Research Background
Traditional approaches to frailty screening include administering physical assessments such as walking speed and grip strength, and/or questionnaire assessments by a trained professional in a clinical setting. However, technology-based solutions are increasingly gaining popularity as convenient methods to continuously monitor and quantify physical health of humans. Technologies such as wearables that can measure health vitals and physical activities [7], home-based frailty or fall detection devices [8, 9], smart furniture which can measures gait, balance and weight of the elderly [10], and mobile phone based solutions [11] are among the technologies that are frequently used to measure the physical health of the elderly.
In recent years, Ambient Assisted Living Technologies which encompass systems that support the elderly in their daily living have gained popularity among researchers and practitioners. These refer to technologies that “render their service in a sensitive and responsive way and are unobtrusively integrated into our daily environment” [12]. Such technologies can be used not only to meet the safety needs of the elderly but also to monitor and improve their social, emotional and physical wellbeing. Specifically, non-intrusive in-home sensor technologies have been shown to be effective in early detection of the onset of physical health conditions, mental health disorders such as forgetfulness and depression, and social wellbeing such as loneliness and social isolation [13, 14].
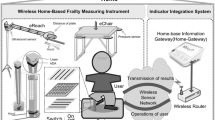
SHINESeniorsFootnote 1 is a research project which aims to create sensor-enabled homes in support of ageing-in-place through inter-disciplinary research efforts. The project has deployed over 80 sensor-enabled homes to remotely monitor elderly when they are alone at home. As shown in Fig. 1, each apartment is installed with a set of motion sensors and a door contact sensor. One or more motion sensors are installed in each room of the house and a door contact sensor is installed on the main door. The motion sensors function by firing a signal at 10 s intervals to indicate whether motion is detected or not. Each house has a minimum of 4 motion sensors, installed in the living room, bedroom, kitchen and toilet. The door contact sensor is magnetic and has two parts: one attached to the main door and the other to the frame. It fires a signal when the two magnets are apart to indicate a door open or close event.
We have developed algorithms to generate meaningful features from raw sensor readings to depict in-home living patterns of elderly participants. Descriptions of the features used in this study are provided in the following section.
3 Data Collection and Feature Extraction
3.1 Data Collection
The data used in this study was collected from sensor-enabled homes of 46 elderly participants in the SHINESeniors project. Participation for the project was voluntary and all the elderly agreed to have sensors installed in their apartments and participate in surveys and interviews. All elderly lived alone in government subsidized one-bedroom apartments in Singapore and were above 60 years.
The installation of the sensor-based elderly monitoring system began in 2015. We conducted two guided surveys to collect information pertaining to elderly participants’ demographics, physical health, mental health and psychosocial wellbeing. The baseline survey was carried out in March 2016 and a follow-up survey was conducted in March 2017. The data extraction methodology is further discussed under ‘Methods’.
3.2 Measure of Frailty
Frailty embodies an elevated risk of declines in health and function among older adults. Clinically, there are two widely used approaches to determine frailty: Phenotype Frailty approach and Deficit Accumulation Frailty approach [15,16,17]. Phenotype approach classifies frailty based on five physical indicators including unintentional weight loss, exhaustion, weakness, slow walking and low physical activity [18]. On the other hand, deficit accumulation approach uses a variety of individual health deficits to quantify the cumulative effect of health deficits. People accumulate deficits that could eventually manifest as frailty as they age. In this study, we use deficit accumulation frailty approach to generate a score of frailty. This approach presents greater discriminatory ability for people with frailty than that of the categorical phenotypic model [19].
We have used the deficit accumulation frailty items used by the Canadian Study of Health and Aging (CSHA) to generate the frailty index [20]. It uses a range of deficits that are readily available in survey or clinical data. The Deficit Frailty accumulation Index (DFI) used in this study was calculated using 39 deficits from the CSHA.
We have gathered inputs needed to generate the DFI through surveys conducted at the baseline (n = 46) and follow-up (n = 39). The final deficit accumulation score was calculated based on the proportion of potential deficits that are present in an elderly [16]. Please refer to the Appendix for the complete list of deficits.
Figure 2 shows the distribution of the frailty index. The DFI score ranged between 0.06 and 0.56, while a majority showed a score of below 0.3. Further, 17 elderly showed reduced DFI score at the follow-up assessment compared to the baseline, while 12 elderly showed an increased score. In other words, the health status improved for 17 elderly, but deteriorated for 12 elderly by the time of the follow-up assessment (Fig. 3).
The deficit frailty accumulation index served as the ground truth to determine if an elderly is frail or robust. We have used the median split at each survey (0.25 at the baseline and 0.22 at the follow-up) to divide elderly into two groups: robust and frail. Therefore, the problem of predicting elderly who are frail can be formulated as a binary classification problem.
3.3 Feature Extraction
From sensor data, a number of pre-defined features were generated to depict elderly’s daily living pattern. All features were generated based on the following definitions:
-
(1)
Away duration and frequency: going out intervals were calculated based on the door contact sensor and when no-activity is detected by the motion sensors. The elderly resident is considered to be out of the flat if no motion is detected between two consecutive door contact events for more than 30 min. Away frequency is the number of times the elderly has gone out of the house.
-
(2)
Sleep duration: sleep durations and intervals were derived based on the motion sensor in the bedroom. The elderly is considered asleep if no motion is detected in any area other than the bedroom for at least 30 min. Sleep events between 7 am to 7 pm are considered as napping durations while those occurring between 7 pm to 7am are considered night-time sleep [14].
-
(3)
Location occupancy and frequency: the time spent in each location of the flat (i.e. living room, bedroom, kitchen, and toilet) was determined based on sensor firings of respective PIR sensors. Location occupancy durations were derived for each location in a similar way as the sleep duration calculation, but with a 2 min threshold. This 2-min threshold was used to ensure that the elderly is actually performing some activity in a particular location. Further, occupancy frequency for each location was calculated based on the number of times the location is used.
-
(4)
Intensity of sensor firings: elderly who are fully independent in performing activities of daily living are likely to perform more household chores, thus triggering more sensor signals. The intensity of the sensor signal in each room was calculated based on the total number of motions detected by the respective PIR sensor. If the resident is active in a particular area, the number of sensor firings should be higher than when the elderly is stationary within a given time interval.
-
(5)
In-home transitions: number of times the elderly transited between rooms was calculated as an indicator for the in-home activity level. Transitions were counted based on the changes in the location occupancy status. For example, if the elderly moved from the bedroom to the living room, the location status will also change accordingly, resulting in one transition. If the elderly is active in the home, the number of transitions should be high, as there will be more movements between different rooms in the flat.
From the above feature categories, three sets of features were derived to represent (1) whole day (which we refer to as ‘generic’ in latter sections), (2) daytime and (3) nighttime living pattern. Activities between 7 am to 7 pm are labeled as daytime while those between 7 pm to 7 am are labeled as nighttime. Furthermore, all features were normalized based on the in-home duration and averaged to a day. Thus, feature values are proportionate to the time duration that the elderly resident is actually at home and represent his/her average in-home living pattern.
4 Methods
For the features identified in Sect. 3, we conducted a correlation analysis between sensor-derived features and the survey-derived frailty category to determine the optimal time window for the prediction model. This step will ensure that the sensor observed living pattern is a true representation of the health status of the elderly as measured by the surveys.
Figure 4 depicts a heat map of 7 features (i.e., a subset of features used for the analysis) for one elderly. As illustrated, frailty categories calculated using the baseline and the follow-up survey data were used to label sensor-derived feature vectors for each elderly. Second, sensor derived feature scores measured over the time window (t) were averaged to generate daily scores. This process of feature extraction resulted in 3 datasets representing 15 day, 30 day and 60 day time windows before the survey date.
Figure 5 depicts the results of the correlation analysis. Daytime napping duration and kitchen use duration showed the highest correlation with the frailty category. Further, correlation coefficients did not show a significant difference across the three time windows. Assuming the frailty category of the elderly would not change over a 30 day period, sensor data up to 30 days before the survey date was chosen for the final analysis. Furthermore, subjects were removed from the final analysis, (1) if there was not enough sensor-data gathered during the 30 day window and (2) if the elderly did not participate in the survey. This resulted in 43 subjects from the baseline and 39 from the follow-up survey (please refer to Table 1). In total, the dataset consists of 37 data points to represent ‘frail’ category and 45 for ‘robust’.
First, based on the features illustrated in Fig. 5, we defined a series of feature combinations to depict different behavioral aspects of elderly. For example, features representing night-time behaviors: such as night-time toilet usage, time spent in the living room and kitchen usage during the night, night-time sleep etc., and day-time behaviors: such as going out, napping, kitchen activity during the daytime etc. Second, we used a filter based feature selection method using correlation coefficients (r = 0.2) to select the most significant features of a given feature combination. Each selected feature combination was then used as input vectors to train and test machine learning algorithms.
Finally, to predict if an elderly is frail or robust, we examined several machine learning algorithms using scikitlearn. Each algorithm was trained, validated and tested with each identified feature vector. Out of which, Logistic Regression (LR), Linear Discriminant Analysis (LDR), and Naïve Bayes (NB) were selected as they gave the best validation accuracy. The next section describes the results of best machine learning algorithm and feature vector combinations.
5 Results and Discussion
All 46 elderly who participated in our study were within the age range of 60 to 91, had primary or no formal education, 27 were female and 19 were male. 87% of the elderly were of Chinese descent and 3 were married but living alone most of the day.
Table 2 shows the Pearson Correlation Coefficients of the features selected for the two feature vectors, which yielded the best validation scores under three machine learning algorithms. Correlation Coefficients could give a better understanding of the relationship between the survey-derived DFI category and the features generated by the sensors. Feature vector one includes ‘generic features’ representing daily average values. According to the analysis, kitchen usage duration, kitchen activity level and transitions are negatively correlated with DFI. This result indicates that the intensity of in-home activities is lower for frail elderly. Furthermore, results derived from the bedroom sensor (i.e. time spent in the bedroom, napping and night-time sleep duration) showed a positive relationship with DFI, indicating that the frail elderly are likely to spend more time in the bedroom.
Feature vector two represents selected ‘daytime features’ (please note that the away duration is considered as a daytime feature). Contrary to the first set of features (i.e. feature vector one), daytime features derived from the kitchen sensor and transitions during the daytime did not show strong correlation with DFI. On the other hand, Away duration is negatively correlated while the door open count shows a positive correlation with the DFI. As frail elderly are less likely to go out of the house, they may open/close the door frequently between multiple periods of rest in the bedroom.
Both feature vectors were then used to train and test three machine learning algorithms; Logistic Regression (LR), Linear Discriminant Analysis (LDA) and Naïve Bayes (NB). First, training and validation was done using k-fold validation, with k = 6. Training and cross validation results for each model are presented in Fig. 6.
After the cross validation, trained classifiers were tested on 16 randomly assigned data points. The performance was quantified by generating the ROC curves and calculating the areas under them (AUC) in predicting the ‘Frail’ class. Figure 7a and 7b depicts ROC curves for the above two feature combinations. LR resulted in the highest area under the ROC curve for both generic and daytime input feature vectors (98% and 90%), LDA showed 79% and 67% and NB showed 93% and 79% respectively.
The results are encouraging and suggest that seven selected generic features, depicting whole day average living patterns of elderly, can be used to classify frail elderly with a 100% of true positive rate, if a 19% false positive rate is tolerable. Similarly, features used for the daytime feature vector are able to predict frail elderly with an 81% of accuracy if a 19% false positive rate is tolerable.
Finally, we used results of the Logistic Regression to derive feature scores for both input vectors to determine the relative importance of each feature in predicting frail elderly. Figure 8 shows the feature rankings based on the coefficient scores of the Logistic Regression. According to the results, features derived based on the bedroom sensor, namely, napping duration, night-time sleep duration and the time spent in the bedroom, showed highest significance in predicting frailty in the elderly. This suggests that, frail elderly are likely to sleep more and spend more time in the bedroom than the robust elderly. When considering the daytime features, the number of times the door was open showed the highest significance, as frail elderly are likely to open the door more frequently during the daytime as they might be spending more time at the home compared to robust elderly.
6 Conclusion
In this study, we demonstrated the feasibility of using in-home unobtrusive sensors to autonomously detect frail elderly. Based on motion sensors installed in each room of the apartment and one door contact sensor on the main door, we derived a set of pre-defined features to reflect an elderly’s in-home living pattern. Further, we used the deficit accumulation frailty index calculated using 39 questions from the Canadian Study of Health and Aging and used the median split to categorize frail and robust elderly. Using a time window of 30 days for sensor-derived features, a series of feature vectors to depict different behavioral aspects of elderly were derived. Out of which, two combinations representing elderly’s (1) daytime behavioral pattern and (2) whole day behavioral pattern (i.e. generic features), performed best under three machine learning algorithms: Logistic Regression, Linear Discriminant Analysis and Naïve Bayes.
Overall, the results are encouraging. Our findings showed that the in-home living pattern of elderly detected by a minimal set of motion sensors and a door contact sensor, could unobtrusively identify if an elderly is frail or robust. The input vector which performed best under three machine learning algorithms included 7 features: napping, time in the bedroom, night-time sleep, kitchen activity level, kitchen use duration, in-home transitions and away duration. These features yielded an area under the ROC curve of 98%, 79% and 93% for Logistic Regression, Linear Discriminant Analysis and Naïve Bayes classifiers respectively. We also examined the importance of features and found that, napping duration is the most useful in discriminating frail from robust elderly, followed by the average time spent in the bedroom and night-time sleep duration.
Our findings have important implications for social and community care and practice. Our study showed the possibility of using sensor-based monitoring systems to unobtrusively predict frail elderly based on their in-home living pattern. Future research will be done to extend the findings to continuous monitoring and detection of frailty level accelerations of community dwelling elderly. This will enable community caregivers to take timely measures and carry out necessary interventions to slow down the health deterioration or significantly reduce adverse health events.
Notes
- 1.
SHINESeniors: http://centres.smu.edu.sg/icity/shinesenior/.
References
United Nations: Ageing in the Asian and Pacific Region: An overview (2016)
National Academies of Sciences, Engineering and Medicine: Relevance of Health Literacy to Precision Medicine: Proceedings of a Workshop. National Academies Press (2016)
Fried, L.P., et al.: Frailty in older adults: evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 56(3), M146–M157 (2001)
Boyle, P.A., et al.: Physical frailty is associated with incident mild cognitive impairment in community-based older persons. J. Am. Geriatr. Soc. 58(2), 248–255 (2010)
Masel, M.C., et al.: Frailty and health related quality of life in older Mexican Americans. Health Qual. Life Outcomes 7(1), 70 (2009)
Rozzini, R., et al.: Relationship between functional loss before hospital admission and mortality in elderly persons with medical illness. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 60(9), 1180–1183 (2005)
Schwenk, M., et al.: Wearable sensor-based in-home assessment of gait, balance, and physical activity for discrimination of frailty status: baseline results of the Arizona frailty cohort study. Gerontology 61(3), 258–267 (2015)
Lin, C.-C., et al.: Development of home-based frailty detection device using wireless sensor networks. J. Med. Biol. Eng. 36(2), 168–177 (2016)
Schwenk, M., et al.: Frailty and technology: a systematic review of gait analysis in those with frailty. Gerontology 60(1), 79–89 (2014)
Chang, Y.-C., et al.: eFurniture for home-based frailty detection using artificial neural networks and wireless sensors. Med. Eng. Phys. 35(2), 263–268 (2013)
Fontecha, J., et al.: Elderly frailty detection by using accelerometer-enabled smartphones and clinical information records. Pers. Ubiquit. Comput. 17(6), 1073–1083 (2013)
Kleinberger, T., Becker, M., Ras, E., Holzinger, A., Müller, P.: Ambient intelligence in assisted living: enable elderly people to handle future interfaces. In: Stephanidis, C. (ed.) UAHCI 2007. LNCS, vol. 4555, pp. 103–112. Springer, Heidelberg (2007). https://doi.org/10.1007/978-3-540-73281-5_11
Yefimova, M.: Using in-Home Monitoring Technology to Identify Deviations in Daily Routines Preceding Changes in Health Trajectory of Older Adults (2016)
Goonawardene, N., Toh, X., Tan, H.-P.: Sensor-driven detection of social isolation in community-dwelling elderly. In: Zhou, J., Salvendy, G. (eds.) ITAP 2017. LNCS, vol. 10298, pp. 378–392. Springer, Cham (2017). https://doi.org/10.1007/978-3-319-58536-9_30
Theou, O., et al.: Identifying common characteristics of frailty across seven scales. J. Am. Geriatr. Soc. 62(5), 901–906 (2014)
Rockwood, K., Mitnitski, A.: Frailty in relation to the accumulation of deficits. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 62(7), 722–727 (2007)
Rockwood, K., Andrew, M., Mitnitski, A.: A comparison of two approaches to measuring frailty in elderly people. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 62(7), 738–743 (2007)
Fried, L.P.: Cardiovascular health study collaborative research group: frailty in older adults: evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56, M146–M156 (2001)
Clegg, A., et al.: Frailty in elderly people. The Lancet 381(9868), 752–762 (2013)
Rockwood, K., et al.: A global clinical measure of fitness and frailty in elderly people. Can. Med. Assoc. J. 173(5), 489–495 (2005)
Acknowledgements
This research was supported by the Singapore Ministry of National Development and National Research Foundation under the Land and Livability National Innovation Challenge (L2NIC) Award No. L2NICCFP1-2013-5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Appendix
Appendix
List of deficits:
Activities of daily living and instrumental activities of daily living |
|---|
• Difficulty with preparing meals |
• Difficulty in eating |
• Difficulty with housework |
• Difficulty with going out |
• Difficulty with moving around |
• Difficulty with taking shower |
• Difficulty with dressing |
• Difficulty with toileting |
• Difficulty with going out |
• Urinary incontinent |
Physical health |
|---|
• Falls |
• Eye trouble |
• Chronic conditions |
– History of heart failure |
– Other heart conditions |
– Cancer |
– History of stroke |
– Hypertension |
– Diabetes |
– Respiratory disorder |
– Stomach/intestine problem |
– Renal/kidney or urinary tract |
– Prostrate problem |
– Joint pain, arthritis or chronic back pain |
– Osteoporosis |
– Hyperlipidaemia |
– Fractures of the hip, thigh or pelvis |
– Other fractures |
– Cataract |
– Glaucoma |
– History of thyroid disease |
– ther chronic conditions |
Mental health |
|---|
• Depression |
• Short term memory problem |
• Cognition impairment |
• Mental/emotion problem |
• Feel unhappy |
Sleep |
|---|
• Taking medicine to fall sleep |
• Sleeping disorder |
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this paper
Cite this paper
Goonawardene, N., Tan, HP., Tan, L.B. (2018). Unobtrusive Detection of Frailty in Older Adults. In: Zhou, J., Salvendy, G. (eds) Human Aspects of IT for the Aged Population. Applications in Health, Assistance, and Entertainment. ITAP 2018. Lecture Notes in Computer Science(), vol 10927. Springer, Cham. https://doi.org/10.1007/978-3-319-92037-5_22
Download citation
DOI: https://doi.org/10.1007/978-3-319-92037-5_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92036-8
Online ISBN: 978-3-319-92037-5
eBook Packages: Computer ScienceComputer Science (R0)