Abstract
This research investigates the impact of socio-demographic factors such as age, gender, income and location on ICT acceptance for diabetes self-care. The investigation is due to the increasing number of diabetic patients in South Africa, where large segments of the population experience technological forms of exclusions. The context warrants research in geographical areas where ICT use is not pervasive yet. This research, used the UTAUT model with purposive sampling for 497 diabetic respondents, residing in low socio-economic communities. It analysed survey data using linear regression. It found that age had a strong moderating effect on all four UTAUT constructs. Gender only had a moderating effect on performance expectancy and social influence. In contrast to findings in the extant literature, income and location had no significant moderating effect in this context.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The Western Cape, one of the nine provinces in South Africa, [1] has a history of racial segregation, officially implemented by the Group Areas Act in 1950 [2]. The Act issued identity cards, which indicated has five racial groups; Black, Coloured, Indian, Malay and White [2]. Coloured people are typically mixed race, descendants of Malaysian slaves or Khoisan descendants [3]. ‘Non-white’ groups were forcibly removed from areas in the City, such as District Six, and placed in township areas such as Khayelitsha and Mitchells Plain [4]. These areas are regarded as the Cape Flats [4]. Approximately 63% of households in the Khayelitsha and Mitchells Plain have incomes of less than R4166 per month (approximately $296), of which 16.5% have no income [5].
The Western Cape reports a decline in the number of households connected to the mains electricity supply, from 93.5% in 2008 to 87.9% in 2018 [6]. Also, 19% of the Western Cape population live in informal dwellings [6]. Informal dwellings may not have access to water and electricity. However, it was found that “having adequate access to appropriate forms of energy is critical for improving living standards, health and reducing poverty” [7]. Therefore, the demographics of the province reflect that the socio-economic plight of a substantive population is bleak.
The Western Cape includes large segments of the South African population who experience “technological forms of exclusion” as well as educational and income inequalities [8]. Despite the penetration of mobile phones (95.5%) in the Western Cape, 25.8% had internet access at home [6]. Therefore, the resulting digital divide between rich and poor is substantial [8]. This may impact the achievement of diabetes self-management as access to information is a key component in managing chronic conditions [9].
The Western Cape Government has recognised that broadband costs are still unaffordable to many citizens, so the Broadband Game Changer aims to provide all residents with access to affordable high-speed broadband infrastructure [10]. Also, the City of Cape Town is providing public Wi-Fi zones in more than 100 public buildings such as clinics, administration buildings and traffic departments, across Cape Town. Also, Wi-Fi is available in several public spaces, such as the Company Gardens. Wi-Fi services are also being implemented at public transport interchanges such as Athlone, Atlantis, City Centre, Langa, Nyanga, Uitsig and Valhalla Park. Users are allowed 50 MB per day and may purchase more data after that [11]. This improvement in the access layer provides a fertile ground for citizens, even from low socio-economic demographics, to harness m-health apps for various personal uses, including that of diabetes self- management.
According to the annual trends for diabetes incidence by province, 2013/14–2016/17, the Western Cape is indicating a rapid increase [12]. The Overberg West has the highest average (1.4) of diabetes incidence per 1000 total population, followed by Cape Town (1.2) [12]. It is also the leading cause of mortality in this province [13].
Therefore, there is a significant disease burden that requires comprehensive health care to manage these conditions [14]. However, health care in South Africa experiences severe staff shortages in the public health sector [15]. These shortages are particularly prevalent in rural and underserved areas [15]. Therefore, there is an increased need for patients to practice self-care.
Self-care involves “the ability to make decisions and perform actions directly under the control of the individual, and is influenced by a variety of individual characteristics” [9 p. 1734]. Diabetes self-care is multidimensional and includes a range of activities such as self-monitoring of blood glucose, diet and foot care [16]. It is found that self-care is situationally influenced [9].
The use of Information, Communication and Technology (ICT) as an enabler for self-care activities, performed by the patient, includes the use of the Internet (47%), cellular phones (32%), telemedicine (12%), and decision support techniques (9%) [17]. Also, ICT interventions can also be used to reduce diabetes risk factors by improving physical inactivity and smoking [18].
However, despite increased access to ICT in developing countries like South Africa, the promise of ICT to deliver diabetes self-care improvements will be limited by uptake and high attrition rates [19]. The use of ICT, such as mobile health (m-health) applications for diabetes, is low [20]. The low usage is prevalent, especially amongst older patients [20]. A population study in Germany supports this finding. It revealed that age and socio-economic status led to disparities in m-health usage [21]. However, the most prominent type of diabetes (90%) is type 2 diabetes [22]. Type 2 diabetes is most often diagnosed in older patients [22]. Therefore, the introduction of ICT, will not lead to the improvement of self-care unless it is accepted and used by the intended user population, i.e. older patients with diabetes [23].
In order to assess the acceptance and use of technology, the literature points to a number of models such as the Theory of Reasoned Action (TRA) [24], Theory of Planned Behaviour (TPB) [25], Technology Acceptance Model (TAM) [26] and the Unified Theory of Acceptance and Use of Technology (UTAUT) [27]. It was found that the eight models used to develop UTAUT, including TRA, TPB and TAM, explained between 17% and 53% variance in user intentions to use technology [27]. However, the UTAUT model explained 77% of the variance in behavioural intention to use technology and 52% of the variance in technology use [28]. The UTAUT model was therefore applied in this study, given that it outperforms other models of acceptance.
More recent research provide evidence of 1,267 UTAUT citations including new exogenous, endogenous or moderation variables [28]. This research provides new moderation variables in the South African context. Additionally, it was used in a study conducted in the Western Cape on the usage of ICT for diabetes self-management [29]. In that study, it was found that despite a high behavioural intention, there is low usage to almost 70% of the target population not using forms of ICT, such as mobile health. However, the Petersen et al. [29] study did account for how socio-demographic factors (e.g. age, gender, income or location), could explain the lack of use. Consequently, the main research question that forms the basis of this paper is ‘what is the impact of socio-demographic factors on the acceptance of ICT for diabetes self-care?’
2 Objectives
Behavioural intention has a direct influence on the usage of technology [27]. The extant literature indicates that low levels of ICT for DM self-management amongst the elderly. Therefore, for succinctness, only behavioural intention was examined. This is due to the main objective is to understand the impact of socio-demographic factors on technology acceptance for diabetes self-care. This study, therefore, expands on the original study [29], and seeks to determine if the following factors affect the acceptance of ICT for diabetes self-care in the Western Cape, South Africa using constructs identified by Venkatesh et al. [28]:
-
Age,
-
Gender,
-
Income and
-
Patient’s location, i.e. rural/urban [28].
3 Methodology
This research was framed within a positivist paradigm which posits that at an ontological level, knowledge is quantifiable and objective [30]. Positivist methodology uses quantitative methods and quantitative analysis [31]. Purposive sampling [32] was used in this research to select patients with diabetes (n = 497) living predominantly within low socio-economic communities in Western Cape.
Quantitative data from online surveys were analysed via descriptive statistics and linear regression, using SPSS software [33]. A 6 point Likert scale (strongly disagree to strongly agree) was used. The survey questions were based on the core constructs inherent in the UTAUT model [27] and adapted for this research. The survey questions are provided in Table 1.
Based on [34], no clinical data or unique identifiers (such as names or ID numbers) were collected to ensure anonymity and the protection of the identities and interests of those involved. The researchers respected the confidentiality of the data supplied by all parties involved by storing data in a restricted access folder on Google drive.
4 Research Model
The UTAUT model includes four independent variables [27]:
-
1.
Performance expectancy (PE): “is the degree to which an individual believes that using the system will help him or her to attain gains in job performance” (p. 447).
-
2.
Effort expectancy (EE): “is the degree of ease associated with the use of the system” (p. 450).
-
3.
Social influence (SI): “is the degree to which an individual perceives that important others believe he or she should use the new system” (p. 451).
-
4.
Facilitating conditions (FC): “is the degree to which an individual believes that an organisational and technical infrastructure exists to support the use of the system” (p. 453).
The relationships between the key constructs and moderators were hypothesised as follows (Table 2):
The conceptual model, based on the UTAUT model [27], was developed to achieve the stated research objectives (Fig. 1).
5 Results
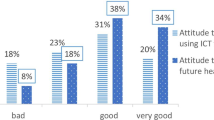
The 497 Western Cape respondents, who participated in this research, were predominantly females (55.9%) older than 50 years (40.6%) who had type 2 diabetes (89.1%). They resided in low socio-economic areas on the Cape Flats such as Mitchell’s Plain (11.4%), Belhar (10.8%), Khayelitsha (9.4%), Athlone (6.0%), Delft as well as Gugulethu (4.6%).
A series of regression analyses were run to examine the relationships between effort expectancy, performance expectancy, social influence and facilitating conditions. Table 3 shows the univariate statistics, correlations of each variable with behavioural intention, and the regression weights for the socio-demographic moderators added.
The strength of the linear fit is explained by R-squared (R2). This explains the amount of variation of the independent variables on the dependent variable, behavioural intention [33]. The full model had an R2 = 0.534 and p < .0001.
Despite high behavioural intention and the socio-demographic factors investigated, 67.4% of respondents indicated that they did not use ICT such as diabetes applications on their smartphone, insulin pump, continuous glucose monitoring (CGM).
6 Discussion
This discussion will address the significant and non-significant factors affecting the acceptance of ICT for diabetes self-care.
6.1 Significant Factors
The summarised table of findings indicates that the strongest moderating factor was age (Table 3). Age had a significant effect on all four of the constructs but reduced the p-values. However, the relationships were still significant at a 95% confidence interval. Gender affected PE and SI but also reduced the original model p-values. However, it was still significant at a 95% confidence interval. Age and gender have been identified in previous studies as a critical factor for the acceptance and use of ICT, such as m-health applications in developed [21] and developing countries [35].
Literature also indicates that the digital divide is more prevalent for people older than 65 years [36], an age group that is linked to patients with Type 2 (non-insulin-dependent) diabetes [37]. The needs of diabetic patients may be varied due to varying previous knowledge, education, age, income, type of diabetes and therapy [38, 39]. Interventions should include the elderly as part of the stakeholder group, or critical factors that are necessary to address the real problem may be overlooked. This may result in poor adoption and inefficient use of technology [40]. Interventions should include new perspectives and use patients’ tactic knowledge [40].
6.2 Non-significant Factors
Diabetes is a non-communicable disease that affects disadvantaged populations more than in higher-income countries [41]. This constitutes a challenge to the achievement of the third SDG, focusing on the health and wellbeing of all [42]. Literature indicates that people of low socioeconomic status may not have the capability to achieve optimal health functioning [43]. Low income is identified as a barrier to achieving diabetes treatment goals [44]. This is prevalent for medication non-adherence being higher among minorities groups and those with low socio-economic status [45].
However, in this research, income and locations proved not to be significant for any constructs. This finding is contrary to research conducted in urban China, that indicates that age and location have strong moderating effects on acceptance [46]. This suggests that findings in respect of technology acceptance are not necessarily transferable between different geographical locations.
7 Conclusion
The research aimed to expand on an exploratory study [29] by investigating additional socio-demographic factors which affect the acceptance of ICTs for diabetes self-care. Despite findings that indicate age is a significant moderating variable, income and location were not. Intervention design, including co-design strategies, should consider highlighting the additional benefits of using ICT interventions. This could result in making m-health applications easier to use, especially for older users.
It is possible that acceptance may be influenced by other factors. For instance, in lower-income groups where medication non-adherence is common, patient engagement is crucial for an intervention’s success [45]. Research suggests, for patients 50 years or older, the lack of additional benefits and ease of use are significant factors for the acceptance of diabetes m-health applications. Therefore, intervention design in the case of ICT applications for diabetes self-management should take into consideration these factors.
Further research should use qualitative methods to examine why location and income are not moderating factors, despite research indicating this in other contexts.
References
The Local Government Handbook: City of Cape Town Metropolitan Municipality. The Local Government Handbook: A Complete guide to municipalities in South Africa (2017). https://municipalities.co.za/map/6/city-of-cape-town-metropolitan-municipality. Accessed 18 Jan 2018
South African History Online. Cape Town the Segregated city (2011)
Mthembu, J.: What it means to be a coloured man on the Cape Flats. UCT News (2015). https://www.news.uct.ac.za/article/-2015-07-30-what-it-means-to-be-a-coloured-man-on-the-cape-flats. Accessed 24 Oct 2018
Bähre, E.: Housing for the urban poor: a post-apartheid dream or nightmare? South African History Online (2014)
Western Cape Government: Socio-economic Profile (2017)
Statistics South Africa: P0318 - General Household Survey (GHS), 2018 (2018)
Statistics South Africa: Mbalo Brief - the missing piece of the puzzle, Pretoria (2015)
Gillwald, A., Mothobi, O., Rademan, B.: After access paper series: the state of ICT in South Africa (2017)
Omisakin, F.D., Ncama, B.P.: Self, self-care and self-management concepts: implications for self-management education. Educ. Res. 2(12), 2141–5161 (2011)
Western Cape Government: Switching on public Wi-Fi hotspots across the Western Cape (2017). https://www.westerncape.gov.za/general-publication/switching-public-wi-fi-hotspots-across-western-cape. Accessed 24 Aug 2018
City of Cape Town: Wi-Fi zones across Cape Town (2018). http://www.capetown.gov.za/Localandcommunities/Get-online/Public-WiFi-Zones/Public-WiFi-across-the-City. Accessed 23 Aug 2018
Kengne, A.P., Sayed, B.: Non-communicable diseases, vol. 56, no. July, pp. 83–95 (2017)
Statistics South Africa: Mortality and causes of death in South Africa, Pretoria (2016)
International Diabetes Federation (IDF): IDF Diabetes Atlas Eighth edition, pp. 8–30 (2017)
Health Systems Trust: South African Health Review 2018 (2018)
Toobert, D.J., Hampson, S.E., Glasgow, R.E.: The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabet. Care 23(7), 943–950 (2000)
El-Gayar, O., Timsina, P., Nawar, N., Eid, W.: A systematic review of IT for diabetes self-management: Are we there yet? Int. J. Med. Inform. 82(8), 637–652 (2013)
Rehman, H., Kamal, A.K., Sayani, S., Morris, P.B., Merchant, A.T., Virani, S.S.: Using mobile health (mHealth) technology in the management of diabetes mellitus, physical inactivity, and smoking. Curr. Atheroscler. Rep. 19(4), 16 (2017)
Yu, C.H., et al.: A web-based intervention to support self-management of patients with type 2 diabetes mellitus: effect on self-efficacy, self-care and diabetes distress. BMC Med. Inform. Decis. Mak. 14(1), 117 (2014)
Li, M., et al.: Analysis of obstacles and motivations found utilizing a diabetes health app for older patients. Innov. Aging 1(suppl_1), 642 (2017)
Ernsting, C., et al.: Using smartphones and health apps to change and manage health behaviors: a population-based survey. J. Med. Internet Res. 19(4), e101 (2017)
IDF: IDF Africa Members (2018). https://www.idf.org/our-network/regions-members/africa/members/25-south-africa. Accessed 22 Oct 2018
Heffernan, C., Lin, Y., Thomson, K.: Drawing from development: towards unifying theory and practice of ICT4D. J. Int. Dev. 28(6), 902–918 (2016)
Fishbein, M., Ajzen, I.: Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Addison-Wesley, Boston (1975)
Ajzen, I.: The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 50, 179–211 (1991)
Davis, F.D.: Perceived ease of use, and user acceptance of information technology. MIS Q. 13(3), 319–340 (1989)
Venkatesh, V., Morris, M.G., Davis, G.B., Davis, F.D.: User acceptance of information technology: toward a unified view. MIS Q. 27(3), 425–478 (2003)
Venkatesh, V., Thong, J., Xu, X.: Unified theory of acceptance and use of technology: a synthesis and the road ahead. J. Assoc. Inf. Syst. 17(5), 328–376 (2016)
Petersen, F., Pather, S., Tucker, W.D.: User acceptance of ICT for diabetes self-management in the Western Cape, South Africa. In: African Conference of Information Systems and Technology (ACIST), pp. 1–11 (2018)
Mingers, J.: Philosophical foundations: critical realism. In: Mingers, J. (ed.) Realising Systems Thinking: Knowledge and Action in Management Science, pp. 11–31. Springer, Boston (2006). https://doi.org/10.1007/0-387-29841-X_2
Thomas, P.Y.: Research methodology and design. In: Research Methodology and Design, pp. 291–334. Unisa, South Africa (2010)
Marshall, M.N.: Sampling for qualitative research. Family Pract. 13(6), 522–525 (1996)
Diez, D.M., Barr, C.D., Centinkaya, M.: OpenIntro: Statistics Preliminary Edition, vol. 1, CreateSpace Independent Publishing Platform (2012)
Dearden, A., Kleine, D.: A proposal for minimum ethical standards in ICTD/ICT4D research (2018)
Jennings, L., Omoni, A., Akerele, A., Ibrahim, Y., Ekanem, E.: Disparities in mobile phone access and maternal health service utilization in Nigeria: a population-based survey. Int. J. Med. Inform. 84(5), 341–348 (2015)
Friemel, T.N.: The digital divide has grown old: determinants of a digital divide among seniors. New Media Soc. 18(2), 313–331 (2016)
American Diabetes Association: Improving care and promoting health in populations: standards of medical care in diabetes (2019)
Scheibe, M., Reichelt, J., Bellmann, M., Kirch, W.: Acceptance factors of mobile apps for diabetes by patients aged 50 or older: a qualitative study. Medicine 2.0 4(1), e1 (2015)
Coetzer, J.: Application of HCI design principles in overcoming information illiteracy: case of a M-health application for a rural community in South Africa. In: 2018 International Conference on Intelligent and Innovative Computing Applications, ICONIC 2018, pp. 1–7 (2018)
Isaković, M., Sedlar, U., Volk, M., Bešter, J.: Usability pitfalls of diabetes mHealth apps for the elderly. J. Diabetes Res. 2016, 9 p (2016)
World Health Organisation: Diabetes (2018). http://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed 25 Nov 2018
United Nations: Transforming our world: the 2030 Agenda for Sustainable Development, vol. 16301, no. October, pp. 1–35 (2015)
Weaver, R.R., Lemonde, M., Payman, N., Goodman, W.M.: Health capabilities and diabetes self-management: the impact of economic, social, and cultural resources. Soc. Sci. Med. 102, 58–68 (2014)
American Diabetes Association: Standards of medical care in diabetes - 2015. J. Clin. Appl. Res. Educ. 38(January), 1–94 (2015)
Nelson, L.A., Mulvaney, S.A., Gebretsadik, T., Ho, Y.X., Johnson, K.B., Osborn, C.Y.: Disparities in the use of a mHealth medication adherence promotion intervention for low-income adults with type 2 diabetes. J. Am. Med. Inform. Assoc. 23(1), 12–18 (2016)
Lu, J., Yu, C.-S., Liu, C.: Mobile data service demographics in urban china. J. Comput. Inf. Syst. 50(2), 117–126 (2009)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 IFIP International Federation for Information Processing
About this paper
Cite this paper
Petersen, F., Baker, A., Pather, S., Tucker, W.D. (2020). Impact of Socio-Demographic Factors on the Acceptance of Information Communication and Technology (ICT) for Diabetes Self-care. In: Hattingh, M., Matthee, M., Smuts, H., Pappas, I., Dwivedi, Y.K., Mäntymäki, M. (eds) Responsible Design, Implementation and Use of Information and Communication Technology. I3E 2020. Lecture Notes in Computer Science(), vol 12067. Springer, Cham. https://doi.org/10.1007/978-3-030-45002-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-45002-1_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-45001-4
Online ISBN: 978-3-030-45002-1
eBook Packages: Computer ScienceComputer Science (R0)