Abstract
Much of the information produced in hospitals is clinical and stored for the purposes of documentation. In practice, most of it is never used. The potential of analytics is to reuse this information for other purposes. This is easier said than done, because of technical, semantic, legal and organizational hindrances. In particular, hospitals are not organized to leverage the value of big data. In this study we ask, what does it take to establish an analytics capability in a large hospital? Our empirical evidence is a longitudinal study in a high-tech hospital in Norway, where we followed the development an analytics capability, and assessed the organisational benefits. We offer two findings. First, the analytics capability is much more than the technology; it is the network of analytics technology, an analytics team and the medical and administrative decision makers. Second, we identify institutionalization, both organizationally and temporally, of the analytics process as the key success factor.
You have full access to this open access chapter, Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
This study deals with the challenge of establishing an analytics capability at hospitals. The motivation is both practical and theoretical. From a practical point of view, most hospitals produce large amounts of clinical and administrative information every day, but mainly for documentation needs. Most of it is never used for other purposes, such as analytics, in order to support decision-making and improvement processes. From a theoretical perspective, we know much about analytics in general, but much less about analytics in hospitals.
Several challenges have been identified:
-
The current portfolios of Health systems are often fragmented and silo oriented, making it difficult to get access to data [1]
-
Data are defined and stored in many formats, and the lack of technical and semantic standardisation makes it difficult to combine data from many sources [2]
-
Security and privacy concerns are certainly important in the health sector, but also puts serious limitations on the reuse of data [3]
One issue is clearly under-researched; the organisational aspect of hospital analytics, which deals with the managerial (and to some extent the clinical) use and benefits. Although there is a body of research within strategic management of commercial health organisations [4], the organisation and culture of hospitals are naturally focused on medical treatment. Therefore, we have much less knowledge on how to organise and use analytics, than we have on the technical and application issues. For instance, we know that analytics is more than simply the technology solutions, but what this actually means in a hospital is less clear. We also know little about which governance regime that is effective; should it be centralised or distributed?
Our lens to understand this topic in more depth is analytics capability, which we broadly understand as the ability to produce relevant information, and benefit from analytics [5]. In this explorative study we investigate what is takes to establish an analytics capability in a large hospital, and our research questions are:
-
What are the requirements for an analytics capability for a hospital?
-
How do we organize an analytics capability for a hospital?
We proceed by reviewing the current research on analytics in general, and the particular challenge of hospital analytics. Then we present our method and empirical evidence, which is a case study in Norway. Our findings highlights that the analytics capability is much more than the technology; it is the network of analytics technology, an analytics team and the medical, administrative and clinical decision makers.
2 Relevant Research
We conduct our research within the information infrastructure perspective [6], which focuses on socio-technical networks, not single systems. This stream of literature have mostly been occupied with evolution of the user base through bootstrapping, network economics and cultivation, and to a lesser degree investigated how re-use of the information contributes to inform patterns of production and performance.
2.1 Analytics
Analytics is defined as “the extensive use of data, statistical and quantitative analysis, explanatory and predictive models, and fact-based management to drive decisions and actions” [7:9–10]. The definition highlights two important aspects; it is extensive use of data (i.e. Big Data, not simply using quantitative material) and the aim is to drive decisions and actions (not simply providing background information for managers).
Both the media and research have provided spectacular examples of how analytics (and “Big Data”) have provided new insights and competitive advantage. Global platform firms, such as Google and Facebook, base their multisided business models on analytics, and in the public sector police and tax authorities use analytics to uncover new patterns and insights. In industrial and retail environments, process analytics provides a tool for on-going improvement and optimisation [7].
In order to leverage analytics, it is commonly assumed that an organisation needs to develop an analytics capability, [5] defined as “the ability to utilize resources to perform a business analytics task, based on the interaction between IT assets and other firm resources” [5:4]. To help practitioners and researchers to assess a particular instance, some analytics maturity frameworks have been introduced [5].
2.2 Hospital Analytics
Several researchers have pointed to the large potential of analytics within health care. Some uses are:
-
Medical research based on large datasets, such as images, medical signs and genomics data repositories [8, 9]
-
Clinical decision support including machine learning and AI solutions for IT supported clinical decision making [10] and ambient intelligence solutions [11]
-
Logistics, for instance flow of patients, and waiting lists [12]
-
Management, such as financial and process management [13, 14]
-
Quality management, such as key factors for patient satisfaction [15]
Despite these promises, the status of hospital analytics is generally poor; partly because of fragmented clinical systems and partly because of lack of analytics capacity [2]. In order to understand the issues in more depth we conducted a case study at a high-tech hospital in Norway.
3 Method and Case
The setting for our empirical research is Kalnes general hospital in Østfold County (near Oslo) in Norway. Østfold has about 300.000 inhabitants. The 85.500 square meters high-tech hospital opened in November 2015 and replaced the old Fredrikstad hospital. Kalnes has one of Norway’s largest emergency units in addition to general hospital functions such as delivery wards, clinical and surgical departments and psychiatry. Kalnes Hospital serves as an extreme case of our area of concern [16], because of the ambitious efforts to integrate and align clinical work processes and patient records keeping with novel innovative technology to support horizontal process innovation and coordination.
Our case study research approach is based on engaged scholarship [17, 18] inspired by an “insiders ontology” [19] where informants are not only sources of empirical data, but also helpful in constructing narratives and discuss theoretical and practical implications [17]. The approach requires a longitudinal perspective, with strong and trustful relationships between researchers and practitioners.
Our unit of analysis is the whole hospital, i.e. how analytics can exploit the whole digital infrastructure of the hospital. Selected cases are therefore hospitals that have a high degree of digitalisation. Such “extreme cases” are a prerequisite for developing a state-of-the-art analytical capability, and well suited to develop new theory [16].
3.1 Data Collection
From July 2016 to January 2018, we conducted 33 interviews, with CEO, CTO, process manager, analytics experts, clinicians, project leaders, technical experts and cleaning personnel as well as system suppliers. Round one started with interviews where Kalnes management and project leaders presented the main goals as well as the organizing of the IT oriented process innovation initiative. We proceeded by performing observations within the emergency unit and the health wards, where challenges related to process flow were addressed. We followed up with new interviews as well as analyses of documents on patient treatment regulations, political requirements from the regional health authorities and descriptions of the technical solutions. We also participated in local and regional meetings and workshops where findings, including ours, were discussed. Through this bottom-up-investigation, we identified coordinative actors, actors whose central role is to plan and coordinate the movement of patients and information across hospital departments, and were particularly interested in how they use IT to perform and coordinate their work.
In round two, we observed meetings at all levels, particularly the ones related to flow challenges, and where analytics was used in order to shed light on patterns of production and performance. Data was used extensively to inform decisions and solving concrete challenges (Tables 1 and 2).
3.2 Data Analysis
We first established a chronology of important events, before we investigated in detail what it takes to establish and maintain analytics activities. In particular, we analysed the interplays between the technologies in use, the analytics team and the various decision makers. From this we constructed a framework of the requirements needed for enabling analytic. Lastly, we analysed and assessed the organisation of the analytics activities.
3.3 Case Chronology
Background 2013–2016
Kalnes Hospital opened in 2015, but work had started already in 2013 to improve horizontal process performance. A work group with organizational workers as well as a number of external consultants modelled 65 work processes. Most of these work processes were sub-processes of 38 different clinical pathways. The Kalnes hospital management signed a contract with a supplier called Imatis. The Imatis solution included three main services:
-
A solution for patient self check-in and dealing with queues
-
A system for visualisation of patient flow and logistics, with whiteboards
-
A message broker for distribution of messages to mobile phones and other units
A separate group worked with the details of the Imatis solution and the integration between the package of EPR systems and Imatis to digitalize the processes. The “regional package” consisted of more than 300 applications, maintained and run by the regional IT Centre. The key applications were the electronic patient record (EPR) system, lab system, radiology system and chart and medication system. Because of slow progress, the governance of the start-up package was transferred from the big regional Digital Renewal program, to the Kalnes Hospital project in order to reach the deadline for the opening of the hospital in 2015. The Imatis, or lightweight solution, to support logistics and communication, was strongly supported by the management, and organized as a sub-project.
The solution used self check-in automats, mobile phones, tablets and electronic whiteboards, which were modelled in the processes. The hospital opened November 2015, and the start-up was, although successful, not without challenges. Kalnes was the first hospital in Norway that to this extent used a combination of process innovation technology – to improve patient flow – and the package of EPR systems feeding Imatis through a common interface. At the same time, the combination of these two system regimes enabled the organization to both improve the performance and the communication of the performance, and inspired the organization to strive for continual improvement. The improved transparency of horizontal processes has led to the establishment of collaborative arenas to discuss and find solutions to flow issues. A common aspect of these meetings is that they are short, around 10–15 min, and targeted, and they have become arenas for both identifying challenges and make decisions to deal with them.
The coming of analytics 2017–2018
The main reason for the relatively significant change from being merely occupied with the functional production, to strengthen the focus on horizontal performance, was “a deep feeling of crises related to the patient flow” [process director]. The waiting time at the emergency unit was over 5 h. In 2016, they found that, despite all the work on process innovation, there were few clear improvements in patient flow. Consequently, they had to address the challenges more systematically. They established several interdisciplinary work groups and corresponding arenas to discuss the specific challenges. Examples of such arenas and meetings are improvement teams, capacity meetings, interdisciplinary improvement meeting and weekly status meeting between process director and the teams. The point is to monitor and improve performance on several important areas.
-
Improved overview of performance related to interventions
-
Improve the overview of lag related to patients on waiting lists
-
Identify the amount of postponed interventions
-
The time of day when patients are being discharged
-
How long it takes to switch between interventions
-
Occupancy rate per department
The process director is occupied with underuse and overuse of resources in order to optimize performance. “Our main goal is to ensure even and secure patient flow”. But, what does it take to establish an analytic capability in order to reach this goal?
4 Findings
In this part, we will first describe the background for obtaining an analytics capability, that is, what does it take to establish, implement and maintain institutionalization of analytics? Then we describe insights from the particular inform and decision structure Kalnes have established through this work. By institutionalization, we mean that the practice of performing analytics is implemented into the organization as regular activities.
4.1 Analytics Capability
In 2016 when Kalnes acknowledged that the work on process innovation - although successful in changing the digital infrastructure and make more use of information - had made little impact on the flow performance, they decided to establish an analytics capability within the organisation.
The first move was to organise an analytics team, consisting of two data scientists and two clinicians. The team established an ETA structure (Fig. 2) where data from clinical core systems and Imatis was loaded into a file system/transformation system and transformed into analytical data. The task may seem trivial, but neither DIPS nor MetaVision – two of the core clinical systems - had APIs from where structured and ‘ready-made’ data could be extracted. MetaVision’s APIs were inaccessible, and data thus had to be delivered from the supplier to the analytics team. DIPS data sometimes had to be restructured and contextualized to make sense together with Imatis data. The Imatis data were easier to access and extract because of the suppliers interest in making data available across particular sections of the hospital.
In addition, this structured ETA system had to be maintained and developed further. The continuous work with data gave qualified insight into how data might be brought together in order to provide a foundation for decision. In this way, the analytics team became a significant expertise on patterns of performance.
The second part of the analytics capability was the establishment of improvement teams, consisting of clinicians and managers. The key task for the improvement teams was to make use of the available analytics to take better decisions. They met regularly to make sense of the data and to take running decisions based on them. At the meetings, important actors from the respective wards participated in the interdisciplinary meetings, provided explanations, and suggested possible solutions to solve a challenge. We offer, below, a more detailed description of how this was organised.
4.2 Organisation of Analytics Process
Five different teams were established as the decision-making part of the analytics capability, as shown in Table 3.
One of the meetings was the interdisciplinary improvement meeting, chaired by the process director and held every Friday from 08:45. It is a short and intensive meeting, only 15–20 min. The participants were the managers from the different clinical departments. A typical meeting followed this structure:
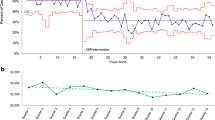
The analytics expert presented data from both Imatis and EPR systems like Dips and Metavision (see Fig. 2) to create tailored graphs and columns showing trends and fluctuations. The graphs and numbers belonged mainly within three categories of data: time spent on particular processes as well as how long patients are admitted; the number of patients admitted to each ward including corridors, and the performance of the housekeeping department regarding cleaning and dietary services from the order is received to completion. All in all the tailored data provides a good basis for making decisions.
The clinical managers (doctors and nurses) would often interrupt to ask questions: Why is the trend not reflecting the influenza season? Can I have details specified only for my own department? And sometimes protests: This graph shows that our throughput efficiency is lower than the others, but the numbers do not reflect the particulars of our process.
The Process director might take decisions at the table. An example was a decision to admit more than one patient to each patient rooms during the influenza season. Another is to order particular rooms to be cleaned at particular times, for example at 2 pm when the number of tasks may create performance bottlenecks. The ward managers provide contexts for why the numbers is as they are, and what they have done to deal with them. The ward managers might also suggest particular solutions to each challenge, but also request further data to gain more insight. A ward manager said that
I need an overview of the NIV patients (patients with copd, multiple sclerosis or in need of a respirator) and how much each room is used by the particular patient category. To improve the performance i need more data. Facts are very important.
The point with the meeting, then, was cooperation across different sections. As the clinical doctors may “be afraid to lose their beds” [ward manager], some of the data may create tensions. This because logistics might threaten the integrity of medical decisions provided by the clinicians. “I only show numbers, but they must be displayed carefully so that clinicians are not provoked,” the analytic expert comments. He continued saying that the meeting has improved the cooperation in that “they understand each other’s problems”. He also claimed that the “understanding of the mechanisms leading to the trends is increased by repeated focus.” “Although it is hard constantly seeking improvement, we know that it takes time to build a culture for doing this.” The process director agreed, and claimed that “the meeting has given [the organizational actors] an ability to see the whole that was absent earlier.”
5 Discussion
In this part, we return to our research questions. According to Davenport [7: 9-10], analytics is the “extensive use of data, statistical and quantitative analysis, explanatory and predictive models, and fact-based management to drive decisions and actions.” Framing this within infrastructure theory [6], we are interested in the relations between the elements described in Sect. 4.1. What does it take to connect the elements in a way that establish an analytic capability? This will be addressed in Sect. 5.1 where we ask: What are the requirements for an analytics capability for a hospital? In the Sect. 5.2 we respond to the question: How do we organize an analytics capability for a hospital?
5.1 What Are the Requirements for an Analytics Capability for a Hospital?
Cosic [5] define analytics capability as “the ability to utilize resources to perform a business analytics task, based on the interaction between IT assets and other firm resources”. It is not enough to have all the elements; they have to be connected. Their value as analytic capability rests on the establishment of a network between them, enabling interaction.
In Sect. 4.1, we identified three central elements in establishing an analytic capability at Kalnes hospital. Figure 3 illustrates our overall argument.
The technology is important, in that structured and systematic data collection and analyses are at the core of decision-making. A core element is the ETL process, which transforms transaction data into actionable information.
Then, the analytics team, in that data has to be carved out, re-structured, and appropriated in order to be comparable. This team really has to understand the detailed context and relationship between detailed clinical data in order to enable a qualified synchronization of these data across wards and sections.
The third element, the decision makers, comprises in addition to the medical expertise, also the administrative and strategic management. The administrative management is distributed within the organization, for example as ward managers, or as workflow coordinator within and between wards. The top management like the process director or research director both take important decision to overarching challenges, and contributes to fulfilling the performance goals set by strategic management.
At Kalnes, these elements, although organized separately, flourished through the interaction. The interdisciplinary improvement meeting where graphs and patterns identified through technology, interpreted and visualized by the analytics team, and displayed in front of decision makers who respond to challenges, demonstrates the advanced capability of Kalnes to use data in the decision-making.
The common team of improved performance, aligning medical and logistical interests served by precise and detailed data on performance and production, contributed strongly to bind the elements in the triangle together. This was a foundation for the institutionalization of analytics: the ability to implement, adopt and maintain analytics for a longer time.
Thus, the analytics capability is much more than the technology; it is the on-going network of analytics technology (including the clinical systems), an analytics team and the medical and administrative decision makers. We regard this as an evolving information infrastructure.
5.2 How Do We Organize an Analytics Capability for a Hospital?
Research has shown a significant potential for improvement of patient flow by visual analytics, but creation of shared understandings and shared interpretations are essential for the success of the analytics project [1]. We believe that the key to this is continuous engagement with stakeholders, and in particular we think it is essential to institutionalize the co-operation as a learning process.
How should analytics be formally organised? Davenport [7] recommended a centralised approach, because analytics requires specialised competence. Also, a centralised unit is more likely to prevail over time. Our findings support this, as the success of the analytics group at Kalnes corroborate. However, this point should not be overstated. Our evidence indicates that the most important success factor is the close and regular co-operation between the analytics team and the decision makers. This is because visual analytics is highly contextual [1], and requires continuous interaction and learning. As our case clearly shows, institutionalization of analytics depends on something more than merely the technological extraction of sophisticated data. In the case of Kalnes, we do not believe that the hospital would have been well served by a regional analytics solution, which would have been too far from the decision makers.
At Kalnes hospital the network of technology, analytics team and decision makers worked so closely that they had to be positioned with proximity. This kept the analytics work more intensive, with shorter loops from needed information was requested until it was received, and with more agility in the performance. The elements in the analytics network need to be kept close so that the challenges are taken seriously and solutions may be suggested right away. However, there is a need to maintain a balance between managerial goals and local adaptation. This also because an important overlaying aspect is the importance of management participating in analytics. To motivate for the continuous analytics process, the management has to make sure that institutional performance is actually improved, and that necessary resources are given to the teams and actors. There is consequently a continuous interaction between top management, ward management and clinicians in order to enable and leverage the data-driven organisation.
5.3 Conclusion and Limitations
This study deals with the practical and theoretical challenge of establishing an analytics capability at hospitals. Through a case study at a high-tech hospital in Norway, we offer two contributions. First, the analytics capability is much more than the technology; it is the network of analytics technology, an analytics team and the medical and administrative decision makers. Second, we identify institutionalization, both organizationally and temporally, of the analytics process as the key success factor.
In this study, we have not interviewed patients or relatives, but focuses on the interplay of managers, clinicians and IT staff. The paper is primarily practice-oriented, and we acknowledge that a deeper and more precise investigation into analytics capability will require more quantification and more precise criteria for measuring such capabilities.
References
Fitzgerald, J.A., Dadich, A.: Using visual analytics to improve hospital scheduling and patient flow. J. Theor. Appl. Electron. Commer. Res. 4(2), 20–30 (2009)
Raghupathi, W., Raghupathi, V.: Big data analytics in healthcare: promise and potential. Health Inf. Sci. Syst. 2, 3 (2014)
Bellala, G., Huberman, B.A.: Securing Private Data Sharing in Multi-Party Analytics, 29 July 2016. SSRN: https://ssrn.com/abstract=2816140 or https://doi.org/10.2139/ssrn.2816140
Swayne, L.E., Duncan, W.J., Ginter, P.M.: Strategic Management of Health Care Organizations. Wiley, Chichester (2012)
Cosic, R., Shanks, G., Maynard, S.: Towards a business analytics capability maturity model. In: Proceeding of 23rd Australasian Conference on Information Systems, Geelon (2012)
Hanseth, O., Lyytinen, K.: Design theory for dynamic complexity in information infrastructures: the case of building internet. JIT 25(1), 1–19 (2010)
Davenport, T.H.: Enterprise Analytics. Pearson, Upper Saddle River (2014)
Belle, A., Thiagarajan, R., Reza Soroushmehr, S.M., Navidi, F., Beard, D.A., Najarian, K.: Big data analytics in healthcare. Biomed. Res. Int. 2015, 16 (2015). https://doi.org/10.1155/2015/370194. Article ID 370194
Wang, Y., Kung, L., Wang, W.Y.C., Cegielski, C.G.: An integrated big data analytics-enabled transformation model: application to health care. Inf. Manage. 55(1), 64–79 (2018)
Kannampallil, T.G., Franklin, A., Mishra, R., Almoosa, K.F., Cohen, T., Patel, V.L.: Understanding the nature of information seeking behavior in critical care: implications for the design of health information technology. Artif. Intell. Med. 57(1), 21–29 (2013)
Acampora, G, Cook, D.J., Rashidi, P., Vasilakos, A.V.: A survey on ambient intelligence in healthcare. In: Proceedings of the IEEE, vol. 101, no. 12 (2013)
Bygstad, B., Bergquist, M.: Horizontal affordances for patient centred care in hospitals. In: Proceedings of the 51st Hawaii International Conference on System Sciences (2018)
Agarwal, R., Gao, G., DesRoches, C., Jha, A.K.: Research commentary—the digital transformation of healthcare: current status and the road ahead. Inf. Syst. Res. 21(4), 796–809 (2010)
Fichman, R.G., Kohli, R., Krishnan, R.: The role of information systems in healthcare: current research and future trends. Inf. Syst. Res. 22(3), 419–428 (2011)
Anhang Price, R., et al.: Examining the role of patient experience surveys in measuring health care quality. Med. Care Res. Rev. 71(5), 522–554 (2014)
Gerring, J.: Case Study Research: Principles and Practices. Cambridge University Press, Cambridge (2006)
Bygstad, B., Munkvold, B.E.: Exploring the role of informants in interpretive case studies research in IS. J. Inf. Technol. 26, 32–45 (2011)
Mathiassen, L.: Designing engaged scholarship: from real-world problems to research publications. Engaged Manage. Rev. 1, 2 (2017)
Garud, R., Kumaraswamy, A., Karnøe, P.: Path dependence or path creation. J. Manage. Stud. 47(4), 760–774 (2010)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 IFIP International Federation for Information Processing
About this paper
Cite this paper
Bygstad, B., Øvrelid, E., Lie, T. (2019). Establishing an Analytics Capability in a Hospital. In: Elbanna, A., Dwivedi, Y., Bunker, D., Wastell, D. (eds) Smart Working, Living and Organising. TDIT 2018. IFIP Advances in Information and Communication Technology, vol 533. Springer, Cham. https://doi.org/10.1007/978-3-030-04315-5_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-04315-5_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-04314-8
Online ISBN: 978-3-030-04315-5
eBook Packages: Computer ScienceComputer Science (R0)