Abstract
PET-CT is now the mainstay for imaging lymphoma patients. The complimentary nature of the metabolic and anatomic information provided by a PET-CT examination has become an essential component of patient management, complimenting clinical and laboratory criteria used in staging, restaging, and therapy monitoring. The nature of a particular lymphoma subtype and the patient’s clinical presentation will determine the extent PET-CT imaging is best employed in a particular patient’s management.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Standardize Uptake Value
- Mantle Cell Lymphoma
- Graft Versus Host Disease
- International Prognostic Index
- Central Nervous System Lymphoma
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Effective combination therapy protocols can produce prolonged disease-free and overall survival in the majority of patients with Hodgkin’s disease (HD) and certain subtypes of non-Hodgkin’s lymphoma (NHL). Even in patients with advanced-stage HD and aggressive NHL, complete remission can be achieved in up to 75% of patients at first presentation with proper management [1, 2]. Accurate risk factor profiling using staging and established predictors of outcome, including gene profiting as well as effective restaging and response evaluation during or following therapy are prerequisites in the determination of optimal treatment. This may also lead to selection of a proper subset of patients in whom radiation therapy (RT) could be avoided. Anatomic imaging modalities such as computed tomography (CT) lack the ability to identify lymphoma in normal size lymph nodes and are unable to differentiate nodes which are enlarged due to other therapy-related benign causes [3]. Similar to CT, magnetic resonance imaging (MRI) findings are not specific for viable tumor and cannot differentiate active lymphoma from infectious or inflammatory processes including radiation fibrosis [4, 5]. Ga-67 scintigraphy, despite its proven prognostic value as a predictor of therapy response during or after therapy, suffers from low spatial resolution, lack of specificity, low sensitivity in infradiaphragmatic lesions, and low-grade lymphoma [6, 7]. Ga-67 scintigraphy has now largely been superseded by positron emission tomography imaging using [F-18]fluorodeoxyglucose (FDG PET).
FDG PET has become an integral part of the initial staging and response evaluation algorithm for lymphoma, providing vital information regarding tumor biology and metabolism. There is now convincing evidence that FDG PET is a more accurate imaging modality in the staging and evaluation of treatment response in lymphomas compared to conventional imaging techniques [8–20], including both CT and Ga-67 scintigraphy. Furthermore, persistent FDG uptake during and after chemotherapy has proven highly sensitive and specific in the differentiation of residual viable disease from benign posttherapy changes. This superior feature can potentially alter patient management and outcome by identifying the subset of patients requiring additional therapy or a change in treatment regimen. The accuracy of FDG PET imaging has significantly improved with the recent introduction of combined modality PET-CT [19]. PET-CT provides a comprehensive examination that combines morphologic diagnosis and functional/metabolic information in the same imaging session [21].
This chapter summarizes the data on the proven and potential utility of FDG PET imaging in combination with CT at staging, restaging, and predicting response to therapy as well as the current limitations of this combined imaging modality in patients with lymphoma.
Pathologic and Clinical Classification of Lymphomas
The current lymphoma classification system is based on both morphologic and biologic characteristics of lymphomas. The Revised European-American Classification of Lymphoid Neoplasms (REAL) system was developed in 1994 to incorporate morphology, clinical features, immunophenotype and cytogenetics [22]. The World Health Organization (WHO) classification subsequently updated the REAL system with minor modifications [23]. This integrated system – WHO/REAL classification – is currently in clinical use for both HD and NHL [24]. Despite the complexity and diversity of this integrated system, lymphomas are traditionally subdivided into two broad categories: Hodgkin’s disease (HD) and non-Hodgkin’s lymphomas (NHL). Also for practical purposes NHL can be classified into indolent (low-grade) and aggressive lymphomas. NHL accounts for more than 85% of the lymphomas. Aggressive lymphomas constitute approximately 60% of NHL series, while indolent lymphomas account for approximately 40% of new diagnoses. The vast majority of NHL (∼90%) are of B-cell origin. Early stage lymphoma is curable in greater than 75% of patients; however, advanced stage disease is curable in only 50% of patients [25].
HD accounts for 10–15% of lymphomas and composed of two different entities, classical HD representing 95% of cases, and nodular lymphocyte-predominant HD that makes up 5% of cases. Classical HD is further subdivided into nodular sclerosis (accounts for 65–80% of all cases), mixed cellularity, lymphocyte rich, and lymphocyte depletion types. With polychemotherapy the cure rate for HD is greater than 80% of patients with first-line therapy. Patients with nodular lymphocyte-predominant HD, usually present with isolated peripheral lymph node involvement. These patients have a clinical course resembling NHL with an indolent growth pattern with single and multiple relapses as well as late relapses. Diffuse large cell lymphoma, most common type of aggressive NHL, sometimes occurs concurrently or subsequently in patients with nodular lymphocyte-predominant HD with a cumulative risk of 9% at 10 years [26].
Staging of Lymphomas
The TNM (tumor, node, metastasis) system is not applicable in lymphomas because usually the specific origin of tumor is not clearly identified. The Ann Arbor staging system remains the most widely used staging system which was introduced for HD and a modified version of this system is adopted for the use in NHL (Table 22.1) [27, 28]. There are basically four stages of lymphomas as demonstrated in Table 22.1. Subscript suffixes are affixed to any stage for more detailed staging. The constitutional symptoms (B) (Fever higher than 100.5°F, night sweats, and weight loss) and bulky disease (X) (tumor >10 cm) portend worse prognosis for each stage of HD. The subscript is “E” denotes extranodal disease contiguous or proximal to the known nodal site: Stages I and IIA are considered early-stage disease although up to 35% of patients with early-stage HD have occult abdominal nodal or splenic involvement [29]. Stages IIB (particularly bulky), III, and IV are considered advanced-stage disease.
Staging Workup of Lymphomas
Recommended procedures for a thorough staging workup include medical history and physical examination, laboratory procedures (complete blood cell count with differential, peripheral blood smear, lactate dehydrogenase, β2 microglobulin, serum protein electrophoresis, sedimentation rate, and blood chemistries), bone marrow biopsy in patients with B symptoms and advanced stage disease. The imaging studies typically include chest radiograph, chest, abdomen, and pelvis CT, and may also involve ultrasonography, endoscopy, and MRI, and lately whole-body FDG PET. Ga-67 SPECT imaging can still be used, although it has been replaced by FDG PET imaging in most centers. Other studies, including organ biopsy and CSF sampling, are considered in certain clinical situations.
Role of Imaging in Management of Lymphoma
Aggressive NHL and HD
At initial staging, an accurate and objective imaging modality is of particular importance in guiding therapeutic approach, especially the use of radiation therapy (RT). Although staging is clinically important, studies of immunophenotype and molecular genetics are essential to refine diagnosis and management, particularly in NHL. Until recently, extended field RT has been considered the standard treatment for early stage HD. There is, however, an increasing trend to employ chemotherapy and most groups adopted a strategy using short duration chemotherapy combined with involved field RT (restricted to involved lymph nodes) in this group of patients [30]. Advanced stage (stages III–IV) disease is invariably treated with multiple chemotherapy protocols. Thus, staging still holds its critical position in the management of lymphoma even with the latest changes in therapeutic approach. In patients with HD or aggressive NHL (mostly DLCL), the therapy objective is the complete eradication of disease while minimizing adverse short- or long-term complications of therapy, particularly related to the RT. Unnecessary use of RT could result in excess toxicity such as secondary malignancies and cardiac disease, while appropriate use can potentially decrease risk of disease recurrence and allow for shorter courses of chemotherapy cycles attendant reduction of chemotherapy toxicity [31]. Hence, segregating patients who could achieve cure without the need of RT is an important management strategy involving imaging.
Perhaps the most clinically relevant issue surrounding aggressive NHL and HD is the ability to perform prognostic determination. FDG PET findings can be an independent predictor of tumor response or complementary to the established prognostic factors; international prognostic index in NHL and international prognostic score in HD, and potentially contribute to, or single-handedly, direct a change in management. For this concept to be of practical value, however, alternative treatment options should be available and also establishment of prognosis as favorable or poor must be followed up with a treatment change that is necessary and sufficiently effective to improve outcomes.
Mantle Cell Lymphoma
Mantle cell lymphoma is a rare and distinct entity of lymphomas which accounts for 5–10% of all lymphoma cases. Patients usually present with advanced stage disease (Ann Arbor stages II and IV) with generalized lymphadenopathy and extranodal involvement (90%) (BM, liver spleen GIT) similar to other indolent lymphomas. The prognosis is invariably poor, however, due to aggressive and progressive clinical course with no curative conventional therapy generally available. Imaging for staging purposes does not have major influence on management due to disseminated nature of disease; however, evaluation of therapy response is important for potential therapeutic alterations. PET-CT may have a niche in the posttherapy period for evaluating residual masses and therapy response. Nonetheless, in the absence of effective alternative therapy options, the role for imaging in the management of mantle cell lymphoma is relatively limited.
Indolent (Low-Grade) NHL
Low-grade lymphomas are incurable with current treatment modalities. The treatment in indolent lymphomas is defined by clinical symptoms rather than disease extent; therefore, determination of extent of disease or therapy response may not lead to improved outcomes. With current therapeutic strategies, identification of additional disease sites using PET-CT in the staging of indolent NHL is not an important determinant of management, as 80–90% of patients initially present with advanced-stage disease with generalized nodal and extranodal disease (mainly BM) involvement. New approaches combining classical dose-intense chemotherapy with “tumor-specific” antibody targeting may lead to a survival benefit [32], potentially increasing the role of imaging in the management of low-grade NHL. Nonetheless, imaging currently has a limited role in the management of indolent lymphoma owing to specific features of the disease. A characteristic of indolent lymphomas is the phenomenon of spontaneous regression. Such spontaneous regression is usually partial and short-lived, and imaging findings can help determine the disease status which may prompt therapy during the active course of disease. Other characteristics of indolent lymphomas include synchronous discordant lymphomas (20–30% of newly diagnosed patients) and transformation to an aggressive subtype (30–50%) during the first 10 years following diagnosis [33]. In these situations, PET-CT has a definite role to determine the sites of discordant lymphomas as well as transformation for biopsy guidance and subsequent effective management.
PET-CT for Diagnosis and Staging of Lymphoma
The diagnosis of lymphoma requires adequate tissue for histopathologic diagnosis, and imaging can direct the site of biopsy when such is not clinically obvious. Accurate initial staging of patients with lymphoma can be crucial for determining treatment strategy, including the use of RT. Advanced-stage HD or NHL is treated with combination chemotherapy. Early-stage HD patients (stage I and II) are generally divided into favorable or unfavorable groups based on prognostic factors. The patients in the favorable group are managed with treatment reduction strategies; the patients in the unfavorable group are managed with combined modality therapy.
Traditionally the imaging modality of choice for the diagnosis and staging of lymphoma has been CT, in some instances accompanied by sonography or endoscopy. MRI is a competitive anatomic imaging technique which can provide images of the abdomen of somewhat comparable diagnostic quality with the advent of faster acquisition sequences, particularly the turbo spin-echo (TSA) or fast spin-echo sequences. Additionally, MRI offers advantages including better tissue discrimination, lack of ionizing radiation and use of contrast agents with less risk of systemic effects [34–36]. Nevertheless, the diagnostic accuracy of both CT and MRI depends largely on lymph node enlargement and multiplicity. Thus, false-negative results occur in normal size lymph nodes that harbor lymphoma and lymph nodes that are enlarged due to reactive changes can give rise to false-positive findings.
FDG PET as a metabolic imaging modality and more recently PET-CT as a combined morphologic and metabolic modality has been integrated into the diagnostic algorithm of staging for both HD and NHL. The findings of FDG PET are usually concordant with those of CT at initial staging, even though, PET detects additional tumor sites and also can upstage or downstage disease in some patients (Fig. 22.1) [10–12]. One should also realize, however, that although the additional information derived from an imaging modality can upstage or downstage disease, the findings may not lead to management changes unless early stage disease is upstaged to advanced stage disease or vice versa.
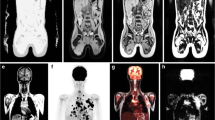
Hodgkin’s lymphoma on left supraclavicular lymph node biopsy. Anterior FDG PET (a) maximum intensity projection image (MIP) shows mediastinal FDG uptake as well as small foci in the left axilla, left supraclavicular fossa, and in the upper abdomen. Coronal contrast enhanced CT (b) and FDG PET (c) images demonstrate the confluent bulky intensely FDG avid mediastinal soft tissue and a 1.2-cm FDG avid left supraclavicular lymph node (arrow). Transaxial contrast-enhanced CT (d) and FDG PET (e) images demonstrate an FDG avid 1.3-cm lymph node just below the gastroesophageal junction (arrow) and FDG avid nodal mass at the anterior cardiophrenic sulcus (arrowhead). The cardiophrenic nodal involvement is still considered above the diaphragm disease; however the gastrohepatic ligament node involvement, not readily apparent on CT images alone, is below the diaphragm and renders the patient stage III
Nodal Lymphoma
HD and NHL have different presentations both in the chest and abdomen, including different morphologic and metabolic features (Tables 22.2 and 22.3). Lymph node involvement is a central feature of diseases.
CT in Nodal Lymphoma
At initial staging, CT is usually performed with oral and intravenous contrast and in the follow-up evaluation is performed without the use of intravenous contrast at some centers. Most mediastinal lymph nodes can be detected without intravenous contrast, but are more reliably measured on contrast enhanced scans. Inclusion of the neck in the CT or MRI evaluation yields a more accurate staging as lymphoma, particularly with HD, which accounts for 10% of the head and neck tumors. When lymphoma involves cervical lymph nodes they can be either enlarged or numerous. In general cervical, axillary, and mediastinal lymph nodes are considered abnormal when their short axis diameter exceeds 10 mm. This size criterion of 6 mm has been advocated for prevascular, internal mammary, posterior mediastinal, and anterior diaphragmatic lymph nodes [37].
In patients with HD, thoracic disease, mediastinal nodes, particularly those in the superior mediastinal location, is more frequently involved (≥85%), while intrathoracic lymphoma in NHL is an extension of widespread disease process (Tables 22.2 and 22.3). Mediastinal HD is characterized by the presence of a discrete anterior superior mediastinal mass with surface lobulation due to involvement and coalescence of multiple lymph nodes (Fig. 22.2), while characteristic features of mediastinal aggressive NHL, mainly diffuse large cell type, included regular contour and absence of associated cervical and abdominal lymphadenopathy [38]. In general, extranodal involvement of the lung parenchyma, pleura, and pericardium is more common with NHL than with HD because of the frequent vascular invasion and hematogenous spread associated with the former [39]. Although CT and MRI are equally sensitive in the evaluation of mediastinal involvement, CT is usually preferred for its availability and relatively lower cost. MRI is spared for patients with iodine allergies and poor renal function. CT plays a significant role for recognizing bulky mediastinal HD as these patients have worse prognosis due to higher risk of disease recurrence compared to those with nonbulky disease. Bulky disease is defined as a mediastinal mass exceeding one third of the chest diameter or greater than 10 cm in diameter.
Nodular sclerosing Hodgkin’s lymphoma. Anterior FDG PET MIP image (a) shows bulky mediastinal disease and left supraclavicular lymph node involvement. Transaxial contrast-enhanced CT (b) and FDG PET-CT fusion (c) images of the chest reveal surface lobulation of the mediastinal mass due to coalescence of enlarging lymph nodes as typically seen with Hodgkin’s lymphoma. Transaxial contrast enhanced CT (d) and FDG PET (e) images of the abdomen demonstrate two small foci of FDG tracer uptake in the spleen (arrows), only seen as subtle findings on the FDG PET MIP image, and without corresponding abnormality on the portal venous phase contrast enhanced CT images, corresponding to splenic involvement, rendering the patient stage III
In the abdomen, lymph node enlargement of greater than 10 mm, most often retroperitoneal, are generally considered pathologic. It should be noted that with HD, retroperitoneal lymph nodes may be involved without enlargement compromising the sensitivity of CT scans with a reported false-negative rate of 20–80% [40]. With NHL, bulky and usually confluent retroperitoneal lymph node involvement is more common (Fig. 22.3) and mesenteric disease is seen in approximately 50% of the patients, unlike in HD (∼15%) [36]. Lymph node calcification at initial presentation is very rare. MRI with a T2-weighted TSE sequence is considered equivalent to multidetector helical CT and represents an alternative morphologic method of examination in abdominal lymphoma [35].
Non-Hodgkin’s lymphoma. Anterior FDG PET MIP image (a) shows multiple foci of widely distributed nodal disease including lymph node involvement in cervical, axillary, mediastinal, mesenteric, and retroperitoneal nodal basins. Unlike classic Hodgkin’s lymphoma, disease is not centripetally extending from a dominant focus. Transaxial contrast enhanced CT (b) and FDG PET-CT fusion (c) images reveal enlarged FDG avid right common iliac lymph nodes and nonenlarged FDG avid left common iliac and mesenteric lymph nodes. Aside from the right iliac lymphadenopathy, the involved lymph nodes elsewhere are, at most, borderline enlarged, and thus largely diagnosed as disease involvement based on the abnormal FDG tracer uptake depicted on the FDG PET images
FDG PET in Nodal Lymphoma
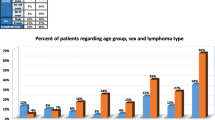
Although FDG accumulates in the majority of lymphomas, because of the differences in immunophenotype and cytogenetics, glucose utilization may vary as evidenced by FDG uptake characteristics among various subtypes (Table 22.4). In a review of 172 patients, FDG PET detected disease in at least one site in 94% of patients, including 100% of patients with aggressive NHL (diffuse large cell lymphoma) and 98% of patients with HD. In contrast, FDG PET detected disease in only 67% of marginal zone and 40% of peripheral T-cell lymphoma [41]. Our experience has been in line with these findings with regard to sensitivity of FDG PET in different subtypes of lymphoma.
The lower typical FDG tracer uptake in certain indolent lymphomas diminishes the sensitivity advantage of FDG PET images relative to conventional morphologic criteria such as used by CT. Nonetheless, several studies have reported a potential role for FDG PET in staging low-grade NHL, particularly follicular cell and nodal marginal zone lymphoma [8, 11, 14, 20, 42, 43]. In contrast to marginal zone lymphoma, however, FDG PET is considerably less reliable in the detection of extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT) where FDG tracer uptake in involved lymph nodes is usually very low to undetectable (Fig. 22.4) [43, 44]. These differences support other recent data suggesting that nodal and extranodal marginal zone lymphomas may be distinctive entities rather than nodal lymphoma being a more advanced stage of MALT [45].
Non-Hodgkin’s lymphoma on left axillary lymph node biopsy, found consistent with marginal zone of mucosa associated lymphoid tissue (MALT). Anterior FDG PET MIP image (a) shows no appreciable abnormal FDG tracer uptake on the whole torso image. Transaxial contrast enhanced CT; (b) and FDG PET (c) images reveal subcarinal and right hilar lymphadenopathy which is associated with no abnormal FDG tracer uptake. Transaxial contrast-enhanced CT (d) and FDG PET (e) images of the upper abdomen reveal bulky para celiac and porta hepatic lymphadenopathy as well as a large mass in the spleen, none of which is associated with appreciable abnormal FDG tracer uptake
Small lymphocytic subtype (SLL) is also typically associated with low to undetectable FDG tracer uptake in involved lymph nodes resulting in diminished sensitivity relative to CT [42]. SLL and chronic lymphocytic leukemia (CLL) are closely related and in WHO classification wherein SLL is considered as the tissue infiltrate of CLL; this disease is referred to as CLL/SLL. In this entity, the most consistent clinical finding is diffuse lymphadenopathy and the corresponding FDG PET finding is varying degrees (usually low to undetectable) of FDG uptake (Fig. 22.5). A diminished sensitivity for small lymphocytic lymphomas is interestingly seen with Ga-67 imaging as well [46].
Non-Hodgkin’s lymphoma, small lymphocyte subtype. Patient with history of chronic lymphocytic leukemia presenting with axillary lymphadenopathy. Anterior FDG PET MIP image (a) shows only faint FDG tracer uptake in the bulky axillary lymphadenopathy and subtle increased FDG tracer activity in the bulky retroperitoneal lymphadenopathy. Coronal contrast-enhanced CT (b) and FDG PET(c) images demonstrate the extensive discrete enlarged retroperitoneal and axially lymph nodes with very little associated FDG tracer uptake
Mantle cell lymphoma is a rare type subentity of lymphoma associated with aggressive clinical behavior, but with molecular features of low-grade lymphomas. The diagnostic sensitivity of FDG PET for mantle cell lymphoma is high, reported to be 90–100% [43, 47]. In this subtype FDG uptake characteristics are more or less similar to that seen in follicular low-grade lymphoma. Also in this patient population, one should be mindful of extranodal involvement, which is found in approximately 90% of patients and may involve unusual areas such as skin, GIT, breast, and lung (Fig. 22.6).
Cutaneous involvement of non-Hodgkin’s lymphoma (mantle cell lymphoma). Transaxial contrast-enhanced CT (a) and FDG PET-CT fusion image (b) demonstrates intense FDG tracer uptake by the soft tissue centered in the skin over the right anterior chest. Such extranodal involvement is commonly seen with mantle cell lymphoma and can also include gastrointestinal tract, breast, and lung
On initial staging the CT and FDG PET findings will be in agreement for the majority of cases, although the FDG PET images have been reported to manifest additional disease sites in about 10–28% of patients with aggressive NHL or HD (10–17). Overall, FDG PET is more sensitive and specific than CT in identifying lymphoma involved lymph nodes, except in the case of indolent lymphomas, which demonstrate low level or absent FDG tracer uptake [9, 48–52]. In general, FDG PET has been superior to CT alone in the detection of nodal disease except in the abdomen and pelvis, in which the two methods have produced equivalent results. However, combined PET-CT systems can improve the sensitivity and specificity of the FDG PET image further, particularly in the neck, abdomen and pelvis. In a small study of 19 patients with nodal disease (either HD or aggressive NHL) evaluated by both PET-CT and separately acquired contrast enhanced CT studies [53], PET-CT demonstrated additional lesions in four patients which were not detected on contrast-enhanced CT, while contrast-enhanced CT did not depict any nodal involvement that was undetectable on PET-CT [53]. As noted, however, when the lymphoma subtype is one with characteristically low or absent FDG tracer uptake, such as MALT, CLL/SLL, peripheral T cell, and low-grade follicular lymphoma, the CT findings based on lymph node size will be the chief criterion for nodal involvement.
Regarding size criteria for abnormal lymph nodes, in a study comparing one-, two-, and three-dimensional measurements of nodal involvement in lymphoma, there were no significant differences in staging between the three groups, although three-dimensional methods were most accurate and reproducible [54]. Regarding FDG PET criteria for abnormal lymph nodes, tracer uptake greater than mediastinal background activity is considered abnormal, with tracer uptake greater than liver tracer activity definitely abnormal. By semiquantitative measurement of standardized uptake value (SUV), this has generally corresponded to SUV measured values greater than 2–2.5 in the earlier literature. It should be noted that due to rapid changes in scanner design, image acquisition protocols, and image reconstruction methods, measured uptake values referred to as SUVs are no longer reliably comparable.
Differences in FDG tracer uptake observed between aggressive and indolent lymphoma expressed semiquantitatively by SUVs have been reported; SUV = 11.8 ± 4.7 for aggressive lymphomas and SUV = 6.4 ± 5.3 for indolent lymphomas [8, 11, 14, 20]. Our experience has been such that the mean SUVs are 4.5 ± 2.0 (range, 1.5–9.5) in indolent lymphomas and 12.5 ± 5.5 (range, 3.0–36) in aggressive lymphomas with a significant overlap in small lesions (unpublished data). Segregating SUVs into two distinct categories for the differentiation of aggressive and indolent lymphomas may be accurate for majority of cases, but not for all due to the high and low outliers for both groups. Also one of the inherent problems is the inaccurate SUV measurements in small tumors and the need for specification of standardization parameters.
In cases of transformation to a more aggressive subtype of lymphoma FDG uptake characteristics may help identify an area of high-grade transformation in indolent disease and thereby influence management (Fig. 22.7). While the capability of FDG PET has not been prospectively assessed for this purpose, based on the disparate SUVs between high- and low-grade lymphomas, FDG PET may offer clinically valuable information by directing biopsy to the sites with highest FDG tracer uptake relative to other sites of disease involvement.
Transformation to high grade lymphoma. Patient with original diagnosis of low grade follicular lymphoma treated 15 years prior, now presents with left sided abdominal pain. Anterior FDG PET MIP image (a) reveals intense foci of FDG tracer uptake in the abdomen and pelvis, not in an entirely nodal distribution. Transaxial contrast-enhanced CT (b), FDG PET (c), and FDG PET-CT fusion (d) images reveal the residual retroperitoneal soft tissue from the original lymphoma encasing the aorta is without any FDG tracer uptake, but enhancing soft tissue nodules (arrows) are seen in the lower posterior chest wall musculature that are intensely FDG avid. Transaxial contrast enhanced CT (e) and FDG PET-CT (f) fusion images at the level of the pelvis reveal both lymph node involvement and extranodal involvement in the abdominal wall musculature. Such recurrent disease presenting with extranodal involvement will typically be of higher grade than the original disease and requires biopsy for histopathological classification of the new disease. PET-CT findings identify sites of high-grade transformation most suitable for biopsy
Extranodal Lymphoma
The exact definition of extranodal lymphoma remains controversial, but generally extranodal definition indicates presentation outside lymph node areas (i.e., extranodal lesion is the presenting site and constitutes the predominant disease bulk). Extranodal NHL can arise in any organ and encompasses a heterogeneous group of disease presentations. The most common extranodal sites include: central nervous system (CNS), gastrointestinal tract (GIT), especially stomach, Waldeyer’s ring (palatine and lingual tonsils/tongue base, nasopharyngeal lymphoid tissue), liver, spleen, bone, and bone marrow (BM). HD usually involves extranodal sites by direct invasion from nodal sites. The therapeutic strategy in patients with primary extranodal lymphomas is in general analogous to that of nodal lymphomas. In stage I and II disease local therapy is administered, however, detection of occult distant disease necessitates the use of chemotherapy. In state III or IV disease the mainstay of treatment is chemotherapy.
CT and MRI in Extranodal Lymphoma
In the head and neck, the most common site for extranodal lymphoma involvement is the Waldeyer’s ring (Fig. 22.8). Lymphoma of the head and neck cannot be distinguished from squamous cell cancer although necrosis is more common in the latter and calcification is rare with lymphoma. This is followed by sinus, nasal cavity, nodal sites, salivary glands (mostly parotid), and orbit. Almost 50% of extranodal head and neck lymphoma is associated with nodal disease. Patients with Waldeyer’s ring involvement have a slightly worse prognosis [55].
Extranodal lymphoma involving Waldeyer’s ring in the neck. Anterior (a) and lateral (b) FDG PET MIP images reveal intense FDG tracer uptake in the right parapharyngeal region with moderately low level physiologic FDG tracer activity seen elsewhere in Waldeyer’s ring. Low level FDG tracer uptake is seen in cervical lymph nodes as well. On the transaxial contrast-enhanced CT image (c) the mass in the right palatine tonsil is discernable by nonenhancing asymmetric soft tissue which is intensely FDG avid on the corresponding FDG PET image (d) normal physiologic FDG tracer activity in the left palatine tonsil is seen (arrowhead), as well as low level tracer activity in a left level II cervical lymph node (small arrow) due to unrelated benign inflammatory response
The gastrointestinal tract can be involved by primary NHL or by extension of nodal or adjacent organ involvement of NHL or HD (Fig. 22.9). The most common site is the stomach accounting for 50% of the gastrointestinal tract lymphoma presentations. Generally gastric lymphoma cannot be differentiated from gastric carcinoma, although luminal obstruction is uncommon with lymphoma due to lack of fibrous tissue response [56]. Low-grade primary gastric NHL of the MALT type is a common gastrointestinal tract lymphoma and there is a connection between this type of lymphoma with Helicobacter pylori infection [57]. In the small intestine, aneurysmal dilatation may be seen due to transmural extension of lymphoma, but differentiation from other malignant processes is not easy unless it is associated with bulky lymphadenopathy. The most common site for small intestinal lymphoma is the ileum; however, it may also involve the proximal jejunum particularly in association with celiac disease [58]. Colonic involvement is not common, but may occur in the cecum and rectum.
High-grade diffuse B cell lymphoma involving small bowel. Transaxial contrast enhanced CT (a) and FDG PET-CT fusion (b) images demonstrate extensive soft tissue thickening of a segment of duodenum that is associated with intense abnormal FDG tracer uptake. Lymphomatous involvement of bowel typically is extensive before obstructive symptoms occur
Lymphomatous involvement can be seen in the BM or the cortex of the bone. Bone and BM involvement is more common in NHL (especially in low-grade lymphoma) than in HD and confers stage IV disease. MRI is more sensitive than biopsy in detecting BM infiltration due to sampling errors associated with biopsy. It is becoming now feasible to routinely assess the entire marrow using MRI; however, in the follow-up period, persistent posttherapy MRI abnormalities may give rise to false positive results [59]. Cortical bone involvement can be primary or secondary, the former is usually of NHL type. Primary bone lymphoma has a tendency to involve the metaphyseal regions of the appendicular skeleton while secondary bone lymphoma usually involves the spine. In patients with bone involvement by direct extension from adjacent nodal disease, as it happens in HD, stage does not change. Bone involvement of HD is more often sclerotic (∼50%) and NHL is osteolytic (∼80%). This condition is denoted as “E.” In patients with both BM and adjacent soft tissue involvement, MRI is preferred over CT; however, assessment of cortical bone integrity is performed with CT for better definition of disease.
Primary CNS lymphoma, which is exclusively of the NHL type (>80% B cell), is more frequently seen in immunocompromised patients, including patients with AIDS and those with prior organ transplantation; however, it can also occur in immunocompetent patients [60]. CT and MRI generally provide findings that are suggestive but not conclusive for CNS lymphoma [61]. The most frequent locations are supratentorial brain, including cerebral hemispheres, corpus callosum, basal ganglia, and rarely cerebellum and spinal cord [62]. Although MR perfusion imaging has been reported to distinguish between AIDS-associated CNS lymphoma and toxoplasmosis, imaging characteristics can be similar in both, and accurate differentiation between these two diseases still remains challenging.
The spleen is more frequently involved with lymphoma than is the liver. Approximately 30% of patients with either NHL or HD have splenic involvement while only up to 9% patients with HD and 14% patients with NHL have hepatic involvement [63]. The liver involvement is rare without the association of splenic lymphoma. In about one third of the time lymphoma involvement can be seen in normal size spleens [64]. CT can detect splenic lesions only when there are focal macroscopic lesions or substantial splenomegaly. Nodular disease is usually associated with aggressive NHL and diffuse disease with low-grade NHL [65].
FDG PET in Extranodal Lymphoma
A multitude of studies have reported that FDG PET may provide more information about the extent of disease in cases with extranodal lymphoma compared to CT alone [11, 15, 18, 66].
FDG PET can differentiate primary lymphomas of the CNS from infectious processes, with a reported accuracy of 89% [67, 68]. Distinguishing infectious etiology such as toxoplasmosis can be a challenge for morphologic imaging studies, including CT and MRI, particularly in patients with AIDS. Due to the low sensitivity and specificity of polymerase chain reaction test for toxoplasmosis and Epstein-Barr virus titers for lymphoma, patients with AIDS and CNS lesions are empirically treated with pyrimethamine and sulfadiazine for 2–4 weeks. Essentially, a lesion with an FDG uptake higher than the adjacent gray matter indicates a malignant process which should be biopsied for confirmation rather than empirically treated as infectious. T1-201 is also known as a valuable imaging tool in the differentiation of CNS lymphoma from infectious causes, especially toxoplasmosis [69]. There are no systematic prospective data comparing T1-201 findings with those of FDG PET in the evaluation of CNS lymphoma, however, in few anecdotal cases we have observed that the sensitivity of FDG PET appears to be better than T1-201 imaging in the detection of CNS lymphoma. Difficulty arises, however, when CNS lymphoma undergoes necrosis or is below the resolution limits of PET systems (<8 mm).
The detection of BM involvement identifies a group of high-risk patients and changes disease management; hence, this is particularly important in early stage patients given the trend toward less intensive treatment in this group of patients (Fig. 22.10). The incidence of BM involvement at diagnosis varies according to the type of lymphoma. In general, the incidence is very low in patients with HD (as low as 1–2%), while it is commonly observed in low-grade lymphoma (mainly follicular cell subtype) (60–70%), chronic lymphocytic leukemia, and mantle cell lymphoma (90–100%). In aggressive NHL (mainly diffuse large cell lymphoma), BM infiltration is seen in 25–40% of patients [70]. BM biopsy is the mainstay of BM evaluation despite its association with a high rate of false-negative findings due to sampling errors. MRI is especially useful in detecting BM involvement; however, its sensitivity is much higher than its specificity and thus benign entities such as hemangiomas and inflammatory processes can easily mimic lymphoma. Overall, focal FDG uptake suggests pathological BM activity, a pattern more commonly seen in HD patients (Fig. 22.11). In aggressive NHL, the degree of BM involvement may range from a few cells to complete marrow replacement. In cases with the latter condition, FDG uptake is usually diffuse and somewhat heterogeneous. Diffusely increased FDG uptake is also observed in patients with BM hyperplasia, particularly following administration of colony stimulating factors (e.g., G-CSF) (Fig. 22.12) [71, 72].
Extranodal lymphoma. Anterior FDG PET MIP image (a) reveals abnormal FDG tracer uptake corresponding to a retroperitoneal nodal mass and extensive multiple foci of disease in the skeleton, liver, and spleen. Coronal contrast enhanced CT (b) and FDG PET (c) images show the 3-cm precaval lymph node mass which is intensely FDG avid, and multiple foci of abnormal FDG tracer uptake in the skeleton, and the liver and spleen with subtle corresponding findings on the portal venous–enhanced CT images of the liver and spleen, but no corresponding CT findings in the involved skeleton. Transaxial contrast-enhanced CT (d), FDG PET (e), and FDG PET-CT fusion images (f) reveal the osseous involvement in the right sacrum and left ileum are without discernable sclerotic or lytic abnormalities, including at the anterior cortex of the right sacrum where there is clear extension of soft tissue beyond the cortex (arrow). Osseous involvement of lymphoma is almost always marrow based and often without appreciable CT findings, despite extensive abnormal tracer uptake depicted on the FDG PET images. The disseminated involvement of extralymphatic organs renders the patient stage IV
Hodgkin’s lymphoma with osseous involvement. Anterior FDG PET MIP image (a) demonstrates abnormal FDG tracer uptake corresponding to mediastinal lymphadenopathy and bilateral supraclavicular lymph nodes, and intense FDG tracer uptake at the T12 vertebral body and in the right ileum. Sagittal CT (b) and FDG PET (c) images reveal diffuse sclerosis in the T12 thoracic vertebral body and intense uniform FDG tracer uptake throughout the vertebral body. Transaxial CT (d) and FDG PET (e) images reveal mixed lytic and sclerotic changes in the region of intense FDG tracer uptake in the right ileum (arrow). Osseous involvement of Hodgkin’s lymphoma more typically will have sclerotic changes on the CT images
Diffuse bone marrow hypermetabolism secondary to colony-stimulating factor on anterior FDG PET MIP image. Bone marrow stimulated by hematopoietic stimulation factors used in conjunction with chemotherapy can be very intense but uniform. Osseous lymphomatous involvement is usually heterogenous, but when extensive can be relatively uniform
While several studies reported that FDG PET is an effective means for the detection of extranodal lymphoma, the sensitivity to detect BM infiltration is usually limited to about 80%, regardless of the subtype of lymphoma [41, 43, 73, 74]. In patients with negative BM biopsy, FDG PET may reveal focal BM infiltration is present remote to the biopsy site owing to the virtue of evaluating the entire body at one acquisition. Nevertheless, a minimal degree of BM involvement can result in false-negative findings on FDG PET due to the inherent resolution limits of FDG PET imaging [18, 73, 74].
Bone marrow involvement of lymphoma should not be confused with primary bone lymphoma which is a separate entity and accounts for less than 5% of all primary bone tumors. Although there is no series of cases performed using FDG PET, our experience is that FDG avidly accumulates in all primary bone lesions or osseous extension of lymphoma of advanced-stage disease unlike bone marrow involvement.
Splenic involvement by lymphoma is more sensitively detected on FDG PET images than CT [11, 15], or conventional Gallium-67 imaging [75]. Both focal and diffuse involvement can be seen on FDG PET images even when contrast-enhanced CT is normal (Fig. 22.13). Certain hemopoietic stimulants used in chemotherapy regimens, however, can cause diffuse splenic FDG uptake as well as diffuse bone marrow FDG activity. With the advent of combined PET-CT imaging, accuracy in the detection of extranodal lymphoma is advanced by the complementary strengths of the two modalities. In a small series involving 19 patients comparing PET-CT with non–contrast-enhanced CT to conventional fully optimized contrast-enhanced CT alone, the PET-CT detected extranodal disease (bone and splenic involvements) in three patients while separately acquired contrast-enhanced CT was false-negative at these sites. However, in one patient, contrast-enhanced CT revealed small bowel involvement while the non–contrast-enhanced PET-CT was false-negative [53]. Since PET-CT studies have now evolved to more widely include intravenous contrast administration, the fully complementary nature of combined PET-CT examination in the detection of extranodal involvement of lymphoma is realized.
Follicular B cell lymphoma with splenic involvement. Anterior FDG PET MIP image (a) reveals intense heterogenous FDG tracer uptake in the spleen as well as lymph node involvement above and below the diaphragm, including bulky retroperitoneal disease. Transaxial contrast-enhanced CT (b) and FDG PET (c) images demonstrate diffusely increased FDG tracer uptake throughout the spleen with additional multiple intense foci of abnormal FDG tracer uptake. Subtle corresponding regions of decreased attenuation are seen on the portal venous phase contrast-enhanced CT images. Lymphomatous involvement of the spleen can manifest as a spleen with no parenchymal abnormalities on the CT images, including contrast-enhanced CT images (d), but with uniform intense abnormal FDG tracer activity on the FDG PET images (e)
FDG PET Versus Ga-67 Imaging
There is no comparative study using PET-CT and Ga-67 imaging in the same lymphoma population; however, and FDG PET has been shown to have superior sensitivity to Ga-67 scintigraphy and provide superior incremental value when combined with conventional diagnostic methods [76–80]. The discrepancy in the detection sensitivity between Ga-67 and FDG PET imaging has recently been shown to be independent of the disease volume, location, and histology in both nodal and extranodal disease. The discrepancy in the detection sensitivity between these two radiotracers can be explained not only by the superior counting statistics and spatial resolution of PET tomograph technology, but also by biologic differences considering the significant disparities in the mechanism of uptake of Ga-67 and FDG [80, 81]. Consequently, at present, FDG PET, particularly PET-CT, has largely downgraded Ga-67 imaging to an infection imaging agent from its past position as a staging or restaging modality in HD or aggressive NHL.
Influence of PET-CT on Patient Management at Initial Staging
As noted previously, accurate staging is more clinically relevant in aggressive NHL and HD than in indolent and mantle cell lymphoma, as the latter pair are associated with advanced-stage disease in a vast majority of patients. Even in the aggressive lymphomas, one should realize that not all stage changes as a result of PET-CT findings would translate into changes in therapeutic strategy. In routine practice, the stage category is usually altered within the same risk category (early stage vs advanced stage) and thus does not lead to management changes, but if additional information obtained from FDG PET, upstages early stage disease to advanced stage or vice versa, and therapy may be changed accordingly. Hence, the additional information provided by FDG PET is felt to be more useful in patients who are diagnosed with early stage disease than in advanced stage disease as treatment strategy may be altered by detection of unexpected disease sites in the former patient population not in the latter [82].
The superior sensitivity of FDG PET has been reported to lead to a change in disease stage in 8–48% of patients with untreated NHL and HD by virtue of revealing additional disease sites not revealed on anatomic imaging that were confirmed by either biopsy or long-term clinical follow-up [9, 17, 48–50, 83–85]. Based on the significance of change in stage for therapeutic strategy, FDG PET findings may result in intra or intermodality treatment modifications in 8–25% of HD or aggressive NHL patients [17, 49, 50, 83–86].
The most important imaging data derived influence on therapy would be the accurate separation of patients into favorable and unfavorable risk categories, especially in the early-stage HD patient population. The relevant therapeutic changes in early-stage disease with favorable prognostic factors group include treatment reduction strategies, essentially shorter courses of chemotherapy rather than a longer course as exclusive treatment, as opposed to a shorter course of chemotherapy followed by radiation therapy.
PET-CT for Restaging and Evaluationof Therapy Response
Following therapy, evaluation of residual disease and the efficacy of therapy is crucial when alternative therapeutic strategies exist, so that intramodality or intermodality treatment changes can be made to increase progression-free or overall survival. In early stage lymphoma (aggressive NHL or HD) up to 90% of patients respond to therapy; however, advanced stage lymphoma confer poor prognosis with a cure rate of less than 50% in newly diagnosed patients [87, 88]. Assessment of therapy response is therefore, more important in patients with advanced stage disease than with early stage. Also one important issue is that the treatment strategy for aggressive NHL is determined based upon immunophenotype and molecular genetics of the tumor rather than the anatomic extent alone. Aggressive NHL is treated exclusively with chemotherapy except in some cases local therapy may be added. Thus in this patient population, the primary role for imaging is the assessment of therapy response.
CT in the Posttherapy Evaluationof Lymphoma
Evaluation of treatment response using CT can be quite challenging. Differences in slice thickness and inconsistencies in the use of intravenous contrast may render the comparisons difficult. Following therapy, the mass attenuation values of the lymph nodes decreases with or without overall reduction in lymph node size in responding patients; however, there is no established standard for an accurate categorization of responders and nonresponders based on CT criteria. Achieving a complete response, which is defined as complete disappearance of the tumor mass, is the goal of cytotoxic therapy. However, failure to completely eradicate tumor mass with chemotherapy does not always correlate with persistent tumor cells or unfavorable prognosis [89]. This dilemma on anatomic imaging has been recognized in the response criteria for both HD and NHL [90, 91]. Both systems designate residual masses of unclear etiology as CRu, or unconfirmed/uncertain complete responses due to inherent uncertainty associated with posttherapy residual CT masses. Naturally, further and aggressive treatment in patients with benign posttherapy masses only increases morbidity and risk of second malignancies [31]. The patients with HD are at a higher risk of developing solid tumors years after therapy as a long-term side effect of combination chemotherapy and radiotherapy. New masses discovered more than 10 years after therapy in the lung, thyroid, breast, and stomach should be considered as de novo primary tumors and must be verified by biopsy [92].
In patients with bulky lymphoma, chemotherapy followed by RT is the conventional treatment approach in those with residual posttherapy masses. Radiation related tissue changes usually appear within 3–6 months after completion of RT with a presentation of ground glass opacities confined to the mantle radiation ports. Acute changes eventually disappear after 6 months, usually replaced by chronic changes in the ensuing 18 months, presenting as retraction or traction bronchiectasis and mediastinal fibrosis which may resemble granulomatous disease but they are usually symmetrical and confined to the mantle port [93].
FDG PET in the Posttherapy Evaluationof Lymphoma
As many as 50–80% of patients with HD and 30% of those with NHL will have residual masses after treatment. However, only a small percentage (∼15–20%) of these patients relapse. A multitude of studies have demonstrated that FDG PET is an effective imaging modality and more accurate than CT alone in the differentiation of posttherapy inert masses from active residual disease (Fig. 22.14), as well as monitoring response to therapy [13, 14, 86, 94–101].
Compete metabolic response of diffuse large B-cell non-Hodgkin’s lymphoma to chemotherapy with ametabolic residual scarring. Anterior FDG PET MIP image (a) pre-chemotherapy demonstrates intense abnormal FDG tracer activity corresponding to extensive mesenteric lymphadenopathy as well as involvement of axillary and inguinal lymph nodes. The posttherapy anterior FDG PET MIP image (b) reveals complete resolution of all abnormal FDG tracer uptake, with normal physiologic tracer activity distribution. Coronal contrast-enhanced CT (c) and FDG PET images (d) performed prior to therapy reveal the extensive mesenteric lymph node involvement with a conglomerate mass as well as an involved left axillary lymph node. The posttherapy coronal contrast-enhanced CT (e) and FDG PET (f) images demonstrate the residual soft tissue (arrows) along the superior mesenteric vein is entirely without any abnormal FDG tracer activity, indicating this is residual scar tissue, without metabolically active macroscopic lymphoma
FDG PET has been consistently reported to identify residual disease and/or preclinical relapse during the follow-up period (Fig. 22.15) [13, 14, 86, 94–101]. Despite reported high negative predictive values of greater than 90% obtained FDG PET by various investigators, false-negative findings are inevitable in cases with residual microscopic disease. Nevertheless, positive predictive value of FDG PET, also on the order of 90%, should be regarded more vital in the context of identifying patients who need immediate therapy changes or additional treatment after first-line therapy.In this group of patients, FDG PET could also avoid unnecessary further therapy in patients who achieve complete response to chemotherapy. One major concern that has not been addressed adequately, however, is the definition of patient population who would require further treatment with RT in the presence of false-negative findings associated with undetectable low-burden disease.
Incomplete metabolic response of Hodgkin’s lymphoma to chemotherapy. Anterior FDG PET MIP (a) prechemotherapy demonstrates intense abnormal FDG tracer activity corresponding to disease involving bulky mediastinal lymphadenopathy, bilateral lower cervical, and supraclavicular nodal involvement, an isolated right subdiaphragmatic lymph node, as well as focal involvement of the spleen. The posttherapy shallow left anterior oblique FDG PET MIP image (b) reveals complete resolution of all abnormal FDG tracer uptake, except a conspicuous single focus or abnormal FDG tracer uptake in the right mediastinum (arrow). There is additionally on the posttherapy FDG PET diffuse increased bone marrow FDG tracer uptake reflecting the use of hematopoietic stimulants in the chemotherapy regimen. Coronal contrast-enhanced CT (c) and FDG PET (d) images prechemotherapy reveal the intensely FDG avid mediastinal and supraclavicular lymphadenopathy and an intense focus of FDG tracer activity in the spleen The postchemotherapy coronal contrast-enhanced CT (e) and FDG PET (f) images show complete resolution of the lymphadenopathy and of the splenic lesion, with the exception of a 2-cm residual right mediastinal lymph node interposed (arrow) between the superior vena cava and ascending aorta, which maintains intense abnormal FDG tracer uptake, indicating the residual abnormal soft tissue is remaining viable lymphoma
In summary, negative FDG PET findings in areas corresponding to persistent posttherapy masses usually indicate posttreatment fibrosis. Nevertheless, false-negative results can be obtained for small lesions that are below the detection limits of current PET tomographs (<5–6 mm) or diffusely distributed microscopic disease. False-positive FDG PET findings can occasionally be obtained in infectious or inflammatory processes, however, the pattern of FDG uptake in these situations is usually recognizable and can be differentiated in most cased, especially when CT findings are taken into account, with the notable exception of granulomatous disease coexisting with lymphoma. Posttherapy FDG tracer accumulation in the region of original disease should be recognized as a compelling evidence for further therapy, however, owing to the associated high positive predictive value (90%) for residual viable disease.
Prediction of Therapy Outcome After Completion of Therapy
Criteria based on clinical, imaging, and laboratory findings which allow for risk stratification have been developed and validated for HD, known as the international prognostic score (IPS), and for NHL, known as the international prognostic index (IPI) [90, 101]. The IPS for HD (Table 22.5) is based on seven adverse factors, while the IPI, the most widely used system for aggressive NHL (Table 22.6), predicts the risk of recurrence and overall survival by taking into account five adverse factors [102]. In this regard, sequential FDG PET imaging has a role in the determination of tumor response rates [16, 95–99, 103, 104]. For example, in patients categorized as high risk for recurrence by IPI or IPS criteria, recurrent lymphoma should be anticipated in almost all patients with posttherapy residual abnormal FDG tracer uptake and in slightly under half of those with residual posttherapy CT masses [16, 97, 103].
Combined Modality Therapy Including Radiation Therapy
The other important management issue is the avoidance of RT, especially in the HD population. The use of RT is associated with a short-term survival advantage; however, RT has an adverse effect on long-term survival due to significantly increased risk for many late complications such as development of a second malignancy or cardiovascular disease [31, 93]. Ongoing trials investigating treatment reduction, including reduction of radiation dose or radiation field size, and abbreviated chemotherapy, are intended to reduce RT treatment-related long-term complications [31]. PET-CT may well be a valuable imaging tool to risk stratify these patients and select the subgroups that will or not require RT followed by chemotherapy, based on the identification of residual viable disease on the FDG PET images.
In a mixed (HD and aggressive NHL) series of 44 patients presenting with bulky abdominal lymphoma, at the end of chemotherapy with or without RT, all those with positive FDG tracer uptake in residual masses eventually succumbed to disease relapse, while only 4% relapse occurred among those that had residual masses but no associated abnormal FDG tracer uptake [99].
Persistent FDG uptake after first-line chemotherapy was predictive of residual or recurrent disease after completion of first-line chemotherapy for aggressive NHL in a prospective study [103]. The negative predictive value of posttherapy FDG PET findings was 80% with a mean follow-up of approximately 24 months, while positive predictive value was 100% with a mean disease-free survival of only 3 months. This study highlights false-negative FDG PET findings can be as high as 20% probably due to microscopic residual disease. In the small number of studies evaluating exclusively patients with HD, after the first-line treatment, disease-free survival was significantly shorter for the PET positive group at 0–4% and longer for the PET negative group at 85–93% [105, 106]. These results provide grounds for future trials to evaluate the prognosis in patients who are administered abbreviated courses of chemotherapy with or without combined RT given at lower radiation doses in cases with negative FDG PET results.
High-dose Chemotherapy and Autologous Stem Cell Transplantation
For patients with relapsed lymphoma, high-dose chemotherapy (HDT) with autologous stem cell transplantation (SCT) is the treatment of choice resulting in 5-year event-free survival rates of up to 45% [107]. The outcomes after HDT/SCT, however, can be significantly different between chemosensitive and chemoresistant patients. Hence differentiation of these two patient populations is important for the identification of the optimal group that would benefit from HDT/SCT. Patients with less than 25% decrease in SUV measured FDG tracer uptake in the lymphoma after HDT had a progressive disease course while among those with more than 25% decrease in SUVs, 86% remained in complete remission [108]. Similarly, another study found none of the patients with complete resolution of FDG tracer uptake in response to the initial course of therapy before HDT/SCT relapsed subsequently [109], while seven or eight patients with a moderate or high FDG tracer uptake before HDT/SCT relapsed [109].
Early Prediction of Response During Therapy
The rapidity of response to therapy regimen has been suggested to be a good predictor of the ultimate response to that particular therapy regimen [110–112]. Patients with aggressive NHL who experience a partial response or who respond slowly to front-line chemotherapy have been reported to have a poor prognosis. In this group of patients, early introduction of dose-intensive salvage therapy before the development of progressive disease may be beneficial [111]. Since chemotherapy effect on tumor metabolic activity precedes the tumor size reduction, early evaluation of therapy response would be primarily based on the metabolic images.
Based on in vitro studies, FDG tracer uptake is proportional to the viable tumor cells, and viable tumor cells decrease early during effective chemotherapy. In a clinical study, 7 days after initiation of chemotherapy, tumor glucose metabolism as measured by FDG tracer uptake decreased by at least 74% in responding patients [113]. All lesions displayed a further decrease of FDG tracer uptake resulting in a total decrease of 83–96% from baseline to day 42 after initiation of therapy. There was no indication initial enhancement of FDG uptake as suggested by data from cell culture and animal studies. Further, the FDG tracer uptake values at day 42 were lower in patients with long-term remission compared to patients with early relapse [113]. Similarly, persistent FDG tracer uptake in the lymphoma after two to four cycles of chemotherapy was reported to predict poor progression-free survival in patients with aggressive NHL and HD [105, 106]. Persistent FDG uptake after a few cycles of chemotherapy was associated with relapse rates ranging from 70% to 100% while the relapse rate in patients with complete disappearance of FDG tracer uptake during therapy was as low as 8%. In one study, at midtreatment, none of the patients with persistent abnormal FDG tracer uptake achieved a durable complete remission, while 84% of patients with negative FDG PET results remained in complete remission after a median follow-up of approximately 3 years [106]. In this study, multivariate analysis revealed that FDG PET at midtreatment was a stronger prognostic factor for progression free survival compared with IPI criteria.
Could FDG PET predict as early as after one cycle of chemotherapy? It has been demonstrated that FDG PET after one cycle of chemotherapy was predictive of long-term outcome in aggressive NHL and HD [104, 114]. In one series by Kostakoglu et al., patients with persistent FDG uptake after one cycle of chemotherapy had a shorter progression free survival (median, 5 months) than those with negative FDG PET results (progression-free survival medians not reached) after a follow-up of 36 months [104]. The positive and negative predictive values for FDG PET after one cycle chemotherapy were 90% and 85%, respectively. However, these results were obtained on a dual-head camera system which lacks sensitivity and therefore may give rise false-negative results. Recently, in a study by the same investigators, using a dedicated full ring PET system, all patients (17 patients) with no appreciable FDG uptake after one cycle of chemotherapy remained in complete remission after a follow-up of 12 months, whereas 90% of patients with a positive FDG PET result had a relapse or persistent disease requiring further therapy, including bone marrow transplantation. These are promising results; nonetheless, these data should be interpreted with caution until larger, multi-institutional studies with a longer follow-up period are executed. Additionally, comparison of the predictive value of early FDG PET scanning to more conventional prognostic measures (such as the International Prognostic Index in aggressive lymphoma) as not yet been performed with sufficient patients to establish whether FDG PET derived early response criteria provides superior or complementary prognostic information.
If further studies confirm that persistent positive FDG PET results during therapy, preferably after one cycle, indicate a poor prognosis, one could consider an early change in therapy to a more aggressive approach (such as second-line chemotherapy and high-dose treatment with autologous stem cell transplant) early during the course of treatment (either before completion of a full course of initial chemotherapy or in first remission). However, the clinical benefit of such an approach, and whether this early change in therapy would improve upon a predicted outcome would require prospective testing in proper randomized clinical trials.
In conclusion, it appears that the superiority of FDG PET lies in its positive predictive value, especially early in the course of chemotherapy-based treatment of lymphoma, as to therapy resistance or failure. The negative predictive value of FDG PET, however, may not be as reliable as minimal residual disease, especially microscopic, that cannot be detected given the resolution limits of current PET tomographs. Thus, late relapses remain to be a possibility in patients with negative FDG PET results.
Comparison of FDG PET and Ga-67 Imagingin Posttherapy Evaluation
Ga-67 scintigraphy was the antecedent imaging modality to monitor response to chemotherapy in patients with lymphoma. However, with the proven advantages and strength of FDG PET imaging, Ga-67 scintigraphy is no longer widely used. There are only a few studies evaluating the potential of FDG and Ga-67 comparatively, in the posttherapy setting, but generally effective treatment sharply reduces tumor uptake of both Ga-67 and FDG activity within days and prior to volume response, whereas abnormal uptake of both Ga-67 and FDG persisted in treatment failure [115]. Nevertheless, the significantly higher sensitivity and specificity of FDG PET compared to Ga-67 scintigraphy for detection of nodal or extranodal lymphoma in both pretherapy and posttherapy setting has established FDG as the preferred metabolic tracer for lymphoma with Ga-67 scintigraphy in 93% versus 29%.
PET-CT systems provide important information particularly in the posttherapy setting; metabolic findings that are overlooked due to the subtlety of metabolic changes of FDG PET may result in the detection of residual disease after correlation with the simultaneously acquired and registered and aligned CT images. Furthermore, equivocal CT findings, which are suggestive of either recurrent tumor or posttherapy changes, can now be distinguished with the guidance of the additional information obtained from FDG PET images. In addition to diagnosis and staging and restaging of malignant disease, combined PET-CT is useful in planning radiation therapy and determining the optimum approach for CT-guided biopsy [21, 53]. Consequently, the addition of metabolic imaging can have a great effect on treatment in patients with a residual mass at the time of posttreatment evaluation.
Special Considerations with Lymphoma Imaging
Special considerations for imaging patients with lymphoma are summarized in Table 22.7.
Benign Lymphoproliferative Disorders
Benign lymphoproliferative disorders represent a spectrum of lymphoid abnormalities characterized by lymphocyte proliferation. LPD can be divided into two broad categories; benign and posttransplantation. The benign LPD most frequently manifest in the thorax, where the site can be the lymph nodes or in the bronchus associated lymphoid tissue of the lung [116]. Entities such as plasma cell granuloma, pseudolymphoma, posttransplant lymphoproliferative disorders, lymphoid interstitial pneumonia, and lymphomatoid granulomatosis involve the pulmonary parenchyma as a primary site of intrathoracic disease, while Castleman’s disease, infectious mononucleosis and angioimmunoblastic lymphadenopathy involve intrathoracic lymph nodes. It is important to differentiate the “benign” forms of LPD from the more common, aggressive lymphomas. Overall, intrathoracic disease confined to one compartment, either lymph nodes or lung parenchyma, implies a more benign etiology whereas multiple sites of disease, a malignant neoplasm. There is considerable overlap between benign LPD and NHL, especially in the immunocompromised patients. One might assume that the FDG uptake would be lower in this benign form of LPD than that seen in aggressive NHL and HD. Only anecdotal case reports are available regarding the FDG uptake patterns in Castleman’s disease in the literature [117, 118]. FDG accumulation in one of these case reports was modest (SUV: 6.2) in a hilar location and low in the other (SUV: 1.7–3.2) in a pelvic location. It is expected that in the indolent forms of NHL, the differentiation between benign LPD and lymphoma may not be possible. In the absence of a systematic study assessing FDG accumulation patterns, it is only speculative to discuss this topic; however, one must bear in mind that this category of diseases should be considered as a potential false-positive group among other granulomatous processes, especially in the posttherapy setting [119].
AIDS-Related Lymphoma
AIDS-related lymphomas, both NHL and HD, are characterized clinically by the presence of B symptoms (weight loss, night sweats, and fevers) at diagnosis in approximately 90%, advanced clinical stage with extranodal involvement in greater than 60% at presentation, and clinical aggressiveness with poor therapeutic outcomes. Extranodal involvement is a particularly distinctive feature, with the gastrointestinal tract being the most common location. Other sites of involvement include the central nervous system, the bone marrow, the oral cavity, the lungs, and the skin. Recently a primary effusion lymphoma (PEL) has been described in association with HIV. This rare lymphoma develops exclusively in serous body cavities (peritoneum, pleura, or pericardium) as a malignant effusion [120]. FDG PET findings follow the clinical presentation and CT findings with typically high levels of FDG tracer uptake due to the aggressive nature of these lymphomas.
Thymic Uptake
Following chemotherapy, thymic FDG uptake in young adults and pediatric patients is a known phenomenon and should not be mistaken with residual lymphoma, although at times differentiation between the two conditions may be challenging [121–123]. Thymic hyperplasia is a common phenomenon after treatment, especially in children, with an incidence of 16%. It has been proposed that this finding is due to an immunologic rebound phenomenon characterized by lymph follicles with large nuclear centers and infiltration of plasma cells following thymic aplasia secondary to steroid-induced apoptosis and inhibition of lymphocyte proliferation. Rebound thymic hyperplasia is associated with increased FDG tracer uptake and increased thymus volume. In children with a malignancy roughly 75% will have increased thymus FDG tracer uptake both prior to and following chemotherapy, although with a significant increase after therapy, while in young adults only about 5% will manifest increased thymic FDG uptake after chemotherapy [122, 123].
BM Uptake After Administration of Colony Stimulators
In patients with chemotherapy followed by bone marrow stimulants such as granulocyte colony-stimulating factor and granulocyte-macrophage colony-stimulating factor, the BM will have diffuse, intense increased FDG accumulation [71, 72]. Therefore, diffuse BM FDG uptake is commonly attributable to the effect of hematopoietic cytokines. Diffuse bone marrow FDG uptake can, however, also be caused by bone marrow involvement by lymphoma and at times this may be indistinguishable from hematopoietic cytokine-mediated FDG bone marrow uptake.
Posttransplantation Period
Bone marrow transplantation (BMT) and immunocompromised patients require special attention when interpreting images. Lymphoma patients after therapy, in particular after bone marrow transplantation, can develop cellular immunodeficiency until the transplanted marrow engrafts and creates new white blood cells. These patients are extremely susceptible to infections. Pulmonary infections are the most frequent complications in BMT recipients [124]. Idiopathic interstitial pneumonitis/ARDS, pneumocystis carinii, cytomegalovirus, aspergillus, and bacterial pneumonia are among the most common causes of infections [125]. Additionally, acute graft versus host disease (GVHD) often occurs during the first 3 months following an allogeneic BMT. To minimize the risk of graft rejection and GVHD, allogeneic BMT patients are given immunosuppressants to prevent GVHD before and after transplant. Use of these drugs, however, increases the risk of infection. Therefore, caution should be exercised when interpreting PET-CT images in immunocompromised patients as infectious/inflammatory lesions and granulomas can be falsely interpreted as persistent or recurrent tumor.
Conclusion
PET-CT is now the mainstay for imaging lymphoma patients. The complimentary nature of the metabolic and anatomic information provided by a PET-CT examination has become an essential component of patient management, complementing clinical and laboratory criteria used in staging, restaging, and therapy monitoring. As emphasized above, the nature of a particular lymphoma subtype and the patient’s clinical presentation will determine the extent PET-CT imaging is best employed in a particular patient’s management.
References
Canellos GP, Anderson JR, Propert KJ, et al. Chemotherapy of advanced Hodgkin’s disease with MOPP, ABVD, or MOPP alternating with ABVD. NEJM 1992;327:1478–1484.
Fisher RI, Gaynor ER, Dahlberg S, Oken MM, et al. Comparison of a standard regimen (CHOP) with three intensive chemotherapy regimens for advanced non-Hodgkin’s lymphoma. NEJM 1993;328:1002–1006.
Marshall WH Jr, Breiman RS, Harell GS, Glatstein E, Kaplan HS. Computed tomography of abdominal para-aortic lymph node disease: preliminary observation with a 6 second scanner. Am J Roentgenol 1977;128:759–764.
Bendini M, Zuiani C, Bazzocchi M, Dalpiaz G, Zaja F, Englaro E. Magnetic resonance imaging and 67Ga scan versus computed tomography in the staging and in the monitoring of mediastinal malignant lymphoma: a prospective pilot study. MAGMA 1996;4:213–224.
Nyman R, Forsgren G, Glimelius B. Long-term follow-up of residual mediastinal masses in treated Hodgkin’s disease using MR imaging. Acta Radiol 1996;37:323–326.
Front D, Bar-Shalom R, Mor M, et al. Hodgkin’s disease: prediction of outcome with 67Ga scintigraphy after one cycle of chemotherapy. Radiology 1999;210:487–491.
Front D, Bar-Shalom R, Mor M, et al. Aggressive non-Hodgkin lymphoma: early prediction of outcome with 67Ga scintigraphy. Radiology 2000;214:253–257.
Rodriguez M, Rehn S, Ahlstrom H, Sundstrom C, Glimelius B. Predicting malignancy grade with PET in non-Hodgkin’s lymphoma. J Nucl Med 1995,36:1790–1796.
Jerusalem G, Warland V, Najjar F, Paulus P, Fassotte MF, Fillet G, Rigo P. Whole-body 18F-FDG PET for the evaluation of patients with Hodgkin’s disease and non-Hodgkin’s lymphoma. Nucl Med Commun 1999;20:13–20.
Hoh CK, Glaspy J, Rosen P, et al. Whole-body FDG PET imaging for staging of Hodgkin’s disease and lymphoma. J Nucl Med 1997;38:343–348.
Thill R, Neuerburg J, Fabry U, et al. Comparison of findings with 18-FDG PET and CT in pretherapeutic staging of malignant lymphoma. Nuklearmedizin 1997;36:234–239.
Mainolfi C, Maurea S, Varrella P, Alaia C, Imparato C, Alfano B, Aate G, Bazzicalupo L. Positron emission tomography with fluorine-18-deoxyglucose in the staging and control of patients with lymphoma. Comparison with clinico-radiologic assessment. Radiol Med 1998;95:98–104.
Cremerius U, Fabry U, Neuerburg J, Zimny M, Osieka R, Buell. Positron emission tomography with 18F-FDG to detect residual disease after therapy for malignant lymphoma. Nucl Med Commun 1998;19:1055–1063.
Stumpe KD, Urbinelli M, Steinert HC, Glanzmann C, Buck A, von Schulthess GK. Whole-body positron emission tomography using fluorodeoxyglucose for staging of lymphoma: effectiveness and comparison with computed tomography. Eur J Nucl Med 1998;25:721–728.
Moog F, Bangerter M, Diederichs CG, Guhlmann A, Merkle E, Frickhofen N, Reske SN. Extranodal malignant lymphoma: detection with FDG PET versus CT. Radiology 1998;206:475–481.
Jerusalem G, Beguin Y, Fassotte MF, Najjar F, Paulus P, Rigo P, Fillet G. Whole-body positron emission tomography using 18F-fluorodeoxyglucose for post-treatment evaluation in Hodgkin’s disease and non-Hodgkin’s lymphoma has higher diagnostic and prognostic value than classical computed tomography scan imaging. Blood 1999;94:429–433.
Bangerter M, Kotzerke J, Griesshammer M, Elsner K, Reske SN, Bergmann L. Positron emission tomography with 18-fluorodeoxyglucose in the staging and follow-up of lymphoma in the chest. Acta Oncol 1999;38:799–804.
Wiedmann E, Baican B, Hertel A, et al. Positron emission tomography (PET) for staging and evaluation of response to treatment in patients with Hodgkin’s disease. Leuk Lymphoma 1999;34: 545–551.
Hany TF, Steinert HC, Goerres GW, Buck A, von Schulthess GK. PET diagnostic accuracy: improvement with in-line PET-CT system: initial results. Radiology 2002;225:575–581.
Kostakoglu L, Leonard JP, Kuji I, et al. Comparison of fluorine-18 fluorodeoxyglucose positron emission tomography and Ga-67 scintigraphy in evaluation of lymphoma. Cancer 2002;94:879–888.
Townsend DW, Beyer T. A combined PET/CT scanner: the path to true image fusion. Br J Radiol 2002;75:S24–30.
National Cancer Institute–sponsored study of classifications of non-Hodgkin’s lymphomas: summary and description of a working formulation for clinical usage. The Non-Hodgkin’s Lymphoma Pathologic Classification Project. Cancer 1982;49: 2112–2135.
Jaffe E, Harris N, Diebold J, Muller-Hermelink H-K. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues. A progress report. Am J Clin Pathol 1999;111(Suppl 1):S8–S12.
Harris N, Jaffe E, Diebold J, et al. The World Health Organization classification of hematological malignancies. Report of the Clinical Advisory Committee Meeting. Mod Pathol 2000;13:193–207.
Armitage JO. Treatment of non-Hodgkin’s lymphoma. NEJM 1993;328:1023–1030.
Orlandi E, Lazzarino M, Brusamolino E, Paulli M, Astori C, Magrini U, Bernasconi C. Nodular lymphocyte predominance Hodgkin’s disease: long-term observation reveals a continuous pattern of recurrence. Leuk Lymphoma 1997;26:359–368.
Lister TA, Crowther D, Sutcliffe SB, et al. Report of a committee convened to discuss the evaluation and staging of patients with Hodgkin’s disease: Cotswold meeting. J Clin Oncol 1989;7: 1630–1636
Rosenberg S. Validity of the Ann Arbor staging system classification from the non-Hodgkin’s lymphomas. Cancer Treat Rep 1977;61:1023–1027.
Leibenhaut MH, Hoppe RT, Efron B, Halpern J, Nelsen T, Rosenberg SA. Prognostic indicators of laparotomy findings in clinical stage I-II supradiaphragmatic Hodgkin’s disease. J Clin Oncol 1989;7:81–91.
Josting A, Diehl V. Current treatment strategies in early stage Hodgkin’s disease. Curr Treat Options Oncol 2003;4:297–305.
Ng AK, Bernardo MV, Weller E, et al. Second malignancy after Hodgkin disease treated with radiation therapy with or without chemotherapy: long-term risks and risk factors. Blood 2002;100: 1989–1996.
Cheson BD. Radioimmunotherapy of non-Hodgkin lymphomas. Blood 2003;101:391–398.
Winter JN, Gascoyne RD, Van Besien K. Low-grade lymphoma. Hematology 2004;1:203.
Hoane BR, Shields AF, Porter BA, et al. Comparison of initial lymphoma staging using computed tomography (CT) and magnetic resonance (MR) imaging. Am J Hematol 1994;47:100–105.
Jung G, Heindel W, von Bergwelt-Baildon M, et al. Abdominal lymphoma staging: is MR imaging with T2-weighted turbo-spin-echo sequence: a diagnostic alternative to contrast-enhanced spiral CT? J Comput Assist Tomogr 2000;24:783–787.
Ferrucci JT. Advances in abdominal MR imaging. RadioGraphics 1998;18:1569–1586.
North LB, Libshitz HI, Lorigan JG. Thoracic lymphoma. Radiol Clin North Am 1990;28:745–762.
Tateishi U, Muller NL, Johkoh T, Onishi Y, Arai Y, Satake M, Matsuno Y, Tobinai K. Primary mediastinal lymphoma: characteristic features of the various histological subtypes on CT. J Comput Assist Tomogr 2004;28:782–789.
Cazals-Hatem D, Lepage E, Brice P, et al. Primary mediastinal large B-cell lymphoma: a clinicopathologic study of 141 cases compared with 916 nonmediastinal large B-cell lymphomas – a GELA (“Groupe d’Etude des Lymphomas de l’Adulte”) study. Am J Surg Pathol 1996;20:877–888.
Lee JKT, Stanley RJ, Sagel SS, et al. Accuracy of computed tomography in detecting intra-abdominal and pelvic adenopathy in lymphoma. Am J Roentgenol 1978;131:675–679.
Elstrom R, Guan L, Baker G, et al. Utility of FDG PET scanning in lymphoma by WHO classification. Blood 2003;101:3875–3876.
Jerusalem G, Beguin Y, Najjar F, Hustinx R, Fassotte MF, Rigo P, Fillet G. Positron emission tomography (PET) with 18F-fluorodeoxyglucose (18F-FDG) for the staging of low-grade non-Hodgkin’s lymphoma (NHL). Ann Oncol 2001;12:825–830.
Hoffmann M, Kletter K, Becherer A, et al. 18F-fluorodeoxyglucose positron emission tomography (18F-FDG PET) for staging and follow-up of marginal zone B-cell lymphoma. Oncology 2003;64: 336–340.
Yeung HW, Young KS, Schoder H, Beal K, Larson SM. Extranodal marginal zone lymphoma (LAT) is frequently positive on FDG PET scan. J Nucl Med 2004;45:93P.
Nathwani B, Anderson JR, Armitage JO, et al. Marginal zone B-cell lymphoma: A clinical comparison of nodal and mucosa-associated lymphoid tissue types. J Clin Oncol 1999;17:2486–2492.
Ben-Haim S, Bar-Shalom R, Israel O, et al. Utility of gallium-67 scintigraphy in low-grade non-Hodgkin’s lymphoma. J Clin Oncol 1996;14:1936–1942.
Shrikanthan S, Zhuang HM, Schuster S, Alavi A. FDG PET imaging in diagnosis of mantle cell lymphoma. J Nucl Med 2004;45:93P.
Moog F, Bangerter M, Diederichs CG, Guhlmann A, Kotzerke J, Merkle E. Lymphoma: role of FDG PET in nodal staging. Radiology 1997;203:795–800.
Menzel C, Dobert N, Mitrou P, Mose S, Diehl M, Berner U. Positron emission tomography for the staging of Hodgkin’s lymphoma. Acta Oncol 2002;41:430–436.
Weihrauch MR, Re D, Bischoff S, Dietlein M, Scheidhauer K, Krug B. Whole-body positron emission tomography using 18F-fluorodeoxyglucose for initial staging of patients with Hodgkin’s disease. Ann Hematol 2002;81:20–25.
Naumann R, Beuthien-Baumann B, Reiss A, Schulze J, Hanel A, Bredow J. Substantial impact of FDG PET imaging on the therapy decision in patients with early-stage Hodgkin’s lymphoma. Br J Cancer 2004;90:620–625.
Bangerter M, Moog F, Buchmann I, et al. Whole-body 2-[18F]-fluoro-2-deoxy-D-glucose positron emission tomography (FDG PET) for accurate staging of Hodgkin’s disease. Ann Oncol 1998;9:1117–1122.
Schaefer NG, Hany TF, Taverna C, Seifert B, Stumpe KD, von Schulthess GK, Goerres GW. Non-Hodgkin lymphoma and Hodgkin disease: coregistered FDG PET and CT at staging and restaging – do we need contrast-enhanced CT? Radiology 2004;232:823–829.
Sohaib SA, Turner B, Hanson JA, Farquharson M, Oliver RT, Reznek RH. CT assessment of tumour response to treatment: comparison of linear, cross-sectional and volumetric measures of tumour size. Br J Radiol 2000;73:1178–1184.
Economopoulos T, Asprou N, Stathakis N, et al. Primary extranodal non-Hodgkin’s lymphoma of the head and neck. Oncology 1992;49:484–488.
Dodd GD. Lymphoma of the hollow abdominal viscera. Radiol Clin North Am 1990;28:771–783.
Yoo CC, Levine MS, Furth EE, Salhany KE, Rubesin SE, Laufer I, Herlinger H. Gastric mucosa-associated lymphoid tissue lymphoma: radiographic findings in six patients. Radiology 1998;208:239–243.
Levine MS, Rubesin SE, Pantongrag-Brown L, Buck JL, Herlinger H. Non-Hodgkin’s lymphoma of the gastrointestinal tract: radiographic findings. AJR Am J Roentgenol 1997;168(1):165–172.
Yuki M, Narabayashi I, Yamamoto K, Shimizu T, Tanaka Y, Tatsumi T, Komori T. Multifocal primary lymphoma of bone: scintigraphy and MR findings before and after treatment. Radiat Med 2000;18:305–310.
Lanfermann H, Heindel W, Schaper J, Schroeder R, Hansmann ML, Lehrke R, Ernestus RI, Lackner K. CT and MR imaging in primary cerebral non-Hodgkin’s lymphoma. Acta Radiol 1997;38:259–267.
Herrlinger U, Schabet M, Clemens M, Kortmann RD, Petersen D, Will BE, Meyermann R, Dichgans J. Clinical presentation and therapeutic outcome in 26 patients with primary CNS lymphoma. Acta Neurol Scand 1998;97:257–264.
Buhring U, Herrlinger U, Krings T, Thiex R, Weller M, Kuker W. MRI features of primary central nervous system lymphomas at presentation. Neurology 2001;57:393–396.
Buckley JA, Fishman EK.CT evaluation of small bowel neoplasms: spectrum of disease. Radiographics 1998;18:379–392.
Gospodarowicz MK, Ferry JA, Cavalli F. Unique aspects of primary extranodal lymphomas. In: Mauch PM, Armitage JO, Coiffier B, Dalla-Favera R, Harris NL (eds.). Non-Hodgkin’s lymphomas. Philadelphia: Lippincott Williams & Wilkins, 2004:685–707.
Gorg C, Weide R, Schwerk WB. Malignant splenic lymphoma: sonographic patterns, diagnosis and follow-up. Clin Radiol 1997;52:535–540.
Rodriguez M, Ahlstrom H, Sundin A, Rehn S, Sundstrom C, Hagberg H, Glimelius B. 18F FDG PET in gastric non-Hodgkin’s lymphoma. Acta Oncol 1997;36:577–584.
Hoffman JM, Waskin HA, Schifter T, et al. FDG PET in differentiating lymphoma from non-malignant central nervous system lesions in patients with AIDS. J Nucl Med 1993;34:567–575.
Heald AE, Hoffman JM, Bartlett JA, Waskin HA. Differentiation of central nervous system lesions in AIDS patients using positron emission tomography (PET). Int J STD AIDS 1996;7:337–346.
Skiest DJ, Erdman W, Chang WE, Oz OK, Ware A, Fleckenstein J. SPECT thallium-201 combined with Toxoplasma serology for the presumptive diagnosis of focal central nervous system mass lesions in patients with AIDS. J Infect 2000;40:274–281.
Shipp M, Mauch PM, Harris NL. Non-Hodgkin’s lymphomas. In: Devita VT, Hellman S, Rosenberg SA (eds.). Cancer Principles and Practice of Oncology. Philadelphia: Lippincott, 1997, pp. 2165–2220.
Abdel-Dayem HM, Rosen G, El-Zeftawy H, Naddaf S, Kumar M, Atay S, Cacavio A. Fluorine-18 fluorodeoxyglucose splenic uptake from extramedullary hematopoiesis after granulocyte colony-stimulating factor stimulation. Clin Nucl Med 1999;24:319–322.
Gundlapalli S, Ojha B, Mountz JM. Granulocyte colony-stimulating factor: confounding F-18 FDG uptake in outpatient positron emission tomographic facilities for patients receiving ongoing treatment of lymphoma. Clin Nucl Med 2002;27:140–141.
Carr R, Barrington SF, Madan B, ÓDoherty MJ, Saunders CA, van der Walt J, Timothy AR. Detection of lymphoma in bone marrow by whole-body positron emission tomography. Blood 1998;91: 3340–3346.
Moog F, Bangerter M, Kotzerke J, Guhlman A, Frickhofen N, Reske SN. 18-F-fluorodeoxyglucose-positron emission tomography as a new approach to detect lymphomatous bone marrow. J Clin Oncol 1998;16:603–609.
Rini JN, Manalili EY, Hoffman MA, Karayalcin G, Mehrotra B, Tomas MB, Palestro CJ. F-18 FDG versus Ga-67 for detecting splenic involvement in Hodgkin’s disease. Clin Nucl Med 2002;27:572–577.
Bar-Shalom R, Yefremov N, Haim N, et al. Camera-based FDG PET and 67Ga SPECT in evaluation of lymphoma: comparative study. Radiology 2003;227:353–360.
Wirth A, Seymour JF, Hicks RJ, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography, gallium-67 scintigraphy, and conventional staging for Hodgkin’s disease and non-Hodgkin’s lymphoma. Am J Med 2002;112:262–268.
Hong SP, Hahn JS, Lee JD, Bae SW, Youn MJ. 18F-fluorodeoxyglucose-positron emission tomography in the staging of malignant lymphoma compared with CT and 67Ga scan. Yonsei Med J 2003;44:779–786.
Sasaki M, Kuwabara Y, Koga H, Clinical impact of whole body FDG PET on the staging and therapeutic decision making for malignant lymphoma. Ann Nucl Med 2002;16:337–345.
Larson SM, Rasey JS, Allen DR, Nelson NJ, Grunbaum Z, Harp GD, Williams DL. Common pathway for tumor cell uptake of gallium-67 and iron-59 via a transferrin receptor. J Natl Cancer Inst 1980;64:41–53.
Nejmeddine F, Caillat-Vigneron N, Escaig F, Moretti JL, Raphael M, Galle P. Mechanism involved in gallium-67 (Ga-67) uptake by human lymphoid cell lines. Cell Mol Biol (Noisy-le-grand) 1998;44:1215–1220.
Diehl V, Stein H, Hummel M, Zollinger R, Connors JM. Hodgkin’s lymphoma: biology and treatment strategies for primary, refractory, and relapsed disease. Hematology 2003;225–247.
Buchmann I, Reinhardt M, Elsner K, et al. 2-(Fluorine-18)fluoro-2-deoxy-D-glucose positron emission tomography in the detection and staging of malignant lymphoma. A bicenter trial. Cancer 2001;91:889–999.
Partridge S, Timothy A, ÓDoherty MJ, et al. 2-fluorine-18-fluoro-2-deoxy-D glucose positron emission tomography in the pretreatment staging of Hodgkin’s disease: Influence on patients management in a single institution. Ann Oncol 2000;11:1273–1279.
Schoder H, Meta J, Yap C, et al. Effect of whole-body (18)F-FDG PET imaging on clinical staging and management of patients with malignant lymphoma. J Nucl Med 2001;42:1139–1143.
Hueltenschmidt B, Sautter-Bihl ML, Lang O, et al. Whole body positron emission tomography in the treatment of Hodgkin disease. Cancer 2001;91:302–310.
Brandt L, Kimby E, Nygren P, Glimelius B. A systematic overview of chemotherapy effects in Hodgkin’s disease. Acta Oncol 2001;40:185–197.
Coiffier B, Gisselbrecht C, Vose JM, et al. Prognostic factors in aggressive malignant lymphomas. Description and validation of prognostic index that could identify patients requiring a more intensive therapy. J Clin Oncol 1991;9:211–219.
Lewis E, Bernardino ME, Salvador PG, Cabanillas FF, Barnes PA, Thomas JL. Post-therapy CT-detected mass in lymphoma patients: is it viable tissue? J Comput Assist Tomogr 1982;6:792–795.
Cheson BD, Horning SJ, Coiffier B, et al. Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphomas. NCI Sponsored International Working Group. J Clin Oncol 1999;17:1244–1253.
Hasenclever D, Diehl V. International Prognostic Factors Project on Advanced Hodgkin’s Disease. A prognostic score for advanced Hodgkin’s disease. NEJM 1998;339:1506–1514.
Rodriguez MA, Fuller LM, Zimmerman SO, et al. Hodgkin’s disease: study of treatment intensities and incidences of second malignancies. Ann Oncol 1993;4:125–131.
Theuws JC, Seppenwoolde Y, Kwa SL, Boersma LJ, Damen EM, Baas P, Muller SH, Lebesque JV. Changes in local pulmonary injury up to 48 months after irradiation for lymphoma and breast cancer. Int J Radiat Oncol Biol Phys 2000;47:1201–1208.
Cremerius U, Fabry U, Kroll U, Zimny M, Neuerburg J, Osieka R, Bull U. Clinical value of FDG PET for therapy monitoring of malignant lymphoma. Results of a retrospective study in 72 patients. Nuklearmedizin 1999;38:24–30.
Weihrauch MR, Re D, Scheidhauer K, et al. Thoracic positron emission tomography using 18F-fluorodeoxyglucose for the evaluation of residual mediastinal Hodgkin’s disease. Blood 2001;98:2930–2934.
Naumann R, Vaic A, Beuthien-Baumann B, et al. Prognostic value of positron emission tomography in the evaluation of post-treatment residual mass in patients with Hodgkin’s disease and non-Hodgkin’s lymphoma. Br J Haematol 2001;115:793–800.
Mikhaeel NG, Timothy AR, ÓDoherty MJ, Hain S, Maisey MN. 18-FDG PET as a prognostic indicator in the treatment of aggressive Non-Hodgkin’s lymphoma: comparison with CT. Leuk Lymphoma 2000;39:543–553.
de Wit M, Bohuslavizki KH, Buchert, Bumann D, Clausen M, Hossfeld DK. 18FDG PET following treatment as valid predictor for disease-free survival in Hodgkin’s lymphoma. Ann Oncol 2001;12:29–37.
Zinzani PL, Magagnoli M, Chierichetti F, et al. The role of positron emission tomography (PET) in the management of lymphoma patients. Ann Oncol 1999;10:1181–1184.
Jerusalem G, Beguin Y, Fassotte MF, et al. Early detection of relapse by whole-body positron emission tomography in the follow-up of patients with Hodgkin’s disease. Ann Oncol 2003;14: 123–130.
Dittmann H, Sokler M, Kollmannsberger C, et al. Comparison of 18FDG PET with CT scans in the evaluation of patients with residual and recurrent Hodgkin’s lymphoma. Oncol Rep 2001;8:1393–1399.
Shipp MA. Prognostic factors in aggressive non-Hodgkin’s lymphoma: who has “high-risk” disease? Blood 1994;83:1165–1173.
Spaepen K, Stroobants S, Dupont P, et al. Prognostic value of positron emission tomography (PET) with fluorine-18 fluorodeoxyglucose ([18F]FDG after first line chemotherapy in non-Hodgkins lymphoma: is ([18F]FDG PET a valid alternative to conventional diagnostic methods? J Clin Oncol 2001;19:414–419.
Kostakoglu L, Coleman M, Leonard JP, Kuji I, Zoe H, Goldsmith SJ. Positron emission tomography predicts prognosis after one cycle of chemotherapy in aggressive lymphoma and Hodgkin’s disease. J Nucl Med 2002;43:1018–1027.
Mikhaeel NG, Mainwaring P, Nunan T, Timothy AR. Prognostic value of interim and post treatment FDG PET scanning in Hodgkin lymphoma [abstract]. Ann Oncol 2002;13(Suppl 2):21.
Spaepen K, Stroobants S, Dupont P, et al. Early restaging positron emission tomography with 18F-fluorodeoxyglucose predicts outcome in patients with aggressive non-Hodgkin’s lymphoma. Ann Oncol 2002;13:1356–1363.
Philip T, Guglielmi C, Hagenbeek A, et al. Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin’s lymphoma. NEJM 1995;333:1540–1545.
Cremerius U, Fabry U, Wildberger JE, et al. Pre-transplant positron emission tomography using fluorine-18-fluoro-deoxyglucose predicts outcome in patients treated with high-dose chemotherapy and autologous stem cell transplantation for non-Hodgkin’s lymphoma. Bone Marrow Transplant 2002;30:103–111.
Becherer A, Mitterbauer M, Jaeger U, et al. Positron emission tomography with [18F]2-fluoro-D-2-deoxyglucose (FDG PET) predicts relapse of malignant lymphoma after high-dose therapy with stem cell transplantation. Leukemia 2002;16:260–267.
Armitage JO, Weisenburger DD, Hutchins M, et al. Chemotherapy for diffuse large-cell lymphoma – rapidly responding patients have more durable remissions. J Clin Oncol 1986;4:160–164.
Haw R, Sawka CA, Franssen E, Berinstein HL. Significance of a partial or slow response to front-line chemotherapy in the management of intermediate-grade or high-grade non-Hodgkin’s lymphoma: a literature review. J Clin Oncol 1994;12:1074–1084.
Verdonck LF, van Putten WL, Hagenbeek A, Schouten HC, et al. NEJM 1995;20(332):1045–1051.
Romer W, Hanauske A-R, Ziegler S, et al. Positron emission tomography in non-Hodgkin’s lymphoma: assessment of chemotherapy with fluorodeoxyglucose. Blood 1998;91:4464–4471.
Kostakoglu L, Coleman M, Somrov S, Leonard JP, Verma S, Sherman CH,. Goldsmith SJ. FDG PET after one cycle of chemotherapy accurately predicts response to therapy in large cell (aggressive) non-Hodgkin’s lymphoma (NHL) and Hodgkin’s disease (HD). J Nucl Med 2004;45:316P.
Hoekstra O, Ossenkoppele GJ, Golding R, et al. Early treatment response in malignant lymphoma, as determined by planar fluorine-18-fluorodeoxyglucose scintigraphy. J Nucl Med 1993;34: 1706–1710.
Koss MN. Pulmonary lymphoid disorders. Semin Diagn Pathol 1995;12:158–171.
Reddy MP, Graham MM. FDG positron emission tomographic imaging of thoracic Castleman’s disease. Clin Nucl Med 2003;28:325–326.
Murphy SP, Nathan MA, Karwal MW. FDG PET appearance of pelvic Castleman’s disease. J Nucl Med 1997;38:1211–1212.
Bragg DG, Chor PJ, Murray KA, et al. Lymphoproliferative disorders of the lung: histopathology, clinical manifestations, and imaging features. Am J Roentgenol 1994;163:273–281.
Tirelli U, Spina M, Gaidano G, Vaccher E, Franceschi S, Carbone A. Epidemiological, biological and clinical features of HIV-related lymphomas in the era of highly active antiretroviral therapy. AIDS 2000;14:1675–1688.
Weinblatt ME, Zanzi I, Belakhlef A, Babchyck B, Kochen J. False-positive FDG PET imaging of the thymus of a child with Hodgkin’s disease. J Nucl Med 1997;38:888–890.
Ferdinand B, Gupta P, Kramer EL. Spectrum of thymic uptake at 18F-FDG PET. Radiographics 2004;24:1611–1616.
Kawano T, Suzuki A, Ishida A, et al. The clinical relevance of thymic fluorodeoxyglucose uptake in pediatric patients after chemotherapy. Eur J Nucl Med Mol Imag 2004;31:31–36.
Armitage JO. Bone marrow transplantation. NEJM 1994;330: 827–838.
Sandherr M, von Schilling C, Link T, Stock K, von Bubnoff N, Peschel C, Avril N. Pitfalls in imaging Hodgkin’s disease with computed tomography and positron emission tomography using fluorine-18-fluorodeoxyglucose. Ann Oncol 2001;12: 719–722.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Kostakoglu, L. (2011). PET-CT Imaging of Lymphoma. In: Shreve, P., Townsend, D. (eds) Clinical PET-CT in Radiology. Springer, New York, NY. https://doi.org/10.1007/978-0-387-48902-5_22
Download citation
DOI: https://doi.org/10.1007/978-0-387-48902-5_22
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-0-387-48900-1
Online ISBN: 978-0-387-48902-5
eBook Packages: MedicineMedicine (R0)