Abstract
Childhood nephrotic syndrome is a rare condition with an incidence of 1–2 per 100 000 children aged below 16 years. Untreated idiopathic nephrotic syndrome (INS) is associated with increased risks of life-threatening infection, thromboembolism, lipid abnormalities, and malnutrition. The aim of the management of INS in children is to induce and maintain complete remission with resolution of proteinuria and edema without serious adverse effects of therapy.
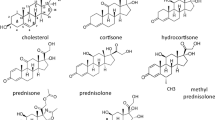
The majority of children have corticosteroid sensitive idiopathic nephrotic syndrome (CSINS), and in these children, corticosteroid therapy is the mainstay of therapy to induce remission. Data from a meta-analysis of randomized controlled trials (RCTs) indicate that prolonged courses of corticosteroids (up to 7 months) given in the first episode of CSINS reduce the risk of relapse. Nevertheless, many children relapse, and are at risk of corticosteroid toxicity if frequent courses of corticosteroids are required. Data from RCTs supports the use of alkylating agents (cyclophosphamide, chlorambucil), cyclosporine, and levamisole in these children to achieve prolonged periods of remission. The specific management of corticosteroid-resistant idiopathic nephrotic syndrome (CRINS) is more difficult since few therapies are consistently effective, and data from RCTs are limited. In such children, cyclosporine, alkylating agents, and high dose intravenous methylprednisone may be used.
In addition to specific therapies for INS, supportive therapies are commonly used to control edema (loop diuretics, aldosterone antagonists, albumin infusions, angiotensin-converting enzyme inhibitors), reduce the risk of infection (antibacterials, pneumococcal vaccination) and thromboembolism (aspirin [acetylsalicylic acid]), and to control hyperlipidemia (HMG-CoA reductase inhibitors), especially in children with CRINS.








Similar content being viewed by others
References
Schlesinger ER, Sultz HA, Mosher WE, et al. The nephrotic syndrome: its incidence and implications for the community. Am J Dis Child 1968; 116: 623–32
McKinney PA, Feltbower RG, Brocklebank JT, et al. Time trends and ethnic patterns of childhood nephrotic syndrome in Yorkshire, UK. Pediatr Nephrol 2001; 16: 1040–4
Hodson EM, Willis NS, Craig JC. Incidence of nephrotic syndrome in children in australia. Seventh Asian Congress of Pediatric Nephrology; 2000 Nov 4–6; Singapore
Srivastava T, Simon SD, Alon US. High incidence of focal and segmental glomerulosclerosis in nephrotic syndrome of childhood. Pediatr Nephrol 1999; 13: 13–8
International Study of Kidney Disease in Children. Nephrotic syndrome in children: prediction of histology from clinical and laboratory characteristics at time of diagnosis. Kidney Int 1978; 13: 159–65
International Study of Kidney Disease in Children. Primary nephrotic syndrome in children: clinical significance of histopathologic variants of minimal change and of diffuse mesangial proliferation. Kidney Int 1981; 20: 765–71
Bhimma R, Coovadia HM, Adhikari M. Nephrotic syndrome in South African children: changing perspectives over 20 years. Pediatr Nephrol 1997; 11: 429–34
International Study of Kidney Disease in Children. The primary nephrotic syndrome in children: identification of patients with minimal change nephrotic syndrome from initial response to prednisone. J Pediatr 1981; 98: 561–4
Cattran DC, Rao P. Long-term outcome in children and adults with classic focal and segmental glomerulosclerosis. Am J Kid Dis 1998; 32: 72–9
Consensus statement on management and audit potential for corticosteroid responsive nephrotic syndrome. Report of a workshop by the British Association for Paediatric Nephrology and Research Unit, Royal College of Physicians. Arch Dis Child 1994; 70: 151–7
Brodehl J. The treatment of minimal change nephrotic syndrome: lessons learned from multicentre co-operative studies. Eur J Pediatr 1991; 150: 380–7
Hogg RJ, Portman RJ, Milliner D, et al. Evaluation and management of proteinuria and nephrotic syndrome in children: recommendations from a pediatric nephrology pestablished at the National Kidney Foundation Conference on proteinuria, albuminuria, risk, assessment, detection and elimination (PARADE). Pediatrics 2000; 105: 1242–9
Koskimies O, Vilska J, Rapola J, et al. Long-term outcome of primary nephrotic syndrome. Arch Dis Child 1982; 57: 544–8
Tarshish P, Tobin JN, Bernstein J, et al. Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol 1997; 8: 769–76
International Study of Kidney Disease in Children. Early identification of frequent relapsers among children with minimal change nephrotic syndrome. J Pediatr 1982; 101: 514–8
Arneil GC. The nephrotic syndrome. Pediatr Clin North Am 1971; 18: 547–59
Hodson EM, Knight JF, Willis NS, et al. Corticosteroid therapy for nephrotic syndrome in children (Cochrane Review). Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 2. Available from URL: www.update-software.com. Oxford: Update Software, 2002
Durkan A, Hodson E, Willis N, et al. Non-corticosteroid treatment for nephrotic syndrome in children (Cochrane Review). Available in The Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 2. Available from URL: www.update-software.com. Oxford: Update Software, 2002
Hodson EM, Knight JF, Willis NS, et al. Corticosteroid therapy in nephrotic syndrome: a meta-analysis of randomised controlled trials. Arch Dis Child 2000; 83: 45–51
Durkan AM, Hodson EM, Willis NS, et al. Immunosuppressive agents in childhood nephrotic syndrome: a meta-analysis of randomised controlled trials. Kidney Int 2001; 59: 1919–27
Dickersin K, Scherer R, Lefebvre C. Identifying relevant studies for systematic reviews. BMJ 1994; 309: 1286–91
Lefebvre C, McDonald S. Development of a sensitive search strategy for reports of randomized controlled trials in EMBASE. Proceedings of the 4th International Cochrane Colloquium; 1996 Oct 20–24; Adelaide
Review Manager (RevMan). 4.1 for Windows. The Cochrane Collaboration; Oxford: Update Software, 2002
Vande Walle JGJ, Donckerwolcke RA. Pathogenesis of edema formation in the nephrotic syndrome. Pediatr Nephrol 2001; 16: 283–93
Alderson P, Bunn F, Lefebvre C, et al. Human albumin solution for resuscitation and volume expansion in critically ill patients (Cochrane Review). Cochrane injuries group. Available in the Cochrane Library [database on disk and CD ROM]. Updated quarterly. The Cochrane Collaboration; issue 1. Oxford: Update Software, 2002
Garin EH. A comparison of combinations of diuretics in nephrotic edema. Am J Dis Child 1987; 141: 769–71
Lilova MI, Velkovski IG, Topalov IB. Thromboembolic complications in children with nephrotic syndrome in Bulgaria (1974-1996). Pediatr Nephrol 2000; 15: 74–8
Bagga A, Mudigoudar BD, Vasudev V, et al. Low (LD) versus high dose (HD) enalapril therapy in corticosteroid resistant nephrotic syndrome. Seventh Asian Congress of Pediatric Nephrology; 2000 Nov 4–6; Singapore
Delucchi A, Cano F, Rodriguez E, et al. Enalapril and prednisone in children with nephrotic-range proteinuria. Pediatr Nephrol 2000; 14: 1088–91
Vehaskari VM. Treatment practices of FSGS among North American pediatric nephrologists. Pediatr Nephrol 1999; 13: 301–3
Mehls O, Andrassay K, Koderisch J, et al. Hemostasis and thromboembolism in children with nephrotic syndrome: differences from adult. J Pediatr 1987; 110: 862–7
McBryde KD, Kershaw DB, Smoyer WE. Pediatric corticosteroid-resistant nephrotic syndrome. Curr Probl Pediatr 2001; 31: 275–307
Minimal change nephrotic syndrome in children: deaths during the first 5–15 years’ observation: a report of the International Study of Kidney Disease in Children. Pediatrics 1984; 73: 497–501
American Academy of Pediatrics. Technical report: prevention of pneumococcal infections, including the use of pneumococcal conjugate and polysaccharide vaccines and antibiotic prophylaxis. Pediatrics 2000; 106: 367–76
Spike JS, Halsey NA, Fish AJ, et al. Serum antibody response to pneumococcal vaccine in children with nephrotic syndrome. Pediatrics 1982; 69: 219–23
Querfeld U. Should hyperlipidemia in children with nephrotic syndrome be treated. Pediatr Nephrol 1999; 13: 74–84
Ordonez JD, Hiatt RA, Killebrew EJ, et al. The increased risk of coronary heart disease associated with nephrotic syndrome. Kidney Int 1993; 44: 638–42
Olbricht CJ, Wanner C, Thiery J, et al. Simvastatin in nephrotic syndrome. Kidney Int 1999; 56Suppl. 71: S1113–6
Thomas ME, Harris KPG, Ramaswamy C, et al. Simvastatin therapy for hypercholesterolemic patients with nephrotic syndrome or significant proteinuria. Kidney Int 1993; 44: 1124–9
Coleman JE, Watson AR. Hyperlipidaemia, diet and simvastatin therapy in corticosteroid-resistant nephrotic syndrome of childhood. Pediatr Nephrol 1996; 10: 171–4
Sanjad SA, Al-Abbad A, Al-Shorafa S. Management of hyperlipidemia in children with refractory nephrotic syndrome: the effect of statin therapy. J Pediatr 1997; 130: 470–4
Arneil GC, Lam CN. Long-term assessment of corticosteroid therapy in childhood nephrosis. Lancet 1966; II: 819–21
Saxena K, Crawford JD. The treatment of nephrosis. N Engl J Med 1965; 272: 522–6
Alternate-day versus intermittent prednisone in frequently relapsing nephrotic syndrome: a report of Arbeitsgemeinschaft für Pädiatrische Nephrologie. Lancet 1979; I: 401–3
Ekka BK, Bagga A, Srivastava RN. Single- versus divided-dose prednisolone therapy for relapses of nephrotic syndrome. Pediatr Nephrol 1997; 11: 597–9
Ueda N, Chihara M, Kawaguchi S, et al. Intermittent versus long-term tapering prednisolone for initial therapy in children with idiopathic nephrotic syndrome. J Pediatr 1988; 112: 122–6
Norero C, Delucchi A, Lagos E, et al. Initial therapy of primary nephrotic syndrome in children: evaluation in a period of 18 months of two prednisone treatment schedules. Chilean Co-operative Group of Study of Nephrotic Syndrome in Children. Rev Med Chile 1996; 124: 567–72
Ehrich JH, Brodehl J. Long versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft für Pädiatrische Nephrologie. Eur J Pediatr 1993; 152: 357–61
Ksiazek J, Wyszynski T. Short versus long initial prednisone treatment in steroid-sensitive nephrotic syndrome in children. Acta Paediatr 1995; 84: 889–93
Bagga A, Hari P, Srivastava RN. Prolonged versus standard initial prednisolone therapy for initial episode of nephrotic syndrome. Pediatr Nephrol 1999; 13: 824–7
Short versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft für Pädiatrische Nephrologie. Lancet 1988; I(8582): 380–3
Kleinknecht C, Broyer M, Parchoux B, et al. Comparison of short and long treatment at onset of steroid sensitive nephrosis (SSN): preliminary results of a multicenter controlled trial from the French Society of Pediatric Nephrology [abstract]. Int J Pediatr Nephrol 1982; 3: 45
Wingen AM, Muller-Wiefel DE, Scharer K. Comparison of different regimens of prednisone therapy in frequently relapsing nephrotic syndrome. Acta Paediatr Scand 1990; 79: 305–10
Broyer M, Guest G, Gagnadoux MF. Growth rate in children receiving alternate-day corticosteroid treatment after kidney transplant. J Pediatr 1992; 120: 721–5
Bargman JM. Management of minimal lesion glomerulonephritis: evidence-based recommendations. Kidney Int 1999; 55: S3–16
Broyer M, Terzi F, Lehnert A, et al. A controlled study of deflazacort in the treatment of idiopathic nephrotic syndrome. Pediatr Nephrol 1997; 11(4): 418–22
Matoo TK, Mahmoud MA. Increased maintenance corticosteroids during upper respiratory infection decrease the risk of relapse in nephrotic syndrome. Nephron 2000; 85: 343–5
Leisti S, Koskimies O, Perheentupa J, et al. Idiopathic nephrotic syndrome: prevention of early relapse [letter]. BMJ 1978; I: 892
Effect of cytotoxic drugs in frequently relapsing nephrotic syndrome with and without corticosteroid dependence. N Engl J Med 1982; 306: 451–4
Cyclophosphamide treatment of corticosteroid dependent nephrotic syndrome: comparison of eight week with 12 week course. Report of Arbeitsgemeinschaft fur Padiatrische Nephrologie. Arch Dis Child 1987; 62: 1102–6
Ueda N, Kuno K, Ito S. Eight and 12 week courses of cyclophosphamide in nephrotic syndrome. Arch Dis Child 1990; 65: 1147–50
Latta K, von Schnakenburg C, Ehrich JHH. A meta-analysis of cytotoxic treatment for frequently relapsing nephrotic syndrome in children. Pediatr Nephrol 2001; 16: 271–82
Gulati S, Pokhariyal S, Sharma RK, et al. Pulse cyclophosphamide therapy in frequently relapsing nephrotic syndrome. Nephrol Dial Transplant 2001; 16: 2013–7
Prospective controlled trial of cyclophosphamide therapy in children with the nephrotic syndrome. Report of the International Study of Kidney Disease in Children. Lancet 1974; II: 423–7
Chiu J, McLaine PN, Drummond KN. A controlled prospective study of cyclophosphamide in relapsing, corticosteroid-responsive, minimal-lesion nephrotic syndrome in childhood. J Pediatr 1973; 82: 607–13
Barratt TM, Soothill JF. Controlled trial of cyclophosphamide in steroid-sensitive relapsing nephrotic syndrome of childhood. Lancet 1970; II: 479–82
Rashid HU, Ahmed S, Fatima N, et al. Levamisole in the treatment of steroid dependent or frequent relapsing nephrotic syndrome in children. Bangladesh Ren J 1996; 15: 6–8
Dayal U, Dayal AK, Shastry JC, et al. Use of levamisole in maintaining remission in steroid-sensitive nephrotic syndrome in children [published erratum appears in Nephron 1994; 67: 507]. Nephron 1994; 66: 408–12
Beattie TJ, Barratt TM, Dillon MJ, et al. Levamisole for corticosteroid-dependent nephrotic syndrome in childhood. Lancet 1991; 337: 1555–7
Grupe WE, Makker SP, Ingelfinger JR. Chlorambucil treatment of frequently relapsing nephrotic syndrome. N Engl J Med 1976; 295: 746–9
Alatas H, Wirya IG, Tambunan T, et al. Controlled trial of chlorambucil in frequently relapsing nephrotic syndrome in children (a preliminary report). J Med Assoc Thai 1978; 61Suppl. 1: 222–8
Abramowicz M, Arneil GC, Barnett HL, et al. Controlled trial of azathioprine in children with nephrotic syndrome. Lancet 1970; I: 959–61
Barratt TM, Cameron JS, Chantier C, et al. Controlled trial of azathioprine in treatment of steroid-responsive nephrotic syndrome of childhood. Arch Dis Child 1977; 52: 462–3
Niaudet P, Broyer M, Habib R. Treatment of idiopathic nephrotic syndrome with cyclosporine A in children. Clin Nephrol 1991; 35Suppl. 1: S31–33
Hulton SA, Neuhaus TJ, Dillon MJ, et al. Long-term cyclosporine A treatment of minimal-change nephrotic syndrome of childhood. Pediatr Nephrol 1994; 8: 401–3
Arbeitsgemeinschaft für Padiatrische Nephrologie. Results of the nephrotic syndrome study VIII of the APN: new standard treatment versus new standard treatment plus 8 weeks cyclosporine A [abstract]. Pediatr Nephrol 1999; 13: C26
Bagga A, Sharma A, Srivastava RN. Levamisole therapy in corticosteroid-dependent nephrotic syndrome. Pediatr Nephrol 1997; 11: 415–7
Alsaran K, Grisaru S, Stephens D, et al. Levamisole vs cyclophosphamide for frequently-relapsing corticosteroid-dependent nephrotic syndrome. Clin Nephrol 2001; 56: 289–94
Palcoux JB, Niaudet P, Goumy P. Side effects of levamisole in children with nephrosis. Pediatr Nephrol 1994; 8: 263–4
Barbano G, Ginevri F, Ghiggeri GM, et al. Disseminated autoimmune disease during levamisole treatment of nephrotic syndrome. Pediatr Nephrol 1999; 13: 602–3
Imbasciati E, Gusmano R, Edefonti A, et al. Controlled trial of methylprednisolone pulses and low dose oral prednisone for the minimal change nephrotic syndrome. BMJ 1985; 291: 1305–8
Yoshioka K, Ohashi Y, Sakai T, et al. A multicenter trial of mizoribine compared with placebo in children with frequently relapsing nephrotic syndrome. Kidney Int 2000; 58: 317–24
Rowe PC, McLean RH, Ruley EJ, et al. Intravenous immunoglobulin in minimal change nephrotic syndrome: a crossover trial. Pediatr Nephrol 1990; 4(1): 32–5
Trompeter RS, Thomson PD, Barratt TM, et al. Controlled trial of disodium cromoglycate in prevention of relapse of corticosteroid-responsive nephrotic syndrome of childhood. Arch Dis Child 1978; 53: 430–2
Yoshikawa N, Ito H, Takehoshi Y, et al. Standard versus long-term prednisolone with Sairer-to in childhood corticosteroid-responsive nephrotic syndrome: a prospective controlled study. Jpn J Nephrol 1998; 40: 587–90
Chandra M, Susin M, Abitbol C. Remission of relapsing childhood nephrotic syndrome with mycophenolate mofetil. Pediatr Nephrol 2000; 14: 224–6
Hiraoka M, Tsukahara H, Hori C, et al. Efficacy of long-term azathioprine for relapsing nephrotic syndrome. Pediatr Nephrol 2000; 14: 776–8
Jayantha UK. Captopril: a new approach to corticosteroid dependent idiopathic nephrotic syndrome. Seventh Asian Congress of Pediatric Nephrology; 2000 Nov 4–6; Singapore
Tarshish P, Tobin JN, Bernstein J, et al. Cyclophosphamide does not benefit patients with focal segmentai glomerulosclerosis. A report of the International Study of Kidney Disease in Children. Pediatr Nephrol 1996; 10: 590–3
Elhence R, Gulati S, Kher V, et al. Intravenous pulse cyclophosphamide: a new regime for corticosteroid-resistant minimal change nephrotic syndrome. Pediatr Nephrol 1994; 8: 1–3
Wyszynska T, Ksiazek J, Uszucka-Karcz M, et al. Evaluation of prednisolone pulse therapy in corticosteroid-resistant nephrotic syndrome. Contr Nephrol 1988; 67: 229–32
Tune BM, Kirpekar R, Sibley RK, et al. Intravenous methylprednisolone and oral alkylating agent therapy of prednisone-resistant pediatric focal segmental glomerulosclerosis: a long-term follow-up. Clin Nephrol 1995; 43: 84–8
Tune BM, Lieberman E, Mendoza SA. Corticosteroid-resistant nephrotic focal segmental glomerulosclerosis: a treatable disease. Pediatr Nephrol 1996; 10: 772–8
Hari P, Bagga A, Jindal N, et al. Treatment of focal glomerulosclerosis with pulse corticosteroids and oral cyclophosphamide. Pediatr Nephrol 2001; 16(11): 901–5
Niaudet P, the French Society of Pediatric Nephrology. Treatment of childhood corticosteroid-resistant idiopathic nephrosis with a combination of cyclosporine and prednisone. J Pediatr 1994; 125: 981–6
Singh A, Tejani C, Tejani A. One-center experience with cyclosporine in refractory nephrotic syndrome in children. Pediatr Nephrol 1999; 13: 26–32
Garin EH, Orak JK, Hiott KL, et al. Cyclosporine therapy for corticosteroid-resistant nephrotic syndrome: a controlled study. Am J Dis Child 1988; 142: 985–8
Lieberman KV, Tejani A. A randomized double-blind placebo-controlled trial of cyclosporine in corticosteroid-resistant idiopathic focal segmental glomerulosclerosis in children. J Am Soc Nephrol 1996; 7: 56–63
Ponticelli C, Rizzoni G, Edefonti A, et al. A randomized trial of cyclosporine in corticosteroid-resistant idiopathic nephrotic syndrome. Kidney Int 1993; 43: 1377–84
McCauley J, Shapiro R, Ellis D, et al. Pilot trial of FK506 in the management of corticosteroid-resistant nephrotic syndrome. Nephrol Dial Transplant 1993; 8: 1286–90
Franke D, Zimmering M, Wolfish N, et al. Treatment of FSGS with plasma exchange and immunadsorption. Pediat Nephrol 2000; 14: 965–9
Vécsei AKW, Müller T, Schratzberger EC, et al. Plasmapheresis-induced remission in otherwise therapy resistant FSGS. Pediatr Nephrol 2001; 16(11): 898–900
Radhakrishnan J, Wang MM, Matalon A, et al. Mycophenolate mofetil (MMF) treatment of idiopathic focal and segmental glomerulosclerosis (FSGS) [abstract]. J Am Soc Nephrol 1999; 10: 114A
Tenbrock K, Muller-Berghaus J, Fuchshuber A, et al. Levamisole treatment in corticosteroid-sensitive and corticosteroid-resistant nephrotic syndrome. Pediatr Nephrol 1998; 12: 459–62
Sharma M, Sharma R, McCarthy ET, et al. The FSGS factor: enrichment and in vivo effect of activity from focal segmental glomerulosclerosis patients. J Am Soc Nephrol 1999; 10: 552–61
Fuchshuber A, Mehls O. Familial corticosteroid-resistant nephrotic syndrome: recent advances. Nephrol Dial Transplant 2000; 15: 1897–900
Acknowledgements
Dr Elisabeth Hodson is employed as a senior staff specialist in pediatric nephrology at The Children’s Hospital at Westmead, Sydney, Australia. Dr Hodson is supported by the National Health and Medical Research Council of Australia, and the Federal Department of Health and Aging of Australia, through grants to the Renal Review Group of the Cochrane Collaboration.
The author has no conflicts of interest that are directly relevant to the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hodson, E.M. The Management of Idiopathic Nephrotic Syndrome in Children. Pediatr-Drugs 5, 335–349 (2003). https://doi.org/10.2165/00128072-200305050-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00128072-200305050-00006