Abstract
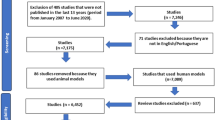
Probiotics are defined as live microorganisms which, when administered in adequate amounts, confer a health benefit on the host. To synthesize the evidence for the effectiveness of probiotics in the treatment or prevention of atopic dermatitis (AD) in children, we reviewed the results of 13 relevant randomized (placebo)-controlled trials (RCTs), 10 of which evaluated probiotics as treatment and 3 for prevention of AD. The main outcome measure in 9 RCTs was the change in SCORAD (SCORing Atopic Dermatitis).
Four RCTs suggested that there was a statistically significant decrease in SCORAD after probiotic administration to infants or children with AD for 1 or 2 months compared with that after placebo, while in two RCTs SCORAD was significantly reduced after treatment with lactobacilli only in children with IgE-associated AD. In four of these six RCTs, clinical improvement was associated with a change in some inflammatory markers. In three RCTs, the change in SCORAD was not statistically significant between probiotic- and placebo-treated children, although in one of these trials SCORAD was significantly lower after probiotic than with placebo treatment in food-sensitized children. In most RCTs, probiotics did not cause a statistically significant change in interferon-γ, interleukin-4, tumor necrosis factor-α, eosinophil cationic protein or transforming growth factor-β compared with placebo.
Regarding the effectiveness of probiotics in the prevention of AD, in two RCTs, infants at high risk for atopy who received probiotics developed AD significantly less frequently during the first 2 years of life than infants who received placebo. In these studies, mothers were administered Lactobacillus rhamnosus GG with or without other probiotics perinatally, followed by treatment of the infants with the same probiotics for the first 6 months of life. However, in another trial, neither the frequency nor the severity of AD during the first year of life were significantly different between infants with atopic mothers who received L. acidophilus for the first 6 months of life compared with infants who received placebo.
Probiotics, especially L. rhamnosus GG, seem to be effective for the prevention of AD. They were also found to reduce the severity of AD in approximately half of the RCTs evaluated, although they were not found to change significantly most of the inflammatory markers measured in the majority of the RCTs evaluated. More RCTs need to be conducted to elucidate whether probiotics are useful for the treatment or prevention of AD.





Similar content being viewed by others
References
Williams HC. Atopic dermatitis. N Engl J Med 2005 352: 2314–24
Reid G, Jass J, Sebulsky T. Potential uses of probiotics in clinical practice. Clin Microbiol Rev 2003 16: 658–72
Bjorksten B, Sepp E, Julge K. Allergy development and the intestinal microflora during the first year of life. J Allergy Clin Immunol 2001 108 (4): 516–20
Bongaerts GPA, Severijnen RSVM. Preventive and curative effects of probiotics in atopic patients. Med Hypotheses 2005 64: 1089–92
Isolauri E, Sutas Y, Kankaanpaa P. Probiotics: effects on immunity. Am J Clin Nutr 2001 73: 444–50
Majamaa H, Isolauri E. Probiotics: a novel approach in the management of food allergy. J Allergy Clin Immunol 1997 99 (2): 179–85
Kirjavainen PV, Salminen SJ, Isolauri E. Probiotic bacteria in the management of atopic disease: underscoring the importance of viability. J Pediatr Gastroenterol Nutr 2003 36: 223–7
Isolauri E, Arvola T, Sutas Y. Probiotics in the management of atopic eczema. Clin Exp Allergy 2000 30 (11): 1604–10
Weston S, Halbert A, Richmond P. Effects of probiotics on atopic dermatitis: a randomised controlled trial. Arch Dis Child 2005 Sep; 90 (9): 892–7
Viljanen M, Savilahti E, Haahtela T. Probiotics in the treatment of atopic eczema/dermatitis syndrome in infants: a double-blind placebo-controlled trial. Allergy 2005 60 (4): 494–500
Rosenfeldt V, Benfeldt E, Nielsen SD. Effect of probiotic Lactobacillus strains in children with atopic dermatitis. J Allergy Clin Immunol 2003 111: 389–95
Sistek D, Kelly R, Wickens K. Is the effect of probiotics on atopic dermatitis confined to food sensitized children? Clin Exp Allergy 2006; 36 (5): 629–33
Brouwer ML, Wolt-Plompen SA, Dubois AE. No effects of probiotics on atopic dermatitis in infancy: a randomized placebo-controlled trial. Clin Exp Allergy 2006 Jul; 36 (7): 899–906
Folster-Holst R, Muller F, Schnopp N. Prospective, randomised controlled trial on Lactobacillus rhamnosus in infants with moderate to severe atopic dermatitis. Br J Dermatol 2006 155: 1256–61
Pohjavuori E, Viljanen M, Korpela R. Lactobacillus GG effect in increasing IFN-gamma production in infants with cow’s milk allergy. J Allergy Clin Immunol 2004 114: 131–6
Prescott SL, Dunstan JA, Hale J. Clinical effects of probiotics are associated with increased interferon-gamma responses in very young children with atopic dermatitis. Clin Exp Allergy 2005 Dec; 35 (12): 1557–64
Viljanen M, Kuitunen M, Haahtela T. Probiotic effects on faecal inflammatory markers and on faecal IgA in food allergic atopic eczema/dermatitis syndrome infants. Pediatr Allergy Immunol 2005 16: 65–71
Rosenfeldt V, Benfeldt E, Valerius NH. Effect of probiotics on gastrointestinal symptoms and small intestinal permeability in children with atopic dermatitis. J Pediatr 2004 145: 612–6
Kankaanpaa PE, Yang B, Kallio HP. Influence of probiotic supplemented infant formula on composition of plasma lipids in atopic infants. J Nutr Biochem 2002 13 (6): 364–9
Rautava S, Kalliomaki M, Isolauri E. Probiotics during pregnancy and breastfeeding might confer immunomodulatory protection against atopic disease in the infant. J Allergy Clin Immunol 2002 109 (1): 119–21
Kalliomaki M, Salminen S, Arvilommi H. Probiotics in primary prevention of atopic disease: a randomised placebo-controlled trial. Lancet 2001 357 (9262): 1076–9
Kukkonen K, Savilahti E, Haahtela T. Probiotics and prebiotic galacto-oligosaccharides in the prevention of allergic diseases: a randomised, double-blind, placebo-controlled trial. J Allergy Clin Immunol 2007 119: 192–8
Taylor A, Dunstan J, Prescott S. Probiotic supplementation for the first 6 months of life fails to reduce the risk of atopic dermatitis and increases the risk of allergen sensitisation in high-risk children: a randomised controlled trial. J Allergy Clin Immunol 2007 119: 184–91
Viljanen M, Pohjavuori E, Haahtela T. Induction of inflammation as a possible mechanism of probiotic effect in atopic eczema-dermatitis syndrome. J Allergy Clin Immunol 2005 115 (6): 1254–9
Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol 1980 92: 44–7
Williams HC, Burney PG, Pembroke AC. The U. K Working Party’s diagnostic criteria for atopic dermatitis: III Independent hospital validation. Br J Dermatol 1994 131: 406–16
Williams HC. Two positive studies of probiotics for atopic dermatitis. Arch Dermatol 2006 142: 1201–3
Kawamoto N, Kaneko H, Takemura M. Age-related changes in intracellular cytokine profiles and Th2 dominance in allergic children. Pediatr Allergy Immunol 2006 17 (2): 125–33
Kallstrom E, Roscher I, Andreasson A. Decreased frequency of intracellular IFN-gamma producing T cells in whole blood preparations from patients with atopic dermatitis. Exp Dermatol 2002 11 (6): 556–63
Tang M, Kemp A, Varigos G. IL-4 and interferon-gamma production in children with atopic disease. Clin Exp Immunol 1993 92 (1): 120–4
Dunstan JA, Hale J, Breckler L. Atopic dermatitis in young children is associated with impaired interleukin-10 and interferon-gamma responses to allergens, vaccines and colonizing skin and gut bacteria. Clin Exp Allergy 2005 35 (10): 1309–17
Machura E, Mazur B, Kwiecien J. Intracellular production of IL-2, IL-4, IFN- gamma, and TNF-alpha by peripheral blood CD3+ and CD4+ T cells in children with atopic dermatitis. Eur J Pediatr 2007 166 (8): 789–95
Sutas Y, Soppi E, Korhonen H. Suppression of lymphocyte proliferation in vitro by bovine caseins hydrolyzed with Lactobacillus casei GG-derived enzymes. J Allergy Clin Immunol 1996 98 (1): 216–24
Sutas Y, Hurme M, Isolauri E. Down-regulation of anti-CD3 antibody-induced IL-4 production by bovine caseins hydrolysed with Lactobacillus GG-derived enzymes. Scand J Immunol 1996 43 (6): 687–9
Miettinen M, Vuopio-Varkila J, Varkila K. Production of human tumor necrosis factor alpha, interleukin-6 and interleukin-10 is induced by lactic acid bacteria. Infect Immun 1996 64: 5403–5
Poulsen LK, Bindslev-Jensen C, Diamant M. Biomolecular regulation of the IgE immune response: III. Cytokine profiles in atopic dermatitis, inhalant allergy and non-allergic donors Cytokine 1996 8 (8): 651–7
Takahashi T, Sasaki Y, Hama K. Production of IL-4, IL-2, IFN-gamma, and TNF-alpha by peripheral blood mononuclear cells of patients with atopic dermatitis. J Dermatol Sci 1992 3 (3): 172–80
Antunez C, Torres MJ, Mayorga C. Different cytokine production and activation marker profiles in circulating cutaneous-lymphocyte-associated anti- gen T cells from patients with acute or chronic atopic dermatitis. Clin Exp Allergy 2004 34 (4): 559–66
Reinhold U, Pawelec G, Wehrmann W. Cytokine release from cultured peripheral blood mononuclear cells of patients with severe atopic dermatitis. Acta Derm Venereol 1989 69 (6): 497–502
Seneviratne SL, Jones L, Bailey AS. Severe atopic dermatitis is associated with a reduced frequency of IL-10 producing allergen-specific CD4+ T cells. Clin Exp Dermatol 2006 31 (5): 689–94
Pellegrino M, Minervini B, Musto P. Tumor necrosis factor-alpha and interleukin-1 beta: two possible mediators of allergic inflammation. Minerva Pediatr 1996 48 (7-8): 309–12
Sumimoto S, Kawai M, Kasajima Y. Increased plasma tumour necrosis factor-alpha concentration in atopic dermatitis. Arch Dis Child 1992 67 (3): 277–9
de Vries IJ, Langeveld-Wildschut EG, van Reijsen FC. Adhesion molecule expression on skin endothelia in atopic dermatitis: effects of TNF-alpha and IL-4. J Allergy Clin Immunol 1998 102 (3): 461–8
Noso N, Sticherling M, Bartels J. Identification of an N-terminally truncated form of the chemokine RANTES and granulocyte-macrophage colony-stimu- lating factor as major eosinophil attractants released by cytokine-stimulated dermal fibroblasts. J Immunol 1996 156 (5): 1946–53
Yamada H, Matsukura M, Yudate T. Enhanced production of RANTES, an eosinophil chemoattractant factor, by cytokine-stimulated epidermal keratinocytes. Int Arch Allergy Immunol 1997 114 Suppl. 1: 28–32
Angelova-Fischer I, Hipler UC, Bauer A. Significance of interleukin-16, macrophage-derived chemokine, eosinophil cationic protein and soluble E- selectin in reflecting disease activity of atopic dermatitis: from laboratory parameters to clinical scores. Br J Dermatol 2006 154 (6): 1112–7
Pucci N, Lombardi E, Novembre E. Urinary eosinophil protein X and serum eosinophil cationic protein in infants and young children with atopic dermatitis: correlation with disease activity. J Allergy Clin Immunol 2000 105 (2Pt1): 353–7
Gebhardt M, Wenzel HC, Hipler UC. Monitoring of serologic immune parameters in inflammatory skin diseases. Allergy 1997 52 (11): 1087–94
Miyasato M, Tsuda S, Nakama T. Serum levels of eosinophil cationic protein reflect the state of in vitro degranulation of blood hypodense eosinophils in atopic dermatitis. J Dermatol 1996 23 (6): 382–8
Nakama T. Relationships between eosinophil-associated parameters and disease severity in atopic dermatitis. Kurume Med J 1995 42 (2): 95–106
Kristjansson S, Shimizu T, Strannegard IL. Eosinophil cationic protein, myeloperoxidase and tryptase in children with asthma and atopic dermatitis. Pediatr Allergy Immunol 1994 5 (4): 223–9
Czech W, Krutmann J, Schopf E. Serum eosinophil cationic protein (ECP) is a sensitive measure for disease activity in atopic dermatitis. Br J Dermatol 1992 126 (4): 351–5
Sugai T, Sakiyama Y, Matumoto S. Eosinophil cationic protein in peripheral blood of pediatric patients with allergic diseases. Clin Exp Allergy 1992 22 (2): 275–81
Paganelli R, Fanales-Belasio E, Carmini D. Serum eosinophil cationic protein in patients with atopic dermatitis. Int Arch Allergy Appl Immunol 1991 96 (2): 175–8
Majamaa H, Laine S, Miettinen A. Eosinophil protein X and eosinophil cationic protein as indicators of intestinal inflammation in infants with atopic eczema and food allergy. Clin Exp Allergy 1999 29 (11): 1502–6
Tsuda S, Kato K, Miyasato M. Eosinophil involvement in atopic dermatitis as reflected by elevated serum levels of eosinophil cationic protein. J Dermatol 1992 19 (4): 208–13
Slobodna MS, Jasna L, Vesna Z. Serum eosinophil cationic protein in children with atopic dermatitis. Int J Dermatol 2006 45 (10): 1156–60
Wolkerstorfer A, Laan MP, Savelkoul HF. Soluble E-selectin, other markers of inflammation and disease severity in children with atopic dermatitis. Br J Dermatol 1998 138 (3): 431–5
Arkwright PD, Chase JM, Babbage S. Atopic dermatitis is associated with a low-producer transforming growth factor beta(1) cytokine genotype. J Allergy Clin Immunol 2001 108 (2): 281–4
Lee HJ, Lee HP, Ha SJ. Spontaneous expression of mRNA for IL-10, GMCSF, TGF-beta, TGF-alpha, and IL-6 in peripheral blood mononuclear cells from atopic dermatitis. Ann Allergy Asthma Immunol 2000 84 (5): 553–8
Laiho K, Lampi AM, Hamalainen M. Breast milk fatty acids, eicosanoids, and cytokines in mothers with and without allergic disease. Pediatr Res 2003 53 (4): 642–7
Nowak-Wegrzyn A. Future approaches to food allergy. Pediatrics 2003 111: 1672–80
Matricardi PM, Bjorksten B, Bonini S. Microbial products in allergy prevention and therapy. Allergy 2003 58: 461–71
Acknowledgments
No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Betsi, G.I., Papadavid, E. & Falagas, M.E. Probiotics for the Treatment or Prevention of Atopic Dermatitis. Am J Clin Dermatol 9, 93–103 (2008). https://doi.org/10.2165/00128071-200809020-00002
Published:
Issue Date:
DOI: https://doi.org/10.2165/00128071-200809020-00002