Abstract
Introduction
In recent years, health plans have turned to disease management programs as a means of reducing inpatient utilization while promoting preventive outpatient services provided for patients with type 2 diabetes mellitus.
Aim
The purpose of this study was to assess the association between four preventive diabetes screenings (retinal eye exams, glycosylated hemoglobin [HbA1c] testing, lipid testing, and albumin testing) in the base study period, and health services utilization patterns during a 24-month follow-up study period for 2641 patients with type 2 diabetes.
Methods
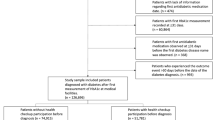
Claims data from Regence BlueShield of Idaho for the three periods of 2000 (base period), 2001, and 2002 (results period) have provided the basis for this empirical analysis. Based on our review of the relevant literature and results from disease management and health plan management programs, the central hypothesis of this study was that the four preventive diabetes screenings in the base study period would be associated with lower inpatient utilization and greater preventive outpatient utilization during a 24-month follow-up study period. Simple linear association analysis was used to measure the relationship between the utilization of preventive diabetes screenings and subsequent utilization of emergency room, inpatient, and preventive outpatient services.
Results
The study results show that for patients who comply with recommended lipid screening services, health plans can expect to see a significant reduction in the number of inpatient admissions over the subsequent 2 years, while marginal inpatient reductions might be expected following HbA1c testing. Furthermore, for patients who comply with recommended screenings of either retinal eye exams or albumin testing, health plans can expect to see these patients utilizing preventive outpatient services more frequently in the subsequent 2 years.
Conclusions
Pursuing a state- or federal-supported screening program for patients with type 2 diabetes could reduce frequent utilization of inpatient services. Furthermore, in support of the goal of disease management programs to reduce inpatient utilization and increase preventive outpatient service utilization among the increasing proportion of members with type 2 diabetes, health plans are encouraged to provide education about and monitor their patients’ compliance with recommended screenings in the future. Further studies should examine the role of lipid testing in reducing the risk of microvascular diseases. Future research should also pursue an understanding of how a reduction in inpatient utilization is associated with an increased emphasis on lipid screening.


Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States 2003, C.f.D.C.a. Prevention, Editor. Atlanta (GA): US Department of Health and Human Services, 2003
Selby JV, Ray GT, Zhang D, et al. Excess costs of medical care for patients with diabetes in a managed care population. Diabetes Care 1997; 20: 1396–402
Krop J, Powe NR, Weller WE, et al. Patterns of expenditures and use of service among older adults with diabetes: implications for the transition to capitated managed care. Diabetes Care 1998; 21: 747–52
Donnon P, Leese GP, Morris AD. Hospitalizations for people with type 1 and type 2 diabetes compared with the nondiabetic population of Tayside, Scotland: a retrospective cohort study of resource use. Diabetes Care 2000; 23: 1774–9
Killilea T. Long-term consequences of type 2 diabetes mellitus: economic impact on society and managed care. Am J Manag Care 2002; 8(16 Suppl.): S441–9
Hogan P, Dall T, Nikolov P. Economic costs of diabetes in the US in 2002. Diabetes Care 2003; 26(3): 917–32
Jiang H, Stryer D, Friedman B, et al. Multiple hospitalizations for patients with diabetes. Diabetes Care 2003; 26: 1421–6
Niefeld M, Braunstein JB, Wu AW, et al. Preventable hospitalization among elderly Medicare beneficiaries with type 2 diabetes. Diabetes Care 2003; 26: 1344–9
Egede L, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care 2002; 25: 464–70
Nichols G, Brown JB. The impact of cardiovascular disease on medical care costs in subjects with and without type 2 diabetes. Diabetes Care 2002; 25: 482–6
Ashton C, Septimus J, Petersen NJ, et al. Healthcare use by veterans treated for diabetes mellitus in the Veterans Affairs Medical Care System. Am J Manag Care 2003; 9: 145–50
Simpson S, Corabian P, Jacobs P, et al. The cost of major comorbidity in people with diabetes mellitus. CMAJ 2003; 168: 1661–7
Brown J, Pedula KL, Bakst AW. The progressive cost of complications in type 2 diabetes mellitus. Arch Intern Med 1999; 159: 1873–80
Ramsey S, Newton K, Blough D, et al. Patient-level estimates of the cost of complications in diabetes in a managed-care population. Pharmacoeconomics 1999; 16: 285–95
CDC Diabetes in Managed Care Work Group. Diabetes mellitus in managed care: complications and resource utilization. Am J Manag Care 2001; 7: 501–8
Selby J, Karter AJ, Ackerson LM, et al. Developing a prediction rule from automated clinical databases to identify high-risk patients in a large population with diabetes. Diabetes Care 2001; 24: 1547–55
Caro J, Ward AJ, O’Brien JA. Lifetime costs of complications resulting from type 2 diabetes in the US. Diabetes Care 2002; 25: 476–81
Bindman A, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA 1995; 274: 305–11
Blustein J, Hanson K, Shea S. Preventable hospitalizations and socioeconomic status. Health Aff 1998; 17: 177–89
Millman ME, editor. Access to health care in America. Washington, DC: Institute of Medicine, 1993
Klarenbach S, Jacobs P. International comparison of health resource utilization in subjects with diabetes: an analysis of Canadian and American national health surveys. Diabetes Care 2003; 26: 1116–22
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of longterm complications in insulin-dependent diabetes mellitus. N Engl J Med 1993; 329(14): 977–86
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet 1998; 352(9131): 837–53
Akinci F, Healey B, Coyne J. Improving the health status of US working adults with type 2 diabetes. Dis Manag Health Outcomes 2003; 11(8): 489–98
Akinci F, Coyne J, Healey B. Interventions for the diabetes disease state: a comparative financial analysis. Chicago (IL): Midwest Business Administration Association, 2003
Akinci F, Coyne J, Healey B, et al. National performance measures for diabetes care: implications for health care providers diabetes. Dis Manag Health Outcomes 2004; 12(5): 285–98
Lafata J, Martin S, Morlock R, et al. Provider type and the receipt of general and diabetes-related preventive health services among patients with diabetes. Med Care 2001; 39: 491–9
Roubideaux Y, Buchwald D, Beals J, et al. Measuring the quality of diabetes care for older American Indians and Alaska Natives. Am J Public Health 2004; 94: 60–5
American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care 2001; 24: S33–43
Wagner E, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q 1996; 74(4): 511–44
Norris S, Nichols PJ, Caspersen CJ, et al. The effectiveness of disease and case management for people with diabetes: a systematic review. Am J Prev Med 2002; 22(4 Suppl.): 15–38
McGlynn E, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003; 348(26): 2635–45
Clark Jr C, Snyder JW, Meek RL, et al. A systematic approach to risk stratification and intervention within a managed care environment improves diabetes outcomes and patient satisfaction. Diabetes Care 2001; 24(6): 1079–86
Saaddine JB, Engelgau MM, Beckles GL, et al. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med 2002; 136(8): 565–74
TRIAD Study Group. The Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care 2002; 25(2): 386–9
Koro C, Bowlin SJ, Bourgeois N, et al. Glycemic control from 1998 to 2000 among US adults diagnosed with type 2 diabetes. Diabetes Care 2004; 27: 17–20
Jencks SF, Cuerdon T, Burwen DR, et al. Quality of medical care delivered to Medicare beneficiaries: a profile at state and national levels. JAMA 2000; 284(13): 1670–6
Jencks S, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries 1998–1999. JAMA 2003; 289(3): 305–12
Welch W, Bersten C, Cutler C, et al. Disease management practices of health plans. Am J Manag Care 2002; 8(4): 353–61
Short A, Mays G, Mittler J. Disease management: a leap of faith to lower-cost, higher-quality health care. Issue Brief Cent Health Syst Change 2003; 69: 1–4
Schauffler H, Chapman SA. Health promotion and managed care: surveys of California’s health plans and population. Am J Prev Med 1998; 14(3): 161–7
Dove H, Duncan I, Robb A. A prediction model for targeting low-cost, high-risk members of managed care organizations. Am J Manag Care 2003; 9(5): 381–9
Rubin RJ, Dietrich KA, Hawk AD. Clinical and economic impact of implementing a comprehensive diabetes management program in managed care. J Clin Endocrinol Metab 1998; 83(8): 2635–42
Domurat E. Diabetes managed care and clinical outcomes: the Harbor City, California Kaiser Permanente diabetes care system. Am J Manag Care 1999; 5(10): 1299–307
Steffens B. Cost-effective management of type 2 diabetes: providing quality care in a cost-constrained environment. Am J Manag Care 2000; 6(13 Suppl.): S697–703
Sadur CN, Moline N, Costa M, et al. Diabetes management in a health maintenance organization: efficacy of care management using cluster visits. Diabetes Care 1999; 22(12): 2011–7
Sidorov J, Shull R, Tomcavage J, et al. Does diabetes management save money and improve outcomes? A report of simultaneous short-term savings and quality improvement associated with a health maintenance organization-sponsored disease management program among patients fulfilling health employer data and information set criteria. Diabetes Care 2002; 25: 684–9
Testa MA, Dimonson DC. Health economic benefits and quality of life during improved glycemic control in patients with type 2 diabetes mellitus: a randomized, controlled, double-blind trial. JAMA 1998; 280(17): 1490–6
Menzin J, Langley-Hawthorne C, Friedman M, et al. Potential short-term economic benefits of improved glycemic control: a managed care perspective. Diabetes Care 2001; 24(1): 51–5
Berg GD, Wadhwa S. Diabetes disease management in a community-based setting. Manag Care 2002; 11(6): 42, 45–50
NCQA. The state of health care quality 2002. Industry trends and analysis. Washington, DC: NCQA, 2002
Mensing C, Boucher J, Cypress M, et al. National standards for diabetes selfmanagement education. Diabetes Care 2002; 25 Suppl. 1: S140–7
Gilmer TP, O’Connor PJ. Cost effectiveness of diabetes mellitus management programs. Dis Manage Health Outcomes 2003; 11(7): 439–53
Acknowledgments
The authors gratefully acknowledge the careful review, insightful comments, and suggestions of both outside and editorial reviewers on an earlier version of this manuscript.
The authors also wish to acknowledge the bibliographical and editorial contributions of Ms Jill Royston, WSU Health Policy and Administration Department Program Assistant, and statistical and graphical analysis assistance from Mr Sher G. Singh.
No sources of funding were used to assist in the preparation of this study. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akinci, F., Coyne, J.S., Minear, J. et al. Examining the Association Between Preventive Screenings and Subsequent Health Services Utilization by Patients with Type 2 Diabetes Mellitus. Dis-Manage-Health-Outcomes 13, 129–135 (2005). https://doi.org/10.2165/00115677-200513020-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-200513020-00006