Abstract
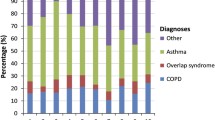
Objectives: The purpose of this study was to evaluate the effects of a recently implemented disease management programme [Asthma Control and Education Program (ACE)] on patient outcomes (clinical and functional) and on resource utilisation in socio-economically disadvantaged (and largely Hispanic) individuals with asthma treated at Hartford Hospital.
Design and Setting: Using standardised measures (i.e. the Health Status Questionnaire [HSQ] and the Center for Epidemiologic Studies Depression Scale) and conducting serial assessments the investigators determined: (i) functional status at intake and follow-up; (ii) change in the level of illness severity over time; (iii) patientss’ acquisition of self-management skills; and (iv) the type and frequency of acute care services utilised pre- and post-enrolment in ACE.
Patient Population:The study participants consisted of consenting individuals, aged 18 years or older, enrolled in ACE from 1 January 1997 to 30 September 1998. Each individual had a comprehensive intake interview (data collected included clinical and financial status) followed by 3 educational sessions.
Results: While only 34.7% (n = 282) of the 813 patients referred from Hartford Hospital to physicians or emergency department services elected to participate in the programme, 60% of participants completed the educational sessions. 73% of these enrollees returned for the 3-month follow-up.
On the HSQ, the mean Physical Composite Summary (PCS) scores increased from 33.3 ± 10.01 at baseline to 41.6 ± 11.48 at the 3-month follow up and 45.3 ± 10.30 at the 6-month follow-up. In an analysis using only those patients (n = 50) with HSQ scores at baseline and 3- and 6-month follow-ups, there were statistically significant increases in both the PCS and the Mental Composite Summary scores (p < 0.001).
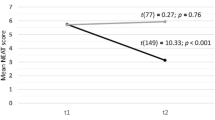
For the 68 patients with severity data at baseline, 3 months and 6 months there was a statistically significant improvement over time (p < 0.001). For example, 4.4% had severe disease at 6 months versus 69.1% at baseline. A subset of 73 patients for whom pre-ACE data were available realised a 37% reduction in emergency department use and a 52% reduction in in-patient visits.
Conclusions: The evaluation of disease management programmes requires outcomes data. The results of this study of an asthma disease management programme indicate there was an improvement in overall functioning, illness severity, self-management, and utilisation of inpatient and emergency department services. Although a cause and effect relationship could not be assumed, the results suggest that the disease management model is an effective one for the studied population of inner-city patients, socioeconomically disadvantaged individuals previously identified as high utilisers of healthcare services and as having significant environmental exposures problematic for patients with asthma. As currently designed, however, this programme does not address the healthcare needs of the large number of referred patients who choose not to enrol or the enrollees (40%) who do not complete the education and follow-up sessions.
Similar content being viewed by others
References
Rice DP, Hodgson TA, Kopstein AN. The economic costs of illness: a replication and update. Health Care Finan Rev 1985; 7: 61–80
Roberts J, Browne GB, Streiner D, et al. The effectiveness and efficiency of health promotion in specialty clinic care. Med Care 1995; 33(9): 892–905
Fries JF. The compression of morbidity: miscellaneous comments about a theme. Gerontologist 1984; 24: 354–9
Goethe JW, Gerulaitis ML, Szarek BL, et al. Measuring outcome: a post-discharge assessment model. In: Mirin SM, Gossett JT, Grob MC, editors. Psychiatric treatment: advances in outcome research. Washington, DC: APA Press, 1991: 293–309
Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions: results from the medical outcomes study. JAMA 1989; 262(7): 907–13
Tarlov AR, Ware JE, Greenfield S, et al. The Medical Outcomes Study: an application of methods for monitoring the results of medical care. JAMA 1989; 262(7): 925–30
Bottorff JL, Johnson JL, Ratner PAA, et al. The effects of cognitive-perceptual factors on health promotion behavior maintenance. Nurs Res 1996; 45(1): 30–6
Fleetwood J, Packa DR. Determinants of health-promoting behaviors in adults. J Cardiovasc Nurs 1991; 5(2): 67–70
Kulbok PA, Baldwin JH. From preventive health behavior to health promotion: advancing a positive construct of health. Adv Nurs Sci 1992; 14(4): 50–64
Freundenberg N, Eng E, Flay B, et al. Strengthening individual and community capacity to prevent disease and promote health: in search of relevant theories and principles. Health Educ Q 1995; 22(3): 290–306
Hyner GC. Strategy for planning and evaluating health risk appraisal and screening interventions. J Health Educ 1995; 26(6): 345–52
Bolton MB, Tilley BC, Kuder J, et al. The cost and effectiveness of an education program for adults who have asthma. J Gen Intern Med 1991; 6: 401–47
Jones KP, Charlton IH, Middletown M, et al. Targeting asthma care in general care practice using a morbidity index. BMJ 1992; 304: 1353–6
National Institutes of Health, National Heart, Lung and Blood Institute Data Fact Sheet, Asthma Statistics, 1992 May
Neuhauser D, Headrick L, Miller DM. The best asthma care: a case problem in continuous quality improvement. Am J Med Q 1992; 7: 76–80
Jones PK, Jones SL, Katz J. Improving compliance for asthmatic patients visiting the emergency department using a Health Belief Model intervention. J Asthma 1987; 24(4): 199–206
US Department of Health and Human Services, Public Health Service. Healthy people 2000: midcourse review and 1995 revisions. Boston (MA): Jones and Bartlett Publishers, 1996: 6–9, 239
Maljanian R, Goethe J, Wolf S, et al. Baseline assessment of an inner city population enrolled in an asthma disease management program: data for continuous programme improvement. Dis Manage Health Outcomes 1999; 5: 135–43
National Institutes of Health. National Heart, Lung and Blood Institute. International consensus report on diagnosis and management of asthma. Eur Respir J 1992; 5: 601–41
Health Status Questionnaire. Bloomington (MN): Health Outcomes Institute, 1993
Ware Jr JE. The SF-36 health survey: manual and interpretation guide. Boston (MA): The Health Intstitute, New England Medical Center, 1993
Cho MJ, Moscicki EK, Narrow WE, et al. Concordance between two measures of depression in the Hispanic Health and Nutrition Survey. Soc Psychiatry Psychiatr Epidemiol 1993; 28: 156–63
Buckstein DA. Practical approach to the use of outcomes in asthma. Immunol Allergy Clin North Am 1996; 16: 859–91
Os’Conner GT, Weis ST. Clinical and symptom measures. Am J Respir Crit Care Med 1994; 149(2 Pt 2): S21–S28
Sullivan S, Elixhauser A, Buist AS, et al. National Asthma Education and Prevention Program Working Group Report on the Cost Effectiveness of Asthma Care. Am J Respir Crit Care Med 1996; 154: S84–S95
Headrick L, Krain E, Evens D, et al. National Asthma Education Prevention Program Working Group on the Quality of Asthma Care. Am J Respir Crit Care Med 1997; 154 Suppl.: SA891
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maljanian, R., Wolf, S., Goethe, J. et al. An Inner-City Asthma Disease Management Initiative. Dis-Manage-Health-Outcomes 5, 285–293 (1999). https://doi.org/10.2165/00115677-199905050-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00115677-199905050-00005