Abstract
Background and objective: Maintenance of effective drug concentrations is essential for adequate treatment of epilepsy. Some antiepileptic drugs can be successfully administered rectally when the oral route of administration is temporarily unavailable. Oxcarbazepine is a newer antiepileptic drug that is rapidly converted to a monohydroxy derivative, the active compound. This study aimed to characterise the bioavailability, metabolism and tolerability of rectally administered oxcarbazepine suspension using a randomised, crossover design in ten healthy volunteers.
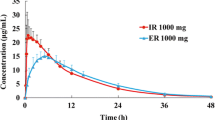
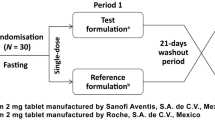
Methods: Two subjects received 300mg doses of oxcarbazepine suspension via rectal and oral routes and eight received 450mg doses. A washout period of at least 2 weeks elapsed between doses. The rectal dose was diluted 1: 1 with water. Blood samples and urine were collected for 72 hours post-dose. Adverse effects were assessed at each blood collection time-point using a self-administered questionnaire. Plasma was assayed for oxcarbazepine and monohydroxy derivative; urine was assayed for monohydroxy derivative and monohydroxy derivative-glucuronide. Maximum plasma concentration (Cmax) and time to reach Cmax (tmax) were obtained directly from the plasma concentration-time curves. The areas under the concentration-time curve (AUCs) were determined via non-compartmental analysis. Relative bioavailability was calculated and the Cmax and AUCs were compared using Wilcoxon signed-rank tests.
Results: Mean relative bioavailability calculated from plasma AUCs was 8.3% (SD 5.5%) for the monohydroxy derivative and 10.8% (SD 7.3%) for oxcarbazepine. Oxcarbazepine and monohydroxy derivative Cmax and AUC values were significantly lower following rectal administration (p < 0.01). The total amount of monohydroxy derivative excreted in the urine following rectal administration was 10 ± 5% of the amount excreted following oral administration. Oral absorption was consistent with previous studies. The most common adverse effects were headache and fatigue with no discernible differences between routes.
Conclusions: Monohydroxy derivative bioavailability following rectal administration of oxcarbazepine suspension is significantly lower than following oral administration, most likely because of poor oxcarbazepine water solubility. It is unlikely that adequate monohydroxy derivative concentrations can be achieved with rectal administration of diluted oxcarbazepine suspension.



Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
de Boer AG, Moolenaar F, de Leede LG, et al. Rectal drag administration: clinical pharmacokinetic considerations. Clin Pharmacokinet 1982 Jul–Aug; 7(4): 285–311
Graves NM, Kriel RL, Jones-Saete C, et al. Relative bioavailability of rectally administered carbamazepine suspension in humans. Epilepsia 1985 Sep–Oct; 26(5): 429–33
Neuvonen PJ, Tokola O. Bioavailability of rectally administered carbamazepine mixture. Br J Clin Pharmacol 1987 Dec; 24(6): 839–41
Arvidsson J, Nilsson HL, Sandstedt P, et al. Replacing carbamazepine slow-release tablets with carbamazepine suppositories: a pharmacokinetic and clinical study in children with epilepsy. J Child Neurol 1995 Mar; 10(2): 114–7
Issakainen J, Bourgeois BF. Bioavailability of sodium valproate suppositories during repeated administration at steady state in epileptic children. Eur J Pediatr 1987 Jul; 146(4): 404–7
Moolenaar F, Greving WJ, Huizinga T. Absorption rate and bioavailability of valproic acid and its sodium from rectal dosage forms. Eur J Clin Pharmacol 1980 May; 17(4): 309–15
Cloyd JC, Kriel RL. Bioavailability of rectally administered valproic acid syrup. Neurology 1981 Oct; 31(10): 1348–52
Holmes GB, Rosenfeld WE, Graves NM, et al. Absorption of valproic acid suppositories in human volunteers. Arch Neurol 1989 Aug; 46(8): 906–9
Dhillon S, Oxley J, Richens A. Bioavailability of diazepam after intravenous, oral and rectal administration in adult epileptic patients. Br J Clin Pharmacol 1982 Mar; 13(3): 427–32
Moolenaar F, Bakker S, Visser J, et al. Biopharmaceutics of rectal administration of drugs in man. IX: comparative biopharmaceutics of diazepam after single rectal, oral, intramuscular, and intravenous administration in man. Int J Pharm 1980 (5): 127-37
Cloyd JC, Lalonde RL, Beniak TE, et al. A single-blind, crossover comparison of the pharmacokinetics and cognitive effects of a new diazepam rectal gel with intravenous diazepam. Epilepsia 1998 May; 39(5): 520–6
Viukari M, Salo H, Lamminsivu U, et al. Pharmacokinetics of diazepam administered rectally in geriatric patients: comparison of suppositories with rectal tubes in a cross-over study. Acta Pharmacol Toxicol (Copenh) 1981 Jul; 49(1): 59–64
Conway JM, Birnbaum AK, Kriel RL, et al. Relative bioavailability of topiramate administered rectally. Epilepsy Res 2003 May; 54(2-3): 91–6
Birnbaum AK, Kriel RL, Burkhardt RT, et al. Rectal absorption of lamotrigine compressed tablets. Epilepsia 2000 Jul; 41(7): 850–3
Birnbaum AK, Kriel RL, Im Y, et al. Relative bioavailability of lamotrigine chewable dispersible tablets administered rectally. Pharmacotherapy 2001 Feb; 21(2): 158–62
Kriel RL, Birnbaum AK, Cloyd JC, et al. Failure of absorption of gabapentin after rectal administration. Epilepsia 1997 Nov; 38(11): 1242–4
Grossmann R, Maytal J, Fernando J. Rectal administration of felbamate in a child with Lennox-Gastaut syndrome. Neurology 1994 Nov; 44(10): 1979
Moolenaar F, Jelsma RBH, Visser J, et al. Manipulation of rectal absorption rate of phenytoin in man. Pharm Weekbl [Sci] 1981; 3: 1051–6
Chang SW, da Silva JH, Kuhl DR. Absorption of rectally administered phenytoin: a pilot study. Ann Pharmacother 1999 Jul–Aug; 33(7-8): 781–6
Burstein AH, Fisher KM, McPherson ML, et al. Absorption of phenytoin from rectal suppositories formulated with a polyethylene glycol base. Pharmacotherapy 2000 Jun; 20(5): 562–7
Van Parys JA, Meinardi H. Survey of 260 epileptic patients treated with oxcarbazepine (Trileptal) on a named-patient basis. Epilepsy Res 1994 Sep; 19(1): 79–85
Bill PA, Vigonius U, Pohlmann H, et al. A double-blind controlled clinical trial of oxcarbazepine versus phenytoin in adults with previously untreated epilepsy. Epilepsy Res 1997 Jun; 27(3): 195–204
Christe W, Kramer G, Vigonius U, et al. A double-blind controlled clinical trial: oxcarbazepine versus sodium valproate in adults with newly diagnosed epilepsy. Epilepsy Res 1997 Mar; 26(3): 451–60
Glauser TA, Pippenger CE. Controversies in blood-level monitoring: reexamining its role in the treatment of epilepsy. Epilepsia 2000; 41Suppl. 8: S6–15
van der Kuy PH, Koppejan EH, Wirtz JJ. Rectal absorption of oxcarbazepine. Pharm World Sci 2000 Aug; 22(4): 165–6
Mandrioli R, Ghedini N, Albani F, et al. Liquid Chromatographic determination of oxcarbazepine and its metabolites in plasma of epileptic patients after solid-phase extraction. J Chromatogr B Analyt Technol Biomed Life Sci 2003 Jan 5; 783(1): 253–63
Faigle JW, Menge GP. Pharmacokinetics and metabolic features of oxcarbazepine and their clinical significance: comparison with carbamazepine. Int Clin Psychopharmacol 1990; 5Suppl. 1: 73–82
van Hoogdalem E, de Boer AG, Breimer DD. Pharmacokinetics of rectal drug administration. Part I: general considerations and clinical applications of centrally acting drugs. Clin Pharmacokinet 1991 Jul; 21(1): 11–26
Flesch G, Tudor D, Denouel J, et al. Assessment of the bioequivalence of two oxcarbazepine oral suspensions versus a film-coated tablet in healthy subjects. Int J Clin Pharmacol Ther 2003 Jul; 41(7): 299–308
Novartis Pharmaceuticals. Trileptal® prescribing information [online]. Available from URL: http://www.pharma.us.novartis.com/product/pi/pdf/trileptal.pdf [Accessed 2006 May 16]
Acknowledgements
This study was supported by Novartis Pharmaceuticals, the University of Minnesota and the American Foundation for Pharmaceutical Education. Novartis provided input during study design and reviewed the manuscript, but final decisions were made by the authors. The authors have no conflicts of interest that are directly relevant to the content of this study. The authors would like to thank Joseph D’Souza, PhD, of Novartis Pharmaceuticals for his assistance during the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clemens, P.L., Cloyd, J.C., Kriel, R.L. et al. Relative Bioavailability, Metabolism and Tolerability of Rectally Administered Oxcarbazepine Suspension. Clin. Drug Investig. 27, 243–250 (2007). https://doi.org/10.2165/00044011-200727040-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00044011-200727040-00003