Abstract
Objective
To compare the bioavailability of two metered-dose inhalers (MDIs) containing salbutamol (albuterol) by means of a spirometric evaluation of the time-course of bronchodilation in patients with moderate asthma.
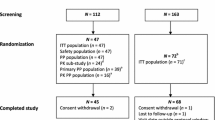
Design and patients
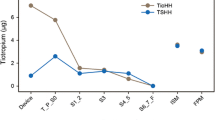
25 asthmatic patients (12 males, 13 females) participated in the study. Study participants received salbutamol 200μg (Ventolin®, GlaxoSmithKline Mexico City, or Assal®, Salus SA de CV, Mexico City) on separate days according to a double-blind, crossover design. Spirometry was performed 30 minutes before and at selected times during the 8 hours following drug administration. The time-course of changes in forced expiratory volume in 1 second (FEV1) [transformed to individual percentage of maximal response] was used to compare the formulations. Pharmacodynamic parameters, maximal effect (Emax) and area under the percentage of response-time curve (AUC) were obtained and compared by analysis of variance, and ratios of AUC and Emax and 90% confidence limits were calculated.
Results
Values obtained for Emax were 94.81 ± 2.19% and 84.45 ± 3.44% for Ventolin® and Assal®, respectively, whereas values for AUC were 25 278 ± 1873 %·min and 18 155 ± 1806 %·min, respectively. Ratios were 89.1 and 71.8% with 90% confidence limits of 79.6 to 98.5% and 53.9 to 89.7% for Emax and AUC, respectively. The probability according to the two one-sided t-test of having values lower than 80% was higher than 0.05 for both AUC and Emax, indicating that the formulations tested are not bioequivalent.
Conclusions
It is concluded that this method is suitable for comparing the bio-availability of MDI formulations of bronchodilatory agents and that the formulations tested were not bioequivalent.







Similar content being viewed by others
Notes
1Tradenames are used for product identification only and do not imply endorsement.
References
Taburet A–M, Schmit B. Pharmacokinetic optimisation of asthma treatment. Clin Pharmacokinet 1994; 26: 396–418
Steinijans VW, Hauschke D, Jonkman JHG. Controversies in bioequivalence studies. Clin Pharmacokinet 1992; 22: 247–53
Chrystyn H. Standards for bioequivalence of inhaled products. Clin Pharmacokinet 1994; 26: 1–6
Byron PR. Inhalation devices. In: D’Arcy PF, McElnay JC, editors. The pharmacy and pharmacotherapy of asthma. Chichester: Ellis Horwood Ltd, 1989: 137–159
Chege JK, Chystyn H. Volumatic usage: some generic albuterol metered dose inhalers can be used. Thorax 1994; 49: 1162–3
Watson JP, Lewis RA. Generic albuterol metered dose inhalers. Thorax 1995; 50: 590
Clark DJ, Gordon-Smith J, McPhate G, et al. Bioavailability of generic and innovator albuterol metered dose inhalers. Thorax 1996; 51: 325–6
Steinijans VW, Neuhäuser M, Hummel T, et al. Asthma management: the challenge of equivalence. Int J Clin Pharmacol Ther 1998; 36: 117–25
Global Initiative for Asthma. A practical guide for public health officials and health care professionals. Medical Communication Resources Inc. NIH publication No 96-3659A, 1995 Dec
American Thoracic Society. Medical Section of the American Lung Association. Standarization of Spirometry [update]. 1994 Nov 11
Blake KV, Harman E, Hendeles L. Evaluation of a generic albuterol metered-dose inhaler: importance of priming the MDI. Ann Allergy 1992; 68: 169–74
Rowland M, Tozer TN. Clinical pharmacokinetics: concepts and applications. 2nd ed. Philadelphia: Lea & Febiger, 1989
Schuirmann DJ. A comparison of the two one-sided tests procedure and the power approach for assessing the equivalence of average bioavailability. J Pharmacokinet Biopharm 1987; 15: 657–80
Sanchis-Aldás J, Casan-Clara P, Castillo-Gómez J, et al. Espirometría Forzada. In: Caminero-Luna JA, Fernández-Fau L, editors. Recomendaciones SEPAR. Sociedad Española de Neumología y Cirugía Torácica (SEPAR). Barcelona, 1998: 1–18
Bowers A. Regulatory considerations associated with the in vivo bioequivalence assessment of metered-dose inhalers. Drug Inf J 1995; 29: 941–59
Newhouse MT. The current laboratory determination of ‘respirable mass’ is not clinically relevant. J Aerosol Med 1998; 11: S122–32
Ahrens RC, Harris JB, Milavetz G, et al. Use of bronchial provocation with histamine to compare the pharmacodynamics of inhaled albuterol and metaproterenol in patients with asthma. J Allergy Clin Immunol 1987; 79: 876–82
Mitchell CA, Armstrong JG, Bartholomew MA, et al. Nebulized fenoterol in severe asthma: determinants of the dose response. Eur J Respir Dis 1983; 64: 340–6
FDA 1996. Transcript of the Advisory Committee for Pharma-ceutical Science and Pulmonary-Allergy Drugs Advisory Committee Center for Drug Evaluation and Research, Food and Drug Administration. Washington: Associated Reporters of Washington, 1996 Aug 16
Acknowledgements
This study was supported by The Instituto Nacional de Enfermedades Respiratorias, México, and Escuela Superior de Medicina, Instituto Politécnico Nacional, México.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
León-Molina, H., Flores-Murrieta, F.J. & Chapela, R. Assessment of Comparative Bioequivalence of Two Metered-Dose Inhaler Formulations of Salbutamol. Clin. Drug Investig. 22, 435–441 (2002). https://doi.org/10.2165/00044011-200222070-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00044011-200222070-00003