Summary
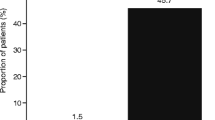
The aim of this study was to compare the efficacy and safety of propafenone (2 mg/kg intravenously over 10 minutes) and digoxin (0.007 mg/kg intravenously over 10 minutes) in the conversion of recent onset <72 hours) atrial fibrillation to sinus rhythm. A consecutive series of 50 uncomplicated patients (no contraindications to either drug and without clinical heart failure) was randomly divided into 2 groups of 25 patients each. The 2 groups were similar in age, gender, concomitant diseases, previous paroxysmal atrial fibrillation, duration of the arrhythmia, electrocardiographic parameters, basal blood pressure and 2D-echocardiographic profile. Sinus rhythm was restored in a higher percentage of propafenone-treated patients [22 of 25 patients (88%) vs 8 of 25 (32%); p = 0.00005] and within a shorter time period (mean 22 vs 96 minutes; p = 0.0004) relative to digoxin-treated patients. The study design allowed for conditional crossover of patients who did not respond to initial drug treatment. 11 of 17 patients who did not respond to digoxin were treated with propafenone; conversion to sinus rhythm was achieved in 6 of 11 (54%) patients within 3 hours. No clinically relevant adverse effects were noted in either treatment group. Neither treatment gave rise to any significant modification in QRS- or QTc-interval morphology. In the propafenone group, normal left atrium measurement values (anteroposterior diameter, longitudinal diameter, transversal diameter and a preserved ejection fraction) were considered predictive factors for conversion to sinus rhythm. Additionally, the high percentage of early conversions obtained with propafenone allowed earlier discharges in this group of patients compared with that of digoxin. In conclusion, propafenone was well tolerated and was more effective than digoxin in the treatment of patients with recent onset atrial fibrillation. The drug offered advantages over digoxin with respect to its rapid onset of action and reduction in the number of patients who required hospitalisation.
Similar content being viewed by others
References
Takahashi N, Seki A, Imataka K, et al. Clinical features of paroxysmal atrial fibrillation, an observation of 94 patients. Jpn Heart J 1981; 22: 143–7
Holzman D, Brown MG. The use of quinidine in established auricular fibrillation and flutter. Am J Med Sci 1951; 222: 664–8
Halpern SW, Ellrodt G, Singh BN, et al. Efficacy of intravenous procainamide infusion in converting atrial fibrillation to sinus rhythm. Relation to left atrial size. Br Heart J 1980; 44: 589–96
Gronda M, Occhetta E, Magnani A, et al. Cardioversione del flutter e della fibrillazione atriale con amiodarone ad alte dosi. G Ital Cardiol 1982; 44: 589–96
Goy JJ, Grbic M, Hurni L, et al. Conversion of supraventricular arrhythmias to sinus rhythm using flecainide. Eur Heart J 1985; 6: 518–23
Haft JI, Habbab MA. Treatment of atrial arrhythmias: effectiveness of verapamil when preceded by calcium infusion. Arch Intern Med 1986; 146: 1085–9
Capucci A, Gubelli S, Carini GC, et al. Cardioversione farmacologica can propafenone di fibrillazione atriale stabile di recente insorgenza. G Ital Cardiol 1987; 17: 975–82
Villani GQ, Rosi A, Piepoli M, et al. Efficacia del trattamento orale con flecainide nella fibrillazione atriale parossistica: Correlazione con le concentrazioni plasmatiche. G Ital Cardiol 1990; 20: 564–9
Alboni P, Capucci A, Marconi M, et al. Linee guida aile indicazioni e modalità per la conversione a ritrno sinusale della fibrillazione atriale. Cardiostimolazione 1993; 11: 398–404
Rawles JM, Metcaefe MJ, Jennings K. Time of occurrence, duration and ventricular rate of paroxysmal atrial fibrillation: the effect of digoxin. Br Heart J 1990; 63: 225–7
Falk RH, Leavitt JI. Digoxin for atrial fibrillation: a drug whose time has gone. Ann Intern Med 1991; 114: 573–5
Connolly SJ, Mulji AS, Hoffert DL, et al. Randomized placebo-controlled trial of propafenone for treatment of atrial tachy-arrhythmias after cardiac surgery. J Am Coll Cardiol 1987; 10: 1145–8
Bellandi F, Cantini F, Pedone T, et al. Efficacia del Propafenone e dell’ Amiodarone endovena nella conversione della fibrillazione atriale recente. G Ital Cardiol 1993; 23: 261–71
Tisi G, Annoni P, Baroffio R, et al. Il trattamento d’emergenza delle tachiaritmie sopraventricolari. Cardiologia 1992; 37: 621–5
Bianconi L, Boccadamo R, Pappalardo A, et al. Effectiveness of intravenous propafenone for conversion of atrial fibrillation and flutter of recent onset. Am J Cardiol 1989; 64: 335–8
Gaita F, Tartaglino B, Vitolo P, et al. Efficacia di due diversi dosaggi di propafenone ev nella cardioversione della fibrillazione atriale parossistica. Cardiologia 1991; 36/12Suppl. 2: 117
Belz GG, Doering W, Munkes R, et al. Interaction between digoxin and calcium antagonist and antiarrhythmic drugs. Clin Pharmacal Ther 1983; 33: 410–7
Funk-Brentano C, Kroemer HK, Lee TJ, et al. Propafenone. N Engl J Med 1990; 322: 518–25
Falk RH, Knowlton AA, Bernard SA, et al. Digoxin for converting recent-onset atrial fibrillation to sinus rhythm. Ann Intern Med 1987; 106: 503–6
Sellers TD, Bashore TM, Gallagher JJ. Digitalis in the pre-excitation syndrome: analysis during atrial fibrillation. Circulation 1977; 50: 260–7
Buscarini L, Imberti D. Elevata incidenza di ripristino spontaneo del ritmo sinusale in pazienti con fibrillazione atriale parossistica. G Ital Cardiol 1992; 22: 949–52
Sanfilippo AJ, Abascal VM, Sheehan M, et al. Atrial enlargement as a consequence of atrial fibrillation. A prospective echocardiographic study. Circulation 1990; 82: 792–7
Roy D, Marchard E, Gange P, et al. Usefulness of anticoagulant therapy in the prevention of embolic complications of atrial fibrillation. Am Heart J 1986; 112: 1039–43
Lavanga S, Sanna GP. Repeated i.v. boluses of propafenone for acute atrial fibrillation: a randomized placebo-controlled trial [abstract]. Circulation 1992; 864Suppl. 1: 664
Proclemer A, Miorelli M, Pavan A, et al. Intravenous propafenone in paroxysmal atrial fibrillation: a randomized, placebo controlled, double-blind, multicentre clinical trial [abstract]. J Am Coli Cardiol 1994; 24 (Special issue): 368A
Capucci A, Boriani G, Botto GL, et al. A controlled study on efficacy and safety of a single oral loading dose of propafenone or flecainide in converting recent onset atrial fibrillation to sinus rhythm [abstract no. 743-4]. J Am Coli Cardiol 1993; 21Suppl. A: l7lA
Brodsky MA, Allen BJ, Abata D, et al. Propafenone therapy for ventricular tachycardia in the setting of congestive heart failure. Am Heart J 1985; 110: 794–9
Author information
Authors and Affiliations
Additional information
Via Galvani, 103 - 20025 Legnano (MI), Italy.
Rights and permissions
About this article
Cite this article
Baroffio, R., Tisi, G., Guzzini, F. et al. A Randomised Study Comparing Digoxin and Propafenone in the Treatment of Recent Onset Atrial Fibrillation. Clinical Drug Investigation 9, 277–283 (1995). https://doi.org/10.2165/00044011-199509050-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00044011-199509050-00005